Abstract
Purpose
Revision surgery for component malrotation in the painful TKA is a relatively novel indication. The purpose of this study was to assess the benefit of revision TKA for component malrotation with regard to the clinical and functional outcomes.
Methods
Our retrospective case–control study included 51 patients who underwent revision surgery for malrotation with mean follow up of 42 months. They were equally matched to patients who had surgery for aseptic loosening.
Results
Knee society scores improved from 44/49 to 75/60 (p < 0.001) for the study group and 44/47 to 76/57 (p < 0.001) for the control group. There was no statistical difference between the groups, including for VAS scores, narcotic reduction or patient satisfaction. Our study showed that revision surgery for malrotation is as beneficial as surgery for aseptic loosening with regard to clinical and functional outcome.
Conclusions
We recommend CT in painful TKA to assess component malrotation for which revision TKA is beneficial.
Introduction
Despite the long-term clinical success of total knee arthroplasty (TKA), with a ten-year survivorship of approximately 95 %, a small percentage of patients will experience clinical failure due to pain and impaired function [1, 2]. This clinical failure can be divided into early and late. The aetiologies of dysfunction and pain after total knee replacement can be numerous, therefore a systematic approach is required. The Australian Joint Registry 2011 reported on more than 11,000 TKA revisions. The most prevalent indications for revision were loosening (35 %), infection (17 %), pain (10 %) and patellofemoral pain (10 %) [1]. Studies have shown that 19 % of patients are dissatisfied at one year after TKA with regard to pain relief and function [3].
A full discussion regarding the assessment of the painful knee is beyond the scope of this paper however it begins with a history focused on whether there was ever a pain-free period after surgery, the relationship to activity, and the location of the pain. Physical examination should assess for visible signs of infection, limb alignment, range of motion, patellar tracking and joint stability. Initial investigations must rule out infection with ESR, C-reactive protein. Often joint aspiration for WBC count, PMN percentage and culture is also indicated. Plain radiographs including full length standing are needed to assess mechanical axis alignment, joint line height, lateral alignment, component size, overhang and loosening.
Component malrotation has previously been recognised as an early onset cause for a painful primary TKA [4–8]. Malrotation relates to the femoral component relative to the epicondylar axis of the femur and the tibial base plate relative to the tibial tubercle. Subtle internal rotation of the femoral and tibial component can only be accurately measured using CT scan. Gross malrotation may cause patellar dislocation, excessive patellofemoral pressure and may be evident on plain radiographs [9].
Since 2004 the senior author has been revising total knee arthroplasty in patients who complain of a painful knee with a routine negative work up and in whom CT shows component internal malrotation. In this retrospective, single-surgeon study we assessed the patient pre-op pain history and location, function, scores and imaging studies and their post revision outcomes. We postulated that component malrotation is a not-uncommon cause of pain and dysfunction in patients and that revision of these components would relieve pain and improve function in a significant number of patients. The primary outcome assessed was the clinical and functional results as measured by the Knee Society Clinical and Functional Scores. Secondary measures included VAS, narcotic consumption and patient satisfaction assessment. These outcomes were compared to a “gold standard” control group of patients whose indication for revision surgery was TKA aseptic loosening. Our hypothesis was that patients undergoing surgery for malrotation do as well as those having surgery for aseptic loosening.
Patients and methods
Fifty-seven patients underwent revision TKA between 2004 and 2011 for the indication of component malrotation. All patients underwent primary TKA at other institutions and were referred to our tertiary arthroplasty revision centre. This retrospective study was based on data collected in our prospective database. Surgery was performed by a single surgeon (DB). Inclusion criteria for the study group included a painful sometimes stiff knee with CT showing preoperative combined internal rotation of more than 3° of the femoral and tibial component or at least 2° of internal rotation of one component, relative to the neutral component rotation. Neutral rotation was defined as 18° of internal tibial component rotation, relative to tibial tubercle. Infection and aseptic loosening were eliminated as potential sources of pain in the study group using blood analysis of sedimentation rate (ESR) and C-reactive protein (CRP) levels as well as radiographs and CT scan. Patients who had evidence of infection on serology or culture, radiographic or intraoperative findings of component loosening were excluded. Full-length standing radiographs were used to rule out mechanical axis mal-alignment. Four patients were excluded from the study group for incomplete data including absence of CT scan and an additional two patients were excluded due to lack of follow up. This left 51 patients, 22 male and 29 female; mean age was 68 years (range 47–84) in the study group. The minimal follow-up time was one year and average follow-up time was 42 months. The study was commenced after institutional review board approval. We included 24 patients whom we have previously reported upon [8].
