Abstract
Purpose
Due to increasing life expectancy we see a rising number of joint replacements. Along with the proximal prosthesis in the femur, more and more people have a second implant on the distal ipsilateral side. This might be a retrograde nail or a locking plate to treat distal femur fractures or a constrained knee prosthesis in the case of severe arthrosis. All these constructs can lead to fractures between the implants. The goal of this study was to evaluate the risk of stress risers for interprosthetic fractures of the femur.
Methods
Thirty human cadaveric femurs were divided into five groups: (1) femurs with a prosthesis on the proximal side only, (2) hip prosthesis on the proximal end and a distal femur nail, (3) femurs with both a hip prosthesis and a constrained knee prosthesis, (4) femurs with a hip prosthesis on the proximal side and a 4.5-mm distal femur locking plate; the locking plate was 230 mm in length, with ten holes in the shaft, and (5) femurs with a proximal hip prosthesis and a 4.5-mm distal femur locking plate; the locking plate was 342 mm in length, with 16 holes in the shaft.
Results
Femurs with a hip prosthesis and knee prosthesis showed significantly higher required fracture force compared to femurs with a hip prosthesis and a distal retrograde nail. Femurs with a distal locking plate of either length showed a higher required fracture force than those with the retrograde nail.
Conclusions
The highest risk for a fracture in the femur with an existing hip prosthesis comes with a retrograde nail. A distal locking plate for the treatment of supracondylar fractures leads to a higher required fracture force. The implantation of a constrained knee prosthesis that is not loosened on the ipsilateral side does not increase the risk for a fracture.
Introduction
Orthopaedic surgeons increasingly face complications associated with arthroplasties. Every trauma surgeon is challenged by fractures of the femoral shaft between an intramedullary nail and an endoprosthesis, or between ipsilateral hip and knee arthroplasties. These so-called interprosthetic fractures occur infrequently, but the incidence is unknown. Kenny et al. found an incidence of 1.25 %, with four cases among a total of 320 limbs with ipsilateral hip and knee arthroplasties [5], while Fink et al. have seen 11 interprosthetic fractures in five years at their institutions [2]. However, a strong increase in the frequency of these fractures is expected, due to the dramatic aging of the population.
Periprosthetic fracture of the femur most commonly occurs immediately distal to the stem tip (Vancouver type B). But they can also occur on the distal end of the femur as Vancouver type C fractures. These fractures, depending on the fracture form, can be treated either by nailing or plating. As a third variation for another ipsilateral implant, constrained knee prostheses are used for the treatment of arthrosis in cases where those knees cannot be balanced adequately and a pure surface replacement is not sufficient.
However, all these various constructs with two implants in the femur occur as stress risers that may lead to interprosthetic fractures between the implants. Several questions therefore are not answered. Is the risk for a fracture between the implants higher with a retrograde nail and might it be better to use a locking plate as an extramedullary implant? Does a constrained knee prosthesis also increase the risk of a fracture or does the cement create a higher required fracture force even with a cement-free zone in the middle of the implants acting as a locus minoris resistentiae? In the present study, we test this hypothesis to evaluate the risk of stress risers in interprosthetic fractures of the femur.
Materials and methods
Specimens
The experimental design included human femurs matched by bone density. In total 30 femurs were frozen at −20 °C directly after dissection, and defrosted prior to the biomechanical testing. The specimens were from eight men and seven women, all aged 65 years and above (average age, 76.3 years; SD, 4.4 years). An osteoporotic bone model was chosen, because patients with osteoporosis have the highest incidence of periprosthetic fractures. The femurs were randomized on the basis of pQCT-data. The specimens were pair-matched by bone density in the same way as in prior biomechanical studies [7, 12–14].
pQCT measurements
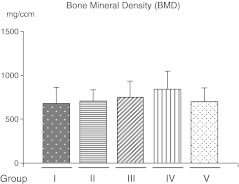
Matched femur pairs were selected based on bone density using a pQCT (XCT-2000; Stratec Medizintechnik, Pforzheim, Germany). The diaphysis and the supracondylar region of the femur were scanned. The pQCT device was calibrated using a standard phantom and a cone phantom provided by the manufacturer. A 2-mm thick single tomographic slice with a pixel size of 0.59 × 0.59 mm was taken from the transverse plane of the condylus and the middle of the diaphysis. Femur length was defined as the distance between the distal end of the condylus and tip of the greater trochanter. Image processing and calculation were performed using the manufacturer’s software package (version 2.01). The total cross-sectional area (CSA) was defined as the area enclosed within the outer bone border. The total volumetric bone mineral density (vBMD) was defined as the quotient of total bone mineral content (BMC) on the volume. Additional parameters were used to assess the cortical structure of the femoral shaft. The total femoral CSA was separated into three parts (cortex, subcortex, and marrow cavity) based on two thresholds: 710 mg/cm3 distinguishing the cortex from the subcortex, and 100 mg/cm3 separating the subcortex from the marrow cavity. The mean bone mineral density (BMD) was 767.5 mg/cm3 (SD 65). The threshold for specimens to be considered osteoporotic was defined as a BMD lower than 1000 mg/cm3 [7, 14]. On the basis of these measurements, the femurs were divided into five different groups in order to obtain maximum comparability (Fig. 1).
