Abstract
Purpose
We performed a prospective study to document, by intra-operative manipulation under anaesthesia (MUA) of the pelvic ring, the stability of lateral compression type 1 injuries that were managed in a Level-I Trauma Centre. The documentation of the short-term outcome of the management of these injuries was our secondary aim.
Methods
A total of 63 patients were included in the study. Thirty-five patients (group A) were treated surgically whereas 28 (group B) were managed nonoperatively. Intraoperative rotational instability, evident by more than two centimetres of translation during the manipulation manoeuvre, was combined with a complete sacral fracture in all cases.
Results
A statistically significant difference was present between the length of hospital stay, the time to independent pain-free mobilisation, post-manipulation pain levels and opioid requirements between the two groups, with group A demonstrating significantly decreased values in all these four variables (p < 0.05). There was also a significant difference between the pre- and 72-hour post-manipulation visual analogue scale and analgesic requirements of the group A patients, whereas the patients in group B did not demonstrate such a difference.
Conclusion
LC-1 injuries with a complete posterior sacral injury are inheritably rotationally unstable and patients presenting with these fracture patterns definitely gain benefit from surgical stabilisation.
Introduction
Lateral compression type I (LC-1) injuries of the pelvic ring represent the most common type of pelvic ring disruptions. The mortality rate associated with LC-1 injuries has been reported to range from 5.1 % [1] to 8.6 % [2]. Their relationship to injury of intra-pelvic structures is also well known [3].
The prevalence of LC-1 pelvic fractures has been reported to be as high as 63 % of all pelvic ring injuries [2]. Most of these injuries are deemed benign and are consequently treated non-operatively. This emanates from the original work from Young and Burgess who proposed that these injuries are stable based on the fact that the main ligaments contributing to pelvic stability remain intact [4]. However, the association of the anterior fracture of the pelvic ring in conjunction with the variability of the posterior lesion remains poorly understood [5].
Recently, the definition of LC-1 injuries was revisited and the spectrum of posterior ring injuries that accompany them was described in detail [6]. According to Lefaivre et al. [6] more than half of these injuries exist in the context of complete disruption and comminution of the sacrum. The need for operative treatment remains unclear [7] and to the best of our knowledge there are no reported series in the current literature describing its effectiveness.
In order to investigate the above queries, we undertook a prospective study in an attempt to document, by intra-operative manipulation under anesthesia (MUA) of the pelvic ring, the stability of LC-1 injuries.
Patients and methods
Institutional Review Board approval was obtained for this study. All patients who were admitted to our institution and fulfilled the following criteria were included in the study: (a) Young and Burgess lateral compression type-1 pelvic injury (OTA 61-B1), (b) no other major lower extremity or spine injury, (c) independent ambulation prior to injury, (d) adult patient 18–65 years of age, (e) no pathological fracture, and (f) no neurological deficit at presentation.
All patients were initially managed as per ATLS protocol. Imaging evaluation included anteroposterior (AP), inlet and outlet plain radiographs as well as 3-mm computerised tomographic (CT) scans of the pelvis.
Stress examination with MUA of the pelvic ring with fluoroscopy was undertaken under general anesthesia according to the following protocol. The patient was placed on the operating table (OSI, Inc., Union City, CA) in the supine position. In order to correct the magnification error, a known diameter radiopaque ruler was placed on the skin over the pubic symphysis. Under fluoroscopy, internal rotation of the lower extremities along with lateral compression at the level of anterior superior iliac spine (ASIS) was applied. One assistant was internally rotating the lower extremities (manipulating the extremity at the level of the tibial tubercle) whilst the senior author (P.G.) was applying rotational force on the axial plane of the pelvis, at the level of the ASIS. The technique of one surgeon applying force to both ASIS was selected (as opposed to two surgeons applying force to each ASIS) in order to more accurately quantify and control the amount of the force applied. Multiple sequential fluoroscopic AP, inlet and outlet views with the aid of a C-arm were then performed. All the injuries that displayed axial/rotational instability were also tested for vertical instability by applying cranially and caudally directed forces (push–pull manoeuvre) to the pelvic side that suffered the posterior pelvic injury.
