Abstract
Dual mobility cup systems in total hip arthroplasty consist of a metal back with a non-constrained liner, in which a constrained standard head articulates. While superior stability of such implants in comparison with standard total hip replacements is assumed, it is the purpose of this study to outline the biomechanical concept of dual mobility cups and to describe implant survival and dislocation rate based on the series published in the English-speaking and Francophone literature. A growing body of evidence indicates reduced dislocation rates in primary and revision total hip arthroplasty and in selected tumour cases. The limited availability of studies evaluating long-term implant survival and existing concerns with regard to increased wear rates and aseptic loosening, leads to the conclusion that such implants have to be used with prudence, particularly in standard primary hip arthroplasty and in young patients.
Introduction
Instability after total hip arthroplasty (THA) remains an important complication, with reported dislocation rates ranging from 2 to 3 % [1–3]. Constrained devices for patients with chronic instability remains an option; however, there are few studies in the current literature that describe its use. Such systems are associated with a high rate of aseptic loosening, which has been reported to be in the order of 10 to 26% [4–6]. Furthermore, cases of dissociation of the liner/cup interface, failure by breakage, and excessive polyethylene wear have also been described [7]. Therefore, in order to increase the stability while avoiding the excessive stress on the cup/bone interface that invariably occurs in fully constrained systems, Bousquet in France designed the “double mobility cup” in 1976. In the English literature, the term “tripolar cup” is commonly used to describe this system, which consists of a combination of two apparent joints, one large unconstrained joint between the metal cup and the liner, and a smaller constrained joint between the liner and a standard metallic head that is attached to the femoral component. As such, the large diameter of the unconstrained joint (i.e. effective head size) theoretically reduces the risk of dislocation.
Nevertheless, many surgeons have been hesitant to use tripolar cups due to fears of excessive polyethylene wear. In vitro studies [8] have shown that large metal-polyethylene friction surfaces are associated with increased polyethylene wear rates. However, these studies are based on experimental models using standard THA with various head sizes. Data on kinematics of tripolar cups in vivo and on its effect on wear rates are currently limited.
In recent times, a number of clinical studies with significant follow-up have been published [9–18]. Therefore the aim of this study was to review the current and historic English and French literature with regard to clinical outcome of tripolar cups and discuss the in vitro studies that have evaluated the biochmechanical basis of such systems.
Factors influence prosthetic joint stability
The factors that influence prosthetic joint stability can be broadly classified into three main groups—patient factors, technical or surgical factors and prosthetic factors. In terms of patient factors that can increase the risk of joint dislocation, both gender and age have been shown to play an important role. Several studies have shown that women have a higher dislocation rate compared to men [1, 3, 19], and the cumulative risk seems to increase with advancing age, in particular when over the age of 70 years [1]. This has been attributed to older patients having possibly poorer soft tissues, with a greater incidence of episodes of confusion and thus noncompliance with dislocation precautions [20]. Technical or surgical factors that contribute to joint instability include previous surgery to the hip [3], posterior approach or trochanteric osteotomy and implant malpositioning [21]. Prosthetic factors include the size of the femoral head component, the size of the acetabular cup and also the degree of femoral neck offset [22]. Jameson et al. [23] examined 247,546 procedures and demonstrated a significant reduction in the dislocation rate when using larger femoral heads.
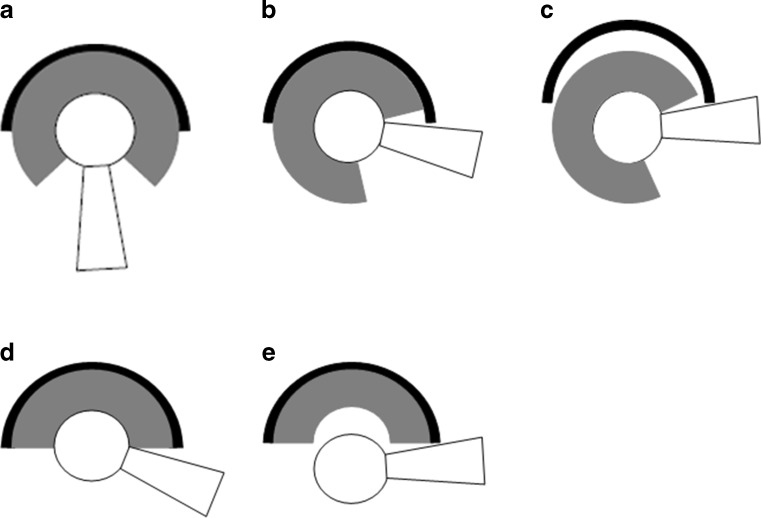
The dual-mobility cup is a tripolar cup with a fixed porous-coated or cemented metal cup, which articulates with a large mobile polyethylene liner (Fig. 1). Into the latter, a standard head (usually 22 or 28 mm) is inserted. The articulation between the head and the liner is constrained, while the articulation between the liner and the metal cup is unconstrained (Fig. 2). The interposition of a mobile insert represents an increase in the effective head diameter. Due to a favourable head-neck ratio, such systems allow greater range of motion whilst avoiding early femoral neck impingement with a fixed liner or metal cup. Tripolar cups, therefore theoretically reduce the risk of dislocation.