Fig. 1.
Bone mineral density was measured through the middle of the femur. Based on these measurements, the femurs were divided into five groups to achieve similar bone mineral density (BMD) and cortical thickness
For comparison, the femurs were divided into five groups to achieve similar bone mineral density (BMD) and cortical thickness:
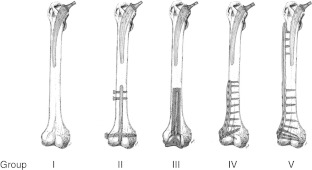
Group I: This group (n = 6) consisted of femurs with a prosthesis (Synergy Cemented Hip Stem, Smith & Nephew, Memphis, USA) on the proximal side only.
Group II: Six femurs with a hip prosthesis on the proximal end and a distal femur nail (length: 220 mm, diameter: 10 mm; T2™ Femoral Nailing System, Stryker GmbH & Co. KG, Duisburg, Germany).
Group III: Six femurs with both a hip prosthesis (Synergy Cemented Hip Stem, Smith & Nephew, Memphis, USA) and a knee prosthesis (Genesis II CC, Smith & Nephew, Memphis, USA).
Group IV: Six femurs with a hip prosthesis on the proximal side and a 4.5-mm distal femur locking plate (ten hole, 230-mm length; Smith & Nephew, Memphis, USA). The locking plate was 230 mm in length, with ten holes in the shaft, each of which can be used for 1 mm of compression or locking and can accept one of four different screws. We used 4.5-mm, locking, self-tapping, cortex screws that were predrilled with a 3.5-mm drill bit. Eight screws were used for each plate, three for the condyle and four for the shaft.
Group V: Six femurs with a proximal hip prosthesis and a 4.5-mm distal femur locking plate (Smith & Nephew, Memphis, USA). The locking plate was 342 mm in length, with 16 holes in the shaft. The plate design allows a choice between locking and compression screw insertion separately for each screw. In this study, all screws were locked and used bicortically.
All femurs were stripped of soft tissue and the medullary canals were prepared for prosthesis implantation. Each femur was implanted with a Synergy Cemented Hip Stem (Smith & Nephew, Memphis, USA) with bone cement (VersaBond Radiopaque Bone Cement, Smith & Nephew, Memphis, USA). The cement stopper was implanted to a depth of 1 cm below the prosthesis, further minimizing the variation in the distance between cement of the hip prosthesis and the knee prosthesis. Radiographs were taken after specimen preparation and implantation of the prosthesis to ensure an adequate cement mantle, position, length, and orientation. As in prior investigations, non-cemented stems were not tested, because it is impossible to simulate osseous ingrowth in a laboratory setting (Fig. 2) [7].
Fig. 2.
Illustration of the tested femur groups
Four-point bending test
A servohydraulic testing machine was used (MTS 858.2, Eden Prairie, MN USA). The femur was loaded between the middle two supports (length l2 in Fig. 3) with a constant bending moment according to Eq. (1).
 |
1 |
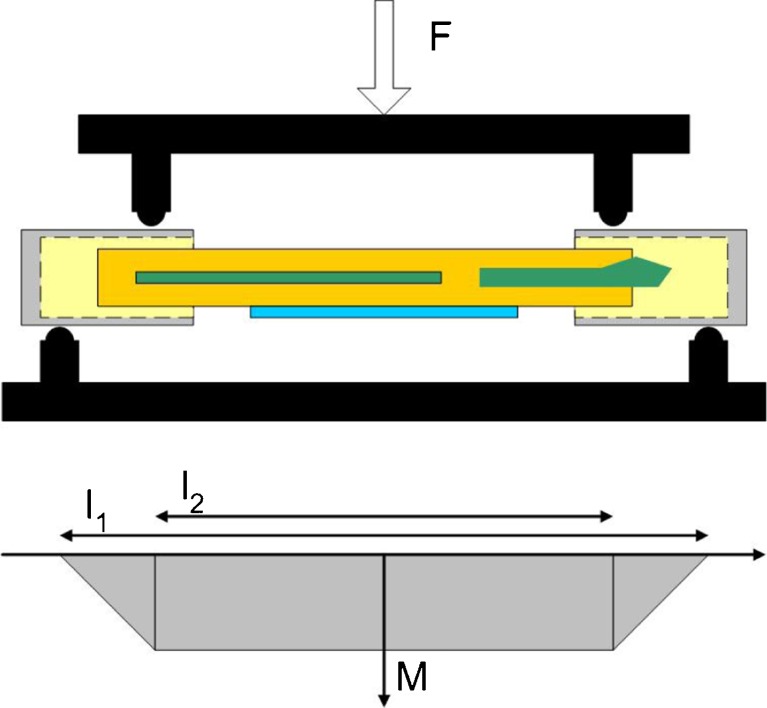
Fig. 3.