A control group of 51 patients who underwent revision knee surgery for aseptic loosening over the same study period were matched for age, gender, preoperative Knee Society clinical score (KSS), and Knee Society functional score. Patients were matched to controls in a 1:1 ratio. This group of patients with aseptic loosening was chosen as a “gold standard” control group with the thought that revision for this reason is clearly indicated as loose components cause significant pain which is predictably improved by revision surgery. If patients with malrotation improve as much as patients with aseptic loosening after revision arthroplasty then surgery for malrotation is justified in the opinion of the authors.
Patients were asked to report maximal pain pre-op and on most recent follow up using a 0–10 visual analogue scale (VAS.) Additional information regarding narcotic use was also obtained as well as satisfaction with the result of revision surgery using a simple yes/no scale. Patella maltracking was assessed radiographically using the skyline view. The primary outcome measured was improvement in functional and clinical Knee Society scores and failure as defined by further surgery.
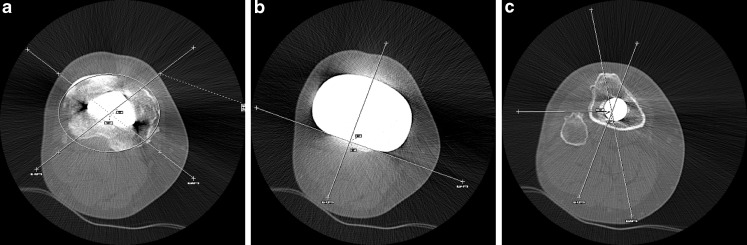
Component rotation was assessed according to the method described by Berger in accordance with the digital picture archiving system available to us (eFILM viewer, Irvine, CA.) [4]. All measurements were undertaken by a single orthopaedic surgeon, uninvolved in the surgery (AS). Tibial component rotation was measured by the angle between the axial tibial component axis and the tibial tubercle axis, as determined by three slices. The geometric centre of the proximal plateau was identified (Fig. 1). Next, a line was drawn perpendicular to the posterior condylar axis of the tibial component, with it translated so that it bisected the geometric centre in the AP axis. Both were transposed to a slice showing the most protuberant tip of the tibial tubercle. A line was then drawn from the tip through the geometric centre, with the angle produced being the rotation of the tibial component. The tibial component was considered neutral when internally rotated 18° in relation to the protuberance of the tibial tubercle. Femoral component rotation was measured at the epicondylar level, as the angle between the transepicondylar axis, connecting the tip of the lateral epicondyle to the sulcus of the medial epicondyle and the posterior condylar axis of the femoral component (Fig. 2). Both tibial and femoral component rotation angles were considered as positive when in external rotation. Internal rotation was considered as mal-rotation and was depicted as a negative value.
Fig. 1.
Tibial component rotational assessment using an axial CT in a 61-year-old male. a The geometric centre of the proximal tibial plateau is determined using an ellipse delineating the tibial plateau. b A line perpendicular to the posterior condylar axis of the tibial component is constructed. c The tibial component rotational angle is determined to be 14° of excessive internal rotation, by transposing the geometric centre as measured in A and the perpendicular line as measured in B to the tibial tuberosity slice and connecting the centre to the protuberant point of the tibial tubercle
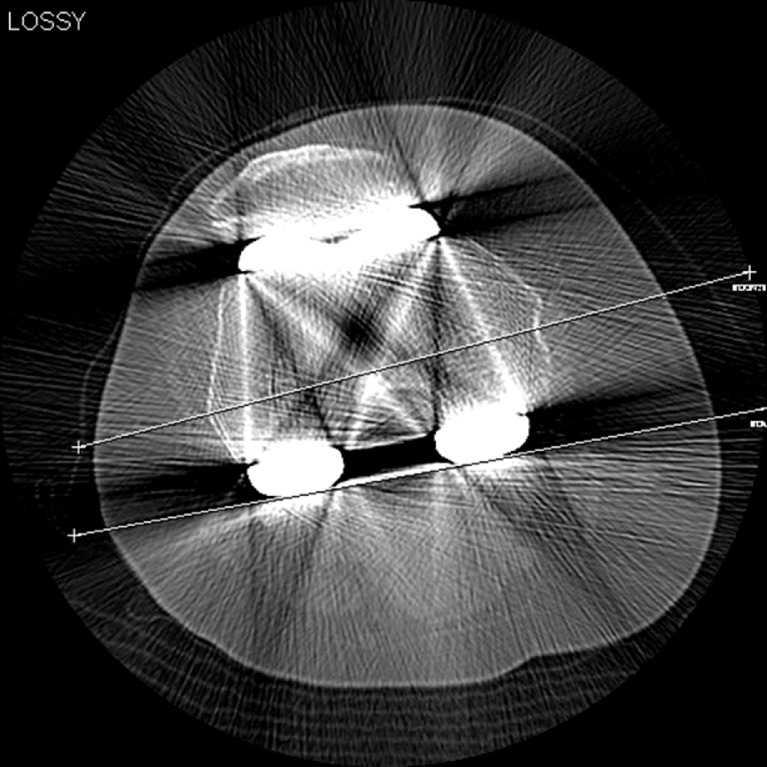
Fig. 2.