Fig. 1.
Uncemented and cemented versions of a dual mobility cup. In this particular cup, a cylindrical extension (double arrow) beyond a hemisphere is added for additional joint stability (courtesy of Symbios SA, Yverdon-les-Bains, Switzerland)
Fig. 2.
Dual mobility cup with metal cup (black), polyethylene liner (grey) and head/neck (white) (a, b, c) and a standard fixed-liner implant (d–e). During motion, the neck impinges with the liner, causing rotation in the unconstrained joint between the liner and the metal cup (b). Subluxation occurs if the neck impinges with the metal cup (or in cases of extra-articular impingement) (c). Due to a more favourable (effective) head-neck ratio, dual mobility cups (b) permit a larger range of motion compared to fixed-liner implants (d) and dislocation occurs earlier (e)
Several studies have shown that the use of large femoral heads reduces the rate of dislocation [23, 24]. However, the theoretical jumping distance (i.e. the amount of lateral femoral head translation necessary for dislocation to occur) does increase with head size. Interestingly, Sariali et al. [25] demonstrated, using numerical models, that the theoretical gain in stability using large head diameters becomes negligible with increasing abduction angle of the cup.
Wear
The usual wear rate of metal-on-polyethylene couples is 0.1–0.2 mm/year [26]. Progression of osteolysis seems to be correlated with wear rates and size of the particulate debris [27]. Dumbleton et al. in 2002 observed that osteolysis was relatively uncommon when linear wear rates were less than 0.1 mm/year [27].
The trade off with larger femoral heads is thinner acetabular bearings. To date, there is a large body of evidence that suggests that thinner liners that are made of conventional polyethylene are associated with excessive wear rates, thereby invariably limiting implant survival [28, 29]. The advent of highly cross-linked polyethylene and hard bearings such as cobalt-chrome or ceramic has therefore been proposed to limit this disadvantage, hence allowing the use of larger heads with low wear rates. The long-term survival rates of highly cross-linked polyethylene has not been fully established; however, short-term studies have shown a 45 to 99 % reduction in wear at three to five years [23, 28, 29]. The benefit of a tripolar acetabular component is that for a given cup diameter, a larger effective head size (i.e. outer diameter of the constrained polyethylene liner) can be used, as compared to all conventional fixed-liner devices.
Measuring the wear of tripolar cups cannot be performed using the X-ray technique described by Wroblewski [30] for standard acetabular cups. This method quantifies the extent of eccentric placement of the head within the liner. In tripolar cups, the femoral head is poorly visible on standard antero-posterior views due to its deep position in the metal cup, which often is designed with a cylindrical extension onto the hemisphere (Fig. 1a). In addition, the position of the mobile liner cannot be accurately determined on plain radiography, as head eccentricity reflects the combined wear of both the inner and outer liner surface, which is difficult to distinguish on plain X-rays. As a result, due to the large diameter of the inserts in tripolar cups, volumetric wear at the interface between the liner and the cup may be substantial even with minimal linear wear.
Another type of liner wear that has been described is “intra-prosthetic dislocation” which has been introduced to describe excessive wear at the head-liner interface, leading to internal subluxation and an incongruent articulation between the head and the metal cup and the development of excessive metallosis.
Adam et al. [31] analysed 40 retrieved tripolar cups (with 22.2 mm heads), which were removed after septic or mechanical failure. The mean interval between implantation and retrieval was eight years (range, 3–15.5 years). Macroscopic examination was followed by a surface analysis with measurement of changes of internal and external liner sphericity. Internal concavity was measured in the three dimensions using a 4-mm stylus. External convexity was measured by lateral projection. Linear and volumetric wear was determined by comparing the corresponding dimensions of new inserts. Linear and volumetric wear observed in these 40 cups were comparable to those reported for standard metal-on-polyethylene bearing couples (with 22.2-mm heads) [30, 32, 33]. In addition, the combined wear on both the convex and concave surface in tripolar cups was comparable with conventional metal-on-polyethylene bearings [33]. Mean linear wear (i.e. sum of wear on the convex and concave surfaces) was 82±72 μm. Total annual volumetric wear was 54±40 mm3/year (29±28 mm3/year on the convex and 26±23 mm3/year for the concave surface).