Schematic representation of the four-point bending test with a servohydraulic testing machine
where l1 is the distance between the outer supports, l2 is the distance between the inner supports, F is the applied force, and l is the lever arm length.
This setup omitted transverse force across the femur. Prior to testing, bones were embedded in polyurethane (Ureol FC53, Gößl & Pfaff, Karlskron, Germany) in steel pots. The lever arm was adjusted to eight cm and load was applied at a constant speed of 0.1 mm/s until fracture (Fig. 3).
Statistics
Statistical analyses were performed using SPSS for windows. The probability of a type I error was set to 5 %. Student’s t-test was used with unequal variances. Data are presented as mean and standard deviation (SD).
Results
There were no differences in bone mineral density between the groups, so every group started with the same source values.
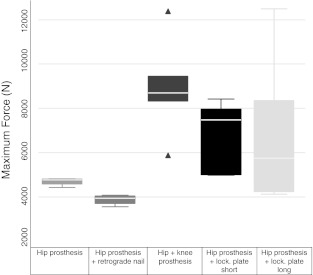
Group I: In group I femurs with hip prosthesis only exhibited periprosthetic fractures around the tip of the stem in all specimens. Mean fracture strength was 4692 N (± 183 N), which is significantly higher than in group II.
Group II: Femurs instrumented with hip prosthesis and intramedullary nail (group 2: F = 3875 N ± 229 N, p = 0.01) revealed the smallest fracture strength of all groups.
Group III: Mean fracture strength in group III (hip prosthesis and knee prosthesis) was 8894 N (± 2103 N), which was significantly higher than all other groups. In group III, the fracture occurred between the two “kissing” implants in all cases examined.
Groups IV and V: The femura were supplied with either short or long distal locking plates (6888 N ± 2103 N and 6335 N ± 3529 N, respectively; p = 0.051). Comparing both groups with locking plates at the distal end of the femur did not reveal any statistically significant differences. In femurs with distal lateral plating, the fracture always occurred at the proximal end of the plate with short locking plates (group IV), whereas the fracture occurred at the tip of the stem with the longer plates (group V).
Examining these results together we found remarkable significant differences between the group with an ipsilateral hip prosthesis and a retrograde nail in the femur and the group with both an ipsilateral hip prosthesis and knee prosthesis (Fig. 4). Two cemented stems in the femur showed much higher fracture strength (8894 N ± 2103 N) than the group with a hip prosthesis and an ipsilateral retrograde nail (3875 N ± 229 N; p = 0.002).
Fig. 4.
Box plot analysis for all tested groups. The required fracture force further decreases considerably if a retrograde nail was implanted. A constrained knee prosthesis did not show this effect; the large cement mantle imparts a very high required fracture force. With locking stable plates in the distal femur, the risk for a fracture is not as high as with a retrograde nail
In femurs stabilized with a distal femur plate, as expected, fracture strength was substantially higher with a plate than with a nail at the distal portion of the femur. Even so, the comparison of fracture strength between the groups with short lateral distal locking plates (group IV) and the group with distal retrograde nails reached statistical significance as tested by a two-sample t test with unequal variances (3875 N ± 229 N vs 6888 N ± 1511 N) (Fig. 4).
Discussion
Due to the increasing older population, more and more hip prostheses get implanted every year. This means that many older patients who suffer from a supracondylar fracture of the femur already have a hip prosthesis implanted. Orthopaedic surgeons have a variety of options available for the treatment of these supracondylar fractures, with retrograde nails or a locking plate being most commonly used to stabilize the fracture. In determining which to use, surgeons must consider multiple factors, including bone quality, fracture morphology, patient age, etc. Furthermore, some authors postulate that a constrained knee prosthesis could be a useful alternative to internal fixation in treating selected elderly patients with these fractures [1].
