Abstract
Purpose
The purpose of this paper is to review our experience and study the feasibility and clinical results of one-stage total knee arthroplasty (TKA) for patients with osteoarthritis of the knee with extra-articular deformity.
Methods
Nine patients with osteoarthritis of the knee associated with extra-articular deformity underwent one-stage TKA from June 2006 to April 2010. There were two men and seven women, with an average age of 51 years (range 34–69 years); four of them had tibial deformities and five had femoral deformities. Eight of the cases resulted from malunion after fracture healing and one from femoral recurvatum. Six of the cases had uniplanar and three had biplanar deformities. The average angles of the femoral deformities were 13.3° in the coronal plane (8–22) and 11.3° in the sagittal plane (6–15); one femur had 10° external rotational deformity. Tibial deformity of 16° in the coronal plane (11–22) was noted, and one had sagittal plane deformity of 21°.
Results
All patients were followed for an average of 29 months. The average Hospital for Special Surgery (HSS) knee score improved from 18.7 points pre-operatively to 89.8 points at the time of last follow-up; the range of knee motion improved from 46.7° preoperatively to 100.6° postoperatively. The average angle of mechanical axis deviation was restored from 11.8° preoperatively to 1° postoperatively. One of the patients had unsatisfactory clinical results due to delayed union at the osteotomy site. No complications such as infection, deep vein thrombosis, ligament instability, low level or subluxed/dislocated patella or component loosening were observed. One-stage TKA with intra-articular correction of the extra-articular deformity was performed in seven patients, included proper planning, appropriate bone cuts to restore alignment and the necessary soft tissue releases to balance the knee in flexion and extension. Two patients underwent simultaneous extra-articular correctional osteotomy and TKA because the deformity was so large. Five knees that had good collateral ligamentous stability and balance received a posterior stabilised prosthesis; four knees that had ligamentous instability received a constrained condylar knee (CCK) prosthesis.
Conclusions
One-stage TKA is a technically difficult but effective treatment for patients with osteoarthritis of the knee and extra-articular deformity. If feasible we recommend TKA with intra-articular bone resection and soft tissue balancing.
Introduction
Our hospital is located in an urban area which provides tertiary care to all patients, mostly from distant rural areas of the province. We did this research in our department, as all of the patients were operated on by a single surgeon. There were nine patients (seven women and two men) aged 34–69 years (mean 51 years) who were treated at our hospital from June 2006 to April 2010. Five of them had femoral deformities, and four had tibial deformities. One of the cases was due to femoral dysplasia and the remaining four were due to fracture malunion. The length of time between fracture and total knee arthroplasty (TKA) ranged from 17 to 197 months. All of the cases were associated with advanced osteoarthritis. One of the cases was associated with ipsilateral muscular atrophy and fibrous ankylosis. Two had knee ligament injury, and two had fibrous healing of the femoral condyle. There were coronal, sagittal or axial plane deformities involved in one of the six cases. Three of the cases involved biplanar deformities.
There was coronal plane deformity of 8–22° (average 13.3) in four cases, sagittal plane deformity of 6–15° in three cases (average 11.3) and one of the cases was associated with external rotational deformity of 10° on clinical examination. There were three cases with coronal plane deformity of 11–22° (average 16). There were three cases with tibial coronal plane deformity of 11–22° (average 16) and one case with tibial sagittal plane deformity of 21° (Table 1).
Table 1.