Femoral component rotational assessment using an axial CT. The angle between the transepicondylar axis and the posterior condylar axis is measured as 4° internal rotation of the femoral component in a 55-year-old female
Revision surgery used the medial parapatellar approach. Malrotation was confirmed intraoperatively by the senior author by comparing the femoral component to the epicondylar line and the tibial component to the line connecting the tibial centre to the tibial tubercle. To facilitate exposure, tibial tubercle osteotomy was performed in two cases in each group. Replacement of both components was required in all but four cases in which the tibia was revised in two and the femur alone in the other two for the malrotation group. The tibia was alone revised in two cases for the loosening group. Revision components were rotationally aligned relative to transepicondylar axis for the femoral component and the middle third of the tibial tubercle for the tibial component. In all cases, revised components were placed in positions of greater external rotation than that of the index surgery. Augments were used not only to reconstruct the joint line and bone loss in revision surgery but to correct rotation as well. To insure adequate femoral external rotation, postero-lateral augments were used in 28 cases. Offset stems were also used to correct rotation in particular for the tibia where they were used in 46 cases. A semi-constrained prosthesis [LCCK (Zimmer, Warsaw, IN)] was used in 23 cases while purposely leaving a loose flexion gap in order to improve range of motion; otherwise a posterior-stabilised prosthesis [LPS-Flex (Zimmer, Warsaw, IN)] was used. Patellar tracking was assessed at the conclusion of each revision to ensure that lateral tilt was not present.
Follow-up visits routinely occurred at six weeks, 12 weeks, six months, and one year after the procedure and then annually with assessments including the KSS and function score.
Statistical analysis
Data analysis was performed using SPSS 16.0 (Chicago, IL). Discrete variables were analysed using χ2 test or Fisher’s test. Continuous variables were compared using the t-test for independent samples. Subgroup analysis was performed using one-way ANOVA. Differences of p < 0.05 were considered to be statistically significant.
Results
Fifty-one patients underwent revision surgery for malrotation with mean follow up of 42 months (range 12–95, SD 23.6). Demographic, clinical and functional scores are summarised in Table 1. Mean pre-operative femoral component rotation was −1.3° (range, −8.5 to 5; SD, 2.5) and mean tibial rotation angle was −2.1° (range, −18 to 10; SD, 6.0). Mean combined rotation was −3.5° (range, −21 to 8, SD, 6.0).
Table 1.