We are not aware of any data regarding the movement in the unconstrained articulation of tripolar cups (i.e. between the liner and the metal cup) over time. It seems likely that this movement diminishes with time, an effect that was observed with bipolar hemi-arthroplasties [34]. The fact that Adam et al. [31] report similar wear rates for both articulations suggests that the volumetric wear per cycle is greater in the unconstrained articulation compared to the articulation between the head and the liner.
To overcome increased wear rates of tripolar cups, highly crossed-linked polyethylene liners have been introduced. Wear rates of such implants appear to be lower than previously reported for standard polyethylene liners [10]. However, this effect has yet to be confirmed by independent clinical trials with long-term clinical follow-up. To date, hard bearings in tripolar cups (i.e. all ceramic tripolar systems [35]) have not yet been introduced into the routine clinical practice and, as such, the data is limited.
Cup fixation
Farizon et al. [36] previously described the changes in design of the first-generation tripolar cup, which were the result of failure of cup fixation due to delamination of the alumina layer coating on a grit-blasted surface. The first modification consisted of substitution of the alumina with hydroxyapatite on grit-blasted surfaces, and at the same time, the fixation of the tripolar cup was converted to a press-fit fixation with additional security achieved with extra-acetabular screws.
Massin et al. [37] analysed the results of the design modification of the second-generation of tripolar cups. The authors retrospectively analysed 2601 s-generation cups, with a mean follow up of five years (5–11 years). They reported that the survival of grit-blasted cups was less than that for press-fit, suggesting that primary fixation of grit-blasted dual-mobility cups should be secured with screws [37].
Clinical series
We conducted a comprehensive literature search on Medline using the search terms dual mobility or tripolar cup. Data was analysed with regard to the type of implant, the bearing couple, head and cup size, implant survival rates and complications such as early and late dislocation and wear rate.
We retained two prospective [38, 39] and 13 retrospective studies (Table 1) for evaluation. With the exception of the first case series by Farizon et al. [36] published in 1998, all studies were dated after 2006. All studies are of level 4 evidence, except the study from Adam et al. [39], which was level 3. The selected studies include 12 retrospective and two prospective case series. In addition, the study by Vielpeau et al. [9] is a case–control study comparing two different types of tripolar cups. Six studies have a mean follow-up of more than ten years [2, 9, 13, 36, 40, 41].
Table 1.
Clinical series of dual mobility cups
| Study | Patients, N | Indication | Study type | Mean follow up (range) | Implant (cup) | Head size | Dislocations | Implant survival 5 years | Aseptic loosening | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Early | Late | Intra-prosthetic | 5 y | 10 y | 15 y | 18 y | 20 y | ||||||||
| Farizon et al. 1998 [36] | 135 | Primary THR | Retrosp. | 10 y | Novae®a | 22.2 mm | n/a | n/a | n/a | n/a | 95.4 % | n/a | n/a | n/a | 4 |
| 2.9 % | |||||||||||||||
| Philippot et al. 2006 [53] | 106 | Primary THR | Retrosp. | 10 y | Novae-1®a | 22.2 mm | 0 | 0 | 2 | n/a | 94.6 % | n/a | n/a | n/a | 2 |
| 1.8 % | |||||||||||||||
| Leclercq et al. 2008 [38] | 194 | Primary THR | Prosp. | 6 y | Evora®b | 22.2 mm (n=175) | 0 | n/a | n/a | 100 % | n/a | n/a | n/a | n/a | |
| 26 mm (n=18) | |||||||||||||||
| 28 mm (n=7) | |||||||||||||||
| Lautridou et al. 2008 [40] | 437 | Primary THR | Retrosp. | 16.5 y | Novae-1®a | 22.2 mm | 2 | 3 | n/a | 84.4 % | n/a | n/a | n/a | n/a | 6.8 % |
| 0.45 % | 0.68 % | ||||||||||||||
| Langlais et al. 2008 [44] | 82 | Revision | Retrosp. | 3 y (2–5) | Medial cup®c | 22 mm | 1 | n/a | n/a | 94.6 % | n/a | n/a | n/a | n/a | 2 |
| 2.3 % | |||||||||||||||
