Abstract
Purpose
The talonavicular joint is a central connection of the human foot. Symptomatic talonavicular arthritis can be adequately addressed by isolated talonavicular fusion. However, non-union remains a relevant clinical challenge to the orthopaedic surgeon. The aim of this study was to analyse the clinicoradiological outcome of talonavicular fusion using angle-stable mini-plates.
Methods
We performed 30 talonavicular fusions in 30 patients (12 male, 18 female) with a mean age of 58.8 years (range, 22–74) between 2005 and 2007. Osseous joint fusion was achieved using mono- and multidirectional angle-stable mini-plates. The patients followed a standardised immobilisation and weight bearing protocol. The mean postoperative follow up was 15.8 months (6.1–23.8).
Results
The American Orthopedic Foot and Ankle Society AOFAS score increased significantly from 31.7 (19–42) to 82.3 points (55–97) (p < 0.001). Neither age at operation nor gender influenced the score results significantly, while the aetiology of talonavicular degeneration showed a significant effect. Mean visual analogue scale (VAS) pain intensity (0–10) reduced from 8.6 to 1.7 (p < 0.001). Good or excellent results were achieved in 26 patients, while two patients reported fair and another two poor results. Complete osseous fusion was observed at a mean of 10.9 weeks (8–13) postoperatively.
Conclusions
For the treatment of talonavicular arthritis, the application of mono- and multidirectional angle-stable mini-plates provided a strong fixation that led to high union rates and good to excellent overall outcome.
Introduction
The talus is the central connecting element of the ankle, allowing a considerable amount of highly controlled movement, while distributing the resulting forces from standing and ambulation among the peritalar joints [1]. Previous studies have identified the pivotal biomechanical role of the talonavicular joint for the rearfoot [2]. Talonavicular joint destruction is found in a multitude of pathological processes, namely, primary osteoarthritis, rheumatoid arthritis and post-traumatic injury. Isolated talonavicular arthrodesis has been shown to provide satisfactory pain relief and to be an adequate measure to control the progression of the developement of flatfoot deformity [3]. However, the orthopaedic surgeon is confronted with a significant rate of osseous non-union after conventional screw or plate fixation [4, 5]. Importantly, angle-stable plates have been used in a wide range of osteosynthetic applications and have been reported to provide rigid fixation leading to reduced interfragmentary strain and high union rates [6]. Today, the industry provides a variety of angle-stable mini plates for foot surgery, though their potential clinical benefit has not yet been studied in depth.
Study evaluated the clinicoradiographic outcome of talonavicular arthrodesis using mono- and multidirectional angle-stable mini-plates.
Methods
Between October 2005 and May 2007, we prospectively enrolled 30 consecutive patients who were suffering from destruction of the talonavicular joint and were treated by talonavicular arthrodesis in a single high volume centre. In all patients, talonavicular arthrodesis was performed using multidirectional (=variable) (Königssee Implantate GmbH, Allendorf, Germany, n = 25) and monodirectional (Darco, Raisting, Germany, n = 5) angle-stable mini-plates (Fig. 1a and b). The joint capsule was opened from a medial longitudinal approach, the sclerotic articular surfaces were removed by using a chisel until bleeding spongious bone was visible. In six patients autologous spongious bone graft from the iliac crest was interpositioned. The decision to graft spongious bone was made by the surgeon intraoperatively. If an effortless reduction of the talonavicular joint could not be achieved graft was harvested from the iliac crest. Postoperatively, ankle and foot were immobiliss using a vacuum orthosis (OPED GmbH, Valley, Germany) for ten to 12 weeks with reduced weight bearing of approximately 20 kg for the first six weeks, full weight bearing in the vacoped-orthosis after six weeks. All patients were followed clinically at regular intervals and treated by a standard protocol, including physiotherapy, pain medication, daily low molecular heparin injections and protected weightbearing. Full weightbearing without orthosis was allowed after osseous consolidation was detected on plain X-ray films. All patients were assessed pre-operatively by clinical examination, plain X-ray and standardised questionnaires including a visual analogue scale (VAS) from 0 to 10. The average follow-up was 15.8 months (6.1–23.8). At follow-up, clinical examination, plain X-ray and standardised questionnaires were repeated. The American Orthopedic Foot and Ankle Society outcome (AOFAS) score was calculated to assess regional preoperative function and overall patient outcome [7]. The study protocol was approved by the local ethics committee.