Demographics and clinical and functional scores of 51 patients with component malrotation compared to a control group of 51 patients with aseptic loosening after total knee arthroplasty
| Characteristic | Malrotation group | Loosening group | p-value |
|---|---|---|---|
| Age (years) | 68 (47–84) | 69 (44–87) | 0.52 |
| M:F | 22:29 | 23:28 | 0.84 |
| Follow-up (months) | 42 (12–95) | 40 (12–92) | 0.55 |
| Interval from index surgery (months) | 30 (5–139) | 128 (20–254) | <0.001 |
| Pre-operative KSS score (/100) | 44 (2–74) | 44 (13–68) | 0.92 |
| Post-operative KSS score (/100) | 75 (43–99) | 76 (44–94) | 0.71 |
| KSS score difference | 31 (1–88) | 32 (9–61) | 0.69 |
| Pre-operative function score (/100) | 49 (25–90) | 47(10–70) | 0.27 |
| Post-operative function score (/100) | 60 (30–100) | 57 (30–90) | 0.25 |
| Function score difference | 11 (−15 to 55) | 10 (0–20) | 0.67 |
| Pre-operative ROM arc (°) | 93 (10–130) | 95 (5–130) | 0.57 |
| Post-operative ROM arc (°) | 103 (20–130) | 106 (55–130) | 0.47 |
| Pre-op VAS score (/10) | 7.1 (3–10) | 6.1 (2–9) | <0.01 |
| Post-op VAS score (/10) | 2.7 (0–9) | 2.5 (0–6) | 0.58 |
| Pain score difference | −4.3 (−9 to 2.5) | −3.6 (−7 to −1) | 0.12 |
| Pre-op narcotic use (Y/N) | 26 (51 %) | 17 (33 %) | 0.07 |
| Post-op narcotic use (Y/N) | 8 (16 %) | 7 (14 %) | 0.78 |
The KSS improved from 44 ± 9 to 75 ± 16 (p < 0.001) at the last follow up for the study group. In comparison to the control group, KSS difference was 31 ± 17 versus 32 ± 13 (p = 0.69). The functional score improved from 49 ± 10 to 60 ± 16 (p < 0.001) for the study group. The functional score improvement was 11 ± 16 versus 10 ± 8 (p = 0.67) for the study group and control group, respectively.
Of the 15 patients who had a ROM arc under 90° pre-operatively (mean 59°, range 10–85°), eight remained stiff at last follow up (mean 70°, range 20–85°).
Fifteen patients in the study group had radiographic patella maltracking pre-operatively compared to none at last follow up. VAS scores were higher pre-operatively for the study group compared to the control group (p < 0.01). The reduction in score in the study group was from 7.1 ± 1.5 to 2.7 ± 2.5 (p < 0.001). Narcotic consumption reduced amongst patients from 26 (51 %) to eight (16 %) at last follow up (p < 0.0001). Thirty-eight patients (75 %) were satisfied with the result of their revision operation compared to 40 patients (79 %) in the loosening group (p = 0.64). Two patients (4 %) underwent further revision surgery in the control group for further aseptic loosening. There were no failures in the study group (p = 0.50).
The malrotation cohort was subdivided into three groups depending upon the predominant component rotation, i.e. femoral, tibial or combined. Subgroup analysis did not show any significant difference for KSS change (p = 0.21). No correlation was found between the degree of combined malrotation and location and degree of pain or limited ROM.
Discussion
Revision TKA for the indication of component malrotation was associated with significant improvement in this group of patients. The improvement was shown in the Knee Society score (KSS) which improved from 44 ± 9 to 75 ± 16 (p < 0.001), the functional score which improved from 49 ± 10 to 60 ± 16 (p < 0.001) and narcotic consumption which was reduced amongst study patients from 51 % to 16 % (p < 0.01). These results were comparable to the control group of patients with aseptic loosening, thus supporting our hypothesis that surgery for malrotation is as beneficial. Three quarters of the patients in the study group reported that they were satisfied with their revision outcome and felt they had made the right choice to proceed with the revision. There were no failures as measured by re-revision in the study group.
Patients with aseptic loosening were chosen as the control group since it is recognised that a loose component is a significant pain generator that once revised and stable would result in less pain and improvement in function. The control group which was revised for component loosening differed from the malrotation group in that they had a long period after their primary arthroplasty in which they were pain free. This is reflected in the time between the primary arthroplasty and their revision. This interval is significantly shorter in the malrotation group in comparison to the loosening group (Table 1). Patients in the malrotation group often never had a pain free period after their primary arthroplasty. This also correlates with the intra-operative impression that at least one component was loose in the control group and none were loose in the malrotation group. This study was powered to demonstrate that malrotation is equally good an indication for revision TKA as aseptic loosening.
Despite the success of this operation for the majority in the study group, not all patients improved after revision of their malrotated components. One quarter were not satisfied with their result. Eight patients (16 %) remained limited in their range of motion even after the revision. Subgroup analysis was employed to better understand the causative relation between malrotation and the location of pain, the degree of malrotation and outcomes, and the influence of the tibial and femoral component malrotation separately on pain location and outcome. Patellar maltracking did not significantly correlate with the degree of malrotation. These subgroup comparisons were not significant, thus pointing to the current limits of our understanding.