| 1.1 % | |||||||||||||||
| Philippot et al. 2009 [2] | 384 | Primary THR | Retrosp. | 15 y (12–20) | 79 Novae-1®a titanium | 22.2 mm | n/a | n/a | 14 | n/a | n/a | 96.7 % | 95.9 | n/a | 13 |
| 3.6 % | |||||||||||||||
| 305 Novae-1®a inox | |||||||||||||||
| Guyen et al. 2009 [43] | 54 | Revision unstable THR | Retrosp. | 2.2 y (2.2-6.8) | Saturne®d | n/a | 3 | n/a | n/a | 94.5 % | n/a | n/a | n/a | n/a | n/a |
| 5.5 % | |||||||||||||||
| Hamadouche et al. 2010 [18] | 51 | Revision | Retrosp. | 51.4 m | Medial cup®c | 22.2 mm | 2 | n/a | 1 | 96 % | n/a | n/a | n/a | n/a | 2 % |
| (25–76.3) | 4.3 % | 2 % | (36 m) | ||||||||||||
| Philippeau et al. 2010 [16] | 71 | Tumor resection | Retrosp. | n/a | 29 Avantage®e | n/a | 7 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| 19 Saturne®d | |||||||||||||||
| 14 Novae®a | 9.8 % | ||||||||||||||
| 9 other | |||||||||||||||
| Massin and Besnier 2010 [17] | 23 | Primary THR | Retrosp. | 4.5 y | Collegia®f | 22 mm (n=17) | 2 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| 28 mm (n=6) | 8.6 % | ||||||||||||||
| Tarasevicius et al. 2010 [14] | 42 | Neck fractures | Retrosp. | 1 y | Avantage®e | 28 mm | 0 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Boyer et al. 2011 [13] | 240 | Primary THR | Retrosp. | 22 y (19–24) | Novae®a | 22 mm | 0 | 0 | 0 | n/a | n/a | 81.4 % | n/a | 75.4 % | n/a |
| Vielpeau et al. 2011 [9] | 668 (437/231) | Primary THR | Retrosp. | 16.5 y group A | Group A original Bousquet cup | 22.2 mm | 2/0 | 3/0 | 2 | 95.6 % | 90 % /n/a | 84.4 % /n/a | n/a | n/a | 30 |
| 5 y group B | Group B Novae-E®a | 0.45 %/0 % | 0.68 %/0 % | 0.45 % | 99.6 % | ||||||||||
| Leider-Wackenheim et al. 2011 [12] | 59 | Revision | Retrosp. | 8 y (6–11) | 44 Novae-1®a | 28 mm | 1 | n/a | n/a | 98 % | n/a | n/a | n/a | n/a | 0 |
| 15 Novae-E®a | 1.7 % | (8 y) | |||||||||||||
| Ada et al. 2012 [39] | 214 | Neck fractures | Retrosp. | 3-9 m | Saturne®d | 28 mm (n=182) | 3 | n/a | 0 | n/a | n/a | n/a | n/a | n/a | 2 |
| 22.2 mm (n = 32) | 1.4 % | 0.9 % | |||||||||||||
y year, m month, retrosp retrospective, prosp prospective, n/a not available
a SERF Dedienne santé, Décines, France
b SEM Science et Médecine, Montrouge, France
c Aston, St Etienne, France
d Amplitude, Rhône-Alpes, France
e Biomet, Indiana, USA
f Wright Medical, Créteil, France
Overall, there was a total of 2,758 total hip arthroplasties with tripolar cups in the 14 studies that were included. The mean follow up ranged from one to 22 years. Case selection was not homogenous in the different series; eight studies included exclusively cases of primary total hip arthroplasty. In four studies, cases of THA revision for recurrent dislocations were selected. Two studies analysed a series of femoral neck fractures [14, 39] and one reconstruction after tumour resections [16].
Vielpeau et al. [9] reported a large series of 668 cases of primary THA. A subgroup of 437 cases with original Bousquet tripolar cups (Novae-1®, Serf, France) with a mean follow up of 16.5 years was compared with a subset of 231 cases with second generation cups (Novae E® Serf, France) with a follow up of 5.2 years. Revision-free survival was 95.6 % and 84.4 % at five and 15 years, respectively, for the original Bousquet cups. The second generation Novae® cups showed a five-year survival rate of 99.6 %.
Philippot et al. [2], Boyer et al. [13], Lautridou et al. [40], and Farizon et al. [36] also reported large series with long follow up including 384, 240, 437 and 135 cases, respectively. These series are homogenous in that the original first generation Bousquet cups with 22.2-mm metal heads were implanted through an anterolateral approach. The 15-year revision-free survival rates ranged from 81.4 to 96.7 %.
These survival rates are comparable to THRs with other bearings. The annual Swedish Joint Registry [42] reported revision-free survival rates of 85–90 % with uncemented cup and 90–95 % with cemented cup. Uncemented stems have a revision-free revision from 97 to 98 % as compared to cemented stems, with rates ranging from 95 to 96 %.
