Abstract
Purpose
The aim of this study was to compare two intramedullary devices used in the treatment of intertrochanteric fractures.
Method
During the period 2006–2007 46 TGN and 51 PFNA were used for the treatment of intertrochanteric fractures in our hospital. Clinical and radiological follow-up were available. Surgical time, blood loss and complications have been considered.
Results
The mean operative time for the TGN group was significantly higher than in the PFNA group (62 min and 45 min, respectively) with a p = 0.04. The mean blood loss was significantly higher in the TGN group (285 ml; SD 145) in relation to the PFNA group (226 ml; SD 136) with p = 0.03. Also, rate of complications was higher in the TGN group (p = 0.01). Clinical outcomes were good for both groups. Intra-operative and post-operative complications in the TGN group were associated with a longer operative time and a higher blood loss, probably due to the reaming needed in TGN that can increase blood loss and risk of comminution or fracture propagation. Moreover, all but one of the procedure-related complications were observed in very elderly patients.
Conclusions
Based on our results in the intertrochanteric fracture, use of PFNA should be recommended in cases of elderly and osteoporotic patients, while TGN should be used in more severely displaced fractures in patients with a slightly better bone mineral density.
Introduction
Intramedullary nailing (IM) has recently become a popular method of stabilisation of proximal femoral fractures in adults [1]. The proposed advantages include a short incision, less operative time, minimal blood loss and rapid rehabilitation of the elderly patient [2, 3], which is essential to minimize the risk of medical complications. Several studies have shown the superiority of IM nailing in this respect compared to other methods of fixation such as plate fixation [1, 4–7].
Optimal positioning of nail devices is of paramount importance for a good outcome, reducing the risk of complications. Complications described with intramedullary devices include fracture propagation, difficulties with interlocking, jamming of the compression screw within the nail, and cut-out and cut-off of the lag screw [8–10].
The methods of intramedullary nailing, with similar biomechanical principles, differ primarily with the need for diaphyseal reaming and the use of anti-rotation systems in fixing the femoral neck. The literature comparing the efficacy of these two implants remains obscure.
In our institution we have used both the Trochanteric Gamma3 Nail (TGN), characterized by the need for reaming and the use of lag screw, and the proximal femoral nail antirotation (PFNA), which is an unreamed nail with an antirotational helical blade. The primary objective of this study therefore is to compare the one year fracture fixation rates between the PFNA and TGN and to evaluate the differences in functional outcomes, quality of life outcomes, safety, radiological results, handling and perceived effectiveness between these two devices.
We completed a prospective comparative randomized study between TGN and the PFNA to evaluate if there were any significant differences between these two types of intramedullary implants characterized by similar surgical technique. Particularly attention was made in order to verify if the helical blade may enhance the overall stability of the construct and potentially reduce failure of fixation, compared to the lag screw and also to assess any differences between reamed and unreamed intramedullary nails.
Patients and methods
Between January 2006 and January 2008, 110 consecutive patients with mean age of 80.4 years were treated in our department for an intertrochanteric fracture. During this period patients were alternately assigned (on a 1:1 ratio) for treatment with a TGN (Trochanteric Gamma3 Nail, Stryker Howmedica) or PFNA (Proximal Femoral Nail Antirotation, Synthes).
Inclusion criteria were patients with isolated, unstable, closed, and type 31-A1, 2, 3 trochanteric fractures as classified with AO system without subgroup [11, 12]. The most common type in both groups was 31-A1, followed by 31-A2 and 31-A3. Exclusion criteria were pathologic fracture of any other cause than osteoporosis, multiple trauma, and life expectancy ≤ three months. All surgical treatments were performed by an expert surgeon, with more than 100 interventions for both fixation systems used in the study, to avoid problems related to learning curve.
In all cases the same antibiotic and thromboprophylaxis was administered with second generation cephalosporins and low molecular weight heparin. Length of operating time was recorded as well as blood loss (calculated with Rosencher method) [13].
