Abstract
Purpose
We conducted a systematic review of the literature in order to take stock of hip resurfacing according to the principle of “evidence based medicine”. Our main objective was to compare the rate of revision of resurfacing implants with survival limits set by the National Institute of Clinical Excellence (NICE).
Methods
A systematic review was undertaken of all published (Medline, Cochrane, EMBASE) literature research databases up to July 2012 as recommended by the PRISMA statement. Data extraction focused on functional outcomes, complications and survival rates. The survival rates of implants were analysed according to the mean of the series in comparison to the NICE criteria.
Results
Fifty-three studies were identified and included 26,456 cases with an average of 499.17 ± 856.7 (range, 38–5000) cases per study. The median survival was 95.57 % ± 3.7 % (range, 84–100). The percentage of studies which satisfied the criteria set by NICE was 69.8 %. In terms of cumulative revision rates pondered by the number of implants, BHR®, Conserve Plus® and Cormet® showed the best results. The mean postoperative score was 91.2 ± 7.72 (range, 68.3–98.6). There was no statistically significant difference between implants in terms of functional outcomes.
Conclusion
On the basis of the current evidence base, this review of the literature emphasises the importance of certain parameters that can improve the results of resurfacing. The type of implant seems to play an important role as does patient selection.
Introduction
After a period of popularity, hip resurfacing has seen a number of indications to be decreasing [1]. It is currently the subject of numerous concerns with regards to the presence of metal ions in the blood, even if there is no conclusive evidence of a carcinogenic effect [2]. Furthermore, many publications seem to show excellent results. We conducted a systematic review of the literature in order to take stock of this surgical technique according to the principle of “evidence based medicine.”
Our main objective was to compare the rate of revision of resurfacing implants with survival limits set by the National Institute of Clinical Excellence (NICE) (maximum of 10 % at ten years), being part of the National Health System (NHS) in England and Wales [3–5]. The secondary objectives were to evaluate the functional outcome and complications associated with hip resurfacing as well as differences between these implants.
Materials and methods
The research was conducted on July 14, 2012 using the Cochrane databases, EMBASE and MEDLINE as recommended by The PRISMA statement [6]. The electronic search included articles published until 25 July 2012. The following terms used the joints “AND”, “NOT” and “OR”: hips, femur head, femoral head, femur neck, femoral neck, resurfac* outcome, follow-up, FU, prosthesis failure, pseudotumor, pseudotumour, mechanical stress, gait, patient satisfaction, activity, activities, surviv* and risk factors. All titles and abstracts were reviewed by a single observer, and for studies meeting eligibility criteria the full article was obtained. The reference lists of meta-analysis and systematic reviews of the literature were examined to avoid missing studies not identified by the search. The inclusion criteria were: publication in English and studies reporting survival or revision of the implant with a minimum of at least six-months follow up. Exclusion criteria were: studies on hemi-arthroplasty, studies reporting results after revision of a resurfacing, retrospective studies on implant failures, technical note type studies, studies reporting only laboratory results, histological studies, in-vitro simulation study, bioengineering studies, radiological studies, studies of national registries, and clinical case studies of peri-prosthetic bone density. If articles described the same series of patients, we included the most recently published series with the largest number of patient population. The criteria for inclusion/exclusion was controlled by two different observers with the inclusion of a third in case of disagreement. Data extraction focused on the type of prosthesis, the design of the study, the baseline characteristics of patients, the mean follow-up, functional scores, survival rates, and the type and number of complications. Functional scores were standardised as far as possible on a scale of 0 to 100, with 100 representing the best possible functional outcome. The survival rate of implants was analysed according with respect to the mean of the series and compared with the NICE criteria. Quality of studies, in terms of level of evidence, was judged using the GRADE evaluation system (Grading of Recommendations Assessment, Development and Evaluations) classifying the quality of education in high, moderate, low and very low [7].
Results
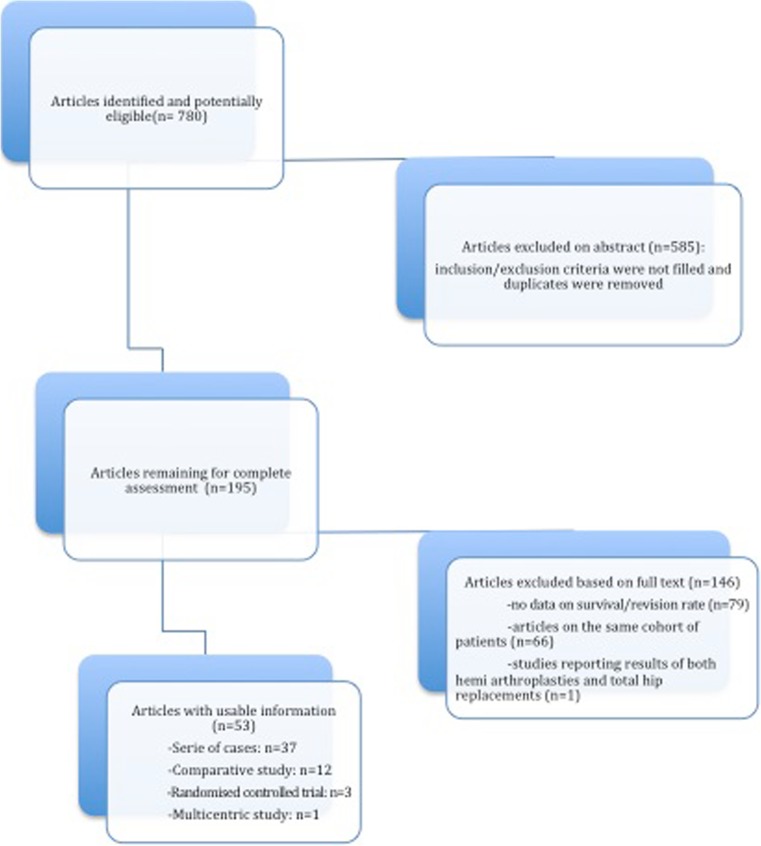
Research has revealed 780 citations published between 1 January 2005 and 14 July 2012. The number of studies identified according to the criteria for inclusion/exclusion was 53 (Fig. 1).