Overlapping of 2 cm of the pubic rami fragments or the symphysis pubis was arbitrarily chosen as the indication for operative treatment. Based on this indication for fixation, two groups of patients were formed. Group A consisted of patients treated operatively and group B included the non-operatively treated patients. In group A, the anterior pelvic ring stabilisation consisted of one or a combination of the following: (a) Anterior Superior Iliac Spine (ASIS) external fixator, (b) pubic plating, (c) antegrade superior pubic ramus screw, and (d) retrograde superior pubic ramus screw. The method of anterior pelvic fixation was based upon the configuration of the fracture and the anatomy of the superior pubic ramus. For the posterior pelvic fixation either one or two percutaneous iliosacral screws were inserted to S1 or S2 bodies respectively.
A review of the imaging studies (plain radiographs and CT scans) allowed us to classify all the injuries according to Nakatani [8] and Denis [9] systems. The sacral fracture was characterised as complete when there was a disruption of both the anterior and posterior cortices, at the S1 level on the axial CT scan. Moreover, fractures extending vertically from S1 to S4 level, as this was evident from the coronal sacral views, were classified as complete. Two of the authors (T.T. and N.K.) classified the posterior pelvic injuries and any disagreements were resolved by consensus.
The post-manipulation protocol was the same in both groups. The patients were placed in regular hospital beds and allowed activity (including ambulation) as tolerated by pain, within 48 hours post-manipulation/fixation. Full weight bearing on the intact side and touch-down weight bearing on the injured side was allowed. A walker or crutches were used for mobilisation. Analgesia included the prescription of regular paracetamol, codeine phosphate, and opioids as needed. Low molecular weight heparin (Tinzaparin 4,500 IU) was administered for thomboprophylaxis for a period of six weeks.
For each patient the following data were collected: patient’s demographics, imaging details of the pelvic injury, pre and post-manipulation (at 72 hours) visual analogue scale (VAS) for pain, the amount of opioids intake, method of stabilisation, time to independent pain-free mobilisation, and length of hospital stay.
Following discharge from the hospital all patients were followed up routinely in the outpatient trauma clinic at four, eight, and 12 weeks and at six, 12, and 24 months.
The SPSS for Windows version 19.0 K (SPSS, Chicago, IL) was used for the analysis. Comparisons of age and the perioperative parameters (hospital stay, ambulation, pre and post manipulation VAS and pain requirements) in between the two groups were performed using the Mann–Whitney U test. Sex distribution between groups was tested using the chi-square Fisher’s exact test. The pre and postoperative VAS in each group was tested with the paired t-test. Values of p < 0.05 were considered statistically significant.
Results
Between January 2007 and January 2011, a total of 210 patients with pelvic ring injuries were admitted to our institution. Sixty-three (30 %) of them met the inclusion criteria. Group A consisted of 35 patients that were treated surgically following MUA whereas group B consisted of the remaining 28 patients that were treated non-operatively. Patient demographic data and the characteristics of their fracture patterns are presented in Table 1.
Table 1.
Patient demographic data and details regarding the fracture classification and the implemented treatment
| Demographic | Group A | Group B | p value |
|---|---|---|---|
| Number of patients | 35 | 28 | |
| Gender | Males: 13 | Males: 17 | 0.08 |
| Females: 22 | Females: 11 | ||
| Median age at the time of surgery | 31.4 years; range (18–57) | 37.6 years; range (18–65) | 0.12 |
| Nakatani classification | Type-1: 7 | Type-1: 16 | |
| Type-2: 17 | Type-2: 8 | ||
| Type-3: 11 | Type-3: 4 | ||
| Denis classification | Type-1: 18 | Type-1: 28 | |
| Type-2: 14 | Type-2: 8 | ||
| Type-3: 3 | Type-3: 0 | ||
| Complete/incomplete fracture | 35/0 | 0/28 | |
| Treatment | EXFIX + 1 IS: 16 | Nonoperative | |
| EXFIX + 2 IS: 2 | |||
| EXFIX + RETRO + IS: 1 | |||
| ANTE + IS: 3 | |||
| RETRO + IS: 3 | |||
| ORIF + IS: 10 |
Group A operative group, Group B nonoperative group, EXFIX external fixator, IS Iliosacral screw, ANTE antegrade screw, RETRO retrogarde screw, ORIF open reduction internal fixation
In the surgical group, all of the patients suffered a complete sacral fracture. Of note is the fact that none of these patients demonstrated vertical instability during the MUA. The most commonly observed sacrum fracture in this group was a Dennis type-1 fracture. According to Nakatani classification, the majority of the patients suffered a type-2 (within the obturator foramen) fracture. The demographics of the patients and the operations that they had are shown on Table 1. Sixteen patients of this group underwent stabilisation with an anterior external fixator (EX-FIX) and one iliosacral screw whereas two patients had double (S1 and S2 level) iliosacral screws placed because of the extent and the amount of comminution of their sacral fracture. The iliosacral screw was combined with open reduction and internal fixation (plating) of the anterior ring lesion in ten patients. Three patients had an iliosacral screw combined with an antegrade superior pubic ramus screw whereas another three had a retrograde superior pubic ramus screw. One patient had an EX-FIX combined with a retrograde superior pubic ramus screw and an iliosacral screw (Figs. 1, 2, and 3).