In preliminary studies, we found that a cemented prosthetic hip stem significantly reduced femoral fracture strength [14]. Treating a supracondylar fracture with a retrograde nail in the presence of a hip prostheses leads to a high risk for an interprosthetic fracture between these two intramedullary implants. Here we could show that an extramedullary implant would be better suited to stabilize such a supracondylar fracture. An extramedullary implant of any length resulted in much higher fracture load compared to the retrograde nail. Extramedullary implants on the distal end of the femur endured more charges than an intramedullary nail. These findings support the statement that an extramedullary implant is a biomechanically better solution for the treatment of supracondylar fractures compared to a retrograde nail. Other data show that locking stable plates in proximal periprosthetic fractures also provide very high stability [8], so that it can be summarized that for the periprosthetic fractures Vancouver type B1 and C locking plates from the biomechanical point of view are the best solution. Another treatment option for supracondylar fractures is the constrained knee prosthesis. Besides fracture treatment, there are multiple other indications for constrained knee prosthesis, including in knees with severe valgus deformities and a stretched or incompetent medial collateral ligament or those knees that cannot be balanced adequately in flexion and extension. Intra-operative disruption or inadvertent sectioning of the medial collateral ligament with a resected or incompetent posterior cruciate ligament may also require this prosthesis for required fracture force [6]. Interprosthetic femoral fractures—ones occurring between ipsilateral total hip and total knee arthroplasties—are an increasingly common and challenging problem for orthopaedic surgeons. Therefore, another purpose of this study was to evaluate the risk for femoral fractures between a hip and a knee prosthesis. Surprisingly, the specimens with another cemented intramedullary implant exhibited a substantially higher force to failure compared to those with retrograde intramedullary locking nails and the locking plates.
Examining the fractures that occurred around the proximal end of the distal femur nail, it was evident that most took place near the locking screws, suggesting that stress in this area decreased the stabilization of the whole construct.
The concept of femoral “stress risers” at or near surgical implants is well documented in the total joint literature and represents a legitimate concern for those treating fractures between hip and knee arthroplasties [9]. There is not yet a precise criteria for defining a femoral “stress riser,” but the term has been associated with the cortical width of the femur as it relates to metabolic bone disease, implant selection, canal preparation, and previous surgery or femoral fractures [4].
There are some limitations of this study. One major factor that cannot be simulated in such a biomechanical study is the loosening of the stem components. From various investigations, we know that this is a major stress riser for a periprosthetic fracture [10, 11]. Some studies have shown that, even for interprosthetic fractures, the loosening between the cement and the stem plays an important role and occurs in most described cases [3]. Biomechanical testing right after the filling of the cement might explain the substantially higher required fracture force compared to the non-cemented retrograde nails. It might be hypothized that, due to the destruction of the endost on the proximal and distal sides in vivo, the cortex weakens between the implants and may also lead to higher stress risers.
Furthermore, we could only show that there are remarkable differences regarding the stress risers in the femur caused by the different implants. But we do not know exactly how much the gap size between the implants influences the fracture strength. It can be assumed that this is negligible. A study by Ieasaka et al. suggests that a variable gap size has only a minor influence on stability and resistance of femoral stems in humans. In their experiments they could demonstrate that the size of the gap between two ipsilateral femoral stems does not affect peak tensile stress on the femur [4]. According to this study, the stress riser effect of an intramedullary metal stem inside a femur is clearly dependent on the femur's cortical density instead of gap distance.
The experimental setup is also somehow limited. We came to this experimental setup because applying the force through the femoral head in preliminary studies led to pertrochanteric fractures. So the periprosthetic fracture without a pre-existing osteotomy was only feasible through a lateral based force. Other methods like a three point bending have the limitation that the highest force acts at the central support and failure is initiated usually directly at this very point. In four-point bending, a constant moment acts between the middle two supports and failure is free to occur anywhere in this region. Furthermore, the load is split between the two middle supports, and such local fatigue at the contact point comprises a smaller problem. Therefore we chose the four point bending, which produces a constant moment between the two middle support points. In our opinion the fractures may not all result from the lateral based force but the cropper to the side as one of the clinical mechanisms, and the resulting fractures in this laboratory setting were most decisive.
In summary, we can conclude that use of a retrograde nail results in the highest stress riser in the femur with an existing hip prosthesis, while a distal locking plate leads to a higher required fracture force. Additionally, implantation of a constrained knee prosthesis that is not loosened on the ipsilateral side with a hip prosthesis in a biomechanical testing does not increase the risk for a fracture as might be expected.