Fig. 1.
Flow chart of the PRISMA procedure of systematic review of the literature
Six studies examined the ASR Hip Resurfacing® implant (DePuy Orthopaedics Inc., Warsaw, Indiana), 22 the BHR implant® (Smith & Nephew Inc., Memphis, Tennessee), 11 the Conserve Plus® implant (Wright Medical Technology Inc, Arlington, Tennessee), five reviewed the Cormet 2000® implant (Corin Group PLC, Cirencester, United Kingdom) and four examined the Durom® implant (Zimmer, Warsaw, Indiana). One study reported the results of both BHR® and ASR® implants. Another study described the use of both the McMinn implant® (Corin Group PLC) and BHR® implant and another described only the second generation McMinn implant® (McMinn hybrid resurfacing; Corin Group PLC) which was only in use around 1996. One study compared the BHR® implant to the Recap® implant (Biomet Inc., Warsaw, Indiana). The data presented only six of the 11 resurfacing devices currently on the market. We were not able to identify studies that met our inclusion/exclusion for ACCIS® implants (Implantcast GmbH, Buxtehude, Germany), Adept® (Finsbury Orthopaedics), EskaBionik® (Eska Implants, Lübeck, Germany), Icon® (International Orthopaedics, Geisingen, Germany), and Mitch® (Stryker, Kalamazoo, Michigan).
Three randomised clinical trials and eight comparative studies compared the results of resurfacing implants to conventional total hip arthroplasty. The average survival rate for resurfacing implants was 94.84 % ± 4.7 (range, 89.1–100) and functional scores were significantly better for them in all studies. The mean duration of follow-up for the majority of these studies was five years. The study by Baker et al. [8] reported a mean follow-up of nine years (range, 8.2–10.3) for the resurfacing group (BHR®) and 10.7 years (range, 7.5– 14.5 ) for the total hip arthroplasty group (THA). A randomised clinical trial had a mean follow-up of 4.7 years for both groups (Durom®).
Only two series directly compared the results of two different resurfacing implants. One study compared the results of 29 patients who underwent bilateral resurfacings, with a BHR® implant on one side and a ReCap® implant on the contralateral side. This study did not show any revision of either implants at a mean follow up of 4.8 years for the BHR® implant and 1.4 years for the ReCap® implant. Another study analysed a prospective series of 660 procedures with BHR® implants, ASR® and ASR® THA implants. This study found that 17 patients needed a revision (ASR® implant in all cases). The revision rate was 0 % for the BHR® implant, 3.2 % for ASR® and 6 % for THA® ASR. Steiger et al. [9] found similar results. The cumulative revision rate at five years was 10.9 % (95 % CI, 8.7–13.6) with the ASR implant and 4 % (95 % CI, 3.7–4.5) for other resurfacing implants. The cumulative revision rate due to metallosis was 1.7 % (95 % CI, 0.9–3.1) with the ASR® implant against 0.3 % (95 % CI, 0.2–0.5) for other implants.
Thirty-seven studies reported single arm results in terms of survival/revision for the different resurfacing implants (Table 1).
Table 1.
Study results
| Authors | Study design | Implant | Number of hips | Percent (%) males | Mean age | % OA primary/ OA secondary/Other | Mean follow-up (years) | Percent (%) lost to follow-up | Number of revisions | Survival rate % (95 % CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| Amstutz et al. [10] | Series of cases | Conserve plus | 1107 | 74 | 50 | NS | 6.8 | 0.2 | 44 | 96 |