Fig. 1.

A preoperative CT scan image of a LC-1 fracture showing the configuration of the sacrum fracture. It is clear that the fracture is extending from the anterior to the posterior cortex
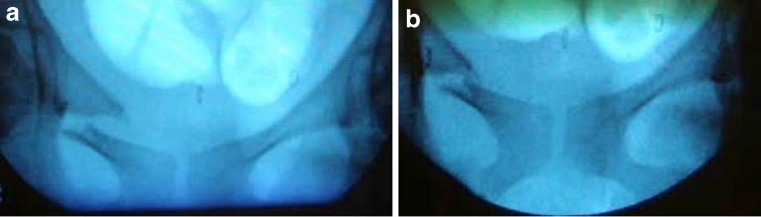
Fig. 2.
Intraoperative radiograph showing the amount of displacement during the manipulation. a Without stress application. b With stress applied
Fig. 3.
a Early postoperative anteroposterior radiograph of the pelvis showing the reduction and fixation with an EXFIX, retropubic and iliosacral screw. b Anteroposterior radiograph of the pelvis two years postoperatively
In group B, 16 patients suffered a type-1, eight a type-2 and four a type-3 Nakatani fracture. Twenty fractures classified as Denis type-1 and eight as type-2. There was no Denis type-3 injury in group B (Table 1).
No statistically significant differences were noted in groups A and B in terms of age, sex distribution and preoperative VAS. There was a statistically significant difference between the length of hospital stay, the time to independent pain-free mobilisation and post-manipulation pain level between the two groups, with group A demonstrating significantly decreased values in all these three variables (Table 2). There was also a significant difference between the pre- and 72-hours post-manipulation VAS and opioids intake of the group A patients, whereas the patients in group B did not demonstrate such a difference (Table 2).
Table 2.
Comparison of perioperative parameters between group A and group B
| Parameter | Group A | Group B | p-value |
|---|---|---|---|
| Duration of hospital stay (days) | 5 (3–7) | 9 (8–16) | p < 0.01 |
| Time to pain free mobilisation (days) | 2 (1–5) | 7 (6–13) | p < 0.01 |
| Pre-manipulation VAS | 9 (7–10) | 9 (7–10) | p = 0.52 |
| Post-manipulation VAS at 72 h | 4 (2–6) | 9 (7–10) | p < 0.01 |
| Pre-versus post-72 h VAS | p < 0.01 | p = 0.16 | |
| Pre-manipulation opioid intake (times per day) | 4 (3–4) | 3 (3–4) | p = 0.41 |
| Post-manipulation opioid intake (times per day) at 72 h | 1 (0–2) | 3 (2–3) | p < 0.03 |
| Pre-versus post 72 h opioids intake | p < 0.01 | p = 0.18 |
Data shown are median values with range in parentheses for each parameter
p < 0.05 is considered statistically significant
VAS visual analogue scale (out of 10, with 10 being the worst)
Discussion
LC type-1 injuries of the pelvic ring have been the subject of heated discussion amongst orthopaedic trauma surgeons [2, 6–8, 10–12]. The traditional dogma related to these injuries suggests their inherent stability because the amount of the pelvic displacement is minimal, the posterior elements of the pelvic ring remain relatively intact and consequently there is rarely a need for operative intervention [1, 13–17]. On the other hand, it has been pointed out that not all of these fractures are inherently stable and displacement can occur when non-operative treatment is instituted [18]. Furthermore, and in line with other studies in the recent literature supporting surgical treatment of pelvic injuries previously thought benign [19], the surgical fixation of a specific subpopulation of patients with LC-1 injuries has been suggested [1, 9, 10, 20, 21]. Other authors support that immediate weight-bearing, for minimally displaced LC sacral fractures is safe and results in union with minimal additional displacement [22].
Our observation that patients with LC-1 pelvic fractures do not represent a homogenous population, as nursing care, mobilisation and pain management differs substantially amongst them, led us to believe that not all lesions are the same and the degree of the mechanical stability of the fracture might have an impact on patient symptomatology. In order to delineate further the above concerns we decided to undertake this study.