Intra- and post-operative complications and medical complications were recorded. Clinical and radiological assessment was performed at one. three, six and 12 months to verify device positioning, bone healing and secondary malalignment. Malalignment was defined as a varus-valgus angulation of greater than 5°. Clinical outcome was evaluated by documentation of pain, restoration of previous walking ability and patient satisfaction. At the last follow up the Harris hip score (HHS) [14] was recorded.
The mean follow up was 15.1 ± 3.0 months (range, 12–24 months).
Statistical analysis of the results was performed with paired t-test to compare the two groups. With an anticipated effect size of 0.8 and a statistical power 0.88 we estimated our minimum sample size required was 62 patients. Minimum required sample size per group was 31.
Results
In group A, 51 patients with mean age of 81.7 (range, 51–97; SD, 9) were treated with PFNA, whereas in group B, 46 patients with mean age 80 (range, 55–98; SD, 9.1) were treated with the TGN. The two groups were homogeneous regarding age (p > 0.05).
In group A (patients selected for treatment with TGN) there were 32 with fracture type 31-A1, 15 with 31-A2 and eight with 31-A3; in group B (patients selected for treatment with PFNA) 35 were 31-A1, 13 were 31-A2 and seven were 31-A3 fractures.
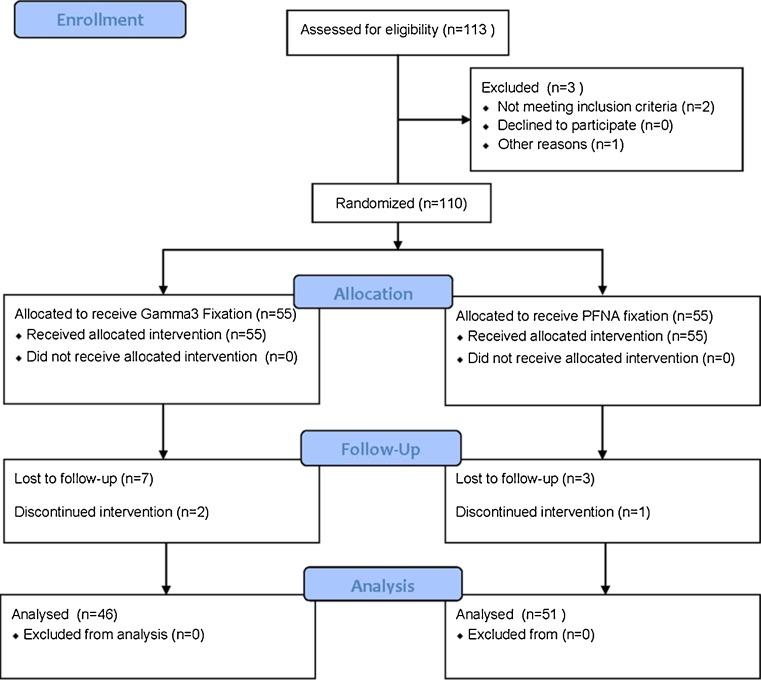
Thirteen patients were excluded from the study because they were lost at the first follow-up (five patients) or due to a discontinuity in the clinical assessment (eight). In total 97 cases were eligible to be included in the final analysis of the results, 51 in the group treated with PFNA and 46 in the group treated with Gamma3 (Fig. 1).
Fig. 1.
Flow diagram
The average pre-surgical stay was 2.4 days (min four hours, max eight days), and the average length of hospital stay was 10.5 days (min five, max 20).
The mean operative time was greater in the TGN group compared to in the PFNA group at 62 min (SD 34) and 45 min (SD 17), respectively (p = 0.04). Also the mean blood loss was higher in the TGN group at 285 ml in the TGN group (SD 145) versus 226 ml in the PFNA group (SD 136) (p = 0.03).