| Aulakh et al. [11] | Series of cases | BHR | 202 | 75 | 42 | 50/0/50 | 7.5 | 0 | 6 | 97.7 AVN; 95 OA |
| Baker et al. [8] | Comparative study BHR vs THA | BHR | 54 BHR vs 54 THA | 74 | 50 | 100/0/0 | 9 | NR | 5 BHR vs 9 THA | NR |
| Beaulé et al. [12] | Series of cases | Conserve plus | 116 | 81 | 47 | 81/9/10 | 3.2 | 1.9 | 2 | 98.1 |
| Bergeron et al. [13] | Series of cases | ASR | 228 | 80 | 54 | 97/0/3 | 4.6 | 3 | 8 | 94.8 |
| Bose et al. [14] | Series of cases | BHR | 96 | 84 | 39 | 0/100/0 | 5.4 | 0 | 3 | 95.4 |
| Carrothers et al. [15] | Multicentric study | BHR | 5000 | 67 | 53 | NS | 7.1 | NR | 182 | 96.3 |
| Costa et al. [16] | Comparative study Cormet vs THA | Cormet | 73 Cormet vs 137 THA | 86 (cormet) vs 47(THA) | 53 | NS | 2.4 | NR | 0 Cormet vs 3 THA | NR |
| Daniel et al. [17] | Series of cases | McMinn et BHR | 446 | 79 | 48 | 100/0/0 | 3.3 | 0 | 1 | 99.8 |
| Daniel et al. [18] | Series of cases | McMinn 2nde generation | 184 | 59 | 54 | 82/0/18 | 10.5 | 0.5 | 30 | 84 |
| De Smet et al. [19] | Series of cases | BHR | 252 | 69 | 50 | 81/6/13 | 5 | 1.5 | 3 | 98.9 |
| De Steiger et al. [9] | Comparative study ASR vs THA | ASR | 1167 ASR | 95 | 53 | NR | 5 | NR | 89.1 | |
| Della Valle et al. [20] | Series of cases | BHR | 537 | 71 | 52 | 89/6/5 | 0.87 | NR | 14 | NR |
| Delport et al. [21] | Comparative study BHR vs Recap | BHR et Recap | 56 | 82 | 52 | NS | 4.8 | NR | 0 | NR |
| Fowble et al. [22] | Comparative study Conserve plus vs THA | Conserve plus | 50 Conserve plus vs 44 THA | 62 | 50 | 98/1/1 | 3.2 | NR | 1 Conserve plus vs 0 THA | NR |
| Giannini et al. [23] | Series of cases | BHR | 350 | 52 | 51 | 52/22/26 | 2 | NS | 4 | 98.8 |
| Gravius et al. [24] | Series of cases | Durom | 82 | 56 | 53 | 93/7/0 | 2.4 | 2.4 | 2 | 97.6 |
| Gross et al. [25] | Series of cases | Cormet | 100 | 8 | NR | 21 | 93 | |||
| Heilpern et al. [26] | Series of cases | BHR | 113 | 58 | 54 | 88/4/8 | 5 | 3 | 4 | 96.3 (92.8–99.8) |
| Hing et al. [27] | Series of cases | BHR | 230 | 66 | 52 | NS | 5 | 0.5 | 2 | 97.8 (97.1–100) |
| Hulst et al. [28] | Series of cases | Conserve plus | 643 | 67 | 49 | 65/15/20 | 10.4 | NR | 45 | 98.3 |
| Jameson et al. [29] | Series of cases | ASR | 214 | 60 | 56 | 68/5/27 | 3.6 | 0 | 12 | 93 (80–98) |
| Khan et al. [30] | Series of cases | BHR | 679 | 60 | 51 | NS | 6 | 2 | 29 | 95.7 (94.4–97.4) |
| Killampalli et al. [31] | Series of cases | Cormet | 100 | 61 | 56 | 97/1/2 | 5 | 0 | 0 | 100 |
| Kim et al. [32] | Series of cases | Conserve plus | 200 | 78 | 49 | 86/4/10 | 2.6 | 0 | 14 | 93 |
| Klein et al. [33] | Series of cases | ASR | 115 | 47 | 58 | 100/0/0 | 1 | 0 | 13 | 88.7 |
| Langton et al. [34] | Comparative study BHR vs ASR | BHR et ASR | 155 BHR vs 505 ASR | 54 | 56 | NS | 2.9 | NR | 17 ASR vs 0 BHR | NR |
| Larbpaiboonpong et al. [35] | Series of cases | BHR | 40 | 58 | 41.3 | 35/52/13 | 1.4 | 0 | 1 | 97.5 |
| Lei et al. [36] | Series of cases | Durom | 90 | 52 | 47 | 50/0/50 | 2.3 | 0 | 1 | 98.9 |
| Mackenzie et al. [37] | Comparative study BHR vs THA | BHR | 499 | 75.5 | 49.1 | 100/0/0 | 2 | 0 | 0 | 100 |
| Madadi et al. [38] | Comparative study ON vs OA | Cormet | 52 | 52 | 35 | 50/0/50 | 3.4 | NR | 6 | 88.4 |