Data on the extra-articular deformity and treatment
| Case | Gender | Age | Preop. diagnosis | Deformity | Type of surgery | Type of implant | ||
|---|---|---|---|---|---|---|---|---|
| Site | Plane | Degrees | ||||||
| 1 | F | 64 | Fracture malunion | Proximal 1/3 tibia | Coronal | Valgus 15 | TKA (intra-articular bone resection) | PS |
| 2 | M | 45 | Fracture maluniona | Tibial metaphysis | Coronal | Varus 22 | TKA (extra-articular correctional osteotomy) | CCK |
| 3 | F | 38 | Fracture malunion | Distal 1/3 femur | Coronal | Varus 9 | TKA (intra-articular bone resection) | PS |
| Sagittal | Retrocurvatum 15 | |||||||
| 4 | F | 34 | Congenital dysplasia | Tibial metaphysis | Sagittal | Retrocurvatum 21 | TKA (extra-articular correctional osteotomy) | PS |
| 5 | F | 37 | Fracture malunionb | Femoral condyle | Coronal | Varus 8 | TKA (intra-articular bone resection) | CCK |
| Sagittal | Retrocurvatum 6 | |||||||
| 6 | M | 62 | Fracture malunionb | Femoral condyle | Coronal | Varus 14 | TKA (intra-articular bone resection) | CCK |
| 7 | F | 53 | Fracture maluniona | Femoral condyle | Coronal | Varus 22 | TKA (intra-articular bone resection) | CCK |
| Sagittal | Antecurvatum 13 | |||||||
| 8 | F | 60 | Fracture malunion | Femoral condyle | Axial | Extorsion 10 | TKA (intra-articular bone resection) | PS |
| 9 | F | 69 | Fracture malunion | Tibial metaphysis | Coronal | Varus 11 | TKA (intra-articular bone resection) | PS |
F female, M male, CCK constrained condylar knee, PS posterior stabilised
aComplicated by injury of knee collateral ligaments
bComplicated by fibrous healing of the femoral condyle
Pre-operative preparation and assessments
Weight-bearing full-length X-rays (anteroposterior view) were taken mainly focusing on the tibia and femur in the neutral position to determine the degree of deformity. These are helpful in determining the limb malformation and anatomical axis malalignments. The most important purpose is to give us an idea of the level of the osteotomy to be performed during the surgery.
Femoral articular deformity due to the result of displacement of the femoral condyles from the knee centre should be considered as the osteotomy level. If the osteotomy line is likely to involve the position of the ligaments, a soft tissue balancing technique with compensatory intra-articular osteotomy should be considered. In order to measure the degree of deformity on the tibial side, X-ray films should be taken and assessed by drawing a straight line (sagittal plane) to measure the angle of deformity; if it involves the tibial plateau then a soft tissue balancing technique should be used to correct the extra-articular deformity [1]. If the thickness of the osteotomy is more than 15 mm, it cannot be guaranteed that the articular surface can be safely stabilised.
Operating technique
Generally the mid-patellar longitudinal incision is preferred along with the medial patellar side approach but in patients who had previous knee surgery, the original incision site should be preferred to avoid skin necrosis.
We had four patients with intramedullary positioning and one with extramedullary positioning. Extramedullary positions should be checked repeatedly for limb alignment. In one case with sagittal plane deformity, we used C-arm fluoroscopy to determine the position of the prosthesis implanted, starting with low thickening osteotomy which must be safe enough to stabilise the prosthesis.
Caution should be taken to avoid injury to the ligaments. Flexion gap should be checked as straightening the leg determines the size of the gap.
The type of prosthesis selected for our cases were generally posterior stabilised (PS), but patients with ligamentous injuries and fibrosis of the lateral femoral condyle were considered unstable and a condylar prosthesis was chosen (constrained condylar knee, CCK). Five of the cases were selected to receive a PS type (Innex 2, P.F.C. Sigma, DePuy Inc.; NexGen 2, Zimmer Inc.), and four of them were selected to receive a CCK (LCCK, Zimmer Inc.).
The decision about the level of osteotomy was made based on C-arm X-ray and intramedullary nail positioning. Lateral osteotomy was done to extend the stem of the prosthesis (case 4).