Important complications described in these four series [2, 13, 36, 40] included, on the acetabular side, aseptic loosening (1.8–3.4 %), granulomas (4 %), polyethylene fracture (0.7 %), “excessive” polyethylene wear (1–1.8 %) or acetabular screw fracture (1 %). On the femoral side, reported complications included aseptic (2–3 %) or septic loosening (0.8 % only described in the study of Boyer et al. [13]), femoral granulomas or osteolysis (0–11 %), unscrewing of the femoral stem (2 %), and stress shielding (1.8 %).
Vielpeau et al. [9] noted in the group of the original Bousquet cup, 30 revisions were for loosening and there were five cases of dislocation (1 %, two early and three delayed). He also reported 28 cases of osteolytic granulomas at five years (6 %). However, no case of dislocation or revision surgery for aseptic loosening was reported in the subset of 231 with the second generation Novea® cups. Two femoral granulomas were described during the first five years of follow-up (1 %).
Leclercq et al. [38] published the only prospective, nonrandomised, multicentre evaluation for primary arthroplasty with the use of tripolar cups. They reported 194 cases with a mean follow up of six years (range, five to seven years). Two cemented stems presented a radiolucent line in the metaphyseal zone. Three patients (1.5 %) underwent revision surgery: one for aseptic loosening of the stem, one for periprosthetic fracture at three years and one for haematogenic infection. No dislocations were reported in this series.
Tarasevicius et al. [14] compared dislocation rates of tripolar cups with that of standard cups in patients undergoing THA for femoral neck fractures. He analysed the dislocation rate in 56 consecutive patients operated with conventional (fixed-liner) cemented acetabular components to that of 42 consecutive patients operated with dual articulation acetabular components. In this series, all the patients were operated upon via posterior approach and were followed up to one year postoperatively. No dislocation was reported in the group with dual mobility compared to eight cases (14 %) of dislocation in the group with conventional fixed liners.
Guyen et al. [43], Langlais et al. [44], Hamadouche et al. [18], and Leider-Wackenheim et al. [12] retrospectively evaluated results of tripolar cups for management of instability after conventional primary THA. The cohorts of patients ranged from 47 to 82 cases and the mean follow-up period was two to eight years. Survival rate at five years was 94.5–98 % and the incidence of dislocation was 1–5.5 %. Of note, in all patients that had a dislocation, only a single episode of dislocation was reported. Complications included trochanteric non union (5.5 % in the study from Guyen et al. [43], where three of 54 THA were associated with preoperative non-union) and deep infection (3–5.5 %), all of which were managed with retention of the implants. Revision for aseptic loosening was required in 2 % of cases. Leider-Wackenheim et al. [12] described four cases (6.7 %) of iliopsoas irritation, which was successfully treated conservatively.
Finally, total hip replacement following tumour resections has been associated with a high risk of dislocation, largely due to loss of bony and soft-tissue structures. Philippeau et al. [16] retrospectively analysed 71 cases of dual mobility cups implanted following extensive tumour resections with a mean follow up of 3.3 years. In their series, dislocation occurred in seven cases (9.8 %), which was in the setting of extensive tumour resections that included removal of substantial acetabular bone stock and the hip stabilisers, in particular gluteus medius. Revision for acetabular loosening was performed in four cases (5.6 %) and there were nine cases of deep infection (12 %).
Conclusions
The rate of instability following THR increases with time, although the dislocation rate is considerably lower in short-term studies (1 % at one year) [1, 3, 45]. Berry et al. [1] have reported a cumulative long-term risk of dislocation after total hip arthroplasty up to 7 % at 25 years. This rate is about two to three times higher in revision surgery [3, 46, 47]. Furthermore, the incidence of dislocation is highest in the first year after arthroplasty and then continues at a relatively constant rate for the life of the arthroplasty [1].
The use of a dual mobility cup is an option to overcome the problem of instability after total hip replacement. However, long-term outcome data regarding its use is limited in the current literature. From our review, we found that there were significant complications after the use of first generation cups, which were mainly due to premature wear of the polyethylene, leading to early intraprosthetic dislocations [2, 9]. Fracture of the polyethylene was described in one case [36].
More recently, the long-term outcomes for second-generation dual-mobility cup have been more promising; however, the durability of the cups seems to be a concern. Recent modifications of the original implant design have aimed to improve the durability of the implant [9]. Such developments include mostly polyethylene manufacturing techniques (cross-linking) and improvements in metal cup fixation.
In the literature, the survival rates of primary total hip arthroplasty with dual mobility cups have been reported to be greater that 95 % at five years. This rate decreased significantly at 15 years, reaching around 80 % and dropping to 75 % at 20 years [13]. Those figures compare to data retrieved from national registries suggest revision risks of 5–20 % ten years following primary THA [48].