The heterogeneity and complexity of LC injuries has recently been evaluated with a quantitative 3D CT analysis, which revealed that the classical LC fracture classification yields a nonhomogenous group of fractures [5]. In addition, the radiographic and CT review of 100 LC-1 injury cases showed that sacral comminution and complete sacral disruption was present in half of the cases [6].
The MUA has recently been introduced and is currently being evaluated as a tool to estimate the severity of the injury and to guide treatment both in LC and APC injuries [7, 23, 24]. Gardner et al. [25] demonstrated that the amount of the displacement seen on the static plain radiographs and CT scan of the pelvis after LC injuries is substantially less than the original deformity at the time of injury due to passive recoil of tissues. The authors pointed out that the initial injury should not be underestimated based on the initial radiographs and CT scans. Furthermore, Sagi et al. [7] proposed a modification of the Young and Burgess classification system for LC-1 injuries, into LC-1a (not requiring surgical treatment) and LC-1b (may require surgical treatment), based on the amount of displacement during MUA which showed that almost 40 % of LC-1 injuries are inherently unstable. The MUA was also used in a recent study to test the stability and guide the treatment of Tile Type-B fractures of the pelvis [26].
Despite the above data, there is still a debate as to whether there is a clear indication for surgical intervention. The real essence of the discussion is whether surgical intervention represents a potential benefit to the patient. To the best of our knowledge, we are the first group to examine patients with LC-1 injuries under general anesthesia and to implement a surgical treatment in the injuries that exhibited gross displacement/instability during the manipulation manoeuvre. We consequently followed the patients during their hospitalisation and documented the short-term outcome of the surgical intervention.
In our series all patients that exhibited more than two centimetres of displacement of the anterior pelvis during manipulation had a complete disruption of the posterior pelvic ring. Consequently, a posterior stabilisation of the pelvis with an iliosacral screw was implemented to every patient in group A. The fact that none of the surgically-treated fractures exhibited vertical displacement during the manipulation concurs with the assumption that the pelvic ligaments remain intact. Our results show that the patients from the surgically treated group had statistically significant lower VAS and need for opioids intake 72 hours post-manipulation, shorter hospital stay and less time to relatively pain-free ambulation compared to non-surgically treated patients. The surgically treated patients also demonstrated significant differences between the pre- and postoperative pain levels and analgesia requirements whereas in the non-surgically treated group there was no significant difference in the above parameters. These findings support the view that surgical intervention provides significant pain relief and raises the question whether even stable fracture patterns should be considered for fixation to better control painful stimuli and to allow early ambulation.
This is one of the few studies in the current literature that sheds light on the early outcome of the surgical treatment of LC-1 injuries after dynamic testing of their stability. Bellabarba et al. [20] also reported on OTA type 61-B2 injuries treated with supra-acetabular external fixation. In our trial, we comment upon the short-term outcome of the surgical treatment, as our primary intention was to clearly define the characteristics of the patient population that exhibited displacement during the manipulation process and had undergone surgical stabilisation.
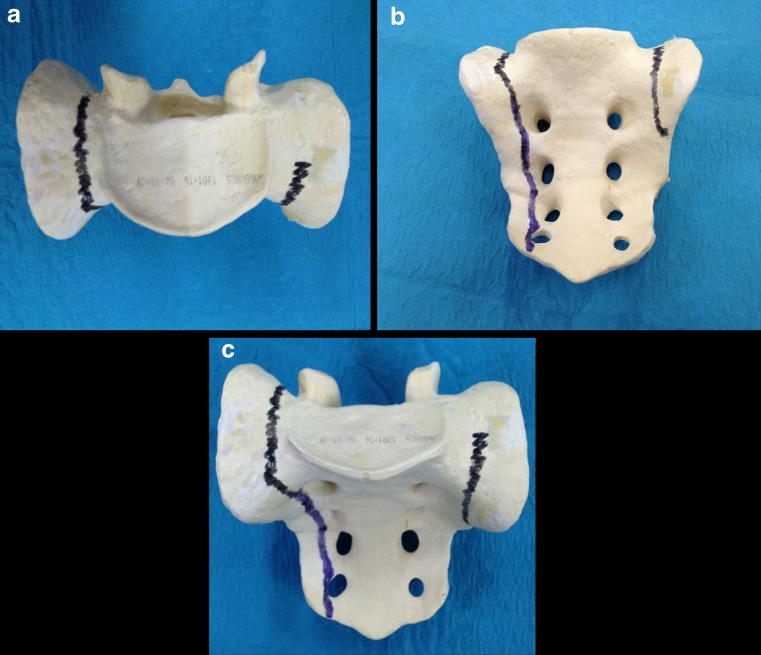
The findings of the CT scan of all the unstable pelvises provided evidence of a complete sacral fracture in both the axial and the frontal plane (Fig. 4). Based on these findings we recommend that when such a fracture pattern is noted on the CT scan, an operative intervention should be offered to the patient.