| Madhu et al. [39] | Series of cases | BHR | 117 | 58 | 54 | 56/44/0 | 7 | 1 | 8 | 91.5 (85.4–97.6) |
| Malhotra et al. [40] | Series of cases | ASR | 32 | 70 | 33 | 0/0/100 | 3.6 | 0 | 1 | 96.8 |
| Marker et al. [41] | Series of cases | Conserve plus | 361 | 71 | 50 | 74/15/11 | 4.9 | NR | 23 | 93.6 |
| Marulanda et al. [42] | Series of cases | BHR | 230 | 73 | 55 | 87/0/13 | 1.3 | NS | 3 | 98.7 |
| McAndrew et al. [43] | Series of cases | BHR | 180 | NS | 56 | 94/0/6 | 2 | 0 | 3 | 98.3 |
| McBryde [44] | Series of cases | BHR | 2123 | 62 | 55 | 100/0/0 | 3.46 | 0 | 48 | 97.5 (96.3–98.3) |
| McMinn et al. [45] | Series of cases | BHR | 3095 | NS | 53 | 8 | 0 | 68 | 98 | |
| Mont et al. [46] | Comparative study Conserve plus vs THA | Conserve plus | 54 Conserve plus vs 54 THA | 75 | 52 | 100/0/0 | 3.5 | 0 | 2 Conserve plus vs 2 THA | NR |
| Mont et al. [47] | Series of cases | Conserve plus | 1016 | 28 | 50 | 77/11/12 | 2.8 | 6.3 | 54 | 94.2 (90–96.7) |
| Naal et al. [48] | Series of cases | Durom | 100 | 66 | 52 | 79/6/15 | 5 | NR | 11 | 88.2 |
| Ollivere et al. [49] | Series of cases | BHR | 463 | 66 | 56 | NS | 5 | 0.6 | 13 | 95.8 (94.1–96.8) |
| Sandiford et al. [50] | Comparative study BHR vs THA | BHR | 141 BHR vs 141 THA | 66 | 54 | 100/0/0 | 1.6 | NS | 0 | NS |
| Siebel et al. [51] | Series of cases | ASR | 300 | 64 | 57 | NS | 0.6 | 0 | 8 | 97.2 |
| Smolders et al. [52] | Clinical randomised trial | Conserve plus | 38 conserve plus vs 33 THA | 55 | 58 | 90/0/10 | 1.7 | NS | 1 Conserve plus vs 2 THA | NS |
| Steffen et al. [53] | Series of cases | BHR | 610 | 59 | 52 | 85/9/6 | 7 | 0.33 | 23 | 95 (95.3–99.2) |
| Stulberg et al. [54] | Series of cases | Cormet | 337 | 68 | 50 | 86/0/14 | 2 | 8.3 | 24 | 92.9 |
| Swank and Alkire [55] | Comparative study BHR vs THA | BHR | 128 BHR vs 106 THA | 62 | 51 | 71/5/24 | 1 | 0 | 2 BHR vs 0 THA | 98.1 |
| Takamura et al. [56] | Comparative study | Conserve plus | 500 | 63 | 48 | 63/18/19 | 8 | NR | 34 without FNN vs 7 with FNN | 86.7 with FNN vs93.6 without FNN |
| Treacy et al. [57] | Series of cases | BHR | 144 | 55 | 100/0/0 | 3.5 | 10 | 48 | 97.5 (96.3–98.3) | |
| Vendittoli et al. [58] | Randomised controlled trial | Durom | 109 Durom vs 100 THA | 63 | 49 | 31/9/60 | 4.7 | 0 | 4 vs 2 | 96.3 |
| Wang et al. [59] | Randomised controlled trial | Conserve plus | 37 Conserve vs 39 THA | 14 | 45.7 | 0/0/100 | 4.9 | 0 | 0 | 100 |
| Witzleb et al. [60] | Series of cases | BHR | 300 | 57 | 49 | 19/63/18 | 2 | 0.7 | 6 | 98 |
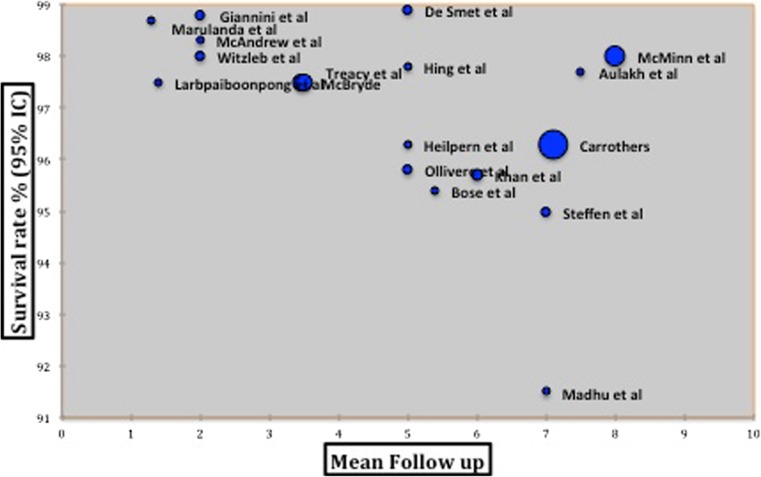
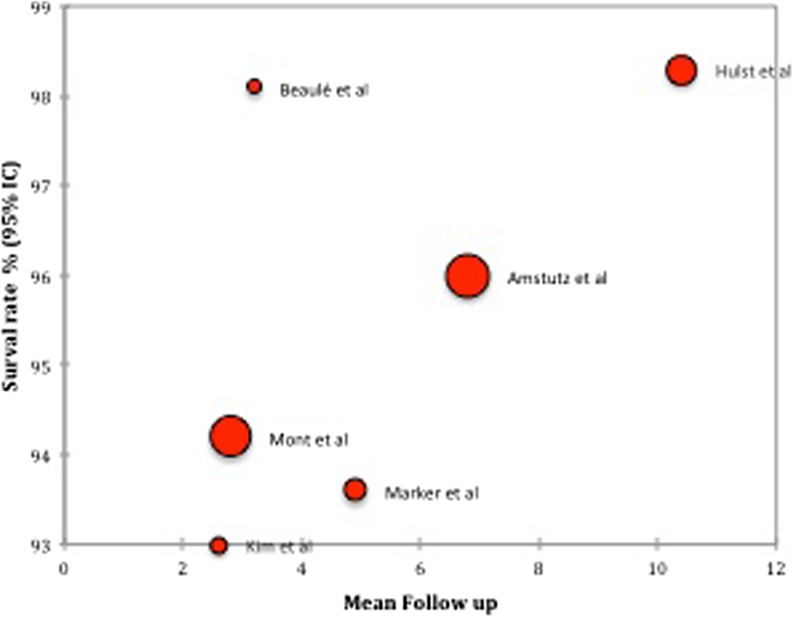
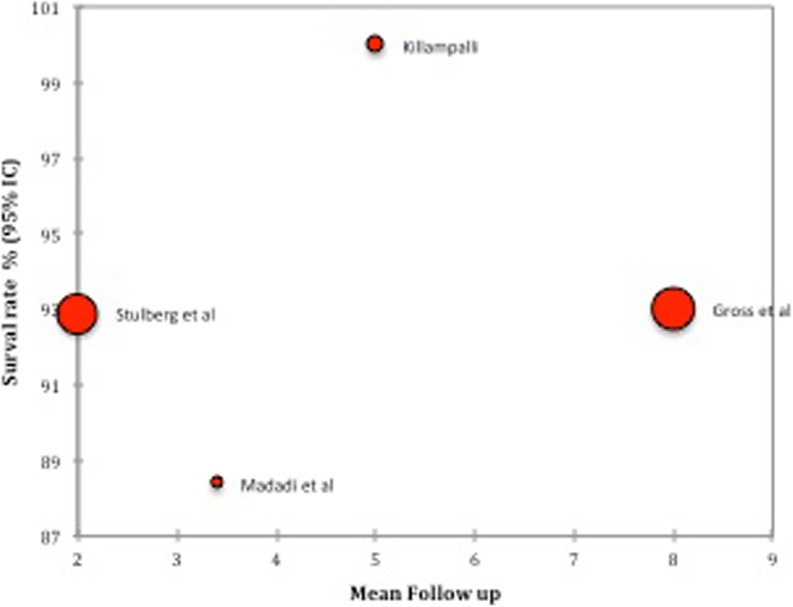
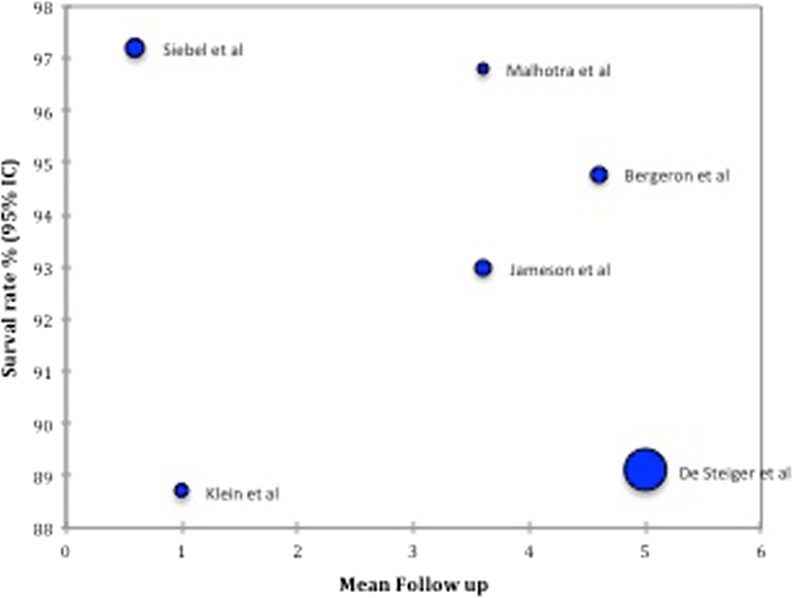
Of all the studies, the total number of resurfacing performed was 26,456 and the average number of cases per study was 499.17 ± 856.7 (range, 38–5000). The mean follow up was 4.3 ± 2.54 (range, 0.6–10.5) years. The average age of patients was 50.75 years ±5.19 (range, 35–58). The percentage of males per study was 64.73 % ± 13.55 (range, 28–95). The median survival was 95.57 % ±3.7 (range, 84–100). The percentage of studies which satisfied the criteria set by NICE was 69.8 %. In terms of cumulative revision rates pondered by the number of implants BHR®, Conserve Plus®, Cormet® showed the best results (Figs. 2, 3, 4, and 5).