In cases of revision surgery for unstable THAs, use of the dual mobility cups has shown to have high survival rates of more than 94 % at five years, with a low incidence of recurrent dislocation [43, 44]. However, it is unclear whether this rate decreases with the length of follow-up. As such, data from large series with long follow-ups are mandatory to fully establish the eventual long-term benefit of tripolar cups.
Furthermore, the dual mobility cup has been shown to be beneficial in the context of tumour resection, with lower dislocation rates described in the literature [49–52]. Thus, this technique remains a therapeutic option in patients with high risk of dislocation following tumour resection. Nevertheless, we need to keep in mind the issue of long-term survival of dual mobility cups in young and active patients, whose life expectancy is to be significantly improved as a result of adjuvant treatments. However, due to the lack of robust long-term results with regard to wear and aseptic loosening, and the lack of clinical data with high levels of evidence, tripolar systems should be used with caution, particularly in young and active patients [40].
In summary, the tripolar cup, which was developed by Bousquet in the late 1970s, was innovative in hip arthroplasty. Since its first design, improvements have been adopted on the acetabular fixation system and the quality of the polyethylene. However, its effects on long-term implant survival remain to be assessed. Studies have shown a clear effect reducing the rate of dislocation in cases of primary THA, revision THA and in cases of periacetabular tumour resection. However, in view of the limited long-term data on tripolar systems and the concerns with regard to theoretical downsides (i.e. wear rates and aseptic loosening), such cups should be used with prudence, particularly in standard primary hip arthroplasty in patients with a long life expectancy.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Berry DJ, Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86-A:9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;33:927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 4.Pattyn C, Haan R, Kloeck A, Maele G, Smet K. Complications encountered with the use of constrained acetabular prostheses in total hip arthroplasty. J Arthroplasty. 2010;25:287–294. doi: 10.1016/j.arth.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 5.Fricka KB, Marshall A, Paprosky WG. Constrained liners in revision total hip arthroplasty: an overuse syndrome: in the affirmative. J Arthroplasty. 2006;21:121–125. doi: 10.1016/j.arth.2006.02.100. [DOI] [PubMed] [Google Scholar]
- 6.Williams JT, Jr, Ragland PS, Clarke S. Constrained components for the unstable hip following total hip arthroplasty: a literature review. Int Orthop. 2007;31:273–277. doi: 10.1007/s00264-006-0191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson MJ, Murray WR, Skinner HB. Constrained acetabular components. J Arthroplasty. 1994;9:17–23. doi: 10.1016/0883-5403(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 8.Schmalzried TP, Callaghan JJ. Wear in total hip and knee replacements. J Bone Joint Surg Am. 1999;81:115–136. doi: 10.2106/00004623-199901000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Vielpeau C, Lebel B, Ardouin L, Burdin G, Lautridou C. The dual mobility socket concept: experience with 668 cases. Int Orthop. 2011;35:225–230. doi: 10.1007/s00264-010-1156-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stulberg SD. Dual poly liner mobility optimizes wear and stability in THA: affirms. Orthopedics. 2011;34:e445–e448. doi: 10.3928/01477447-20110714-23. [DOI] [PubMed] [Google Scholar]
- 11.Mohammed R, Cnudde P (2011) Severe metallosis owing to intraprosthetic dislocation in a failed dual-mobility cup primary total hip arthroplasty. J Arthroplasty. doi:10.1016/j.arth.2010.11.019 [DOI] [PubMed]
- 12.Leiber-Wackenheim F, Brunschweiler B, Ehlinger M, Gabrion A, Mertl P. Treatment of recurrent THR dislocation using of a cementless dual-mobility cup: a 59 cases series with a mean 8 years' follow-up. Orthop Traumatol Surg Res. 2011;97:8–13. doi: 10.1016/j.otsr.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Boyer B, Philippot R, Geringer J, Farizon F (2011) Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop 36(3):511–518. doi:10.1007/s00264-011-1289-4 [DOI] [PMC free article] [PubMed]