Acknowledgments
Conflict of interest
I (we) certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Footnotes
Wolfgang Lehmann and Martin Rupprecht contributed equally and therefore share the first authorship.
References
- 1.Appleton P, Moran M, Houshian S, Robinson CM. Distal femoral fractures treated by hinged total knee replacement in elderly patients. J Bone Joint Surg Br. 2006;88:1065–1070. doi: 10.1302/0301-620X.88B8.17878. [DOI] [PubMed] [Google Scholar]
- 2.Fink B, Fuerst M, Singer J. Periprosthetic fractures of the femur associated with hip arthroplasty. Arch Orthop Trauma Surg. 2005;125:433–442. doi: 10.1007/s00402-005-0828-0. [DOI] [PubMed] [Google Scholar]
- 3.Hou Z, Moore B, Bowen TR, Irgit K, Matzko ME, Strohecker KA, Smith WR. Treatment of interprosthetic fractures of the femur. J Trauma. 2011;71:1715–1719. doi: 10.1097/TA.0b013e31821dd9f1. [DOI] [PubMed] [Google Scholar]
- 4.Iesaka K, Kummer FJ, Cesare PE. Stress risers between two ipsilateral intramedullary stems: a finite-element and biomechanical analysis. J Arthroplasty. 2005;20:386–391. doi: 10.1016/j.arth.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Kenny P, Rice J, Quinlan W. Interprosthetic fracture of the femoral shaft. J Arthroplasty. 1998;13:361–364. doi: 10.1016/S0883-5403(98)90187-5. [DOI] [PubMed] [Google Scholar]
- 6.Lachiewicz PF, Soileau ES. Results of a second-generation constrained condylar prosthesis in primary total knee arthroplasty. J Arthroplasty. 2011;26:1228–1231. doi: 10.1016/j.arth.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 7.Lehmann W, Rupprecht M, Hellmers N, Sellenschloh K, Briem D, Puschel K, Amling M, Morlock M, Rueger JM. Biomechanical evaluation of peri- and interprosthetic fractures of the femur. J Trauma. 2010;68:1459–1463. doi: 10.1097/TA.0b013e3181bb8d89. [DOI] [PubMed] [Google Scholar]
- 8.Lenz M, Windolf M, Muckley T, Hofmann GO, Wagner M, Richards RG, Schwieger K, Gueorguiev B. The locking attachment plate for proximal fixation of periprosthetic femur fractures-a biomechanical comparison of two techniques. Int Orthop. 2012;36:1915–1921. doi: 10.1007/s00264-012-1574-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mamczak CN, Gardner MJ, Bolhofner B, Borrelli J, Jr, Streubel PN, Ricci WM. Interprosthetic femoral fractures. J Orthop Trauma. 2010;24:740–744. doi: 10.1097/BOT.0b013e3181d73508. [DOI] [PubMed] [Google Scholar]
- 10.Mukundan C, Rayan F, Kheir E, Macdonald D. Management of late periprosthetic femur fractures: a retrospective cohort of 72 patients. Int Orthop. 2010;34:485–489. doi: 10.1007/s00264-009-0815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rupprecht M, Grossterlinden L, Barvencik F, Gebauer M, Briem D, Rueger JM, Lehmann W. Periprosthetic fractures. Long-term results after plate osteosynthesis stabilization. Unfallchirurg. 2008;111:812–820. doi: 10.1007/s00113-008-1470-4. [DOI] [PubMed] [Google Scholar]
- 12.Rupprecht M, Grossterlinden L, Ruecker AH, Oliveira AN, Sellenschloh K, Nuchtern J, Puschel K, Morlock M, Rueger JM, Lehmann W. A comparative biomechanical analysis of fixation devices for unstable femoral neck fractures: the Intertan versus cannulated screws or a dynamic hip screw. J Trauma. 2011;71:625–634. doi: 10.1097/TA.0b013e31820e86e6. [DOI] [PubMed] [Google Scholar]
- 13.Rupprecht M, Grossterlinden L, Sellenschloh K, Hoffmann M, Puschel K, Morlock M, Rueger JM, Lehmann W. Internal fixation of femoral neck fractures with posterior comminution: a biomechanical comparison of DHS(R) and Intertan nail(R) Int Orthop. 2011;35:1695–1701. doi: 10.1007/s00264-010-1199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rupprecht M, Sellenschloh K, Grossterlinden L, Puschel K, Morlock M, Amling M, Rueger JM, Lehmann W. Biomechanical evaluation for mechanisms of periprosthetic femoral fractures. J Trauma. 2011;70:E62–E66. doi: 10.1097/TA.0b013e3181e99ff1. [DOI] [PubMed] [Google Scholar]