Results
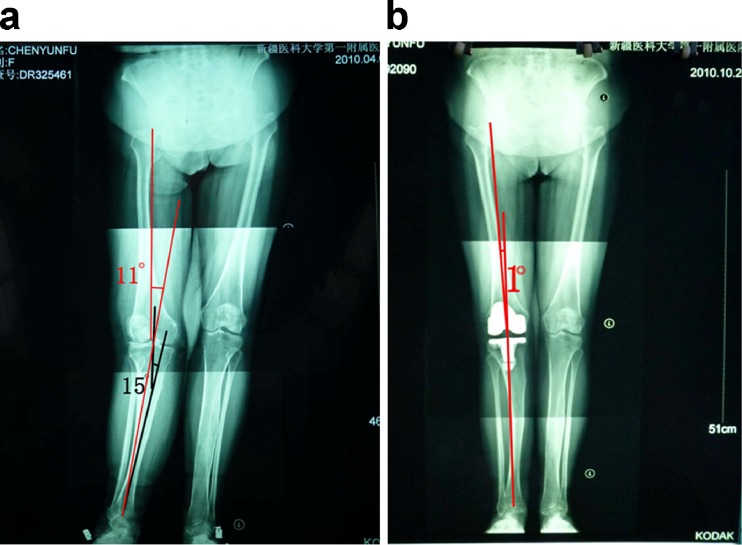
All patients were followed up for seven–54 months, an average of 29 months. The mean preoperative Hospital for Special Surgery (HSS) knee score improved from 18.7 points (6–39 points) and increased to an average final follow-up of 89.8 points (81 ∼ 96 points). The pre-operative knee joint activity of 46.7° (0 ∼ 100°) increased to an average final follow-up of 100.6° (85 ∼ 115°); activity increased to 53.9° in one patient with preoperative stiff knee who had a postoperative range of motion of 85° (case 4). Limb alignments (weight-bearing full-length X-ray measurements, Fig. 1): the average angle of mechanical axis deviation was restored from 11.8° preoperatively (average 2–21) to 1° postoperatively (0–4°). One of the patients had extra-articular deformity with preoperative valgus of 10° but it became varus of 4° postoperatively (case 2). None of the patients were found to have bone fragment or cement between the prosthesis and loosening symptoms. We only had one patient with unsatisfactory clinical results after seven months of follow-up with delayed union at the osteotomy site (case 2). The rest of the cases were without infections, deep vein thrombosis, wound healing problems, knee instability, patellar problems and other complications (Table 2)
Fig. 1.
A 64-year-old woman who had had arthritis with extra-articular deformity. a Preoperative standing full-length radiograph showing 15° valgus deformity caused by malunited proximal tibial fracture, which resulted in a mechanical axis deviation of 11°. b Postoperative radiograph made 6 months after one-stage TKA with intra-articular bone resection and soft tissue balancing, showing restoration of the mechanical axis
Table 2.
Data on the pre-operative and postoperative function
| Case | Motion (°) | Duration of follow-up (months) | Complication | Deviation of postop. mechanical axis | HSS (points) | |||
|---|---|---|---|---|---|---|---|---|
| Preop. | Postop. | Preop. | Postop. | Preop. | Postop. | |||
| 1 | 0–100 | 0–105 | 7 | No | 11 | 1 | 39 | 95 |
| 2 | 15–60 | 0–115 | 7 | Delayed union (osteotomy) | 10 | 4 | 15 | 81 |
| 3 | 10–60 | 5–100 | 54 | No | 15 | 2 | 22 | 92 |
| 4 | 0 | 5–90 | 31 | No | 3 | 0 | 6 | 90 |
| 5 | 20–80 | 0–100 | 41 | No | 12 | 0 | 18 | 90 |
| 6 | 20–45 | 5–95 | 19 | No | 20 | 0 | 13 | 85 |
| 7 | 25–40 | 0–90 | 44 | No | 21 | 0 | 12 | 84 |
| 8 | 0–60 | 0–110 | 26 | No | 2 | 1 | 23 | 96 |
| 9 | 15–80 | 0–105 | 31 | No | 12 | 1 | 20 | 95 |
| Average | 46.7 | 100.6 | 29 | 11.8 | 1.0 | 18.7 | 89.8 | |
HSS Hospital for Special Surgery knee rating score
Discussion
The impact of extra-articular deformities (varus/valgus deformity) in the coronal axis on TKA
The most common intra-articular deformity is caused by bone and cartilage loss of the knee. With appropriate bone cuts and soft tissue releases to balance the knee inflexion and extension, restoration of the mechanical axis of the femur and the tibia and axial planes of rotation can restore alignment, and the direction of bone cuts is not affected by the deformity. No matter how serious the deformity is, it will not change the axis of bone cuts. However, extra-articular deformity is different due to the malformation change in anatomical axis and the alignment. If we want to restore alignment, we cannot only refer to the anatomical axis, but the direction of bone cuts will also be affected by the deformity. This effect is related to the distance to the knee and the angle of deformity. In their in-depth study, Wolff et al. [2] found that bigger malformation angle and nearer distance will have a great effect on TKA.