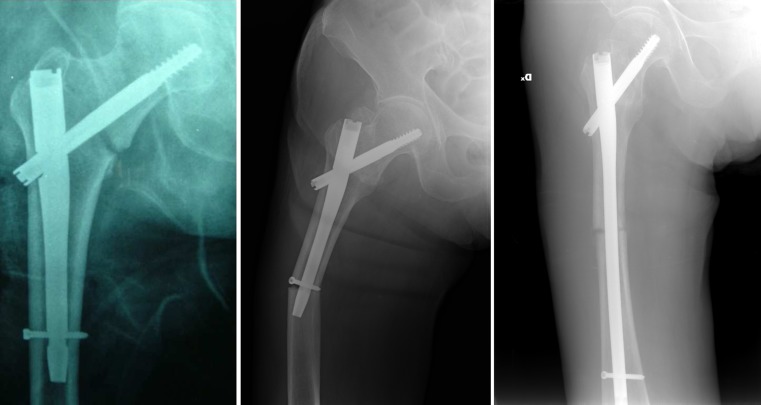
In the PFNA group, intra-operative complications were noted in one case. It was a fracture at the distal locking site treated with cerclage wire. Late complications occurred in 3.9 % of the cases including medial migration of the helical blade in the pelvis, and backing out of the PFNA blade in the soft tissues with loss of reduction (Fig. 2). The salvage treatment for these two cases was an hemiarthroplasty. In both cases the failure can be attributed to the imperfect locking of the helical blade.
Fig. 2.
Late complication in proximal femoral nail antirotation (PFNA) group. Preoperative radiography of intertrochanteric fracture type 31-A2, immediate postoperative radiography, backing out of the PFNA blade in the first month after the surgery
In the TGN group, 6.5 % of intra-operative complications were noted, namely, three fracture propagations during reaming (two cases) or nail insertion (one case), converted to a long gamma nail with cerclage wire in two cases and with just cerclage wire in one case (Fig. 3). Late complication occurred in 8.6 % of the patients including two lag screw cut-outs, one of which was associated with fracture propagation and treated with arthroplasty. One fracture was at the distal locking site treated with a long gamma nail (Fig. 4). Finally, one nonunion was observed and revised with a long gamma nail (Table 1). It is worth mentioning that all but one of these complications occurred in patients older than 81 years (mean 86.1, SD 4.2).
Fig. 3.
Intra-operative complication in Trochanteric Gamma3 Nail (TGN) group. Preoperative radiography of intertrochanteric fracture type 31-A1; immediate post-operative radiography of fracture propagation occurred during reaming and was treated with cerclage wire; radiographic control at 1 month
Fig. 4.
Late complication in the Trochanteric Gamma3 Nail (TGN) group. Immediate postoperative radiography of an intertrochanteric fracture type 31-A1; fracture at the distal locking site in the third month; postoperative radiography of the salvage treatment with long gamma nail
Table 1.
Complications
| Complication | PFNA group (n = 51) | GAMMA3 group (n = 46) | p |
|---|---|---|---|
| Intra-operative complications | 1 (1.9 %) | 3 (6.5 %) | |
| Post-operative complications | 2 (3.9 %) | 4 (8.7 %) | |
| Medical complications | 4 (7.8 %) | 5 (10.8 %) | |
| General complications | 7 (13.7 %) | 12 (26 %) | <0.001 |
| Mortality at six months | 6 (11.7 %) | 6 (13 %) | >0.05 |
PFNA proximal femoral nail antirotation
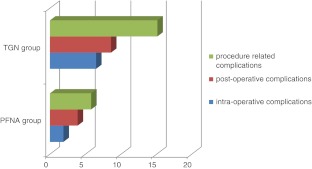
During the hospitalization, 10.8 % of medical complications (five chest infections) and 13 % of deaths (three in the first six months post-op, three in hospital) were noted in the TGN group; 8.6 % of medical complications (three chest infections and one neurosurgical complication) and 11.7 % of deaths (five in the first six months, one in hospital) were in the PFNA group with no significant statistical difference between the two groups. Comparison of procedure-related complications between the two groups are shown in Table 1 and Graph 1.
Graph 1.
Comparison between the two groups regarding the percentage of surgical complications
Statistical comparison showed that total rate of complications was significantly higher in the TGN group (p = 0.01).
Others minor complications encountered in both groups included seromas and haematomas of the surgical wound, which resolved satisfactorily in all cases, and wound infections also evolved favourably once antibiotic treatment was instituted (Table 2).
Table 2.