Our outcomes suggest that revision TKA for malrotation produces results which are inferior to results for primary TKA. While this is not surprising, it highlights the importance of achieving correct component rotation during the primary procedure [10]. While it is not known what proportion of all patients with internally rotated components are symptomatic, this study indicates that when the painful TKA presents with documented malrotation, symptoms can probably be improved by corrective revision surgery. In 51 cases we had no reoperations.
There are several limitations to this study. The first is the lack of post-operative rotation measurement with a CT. We can only assume based on intra-operative judgement and the knowledge of each patients’ pre-operative rotation, that the malrotation was completely corrected with the revision. A second limitation is the retrospective nature of this study. A third limitation is the short-term follow-up with an average of 42 months. An additional limitation relates to the study group which was formed by searching our database for patients who underwent revision TKA with a diagnosis of malrotation and had a CT to assess the degree of malrotation. The degree of malrotation was confirmed by one author. Inter- and intra-observer reliability was not assessed. The reliability of CT measurement of component rotation has been shown to be adequate for the femoral and tibial component [11]. Bergers technique for assessing tibial component rotation, although commonly used and shown to correlate with intra-operative assessment, has not been validated.
Anecdotally, by history, most patients report that pain after the primary TKA was present from the immediate post-operative period, that there was never a pain-free period and that the knee “just never felt right.” We have also found that patients often have the ability to sense if the revision surgery has made a difference almost immediately. We believe that after infection has been excluded as a cause of painful TKA, that CT is beneficial not only in assessing malrotation but also in ruling out loosening where it is not obvious radiographically.
As previously reported, preoperative assessment of component malrotation with plain film radiographs was not found to be an effective method of assessing the degree of malrotation, especially in the tibia [7]. CT measurement depends on the technical ability of the work station to transcend points between serial axial cuts in order to assess tibial rotation. This technique is accurate and reproducible [4, 11, 12]. Intra-operative assessment of component rotation in primary knee arthroplasty relies on several landmarks. Femoral component rotation should be perpendicular to Whiteside’s line and parallel to the trans-epicondylar line. The tibial component rotation may be assessed relative to the anterior tibial border, the medial third of the tibial tuberosity, or the medial third of the patellar tendon [5]. Often when the tibial base plate is placed in such a manner some exposed bone is left uncovered in the posteromedial corner and the base plate may overhang on the lateral side. When this occurs we downsize the base plate and leave the rotation unchanged. Intraoperative rotational alignment in revision knee surgery is assessed by a limited number of landmarks, namely, the transepicondylar axis for the femoral component and the tibial tuberosity for the tibial component.
Several techniques were employed intra-operatively to improve outcomes. In the femur, the epicondyles were referenced for rotational alignment and joint height. Distal augments were used to reconstruct the joint line in 51 % of patients, which should be 2.5–3 cm distal to the epicondyles. A postero-lateral augment was used in 55 % of patients to enhance the posterior condyle and thus improve the external femoral component rotation. In most cases, the posterolateral condyle was deficient since it had been overcut in the primary arthroplasty leading to excessive internal rotation of the femoral component. In order to improve range of motion knees were left with a slightly larger flexion and extension gap. Constrained condylar prostheses were used in 45 % of patients in order not to compromise medial-lateral stability. Offset stems were used in almost all patients, predominantly on the tibial side, in order to improve component location relative to the medullary canal and avoid an overhanging tibial component. The tibial component rotation was referenced relative to the point on the tibial tuberosity between the middle and medial third.
It is the senior author’s routine practice to revise both the femoral and tibial components in most revision TKA cases, and this was true in the study group in all but four cases. Furthermore, both components were malrotated in 24 (47 %) patients.
The Australian Joint Registry data at ten years suggests that the revision rate for primary knee arthroplasty is about 5 % [1]. After aseptic loosening and infection, the third most common cause for revision is pain (10 %) and the forth is patellofemoral pain (10 %). This data suggests that a significant group of patients (20 %) are undergoing revision TKA for “ill defined” pain. A portion of this group is very likely patients with component malrotation. There is a growing body of evidence behind malrotation [13]. From a biomechanical standpoint, a computational simulation study has shown that femoral component internal rotation adversely affects quadriceps strength, collateral ligament forces and varus/valgus kinematics. Tibial malrotation had greater effect on anteroposterior translations [14]. A second simulation has shown that a rotating platform tibial component has the ability to decrease the patello-femoral shear forces induced by femoral component internal rotation in flexion [15]. A third biomechanical study has shown that increased femoral component internal rotation increased patellar height and patellofemoral forces leading to increased patellar wear which could have implications for early loosening [16]. A clinical study focused on 14 patients with femoral component internal rotation showed improved functional outcome after revision of both components [9]. This study concurs with previous clinical retrospective studies regarding benefits of revision TKA for component malrotation [4, 6, 7].