In order to restore alignment, the direction of intra-articular bone cuts will deviate compensatory to the deformity in the coronal plane and the deviation will be bigger with the bigger malformation angle and nearer distance.
After the direction of intra-articular bone cuts have deviated compensatory in the coronal plane (asymmetrical bone resection), this will cause secondary iatrogenic unsteadiness and ligament instability will increase with the malformation angle. Besides it will become restricted by collateral ligament insertion, and it cannot be corrected perfectly by soft tissue balancing or it will damage the collateral ligaments. At this time we consider using extra-articular correctional osteotomy or choose a stabilised prosthesis.
Combined with data from references [1–6] and from our experience, we believe that when extra-articular deformities are less than 20° in the coronal plane, one-stage TKR with intra-articular correction and soft tissue balancing is feasible and effective. There are two problems to consider: first, the ligament instability caused by intra-articular correction of the femoral deformity is different from the tibial deformity. Femoral deformity cannot affect femoral condyle osteotomy, so after correctional osteotomy it will only have extension unsteadiness but inflexion is stabilised. This is difficult to handle because no matter what type of soft tissue balancing you perform to correct the instability, it will cause inflexion unsteadiness. Tigani et al. [7] suggested computer-assisted TKA in severe cases of extra-articular deformity or retained hardware, but in our experience if proper surgical technique and planning are applied computer assistance is not required.
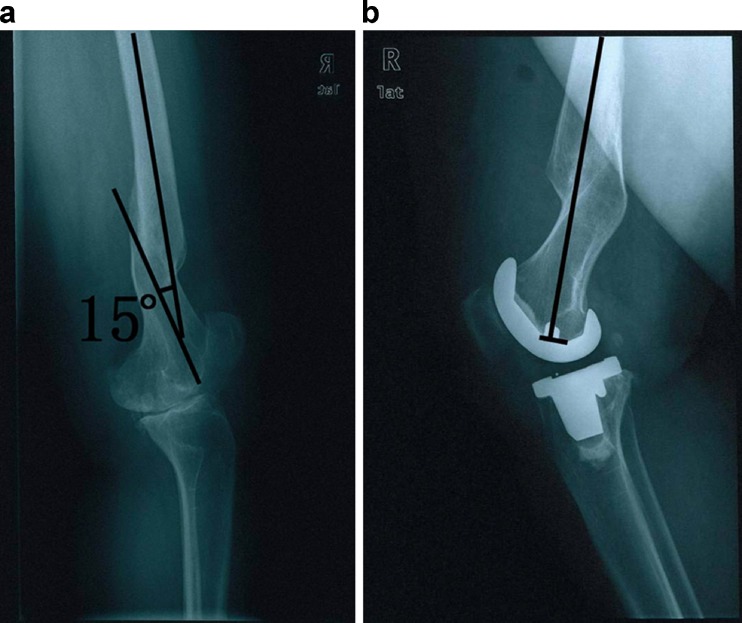
Insall et al. [8] suggested rotating the femoral prosthesis to the unstable side to balance the inflexion gap. But this method only applies to a smaller angle of extra-articular deformities. For tibial deformities, after correctional osteotomy it will have extension and inflexion gap unsteadiness. At this time we can use soft tissue release balancing to achieve stabilisation. The second problem is that tibial deformity affects knee and ankle joint alignment. Intra-articular osteotomy of the proximal tibia only restores knee joint alignment, because osteotomy of the proximal tibia must be perpendicular to knee and ankle joint alignment. Otherwise it would be deflected and the ankle joint will remain misaligned. This phenomenon (Fig. 2) is compensated by varus or valgus of subtalar joint. In the short-term follow-up of four cases in this group, we did not find any abnormal symptoms. But we could not eliminate the possibility of ankle joint osteoarthritis in the long run. If the compensatory angle is too large, then we should use extra-articular correctional osteotomy of the tibia.