Minor complications encountered
| Complication | PFNA group (n = 51) | GAMMA3 group (n = 46) | p |
|---|---|---|---|
| Haematomas | 1 | 1 | |
| Wound infections | 0 | 1 | |
| Seromas | 1 | 0 | |
| Total | 2 | 2 | p > 0.05 |
PFNA proximal femoral nail antirotation
Thirty-one malalignments (13 valgus and four varus) occurred. Six valgus and one varus were observed in the TGN group, seven valgus and three varus in the PFNA group, with a prevalence of varus angulation in the PFNA group (p < 0.01).
With regard to clinical outcome, the average HHS in the third month was 78 (range 35–98, SD 14.7) for the TGN group and 76 (range 38–94, SD 13.1) for the PFNA group.
In the TGN group 51.5 % of patients (20\39) were able to walk, 41 % (16\39) had an assisted walking ability and three patients (7.5 %) were unable to walk. Only 12.5 % of patients (5\39) had pain in the hip while walking.
In the PFNA group, 45.5 % of patients (21\45) were able to walk, 48 % (22\45) had an assisted walking ability and in 6.5 % (three cases) patients were unable to walk. In 17.3 % of cases (eight out of 45) patients had pain in the hip while walking.
However, 95 % of the patients in the TGN group and 97 % of those in the PFNA group were satisfied with the results. Eighty-two percent of patients in the TGN and 86 % in the PFNA group were restored to the previous walking ability at the time of latest follow-up. Clinical outcomes essentially were good for both groups with no statistical differences between TGN and PFNA results (Table 3).
Table 3.
Clinical outcome, p > 0.01
| Outcome | PFNA group (n = 45) | GAMMA3 group (n = 39) |
|---|---|---|
| HHS | 78 (SD 14.7) | 76 (SD 13.1) |
| Restoration of previous walking ability | 86 % | 82 % |
| Satisfaction | 96 % | 95 % |
| Residual pain | 17 % | 12.5 % |
HHS Harris hip score, PFNA proximal femoral nail antirotation, SD standard deviation
Discussion
Lately, due to the increasing age of the elderly population, the incidence of extracapsular hip fractures has been gradually increasing. The poor bone quality in this group of patients requires choosing a fixation device that can increase stability and minimize surgical complications.
In our study both intramedullary systems confirmed their reliability for the treatment of intertrochanteric fractures. Early operation (average pre-surgical stay less than two days) and early mobilisation were practised in all patients to minimize the risk of medical complications and to improve functional outcome according to the literature [11]. We noted a small rate of complications and satisfactory results in both groups in relation to the restoration of walking ability and patient’s satisfaction [15–17]. Both the rate of complications and mortality were relatively low in both groups, even compared to the literature [18].
Nevertheless, we found a significantly higher blood loss, higher rate of intra-operative complications and higher surgical time in the TGN group, despite clinical outcomes being good in both groups. We believe that this result is secondary to the reaming required for the placement of TGN that can increase blood loss and risk of comminution or fracture propagation [19].
With regard to postoperative complications, the PFNA seems to be the most reliable method for an increased stability and higher cut-out resistance. This can be attributed to the helical blade that prevents rotation of the femoral neck. Indeed no cut-outs were found in the PFNA group. In a biomechanical study the dual lag screw implant exhibited significantly less migration and sustained more loading cycles in comparison to the single screw [20]. Some comparative studies have shown an increased number of intra-operative complications in patients treated with PFN, probably due to a more demanding technique [8, 9]. Herrera et al. reported an higher rate of technical complication with gamma nail also in comparison with PFN [16].
The helical blade has probably resolved the problems previously observed with PFN.
Al-Munajjed et al. underlined that the helical blade showed a significantly higher torque for the rotation of the femoral head compared to the lag screw. Bone impaction around the PFNA blade could probably be the reason for the higher biomechanic stability, thus decreasing the risk of malrotation and varus collapse [21].
In the two cases of PFNA where failure was observed, surgical error rather than implant stability issues should probably be attributed. The cutout appeared to result from poor position of the proximal screw in the femoral head, rather than being implant-related. The importance of an optimal position of the screw has been emphasized before [22].