Fig. 1.
a. Preoperative oblique X-ray showing advanced talonavicular joint destruction in a patient suffering from primary osteoarthritis. b. Oblique X-ray of the same patient six weeks postoperatively. Talonavicular fusion was performed using a variable angle-stable mini-plate
Statistical analysis was performed with GraphPad Prism 5 for windows (GraphPad Software, Inc., La Jolla, CA). Normally distributed values were analysed using Student’s t-test, otherwise Mann–Whitney Rank Sum test was applied. One-way analysis of variance was performed to compare the means of the subgroups. A p-value ≤ 0.05 was considered significant.
Results
There were 12 male and 18 female patients with an average age of 58.8 years (range, 22–74 years) who were treated with talonavicular fusion (21 right feet, 9 left feet). Of those, 16 patients suffered from primary osteoarthritis, four from posttraumatic destruction, four from rheumatoid arthritis, two from psoriatic arthritis and in three cases of peripheral neurological impairment resulted in joint instability and destruction. In one case, the procedure was done following non-union after talonavicular fusion for aseptic necrosis of the navicular bone. The mean length of hospital stay was 11 days (range, 7–17 days). Of the 30 fusions, 29 healed without the need for an additional operative procedure. In one case, non-union and subsequent plate fracture occurred. After revision surgery using autologous spongious iliac crest graft and a variable angle-stable mini-plate, osseous union was detectable ten weeks postoperatively. The average time to complete osseous integration was 10.9 weeks (range, 8–13 weeks). The mean preoperative AOFAS score improved significantly (see Table 1) from 31.7 points (range, 19–42 points) to 82.3 points (range, 55–97 points) postoperatively (p < 0.001). Mean subjective pain as assessed by the visual analogue scale (VAS) decreased from 8.6 (range, 5–10) to 1.7 (range, 0–7) postoperatively (p < 0.001) (Table 1).
Table 1.
Results
| Scoring | Preoperative (mean ± standard deviation) | Follow up (mean ± standard deviation) | P value |
|---|---|---|---|
| AOFAS score | 31.7 ± 7.3 | 82.3 ± 9.1 | < 0.001 (t-test) |
| Pain VAS (0–10) | 8.6 ± 1.0 | 1.7 ± 1.8 | < 0.001 (Mann–Whitney rank sum test) |
| Function VAS (0–10) | 6.3 ± 1.6 | 8.9 ± 1.7 | < 0.001 (Mann–Whitney rank sum test) |
AOFAS American Orthopedic Foot and Ankle Society, VAS visual analogue scale
Age 60 years or above at the time of operation (n = 19, mean age 66.2 years) had no statistical influence on overall subjective patient outcome, time to union (p = 0.5333), AOFAS (p = 0.2502) or VAS (p = 0.8527) when compared to the younger age group (n = 11, mean age 45.4 years).
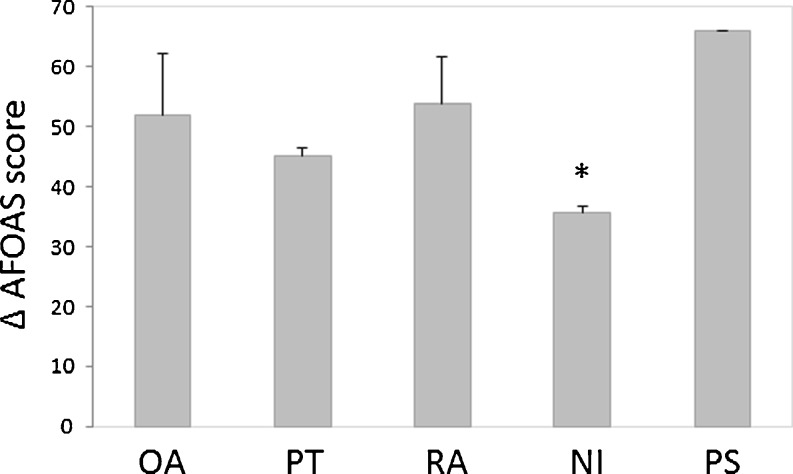
While the aetiology of talonavicular destruction had no significant effects on time to radiological osseous fusion (p = 0.42) or reduction of mean VAS score (p = 0.4721), the improvement in the AOFAS score differed significantly between the four subgroups (p = 0.0343) (Fig. 2).
Fig. 2.