Fig. 2.
To recreate the mechanical axis of the lower extremity, the orientation of the proximal tibial bone resection must be perpendicular to the line across the centre of the knee and ankle joint (red line), not to the distal tibial shaft (black line). However, a residual amount of ankle malorientation will still be present because the tibial shaft deformity remains
The impact of extra-articular deformities (inflexion or hyperextension) in the sagittal axis on TKA
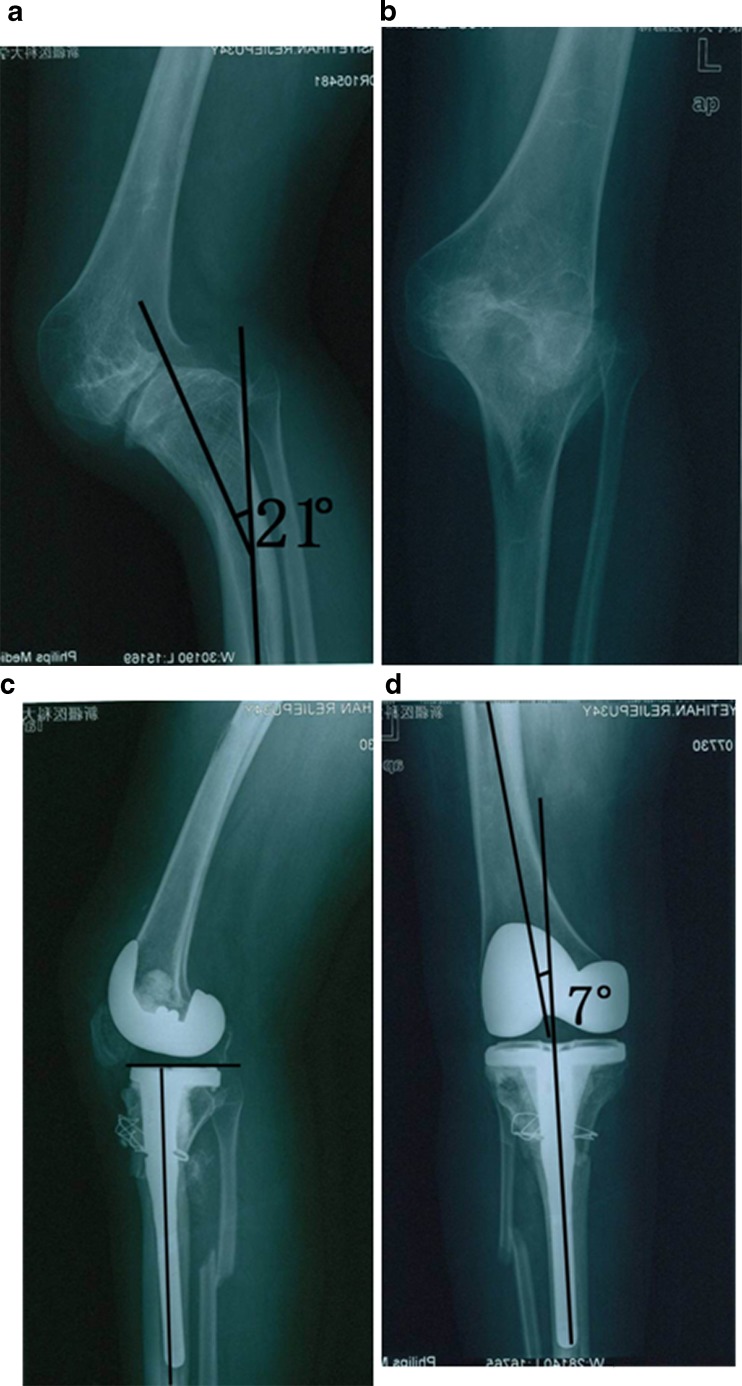
For this kind of deformity, correction on the tibial side is much easier than on the femoral side. If we place the femoral prosthesis in a normal position out of femoral deformity correction, the joint line will not be parallel with the ground, and it will cause hyperextension or change the inflexion alignment. So in the sagittal plane, the femoral prosthesis should be placed in neutral position which is perpendicular to the femoral longitudinal axis (Fig. 3, case 3). In the actual operation, this demands a well-experienced surgeon to achieve this technically, especially when the marrow cavity pole could not pass through the deformity part. In our department, with the guidance of C-arm fluoroscopy we drill a pin from the entry point on the femoral condyle to normal proximal bone marrow cavity, and refer it to bone cuts. We should notice that if the deformity angle is too large, there will be a femoral ventri-cortical notch and damage to the ligamentum patellae insertion when we had forward angulation bone cuts. So we believe that an extra-articular deformity with forward angulation in the sagittal plane is hard to correct. We should do one-stage TKA with extra-articular correctional osteotomy when forward angulation is larger than 10° and backward angulation is larger than 20° in the sagittal plane [3] (Fig. 4, case 4).
Fig. 3.
A 38-year-old woman who had had arthritis with extra-articular deformity. a Preoperative radiograph showing 15° sagittal deformity caused by malunited distal femur fracture. b Postoperative lateral radiograph made 2 years after one-stage TKA with intra-articular bone resection and soft tissue balancing, showing excellent alignment of the femoral component and no radiolucency about the component