Unique aspects of our study are the large number of patients in the case and control groups which powers it to suggest that revision surgery for component malrotation is as beneficial as revision for aseptic loosening. A better understanding is still lacking with regard to which malrotation factors are pain generators and which tend to limit range of motion.
Acknowledgments
We would like to acknowledge the help of Leslie Stover who assisted in patient evaluation of functional outcome and Mathew MacDonald who assisted in collection of data.
References
- 1.Anonymous (2011) Australian Orthopaedic Association National Joint Replacement Registry Annual Report for 2011. Australian Orthopaedic Association, Sydney
- 2.Mortazavi SM, Molligan J, Austin MS, Purtill JJ, Hozack WJ, Parvizi J. Failure following revision total knee arthroplasty: infection is the major cause. Int Orthop. 2011;35:1157–1164. doi: 10.1007/s00264-010-1134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Eckhoff DG, Metzger RG, Vandewalle MV. Malrotation associated with implant alignment technique in total knee arthroplasty. Clin Orthop Relat Res. 1995;321:28–31. [PubMed] [Google Scholar]
- 6.Hofmann S, Romero J, Roth-Schiffl E, Albrecht T. Rotational malalignment of the components may cause chronic pain or early failure in total knee arthroplasty. Orthopade. 2003;32:469–476. doi: 10.1007/s00132-003-0503-5. [DOI] [PubMed] [Google Scholar]
- 7.Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD. Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res. 2007;458:131–136. doi: 10.1097/BLO.0b013e3180332d97. [DOI] [PubMed] [Google Scholar]
- 8.Lakstein D, Zarrabian M, Kosashvili Y, Safir O, Gross AE, Backstein D. Revision total knee arthroplasty for component malrotation is highly beneficial: a case control study. J Arthroplast. 2010;25:1047–1052. doi: 10.1016/j.arth.2009.07.004. [DOI] [Google Scholar]
- 9.Pietsch M, Hofmann S (2012) Early revision for isolated internal malrotation of the femoral component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(6):1057–1063. doi:10.1007/s00167-011-1637-3 [DOI] [PubMed]
- 10.Keating EM, Meding JB, Faris PM, Ritter MA. Long-term followup of nonmodular total knee replacements. Clin Orthop Relat Res. 2002;404:34–39. doi: 10.1097/00003086-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Jazrawi LM, Birdzell L, Kummer FJ, Cesare PE. The accuracy of computed tomography for determining femoral and tibial total knee arthroplasty component rotation. J Arthroplast. 2000;15:761–766. doi: 10.1054/arth.2000.8193. [DOI] [PubMed] [Google Scholar]
- 12.Linden-van der Zwaag HM, Bos J, Heide HJ, Nelissen RG. A computed tomography based study on rotational alignment accuracy of the femoral component in total knee arthroplasty using computer-assisted orthopaedic surgery. Int Orthop. 2011;35:845–850. doi: 10.1007/s00264-010-1082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rienmuller A, Guggi T, Gruber G, Preiss S, Drobny T (2012) The effect of femoral component rotation on the five-year outcome of cemented mobile bearing total knee arthroplasty. Int Orthop. doi:10.1007/s00264-012-1628-0 [DOI] [PMC free article] [PubMed]
- 14.Thompson JA, Hast MW, Granger JF, Piazza SJ, Siston RA. Biomechanical effects of total knee arthroplasty component malrotation: a computational simulation. J Orthop Res. 2011;29:969–975. doi: 10.1002/jor.21344. [DOI] [PubMed] [Google Scholar]
- 15.Colwell CW, Jr, Chen PC, D’Lima D. Extensor malalignment arising from femoral component malrotation in knee arthroplasty: effect of rotating-bearing. Clin Biomech (Bristol, Avon) 2011;26:52–57. doi: 10.1016/j.clinbiomech.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 16.Vanbiervliet J, Bellemans J, Verlinden C, Vandenneucker H, Luyckx JP, Labey L, Innocenti B. The influence of malrotation and femoral component material on patellofemoral wear during gait. J Bone Joint Surg Br. 2011;93:1348–1354. doi: 10.1302/0301-620X.93B10.26831. [DOI] [PubMed] [Google Scholar]