Fig. 2.
Survival rate for the BHR implant
Fig. 3.
Survival rate for implant Conserve Plus
Fig. 4.
Survival rate for implant Cormet
Fig. 5.
Survival rate for the ASR implant
The details of the functional results for each study are reported in Table 2. The mean postoperative score was 91.2 ± 7.72 (range, 68.3–98.6). There was no statistically significant difference between implants in terms of functional outcomes.
Table 2.
Functional results
| Authors | Implant | Number of hips | Functional score | Preoperative | Postoperative |
|---|---|---|---|---|---|
| Amstutz et al. [10] | Conserve plus | 1107 | UCLA | 48 | 86.5 |
| Aulakh et al. [11] | BHR | 202 | HHS | 62 ON vs 58 OA | 96 ON vs 95.8 OA |
| Baker et al. [8] | BHR | 108 | OXFORD | ||
| Beaulé et al. [12] | Conserve plus | 116 | HHS | 53.1 | 90.1 |
| Bergeron et al. [13] | ASR | 228 | HHS | 46.6 | 91 |
| Bose et al. [14] | BHR | 96 | UCLA | NR | 68.6 |
| Carrothers et al. [15] | BHR | 5000 | HHS | NR | 96 |
| Costa et al. [16] | Cormet | 73 | NR | NR | NR |
| Daniel et al. [17] | McMinn and BHR | 446 | OXFORD | NR | 77.5 |
| Daniel et al. [18] | McMinn 2nd generation | 184 | OXFORD | NR | 68.3 |
| De Smet et al. [19] | BHR | 252 | HHS | NR | 97.2 |
| De Steiger et al. [9] | ASR | 1167 | NR | NR | NR |
| Della Valle et al. [20] | BHR | 537 | NR | NR | NR |
| Delport et al. [21] | BHR and Recap | 56 | HHS | 45 | 96.3 |
| Fowble et al. [22] | Conserve plus | 50 | HHS | 45 | 97 |
| Giannini et al. [23] | BHR | 350 | HHS | 57 | 98.6 |
| Gravius et al. [24] | Durom | 82 | HHS | 40.1 | 94.6 |
| Gross et al. [25] | Cormet | 373 | HHS | 57 | 96 |
| Heilpern et al. [26] | BHR | 113 | HHS | NR | 96.4 |
| Hing et al. [27] | BHR | 230 | HHS | 62.2 | 95.2 |
| Hulst et al. [28] | Conserve plus | 643 | NR | NR | NR |
| Jameson et al. [29] | ASR | 214 | HHS | 51.3 | 94.5 |
| Khan et al. [30] | BHR | 679 | HHS | 47 | 95 |
| Killampalli et al. [31] | Cormet | 100 | OXFORD | 37.5 | 89.6 |
| Kim et al. [32] | Conserve plus | 200 | HHS | 55.8 | 92.1 |
| Klein et al. [33] | ASR | 115 | HHS | 59 | 96 |
| Langton et al. [34] | BHR and ASR | 660 | HHS | NR | 94 ASR vs 97 BHR vs 76 ASR THA |
| Larbpaiboonpong et al. [35] | BHR | 40 | HHS | 35.1 | 96.4 |
| Lei et al. [36] | Durom | 90 | HHS | 57 | 93 |
| Mackenzie et al. [37] | BHR | 499 | WOMAC | 49.9 BHR vs 42.3 THA | 91.9 BHR vs 87.1 THA |
| Madadi et al. [38] | Cormet | 52 | HHS | NR | 96 |
| Madhu et al. [39] | BHR | 117 | HHS | NR | 84.4 |
| Malhotra et al. [40] | ASR | 32 | HHS | 39.6 | 88.4 |
| Marker et al. [41] | Conserve plus | 361 | NR | NR | NR |
| Marulanda et al. [42] | BHR | 230 | OXFORD | 27 | 78 |
| McAndrew et al. [43] | BHR | 180 | HHS | 44 | 72 |
| McBryde [44] | BHR | 2123 | NR | NR | NR |
| McMinn et al. [45] | BHR | 3095 | OXFORD | NR | 97.9 (13) |
| Mont et al. [46] | Conserve plus | 54 | HHS | 52 | 90 |
| Mont et al. [47] | Conserve plus | 1016 | HHS | NR | 93.1 |
| Naal et al. [48] | Durom | 100 | HHS | NR | 94.7 |
| Ollivere et al. [49] | BHR | 463 | HHS | NR | NR |
| Sandiford et al. [50] | BHR | 141 | HHS | 54.1 HR vs 46.4 THA | 96.8 HR vs 95.8 THA |
| Siebel et al. [51] | ASR | 300 | HHS | 44 | 89 |
| Smolders et al. [52] | Conserve plus | 38 | UCLA | NR | 80 HR vs 70 THA |
| Steffen et al. [53] | BHR | 610 | HHS | NR | 93.1 |
| Stulberg et al. [54] | Cormet | 337 | HHS | 50.1 | 96.7 |
| Swank and Alkire [55] | BHR | 128 | HHS | 49 | 96 |
| Takamura et al. [56] | Conserve plus | 500 | UCLA | ||
| Treacy et al. [57] | BHR | 2123 | OXFORD | 34.5 | 95.8 |
| Vendittoli et al. [58] | Durom | 109 | WOMAC | 45.1 | 90.6 |
| Wang et al. [59] | Conserve plus | 37 | HHS | 35.4 HR vs 35.9 THA | 94.5 HR vs 95.1 THA |
| Witzleb et al. [60] | BHR | 300 | HHS | 51 | 96 |
UCLA UCLA activity score, HHS Harris hip score, OXFORD Oxford hip score, NR not reported, WOMAC Western Ontario McMaster osteo-arthritis index
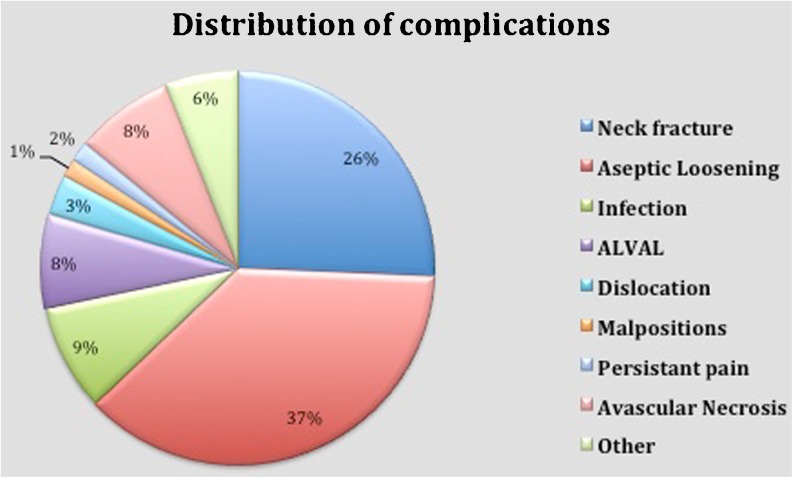
The revision rate was 4.4 % if we considered all cases in these published series. The most frequent complications (Table 3; Fig. 6) were aseptic loosening 33.5 %, followed by femoral fractures.
Table 3.
Complications
| Authors | Implant | Number of hips | Number of revisions | Neck fracture | Aseptic loosening | Infection | ALVAL | Dislocation | Malpositions | Persistent pain | Avascular necrosis | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amstutz et al. [10] | Conserve plus | 1107 | 44 | 9 | 26 | 2 | 0 | 1 | 0 | 0 | 0 | 6 |
| Aulakh et al. [11] | BHR | 202 | 6 | 3 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| Baker et al. [8] | BHR | 108 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 |