Fig. 4.
A 34-year-old woman who had had arthritis with extra-articular deformity. a, b Pre-operative radiographs showing ankylosis and 21° sagittal deformity caused by dysplasia of the left proximal tibia. c, d Postoperative radiographs made 1 month after TKA with simultaneous extra-articular correctional osteotomy, showing restoration of the mechanical axis and excellent alignment of the component
The impact of extra-articular deformities (internal or external rotation) in the axial planes of rotation on TKA
The angle of deformity in the axial planes of rotation is not only hard to calculate exactly, but also hard to restore in TKA. The rotation of the femoral and tibia prosthesis cannot totally refer to the anatomical axis, it must be integrated into the patellofemoral orbit. For example, for femoral external rotation deformity, if we apply a conventional method of rotation alignment with a femoral prosthesis by referring to the anatomical axis, it will cause more external rotation of the femoral prosthesis and imbalance of the inflexion gap. Even the soft tissue release could not achieve the balance. At this time a more effective and convenient method is internal rotation of the femoral prosthesis. But this method also had a problem with the patellofemoral orbit. However, studies [9] have shown that with every 3° of internal or external rotation of the femoral prosthesis, the femoral trochlear fovea will shift 1 mm inward or outward. In this situation, in order to improve the patella orbit, we will perform lateral retinacular release after internal rotation of the femoral prosthesis, shift the femoral prosthesis 1 ∼ 2 mm outward, chose one smaller size of patellar prosthesis and shift it 1 ∼ 2 mm inward. This group had a 60-year-old female patient whose angle of external rotation deformity of the femur was 10° and a satisfactory result was obtained after using this method (case 8). Considering the serious complication, if the angle of rotation deformity is larger than 10°, we suggest performing correctional osteotomy with extra-articular rotation before TKA, especially in young and active patients.