Fig. 4.
a Inlet. b Outlet. c True anterior-posterior view of the sacrum illustrating complete fracture on the right and incomplete fracture on the left
The results of our study show that MUA is a useful tool in the hands of experienced orthopaedic trauma surgeons in evaluating LC-1 pelvic injuries. We recognise though that our study has some limitations. First, we did not compare the surgical versus the non-surgical treatment of “unstable” LC-1 fractures, which might have been the optimal set-up to study these injuries. Second, we are also aware that the cut-off limit of 2 cm of displacement to discriminate between stable and unstable was arbitrarily chosen. This cut-off though, has also been used in a recent study to define significant displacement [7]. Third, we do not report on the long-term outcome as our intention was to identify which type of lesions were associated with the greatest degree of movement (instability) under examination and would benefit from surgical intervention. Strengths of this study however are its prospective nature, the use of stress fluoroscopic examination of the pelvis under general anesthesia to investigate the presence or absence of instability, the same surgeon carrying out all the procedures and the subsequent correlation of the manipulation findings with the fracture pattern on the CT scans.
In conclusion, the results of this study suggest that the subpopulation of LC-1 injuries with a complete posterior sacral injury is inherently rotationally unstable and patients presenting with these fracture patterns would definitely benefit from surgical stabilisation. Operative intervention in this group of patients is associated with a shorter length of hospital stay and significantly reduced pain and analgesic requirements during the immediate post-injury period.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. No funds were received in support of this study.
References
- 1.Burgess AR, Eastridge BJ, Young JW, Ellison TS, Ellison PS, Jr, Poka A, Bathon GH, Brumback RJ. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990;30(7):848–856. doi: 10.1097/00005373-199007000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Manson T, O’Toole RV, Whitney A, Duggan B, Sciadini M, Nascone J. Young-Burgess classification of pelvic ring fractures: does it predict mortality, transfusion requirements, and non-orthopaedic injuries? J Orthop Trauma. 2010;24(10):603–609. doi: 10.1097/BOT.0b013e3181d3cb6b. [DOI] [PubMed] [Google Scholar]
- 3.Mundy AR, Andrich DE. Pelvic fracture-related injuries of the bladder neck and prostate: their nature, cause and management. BJU Int. 2010;105(9):1302–1308. doi: 10.1111/j.1464-410X.2009.08970.x. [DOI] [PubMed] [Google Scholar]
- 4.Young JW, Burgess AR, Brumback RJ, Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986;160(2):445–451. doi: 10.1148/radiology.160.2.3726125. [DOI] [PubMed] [Google Scholar]
- 5.Khoury A, Kreder H, Skrinskas T, Hardisty M, Tile M, Whyne CM. Lateral compression fracture of the pelvis represents a heterogeneous group of complex 3D patterns of displacement. Injury. 2008;39(8):893–902. doi: 10.1016/j.injury.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 6.Lefaivre KA, Padalecki JR, Starr AJ. What constitutes a Young and Burgess lateral compression-I (OTA 61-B2) pelvic ring disruption? A description of computed tomography-based fracture anatomy and associated injuries. J Orthop Trauma. 2009;23(1):16–21. doi: 10.1097/BOT.0b013e31818f8a81. [DOI] [PubMed] [Google Scholar]
- 7.Sagi HC, Coniglione FM, Stanford JH. Examination under anesthetic for occult pelvic ring instability. J Orthop Trauma. 2011;25(9):529–536. doi: 10.1097/BOT.0b013e31822b02ae. [DOI] [PubMed] [Google Scholar]
- 8.Starr AJ, Nakatani T, Reinert CM, Cederberg K. Superior pubic ramus fractures fixed with percutaneous screws: what predicts fixation failure? J Orthop Trauma. 2008;22(2):81–87. doi: 10.1097/BOT.0b013e318162ab6e. [DOI] [PubMed] [Google Scholar]