| Beaulé et al. [12] | Conserve plus | 116 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Bergeron et al. [13] | ASR | 228 | 8 | 8 | 1 | 1 | 5 | 0 | 0 | 0 | 1 | 0 |
| Bose et al. [14] | BHR | 96 | 3 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 0 |
| Carrothers et al. [15] | BHR | 5000 | 182 | 54 | 56 | 17 | 15 | 5 | 3 | 0 | 30 | 2 |
| Costa et al. [16] | Cormet | 73 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Daniel et al. [17] | McMinn and BHR | 446 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Daniel et al. [18] | McMinn 2nd generation | 184 | 30 | 0 | 29 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| De Smet et al. [19] | BHR | 252 | 3 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| De Steiger et al. [9] | ASR | 1167 | 210 | 19 | 92 | 42 | 26 | 15 | 0 | 0 | 0 | 16 |
| Della Valle et al. [20] | BHR | 537 | 14 | 10 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
| Delport et al. [21] | BHR and Recap | 56 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Fowble et al. [22] | Conserve plus | 50 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Giannini et al. [23] | BHR | 350 | 4 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Gravius et al. [24] | Durom | 82 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Gross et al. [25] | Cormet | 373 | 21 | 5 | 12 | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| Heilpern et al. [26] | BHR | 113 | 4 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Hing et al. [27] | BHR | 230 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Hulst et al. [28] | Conserve plus | 643 | 45 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Jameson et al. [29] | ASR | 214 | 12 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 |
| Khan et al. [30] | BHR | 679 | 29 | 11 | 14 | 3 | 1 | 0 | 0 | 0 | 0 | 0 |
| Killampalli et al. [31] | Cormet | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Kim et al. [32] | Conserve plus | 200 | 14 | 2 | 11 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Klein et al. [33] | ASR | 115 | 13 | 4 | 3 | 0 | 0 | 0 | 5 | 1 | 0 | 0 |
| Langton et al. [34] | BHR and ASR | 660 | 17 | 1 | 0 | 0 | 13 | 0 | 0 | 0 | 0 | 12 |
| Larbpaiboonpong et al. [35] | BHR | 40 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Lei et al. [36] | Durom | 90 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mackenzie et al. [37] | BHR | 499 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Madadi et al. [38] | Cormet | 52 | 6 | 3 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Madhu et al. [39] | BHR | 117 | 8 | 5 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 0 |
| Malhotra et al. [40] | ASR | 32 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Marker et al. [41] | Conserve plus | 361 | 23 | 13 | 6 | 0 | 0 | 0 | 2 | 0 | 0 | 2 |
| Marulanda et al. [42] | BHR | 230 | 3 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| McAndrew et al. [43] | BHR | 180 | 3 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| McBryde [44] | BHR | 2123 | 48 | 13 | 9 | 4 | 0 | 0 | 2 | 7 | 6 | 3 |
| McMinn et al. [45] | BHR | 3095 | 68 | 12 | 2 | 14 | 10 | 2 | 0 | 2 | 25 | 1 |
| Mont et al. [46] | Conserve plus | 54 | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mont et al. [47] | Conserve plus | 1016 | 54 | 27 | 24 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Naal et al. [48] | Durom | 100 | 11 | 4 | 3 | 0 | 0 | 0 | 2 | 2 | 0 | 0 |
| Ollivere et al. [49] | BHR | 463 | 13 | 3 | 0 | 1 | 7 | 2 | 0 | 0 | 0 | 0 |
| Sandiford et al. [50] | BHR | 141 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Siebel et al. [51] | ASR | 300 | 8 | 5 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Smolders et al. [52] | Conserve plus | 38 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Steffen et al. [53] | BHR | 610 | 23 | 12 | 4 | 2 | 0 | 2 | 0 | 2 | 0 | 1 |
| Stulberg et al. [54] | Cormet | 337 | 24 | 8 | 15 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Swank and Alkire [55] | BHR | 128 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Takamura et al. [56] | Conserve plus | 500 | 41 | 6 | 26 | 1 | 0 | 1 | 1 | 0 | 0 | 4 |
| Treacy et al. [57] | BHR | 2123 | 48 | 1 | 1 | 3 | 0 | 1 | 0 | 0 | 3 | 1 |
| Vendittoli et al. [58] | Durom | 109 | 4 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Wang et al. [59] | Conserve plus | 37 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Witzleb et al. [60] | BHR | 300 | 6 | 1 | 1 | 2 | 0 | 0 | 1 | 1 | 0 | 0 |
Fig. 6.