The choice of prosthesis
In TKA with intra-articular correction of the extra-articular deformity due to asymmetrical bone resection it is hard to balance posterior cruciate ligament tension; we believe this can be compensated with soft tissue balancing and a stabilised prosthesis. An extra-articular correctional osteotomy will be applied to get higher stability. Four patients in this group who had collateral knee ligament injury or fibrous healing of the external condyle of the femur chose CCK. Even though one-stage extra-articular correctional osteotomy corrects the malalignment and decreases the difficulty of TKA, it in fact leads to overcorrection, malunion or nonunion and other complications [10, 11]. Our preferred method is bone cuts with the guidance of C-arm fluoroscopy, then use of the positioning system in inner marrow and long-stem prosthesis to the fixation incision area. One patient had overcorrection whose alignment changed from pre-operative 10° varus to postoperative 4° valgus and delayed union of the incision area during the follow-ups (case2).
In summary, one-stage TKA with extra-articular deformity is a complex procedure. However, with proper planning, a satisfactory TKA can be achieved. For patients with osteoarthritis of the knee and an extra-articular deformity, if feasible we recommend TKA with intra-articular bone resection and soft tissue balancing. This method has advantages like a small wound, shorter length of stay in the hospital and also avoids the complications like nonunion, delayed union, the chances of infection, fixation failure and the other complications [1–4, 10–12]
References
- 1.Wang JW, Wang CJ. Total knee arthroplasty for arthritis of the knee with extra-articular deformity. J Bone Joint Surg Am. 2002;84:1769–1774. doi: 10.1302/0301-620X.84B3.11609. [DOI] [PubMed] [Google Scholar]
- 2.Wolff AM, Hungerford DS, Pepe CL. The effect of extraarticular varus and valgus deformity on total knee arthroplasty. Clin Orthop Relat Res. 1991;271:35–51. [PubMed] [Google Scholar]
- 3.Lonner JH, Siliski JM, Lotke PA. Simultaneous femoral osteotomy and total knee arthroplasty for treatment of osteoarthritis associated with severe extra-articular deformity. J Bone Joint Surg Am. 2000;82:342–348. doi: 10.2106/00004623-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Koenig JH, Maheshwari AV, Ranawat AS, Ranawat CS (2009) Extra-articular deformity is always correctable intra-articularly: in the affirmative. Orthopedics 32(9) [DOI] [PubMed]
- 5.Treuter S, Schuh A, Hönle W, et al. Long-term results of total knee arthroplasty following high tibial osteotomy according to Wagner. Int Orthop. 2012;36(4):761–764. doi: 10.1007/s00264-011-1373-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bae DK, Song SJ, Yoon KH. Total knee arthroplasty following closed wedge high tibial osteotomy. Int Orthop. 2010;34(2):283–287. doi: 10.1007/s00264-009-0749-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tigani D, Masetti G, Sabbioni G, et al. Computer-assisted surgery as indication of choice: total knee arthroplasty in case of retained hardware or extra-articular deformity. Int Orthop. 2012;36(7):1379–1385. doi: 10.1007/s00264-011-1476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Insall JN, Ranawat CS, Scott WN, et al. Total condylar knee replacement: preliminary report. Clin Orthop Relat Res. 1976;120:149–154. [PubMed] [Google Scholar]
- 9.Scott RD (2007) Surgery of total knee arthroplasty. Xu WD, Zhang XL, Wang translation: Shanghai: the Second Military Medical University Press 2007:75–83
- 10.Ritter MA, Faris GW. Total knee replacement following extra-articular deformities. Orthopedics. 2003;26(9):969–970. doi: 10.3928/0147-7447-20030901-39. [DOI] [PubMed] [Google Scholar]
- 11.Papagelopoulos PJ, Karachalios T, Themistocleous GS, et al. Total knee arthroplasty in patients with pre-existing fracture deformity. Orthopedics. 2007;30(5):373–378. doi: 10.3928/01477447-20070501-17. [DOI] [PubMed] [Google Scholar]
- 12.Archibeck MJ, White RE., Jr What’s new in adult reconstructive knee surgery. J Bone Joint Surg Am. 2003;85(7):1404–1411. doi: 10.2106/00004623-200307000-00056. [DOI] [PubMed] [Google Scholar]