- 9.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67–81. [PubMed] [Google Scholar]
- 10.Manson TT, Nascone JW, Sciadini MF, O’Toole RV. Does fracture pattern predict death with lateral compression type 1 pelvic fractures? J Trauma. 2010;69(4):876–879. doi: 10.1097/TA.0b013e3181e785bf. [DOI] [PubMed] [Google Scholar]
- 11.Lau TW, Leung F. Occult posterior pelvic ring fractures in elderly patients with osteoporotic pubic rami fractures. J Orthop Surg (Hong Kong) 2010;18(2):153–157. doi: 10.1177/230949901001800205. [DOI] [PubMed] [Google Scholar]
- 12.Kanakaris N, Tzioupis C, Nikolaou V, Giannoudis P. Lateral compression type I injuries of the pelvic ring: are they mechanically stable? Inj Extra. 2009;40:183–235. doi: 10.1016/j.injury.2009.06.171. [DOI] [Google Scholar]
- 13.Gordon RO, Mears DC. Lateral compression injury of the pelvis. A case report. J Bone Joint Surg Am. 1991;73(9):1399–1401. [PubMed] [Google Scholar]
- 14.Routt ML, Jr, Simonian PT, Ballmer F. A rational approach to pelvic trauma. Resuscitation and early definitive stabilization. Clin Orthop Relat Res. 1995;318:61–74. [PubMed] [Google Scholar]
- 15.Tile M. Pelvic fractures: operative versus nonoperative treatment. Orthop Clin N Am. 1980;11(3):423–464. [PubMed] [Google Scholar]
- 16.Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988;70(1):1–12. doi: 10.1302/0301-620X.70B1.3276697. [DOI] [PubMed] [Google Scholar]
- 17.Miranda MA, Riemer BL, Butterfield SL, Burke CJ., 3rd Pelvic ring injuries. A long term functional outcome study. Clin Orthop Relat Res. 1996;329:152–159. doi: 10.1097/00003086-199608000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Bruce B, Reilly M, Sims S. OTA highlight paper predicting future displacement of nonoperatively managed lateral compression sacral fractures: can it be done? J Orthop Trauma. 2011;25(9):523–527. doi: 10.1097/BOT.0b013e3181f8be33. [DOI] [PubMed] [Google Scholar]
- 19.Mehling I, Hessmann MH, Rommens PM. Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Operative technique and outcome. Injury. 2012;43(4):446–451. doi: 10.1016/j.injury.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Bellabarba C, Ricci WM, Bolhofner BR. Distraction external fixation in lateral compression pelvic fractures. J Orthop Trauma. 2000;14(7):475–482. doi: 10.1097/00005131-200009000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Osterhoff G, Ossendorf C, Wanner GA, Simmen HP, Werner CM. Posterior screw fixation in rotationally unstable pelvic ring injuries. Injury. 2011;42(10):992–996. doi: 10.1016/j.injury.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 22.Sembler Soles GL, Lien J, Tornetta P 3rd (2012) Nonoperative immediate weightbearing of minimally displaced lateral compression sacral fractures does not result in displacement. J Orthop Trauma 26(10):563–567. doi:10.1097/BOT.0b013e318251217b [DOI] [PubMed]
- 23.Gardner MJ, Parada S, Chip Routt ML., Jr Internal rotation and taping of the lower extremities for closed pelvic reduction. J Orthop Trauma. 2009;23(5):361–364. doi: 10.1097/BOT.0b013e31819c4a3f. [DOI] [PubMed] [Google Scholar]
- 24.Suzuki T, Morgan SJ, Smith WR, Stahel PF, Flierl MA, Hak DJ. Stress radiograph to detect true extent of symphyseal disruption in presumed anteroposterior compression type I pelvic injuries. J Trauma. 2010;69(4):880–885. doi: 10.1097/TA.0b013e3181efbad5. [DOI] [PubMed] [Google Scholar]
- 25.Gardner MJ, Krieg JC, Simpson TS, Bottlang M. Displacement after simulated pelvic ring injuries: a cadaveric model of recoil. J Trauma. 2010;68(1):159–165. doi: 10.1097/TA.0b013e31819adae2. [DOI] [PubMed] [Google Scholar]
- 26.Hoffmann MF, Jones CB, Sietsema DL (2012) Persistent impairment after surgically treated lateral compression pelvic injury. Clin Orthop Relat Res 470(8):2161–2172. doi:10.1007/s11999-012-2247-1 [DOI] [PMC free article] [PubMed]