However, our study seems to suggest that the major difference between these two implant designs (the manner in which the femoral head is stabilized) may have a role in the different rate of complications.
Moreover we observed that all but one of the surgical complications occurred in very old patients (mean age 86 years). We believe that the differences between the two devices may have more significance in osteoporotic bone of very elderly patients.
Predrilling and tapping needed for the TGN-3 sliding screw and reaming practised in the femoral shaft could be the reasons for this increased risk in patients with severe osteoporosis.
Secondary varus malalignment, without clinical significance, occurred at a greater rate when using the PFNA. In our opinion, this is probably due to the different insertion method of the cephalic screw. With the TGN system the best radiographic result could be obtained in terms of the femoral neck angle and reduction of fragment. However, the PFNA is technically demanding. The helical blade is inserted by means of a hammer and this can increase the gap or produce minor changes of femoral neck angle [23]. In any case, this seems not to have influenced clinical results nor complication rate.
According to our results, the PFNA seems currently to be the optimal implant, especially in very old patients with severely osteoporotic bone. We could speculate that in cases of very old patients and in severe osteoporosis the use of a more stabilizing device should be recommended.
In conclusion, on the basis of the results of this study, in the intertrochanteric fracture use of PFNA should be recommended in case of elderly and osteoporotic patients, while TGN should be used in more severely displaced fractures in patients with a slightly better bone mineral density.
Several new treatments for proximal femoral fractures, initially considered extremely reliable, have been proven less effective than expected [24]. In our opinion and according to our results, the choice of implant should be done pre-operatively by evaluating fracture type, patient anatomy, bone quality and patient age. In this way, the characteristics of different devices can be taken into account and identification of some limitations avoided.
Acknowledgments
Conflict of interest
We declare that we have no conflicts of interest in the authorship or publication of this contribution.
References
- 1.Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg. 2008;90:700–707. doi: 10.2106/JBJS.G.00517. [DOI] [PubMed] [Google Scholar]
- 2.Leung KS, So WS, Shen WY. Gamma nails and dynamic hip screw for peritrochanteric fractures a randomized prospective study in elderly patients. J Bone Joint Surg. 1992;74:345–351. doi: 10.1302/0301-620X.74B3.1587874. [DOI] [PubMed] [Google Scholar]
- 3.Sadowski C, Lubbeke A, Saudan M. Treatment of revers oblique and transverse intertrochanteric fractures with use of intramedullary nail or 95° screw plate. J Bone Joint Surg. 2002;84:372–381. [PubMed] [Google Scholar]
- 4.Hardy DCR, Descamps P, Krallis P, Fabeck L, Smets P, Bertens CL, Delince FE. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J Bone Joint Surg. 1998;80:618–630. doi: 10.2106/00004623-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2005;19(4):CD000093. doi: 10.1002/14651858.CD000093.pub3. [DOI] [PubMed] [Google Scholar]
- 6.Pelet S, Arlettaz Y, Chevalley F. Ostheosyntesis of per-and subtrochanteric fractures by blade plate versus gamma nail. A randomized prospective study. Swiss Surg. 2001;7(3):126–133. doi: 10.1024/1023-9332.7.3.126. [DOI] [PubMed] [Google Scholar]
- 7.Moroni A, Faldini C, Pegreffi F. Dynamic hip screw compared with external fixation for treatment of osteoporotic pertrochanteric fractures. A prospective, randomized study. J Bone Joint Surg. 2005;87:753–759. doi: 10.2106/JBJS.D.01789. [DOI] [PubMed] [Google Scholar]