Distribution of complications
According to the GRADE recommendation system, the quality of these studies in terms of level of evidence was very low except for a randomised clinical trial where the quality of results reported was low [7]. We could only find long-term studies for three types of implants: BHR, Conserve Plus, and Cormet. For these implants revision rates seemed to fit the criteria for NICE benchmarks. The implant ReCap had excellent results at 2.9 years of mean follow-up. The randomised clinical trial comparing the results of the Durom implant with those of a THA reported a higher rate of revision for the resurfacing implant. However, the difference was not statistically significant. The ASR implant did not fulfill the NICE criteria in any study.
Discussion
It is interesting to compare the results from the different national registries.
The Nordic Arthroplasty Register Association [10] has three national registries: Danish, Swedish and Norwegian. The total number of total hip replacements performed between 1995 and 2007 has reached a figure of 280,201, of which only 0.5 % represented resurfacing [61]. The revision rate at two years was reported as 2.4 % for all resurfacing vs 1.1 % for conventional THA. The main complications for resurfacings outlined were fractures and aseptic loosening. The Nordic register also highlighted a survival rate significantly higher in those centres performing greater than 70 cases per annum (98.8 %) than those performing fewer (95.5 %).
Analysis of the Australian register by Prosser et al. [1] succeeded the one of Buergi et al. [62] and examined 12,093 hip resurfacings performed between 1999 and 2008. The results were compared with those of conventional THA performed during the same period. Analysis of the registry showed that women had a higher revision rate than men. However, after adjusting the size of the femoral component revision rates were similar. Femoral implants of less than 50 mm in size had a higher revision rate than if the diameter was greater than or equal to 50 mm. At eight years the cumulative percentage revision for resurfacing was 5.3 (range, 4.6–6.2) against 4.0 (range, 3.8–4.2) for THA. However, in patients with primary hip OA, who were aged less than 55 years with a femoral implant size greater than or equal to 50 mm, the cumulative percentage revision was 3.0 (range, 2.2–4.2). Furthermore, Amstutz et al. [10] and McBryde et al. [44] found themselves documenting similar results for implants of smaller head sizes of less than 50 mm. The type of implant seemed to have an influence on the results. Durom implants, ASR, Cormet 2000 HAP and Recap had a higher revision rate and higher risk of fractures; this was statistically significant in comparison to other implants. The implant with the lowest fracture rate was the BHR implant with a five-year rate of 1.2 % (range, 1.0–1.5) against 3 % for ASR (range, 2–5), 2 % for Durom (range, 1–4 ) and 3 % (range, 1–9) for Recap. After adjusting for possible confounding factors, it appeared that the differences were only related to the designs of implants and surgical technique when preparing the femoral head. Finally, the registry highlighted that dysplastic hips were at a higher risk of revision.
Analysis of the English register was made by McMinn et al. [63] and included 283,365 procedures with a mean follow up of 3.6 years (range, 0.01–9.7). The objective of this analysis was unlike other registries, not only to study the revision rates after adjustment (with sex, age, size of implants, ASA / American Society of Anesthesiologists grade) but also to study the mortality rate. After adjusting for all known risk factors for revision surgery, mortality in men was statistically lower for the BHR implant in comparison to the uncemented THA group. The authors concluded for every 23 cases (males), there will be one less death in the BHR group in comparison to the cemented THA group at six years follow up.
In our review the percentage of studies that met the NICE criteria was 69.8 %. The average survival rate in these studies was significantly higher than the national registries. One explanation for this difference is that these studies are often single-operator led being experienced surgeons themselves. The most important series highlighted are those from design centres, which probably introduces a confounding factor.
However, analysis of records despite the large number of prosthesis is not provided to overestimate the information they provide. Indeed there are many confounding factors and bias that can lead to misinterpretation of the results.
First, record completeness is not guaranteed. So if the data collection seems close to 95 % for northern registers, it would be only 30 % for British records [64].
Second, the failure criteria is often the revision of the implant for whatever reason. This criteria is not necessarily impartial. This is because the sensitivity of the revision rate for clinical failure (insufficient functional score) is not identical between a resurfacing implant and a conventional total hip replacement. For example, as for knee arthroplasties, for hips with a poor functional outcome (HHS <30), only 12 % of THA may have been revised, as compared to 63 % of resurfacing with a similar score [63–65]. This calls into question the use of the revision rate for objectively comparing these two types of implants.
Third, the records do not account for the learning curve associated with the use of new implants [41, 66, 67]. Indeed for the implants on the market for over ten years there is no implication of a learning curve within the data held in the registries.
Finally, essential information is often missing: history of the patients, the ASA score, radiographic positioning of the implants, the presence of osteolysis, etc. This information is vital to determine the cause of failure, groups at risk and to compare similar groups of patients after adjustment for these criteria.
In conclusion, this review of the literature emphasises the importance of certain parameters that can improve the results of resurfacing. The type of implant seems to play an important role as does patient selection. This should be based more on the expected size of the implant rather than the gender. Finally, it is clear that the resurfacing implants require a significant learning curve and implants are less “tolerant” than conventional THA, particularly for the orientation of the acetabular component [44, 61, 68].