- 14.Tarasevicius S, Busevicius M, Robertsson O, Wingstrand H. Dual mobility cup reduces dislocation rate after arthroplasty for femoral neck fracture. BMC Musculoskelet Disord. 2010;11:175. doi: 10.1186/1471-2474-11-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pineau V, Lebel B, Gouzy S, Dutheil JJ, Vielpeau C. Dual mobility hip arthroplasty wear measurement: experimental accuracy assessment using radiostereometric analysis (RSA) Orthop Traumatol Surg Res. 2010;96:609–615. doi: 10.1016/j.otsr.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 16.Philippeau JM, Durand JM, Carret JP, Leclercq S, Waast D, Gouin F. Dual mobility design socket use in preventing total hip replacement dislocation following tumor resection. Orthop Traumatol Surg Res. 2010;96:2–8. doi: 10.1016/j.otsr.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 17.Massin P, Besnier L. Acetabular revision using a press-fit dual mobility cup. Orthop Traumatol Surg Res. 2010;96:9–13. doi: 10.1016/j.otsr.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 18.Hamadouche M, Biau DJ, Huten D, Musset T, Gaucher F. The use of a cemented dual mobility socket to treat recurrent dislocation. Clin Orthop Relat Res. 2010;468:3248–3254. doi: 10.1007/s11999-010-1404-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coventry MB. Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am. 1985;67:832–841. [PubMed] [Google Scholar]
- 20.Guyen O, Chen QS, Bejui-Hugues J, Berry DJ, An KN. Unconstrained tripolar hip implants: effect on hip stability. Clin Orthop Relat Res. 2007;455:202–208. doi: 10.1097/01.blo.0000238796.59596.1f. [DOI] [PubMed] [Google Scholar]
- 21.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–288. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 22.Peter R, Lubbeke A, Stern R, Hoffmeyer P (2011) Cup size and risk of dislocation after primary total hip arthroplasty. J Arthroplasty. doi:10.1016/j.arth.2010.11.015 [DOI] [PubMed]
- 23.Jameson SS, Lees D, James P, Serrano-Pedraza I, Partington PF, Muller SD, Meek RM, Reed MR. Lower rates of dislocation with increased femoral head size after primary total hip replacement: a five-year analysis of NHS patients in England. J Bone Joint Surg Br. 2011;93:876–880. doi: 10.1302/0301-620X.93B7.26657. [DOI] [PubMed] [Google Scholar]
- 24.Berry DJ, Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 25.Sariali E, Lazennec JY, Khiami F, Catonne Y. Mathematical evaluation of jumping distance in total hip arthroplasty: influence of abduction angle, femoral head offset, and head diameter. Acta Orthop. 2009;80:277–282. doi: 10.3109/17453670902988378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kerboull L, Hamadouche M, Courpied JP, Kerboull M (2004) Long-term results of Charnley-Kerboull hip arthroplasty in patients younger than 50 years. Clin Orthop Relat Res:112–118 [DOI] [PubMed]
- 27.Dumbleton JH, Manley MT, Edidin AA. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002;17:649–661. doi: 10.1054/arth.2002.33664. [DOI] [PubMed] [Google Scholar]
- 28.Digas G, Karrholm J, Thanner J, Herberts P. 5-Year experience of highly cross-linked polyethylene in cemented and uncemented sockets: two randomized studies using radiostereometric analysis. Acta Orthop. 2007;78:746–754. doi: 10.1080/17453670710014518. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Rey E, Garcia-Cimbrelo E, Cruz-Pardos A, Ortega-Chamarro J. New polyethylenes in total hip replacement: a prospective, comparative clinical study of two types of liner. J Bone Joint Surg Br. 2008;90:149–153. doi: 10.1302/0301-620X.90B2.19887. [DOI] [PubMed] [Google Scholar]
- 30.Wroblewski BM. Direction and rate of socket wear in Charnley low-friction arthroplasty. J Bone Joint Surg Br. 1985;67:757–761. doi: 10.1302/0301-620X.67B5.4055876. [DOI] [PubMed] [Google Scholar]
- 31.Adam P, Farizon F, Fessy MH. Dual articulation retentive acetabular liners and wear: surface analysis of 40 retrieved polyethylene implants. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:627–636. doi: 10.1016/S0035-1040(05)84466-6. [DOI] [PubMed] [Google Scholar]
- 32.Schmalzried TP, Dorey FJ, McKellop H. The multifactorial nature of polyethylene wear in vivo. J Bone Joint Surg Am. 1998;80:1234–1242. doi: 10.2106/00004623-199808000-00018. [DOI] [PubMed] [Google Scholar]
- 33.Wroblewski BM (1986) 15–21-year results of the Charnley low-friction arthroplasty. Clin Orthop Relat Res:30–35 [PubMed]
- 34.Kim YS, Kim YH, Hwang KT, Choi IY (2012) The cartilage degeneration and joint motion of bipolar hemiarthroplasty. Int Orthop. doi:10.1007/s00264-012-1567-9 [DOI] [PMC free article] [PubMed]