- 8.Müller M, Seitz A, Besch L, Hilgert RE, Seekamp A. Proximal femur fractures: results and complications after osteosynthesis with PFN and TGN. Unfallchirurg. 2008;111(2):71–77. doi: 10.1007/s00113-008-1393-0. [DOI] [PubMed] [Google Scholar]
- 9.Megas P, Kaisidis A, Zouboulis P, Papas M, Panagopoulos A, Lambiris E. Comparative study of the treatment of pertrochanteric fractures- trochanteric gamma nail vs proximal femoral nail. Z Orthop Grenzgeb. 2005;143(2):252–257. doi: 10.1055/s-2005-836453. [DOI] [PubMed] [Google Scholar]
- 10.D’Arrigo C, Perugia D, Carcangiu A, Monaco E, Speranza A, Ferretti A. Hip arthroplasty for failed treatment of proximal femoral fractures. Int Orthop. 2010;34(7):939–942. doi: 10.1007/s00264-009-0834-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karunakar AM, McLaurin TM, Morgan JS, Egol KA. (2009) How to improve outcomes after perthrocanteric fracture. Instructional course lecture handout. 2009 AAOS Annual Meeting, Las Vegas, NV
- 12.Pervez H, Parker MJ, Pryor GA, Lutchman L, Chirodian N. Classification of trochanteric fracture of the proximal femur: a study of the reliability of current systems. Injury. 2002;33(8):713. doi: 10.1016/S0020-1383(02)00089-X. [DOI] [PubMed] [Google Scholar]
- 13.Rosencher N, Kerkkamp HE, Macheras G. Orthopedic surgery transfusion haemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion. 2003;43:459–469. doi: 10.1046/j.1537-2995.2003.00348.x. [DOI] [PubMed] [Google Scholar]
- 14.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 15.Brunner A, Jöckel JA, Babst R. The PFNA proximal femur nail in treatment of unstable proximal femur fractures—3 cases of postoperative perforation of the helical blade into the hip joint. J Othop Trauma. 2008;22:731–736. doi: 10.1097/BOT.0b013e3181893b1b. [DOI] [PubMed] [Google Scholar]
- 16.Herrera A, Domingo LJ, Calvo A, Martìnez A, Cuenca JA. Comparative study of trochanteric fractures treated with the gamma nail or the proximal femoral nail. Int Orthop. 2002;26:365–369. doi: 10.1007/s00264-002-0389-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schipper IB, Steyerberg EW, Castelein RM, Heijden FHWM, Hoed PT, Kerver AJH, Vugt AB. Treatment of unstable trochanteric fractures—randomised comparison of the gamma nail and the proximal femoral nail. J Bone Joint Surg Br. 2004;86B:86–94. [PubMed] [Google Scholar]
- 18.Perez JV, Warwick DJ, Case CP, Bannister GC. Death after proximal femoral fracture-an autopsy study. Injury. 1995;26:237–240. doi: 10.1016/0020-1383(95)90008-L. [DOI] [PubMed] [Google Scholar]
- 19.Docquier PL, Manche E, Autrique JC, Geulette B. Complications associated with gamma nailing. A review of 439 cases. Acta Orthop Belg. 2002;68(3):251–257. [PubMed] [Google Scholar]
- 20.Kouvidis GK, Sommers MB, Giannoudis PV, Katonis PG, Bottlang M. Comparison of migration behavior between single and dual lag screw implants for intertrochanteric fracture fixation. J Orthop Surg Res. 2009;18:4–16. doi: 10.1186/1749-799X-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Munajjed AA, Hammer J, Mayr E, Nerlich M, Lenich A. Biomechanical characterisation of osteosyntheses for proximal femur fractures: helical blade versus screw. Stud Health Technol Inform. 2008;133:1–10. [PubMed] [Google Scholar]
- 22.Schipper IB, Steyerberg EW, Castelein RM, et al. Treatment of unstable trochanteric fractures. Randomised comparison of the gamma nail and the proximal femoral. J Bone Joint Surg Br. 2004;86(1):86–94. [PubMed] [Google Scholar]
- 23.Hwang JH, Oh JK, Han SH, Shon WY, Oh CV. Mismatch between PFNa and medullary canal causing difficulty in nailing of the pertrochanteric fracture. Arch Orthop Trauma Surg. 2008;128(12):1443–1446. doi: 10.1007/s00402-008-0736-1. [DOI] [PubMed] [Google Scholar]
- 24.Nikolaou VS, Papathanasopoulos A, Giannoudis PV. What’s new in the management of proximal femoral fractures? Injury. 2008;39(12):1309–1318. doi: 10.1016/j.injury.2008.09.001. [DOI] [PubMed] [Google Scholar]