Improvement of postoperative AOFAS score relative to the aetiology of talonavicular destruction. OA osteoarthritis, PT post-traumatic, RA rheumatoid arthritis, NI neurological impairment, PS psoriatic arthritis. *p < 0.05 as evaluated by analysis of variance
Spongious iliac crest crafts were used in six patients. Neither the time to osseous union (p = 0.3834) nor the improvement in mean AOFAS score (p = 0.6185) or VAS score (p = 0.5219) were significantly influenced by autologous bone grafting. Statistical analysis comparing the outcome of multi- and monodirectional angle-stable mini-plates revealed no superiority of one of the implants in terms of time to union (p = 0.3271), improvement of AOFAS score (p = 0.1286) or VAS score (p = 0.2670).
Discussion
Initially, isolated talonavicular fusion was described as an effective method to tread flatfoot deformity [8]. Later, the procedure was further developed and expanded to a wide variety of rearfoot pathologies. Review of the literature indicates that there are a large variety of osteosynthetic implants for the fusion of the talonavicular joint. Satisfactory outcome from screw arthrodesis [9], non angle-stable plates [10] and memory staples have been reported [11]. A recent report by Jarrell et al. compared the biomechanical properties of screw versus combined plate and screw fixation for talonavicular fusion [12]. Their results indicated a superiority of the plate over the sole use of screws. This finding has been echoed by other groups [13–15].
The isolated use of staples has been criticised, because of a potentially high rate of non unions [10].
This study is the first systematic analysis of the use of monodirectional angle-stable mini-plates and multidirectional angle stable mini-plates for talonavicular joint fusion. Our data show good overall patient outcome using angle-stable mini-plates, while providing excellent intraoperative flexibility during plate and screw positioning using multidirectional (= variable) angle-stable mini-plates.
Formerly, good to excellent results have been reported following talonavicular fusion with patient satisfaction rates above 90 % [16–18]. Our study reports an overall patient satisfaction rate of 93.3 % at the final evaluation. Of note, the aetiology of the talonavicular destruction had a significant influence on the overall functional outcome as assessed by the AOFAS score. Patients suffering from neurological impairment showed the lowest improvement in the AOFAS score, while time to union and VAS score showed no significant differences. The limited benefit following hind foot fusion in neuropathic conditions has already been observed by others [19]. While stabilising the rearfoot and the medial column of the neuropathic foot, the pre-existing impairment of the adaptive flexibility and rigidity during the gait cycle might be further enhanced by the fusion.
In one patient, non-union and resulting plate fracture occurred at seven months postoperatively. In another case radiographic evidence of plate fracture was noted at 16 months after the operation, while clear osseous union and an excellent functional and subjective outcome were noted. No further complications were noted (overall complication rate 10 %). Regarding the relevant non union rate after talonavicular arthrodesis of up to 37 % in historic reports [15], an osseous fusion rate of 97 % using angle stable mini plates appears to be promising.
Until today, the role of autologous bone grafting for hind foot fusions has not been systematically analysed. In our study spongious iliac crest bone grafts were used in six patients, while statistical analysis revealed no significant differences in terms of time to union, AOFAS score or patient satisfaction.
Subsequent development of osteoarthritis of the unfused adjacent joints following talonavicular arthrodesis has been reported to be a relevant clinical sequel. At the time of the last clinicoradiological evaluation, no case of adjacent osteoarthritis was detected. Here, the relatively short follow-up period might be critical [20].
Limitations of our study are the restricted follow-up period and the lack of a control group using established devices for talonavicular fusion.
Nevertheless, using the AOFAS score as a standardised outcome measurement and osseous fusion for assessing interfragmentary stability, the results of our study can be readily compared to previously published series.