- 35.Lazennec J, Ali H, Rousseau M, Hansen S (2006) All ceramic tripolar total hip arthroplasty: experimental data and clinical results. In: Benazzo F, Falez F, Dietrich M (eds) Ceramics in orthopaedics. Steinkopff, Darmstadt, pp 5–9
- 36.Farizon F, Lavison R, Azoulai JJ, Bousquet G. Results with a cementless alumina-coated cup with dual mobility. A twelve-year follow-up study. Int Orthop. 1998;22:219–224. doi: 10.1007/s002640050246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Massin P, Orain V, Philippot R, Farizon F, Fessy MH (2011) Fixation failures of dual mobility cups: a mid-term study of 2601 hip replacements. Clin Orthop Relat Res 470(7):1932–1940. doi:10.1007/s11999-011-2213-3 [DOI] [PMC free article] [PubMed]
- 38.Leclercq S, Benoit JY, Rosa JP, Euvrard P, Leteurtre C, Girardin P. Results of the evora dual-mobility socket after a minimum follow-up of five years. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:e17–e22. doi: 10.1016/j.rco.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 39.Adam P, Philippe R, Ehlinger M, Roche O, Bonnomet F, Mole D, Fessy MH. Dual mobility cups hip arthroplasty as a treatment for displaced fracture of the femoral neck in the elderly. A prospective, systematic, multicenter study with specific focus on postoperative dislocation. Orthop Traumatol Surg Res. 2012;98:296–300. doi: 10.1016/j.otsr.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 40.Lautridou C, Lebel B, Burdin G, Vielpeau C. Survival of the cementless bousquet dual mobility cup: minimum 15-year follow-up of 437 total hip arthroplasties. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:731–739. doi: 10.1016/j.rco.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 41.Philippot R, Adam P, Farizon F, Fessy MH, Bousquet G. Survival of cementless dual mobility sockets: ten-year follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2006;92:326–331. doi: 10.1016/S0035-1040(06)75762-2. [DOI] [PubMed] [Google Scholar]
- 42.Herberts P (2010) Swedish joint registry. Swedish Hip Arthroplasty Register, Sweden
- 43.Guyen O, Pibarot V, Vaz G, Chevillotte C, Bejui-Hugues J. Use of a dual mobility socket to manage total hip arthroplasty instability. Clin Orthop Relat Res. 2009;467:465–472. doi: 10.1007/s11999-008-0476-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Langlais FL, Ropars M, Gaucher F, Musset T, Chaix O. Dual mobility cemented cups have low dislocation rates in THA revisions. Clin Orthop Relat Res. 2008;466:389–395. doi: 10.1007/s11999-007-0047-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Philippot R, Adam P, Reckhaus M, Delangle F, Verdot FX, Curvale G, Farizon F. Prevention of dislocation in total hip revision surgery using a dual mobility design. Orthop Traumatol Surg Res. 2009;95:407–413. doi: 10.1016/j.otsr.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 46.Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23. doi: 10.1097/01.blo.0000218752.22613.78. [DOI] [PubMed] [Google Scholar]
- 47.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84-A:1788–1792. [PubMed] [Google Scholar]
- 48.Corbett KL, Losina E, Nti AA, Prokopetz JJ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: a systematic review. PLoS One. 2010;5:e13520. doi: 10.1371/journal.pone.0013520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zehr RJ, Enneking WF, Scarborough MT (1996) Allograft-prosthesis composite versus megaprosthesis in proximal femoral reconstruction. Clin Orthop Relat Res:207–223 [PubMed]
- 50.Cottias P, Jeanrot C, Vinh TS, Tomeno B, Anract P. Complications and functional evaluation of 17 saddle prostheses for resection of periacetabular tumors. J Surg Oncol. 2001;78:90–100. doi: 10.1002/jso.1127. [DOI] [PubMed] [Google Scholar]
- 51.Haentjens P, Neve W, Casteleyn PP, Opdecam P. Massive resection and prosthetic replacement for the treatment of metastases of the trochanteric and subtrochanteric femoral region bipolar arthroplasty versus total hip arthroplasty. Acta Orthop Belg. 1993;59(Suppl 1):367–371. [PubMed] [Google Scholar]
- 52.Masterson EL, Ferracini R, Griffin AM, Wunder JS, Bell RS. Capsular replacement with synthetic mesh: effectiveness in preventing postoperative dislocation after wide resection of proximal femoral tumors and prosthetic reconstruction. J Arthroplasty. 1998;13:860–866. doi: 10.1016/S0883-5403(98)90190-5. [DOI] [PubMed] [Google Scholar]
- 53.Philippot R, Farizon F, Camilleri JP, Boyer B, Derhi G, Bonnan J, Fessy MH, Lecuire F. Survival of cementless dual mobility socket with a mean 17 years follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:e23–e27. doi: 10.1016/j.rco.2007.10.013. [DOI] [PubMed] [Google Scholar]