Conclusion
Talonavicular fusion using variable and non-variable angle-stable mini-plates led to excellent short and midterm functional results in patients suffering from talonavicular joint damage. Autologous transplantation of spongious ileac crest grafts had no significant effect on overall outcome.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Ledoux WR, Sangeorzan BJ. Clinical biomechanics of the peritalar joint. Foot Ankle Clin. 2004;9:663–683. doi: 10.1016/j.fcl.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 2.Wulker N, Stukenborg C, Savory KM, Alfke D. Hindfoot motion after isolated and combined arthrodeses: measurements in anatomic specimens. Foot Ankle Int. 2000;21:921–927. doi: 10.1177/107110070002101106. [DOI] [PubMed] [Google Scholar]
- 3.Crevoisier X. The isolated talonavicular arthrodesis. Foot Ankle Clin. 2011;16:49–59. doi: 10.1016/j.fcl.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Easley ME, Trnka HJ, Schon LC, Myerson MS. Isolated subtalar arthrodesis. J Bone Joint Surg Am. 2000;82:613–624. doi: 10.2106/00004623-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Plaass C, Knupp M, Barg A, Hintermann B. Anterior double plating for rigid fixation of isolated tibiotalar arthrodesis. Foot Ankle Int. 2009;30:631–639. doi: 10.3113/FAI.2009.0631. [DOI] [PubMed] [Google Scholar]
- 6.Strauss EJ, Schwarzkopf R, Kummer F, Egol KA. The current status of locked plating: the good, the bad, and the ugly. J Orthop Trauma. 2008;22:479–486. doi: 10.1097/BOT.0b013e31817996d6. [DOI] [PubMed] [Google Scholar]
- 7.Button G, Pinney S. A meta-analysis of outcome rating scales in foot and ankle surgery: is there a valid, reliable, and responsive system? Foot Ankle Int. 2004;25:521–525. doi: 10.1177/107110070402500802. [DOI] [PubMed] [Google Scholar]
- 8.Soren A, Waugh TR. The historical evolution of arthrodesis of the foot. Int Orthop. 1980;4:3–11. doi: 10.1007/BF00266597. [DOI] [PubMed] [Google Scholar]
- 9.Zwipp H, Rammelt S, Endres T, Heineck J. High union rates and function scores at midterm followup with ankle arthrodesis using a four screw technique. Clin Orthop Relat Res. 2010;468:958–968. doi: 10.1007/s11999-009-1074-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rammelt S, Marti RK, Zwipp H. Arthrodesis of the talonavicular joint. Orthopade. 2006;35(4):428–434. doi: 10.1007/s00132-005-0868-8. [DOI] [PubMed] [Google Scholar]
- 11.Popelka S, Hromádka R, Vavrík P, Stursa P, Pokorný D, Jahoda D, Sosna A. Isolated talonavicular arthrodesis in patients with rheumatoid arthritis of the foot and tibialis posterior tendon dysfunction. BMC Musculoskelet Disord. 2010;11:38. doi: 10.1186/1471-2474-11-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jarrell SE, 3rd, Owen JR, Wayne JS, Adelaar RS. Biomechanical comparison of screw versus plate/screw construct for talonavicular fusion. Foot Ankle Int. 2009;30:150–156. doi: 10.3113/FAI.2009.0150. [DOI] [PubMed] [Google Scholar]
- 13.DeVries JG, Granata JD, Hyer CF. Fixation of first tarsometatarsal arthrodesis: a retrospective comparative cohort of two techniques. Foot Ankle Int. 2011;32:158–162. doi: 10.3113/FAI.2011.0158. [DOI] [PubMed] [Google Scholar]
- 14.Scranton PE, Coetzee JC, Carreira D. Arthrodesis of the first metatarsocuneiform joint: a comparative study of fixation methods. Foot Ankle Int. 2009;30:341–345. doi: 10.3113/FAI.2009.0341. [DOI] [PubMed] [Google Scholar]
- 15.Moraes Barros Fucs PM, Svartman C, Assumpção RM, Yamada HH, Simis SD. Surgical technique: medial column arthrodesis in rigid spastic planovalgus feet. Clin Orthop Relat Res. 2012;470:1334–1343. doi: 10.1007/s11999-011-2185-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diezi C, Favre P, Vienne P. Primary isolated subtalar arthrodesis: outcome after 2 to 5 years followup. Foot Ankle Int. 2008;29:1195–1202. doi: 10.3113/FAI.2008.1195. [DOI] [PubMed] [Google Scholar]
- 17.Chen CH, Huang PJ, Chen TB, Cheng YM, Lin SY, Chiang HC, Chen LC. Isolated talonavicular arthrodesis for talonavicular arthritis. Foot Ankle Int. 2001;22:633–636. doi: 10.1177/107110070102200803. [DOI] [PubMed] [Google Scholar]
- 18.Harper MC. Talonavicular arthrodesis for the acquired flatfoot in the adult. Clin Orthop Relat Res. 1999;365:65–68. doi: 10.1097/00003086-199908000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Papa J, Myerson M, Girard P. Salvage, with arthrodesis, in intractable diabetic neuropathic arthropathy of the foot and ankle. J Bone Joint Surg Am. 1993;75:1056–1066. doi: 10.2106/00004623-199307000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Harper MC, Tisdel CL. Talonavicular arthrodesis for the painful adult acquired flatfoot. Foot Ankle Int. 1996;17:658–661. doi: 10.1177/107110079601701102. [DOI] [PubMed] [Google Scholar]