Acknowledgments
Conflict of interest
None.
References
- 1.Prosser GH, Yates PJ, Wood DJ, Graves SE, Steiger RN, Miller LN. Outcome of primary resurfacing hip replacement: evaluation of risk factors for early revision. Acta Orthop. 2010;81(1):66–71. doi: 10.3109/17453671003685434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delaunay C, Petit I, Learmonth ID, Oger P, Vendittoli PA. Metal-on-metal bearings total hip arthroplasty: the cobalt and chromium ions release concern. Orthop Traumatol Surg Res. 2010;96(8):894–904. doi: 10.1016/j.otsr.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Guidance on the selection of prostheses for primary total hip replacement (Technology appraisal guidance) London: NICE; 2000. [Google Scholar]
- 4.Cullum N, Sheldon T, Watt I, West P, Wright J. Assessment of NICE guidance. Lancet. 2004;364(9429):136–author reply 137. doi: 10.1016/S0140-6736(04)16618-X. [DOI] [PubMed] [Google Scholar]
- 5.Roberts VI, Esler CN, Harper WM. What impact have NICE guidelines had on the trends of hip arthroplasty since their publication? The results from the Trent Regional Arthroplasty Study between 1990 and 2005. J Bone Joint Surg Br. 2007;89(7):864–867. doi: 10.1302/0301-620X.89B7.18593. [DOI] [PubMed] [Google Scholar]
- 6.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ, Group GW. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336(7651):995–998. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baker RP, Pollard TCB, Eastaugh-Waring SJ, Bannister GC. A medium-term comparison of hybrid hip replacement and Birmingham hip resurfacing in active young patients. J Bone Joint Surg Br. 2011;93(2):158–163. doi: 10.1302/0301-620X.93B2.25625. [DOI] [PubMed] [Google Scholar]
- 9.Australian Orthopaedic Association Five-year results of the ASR XL Acetabular System and the ASR Hip Resurfacing System: an analysis from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg. 2011; 93(24):2287–2293. doi: 10.2106/JBJS.J.01727. [DOI] [PubMed] [Google Scholar]
- 10.Amstutz HC, Wisk LE, Duff MJ. Sex as a patient selection criterion for metal-on-metal hip resurfacing arthroplasty. J Arthroplasty. 2011;26(2):198–208. doi: 10.1016/j.arth.2010.03.033. [DOI] [PubMed] [Google Scholar]
- 11.Aulakh TS, Rao C, Kuiper J-H, Richardson JB. Hip resurfacing and osteonecrosis: results from an independent hip resurfacing register. Arch Orthop Trauma Surg. 2010;130(7):841–845. doi: 10.1007/s00402-009-0963-0. [DOI] [PubMed] [Google Scholar]
- 12.Beaulé PE, Shim P, Banga K. Clinical experience of Ganz surgical dislocation approach for metal-on-metal hip resurfacing. J Arthroplasty. 2009;24(6 Suppl):127–131. doi: 10.1016/j.arth.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Bergeron SG, Desy NM, Nikolaou VS, Debiparshad K, Antoniou J. The early results of metal-on-metal hip resurfacing—a prospective study at a minimum two-year follow-up. Bull NYU Hosp Jt Dis. 2009;67(2):132–134. [PubMed] [Google Scholar]
- 14.Bose VC, Baruah BD. Resurfacing arthroplasty of the hip for avascular necrosis of the femoral head: a minimum follow-up of four years. J Bone Joint Surg Br. 2010;92(7):922–928. doi: 10.1302/0301-620X.92B7.23639. [DOI] [PubMed] [Google Scholar]
- 15.Carrothers AD, Gilbert RE, Richardson JB. Birmingham hip resurfacing in patients who are seventy years of age or older. Hip Int. 2011;21(2):217–224. doi: 10.5301/HIP.2011.6500. [DOI] [PubMed] [Google Scholar]
- 16.Costa CR, Johnson AJ, Naziri Q, Mont MA. Review of total hip resurfacing and total hip arthroplasty in young patients who had Legg-Calvé-Perthes disease. Orthop Clin North Am. 2011;42(3):419–422. doi: 10.1016/j.ocl.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Daniel J, Pynsent PB, McMinn DJW. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86(2):177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 18.Daniel J, Ziaee H, Kamali A, Pradhan C, Band T, McMinn DJW. Ten-year results of a double heat treated metal on metal hip resurfacing. J Bone Joint Surg Br. 2010;92(1):20–27. doi: 10.1302/0301-620X.92B1.21530. [DOI] [PubMed] [Google Scholar]
- 19.Smet KA. Belgium experience with metal-on-metal surface arthroplasty. Orthop Clin North Am. 2005;36(2):203–213. doi: 10.1016/j.ocl.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Valle Della CJ, Nunley RM, Raterman SJ, Barrack RL. Initial American experience with hip resurfacing following FDA approval. Clin Orthop Relat Res. 2009;467(1):72–78. doi: 10.1007/s11999-008-0563-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Delport HP, Schepper J, Smith EJ, Nichols M, Bellemans J. Resurfacing hip arthroplasty. A 3 to 5-year matched pair study of two different implant designs. Acta Orthop Belg. 2011;77(5):609–615. [PubMed] [Google Scholar]
- 22.Fowble VA, Rosa MA, Schmalzried TP. A comparison of total hip resurfacing and total hip arthroplasty—patients and outcomes. Bull NYU Hosp Jt Dis. 2009;67(2):108–112. [PubMed] [Google Scholar]
- 23.Giannini S, Cadossi M, Chiarello E, Faldini C, Moroni A, Romagnoli M. Hip resurfacing arthroplasty: a series of 140 consecutive hips with a minimum five year follow-up. A clinical, radiological and histological analysis. Hip Int. 2011;21(1):52–58. doi: 10.5301/HIP.2011.6281. [DOI] [PubMed] [Google Scholar]
- 24.Gravius S, Mumme T, Weber O, Berdel P, Wirtz DC. Surgical principles and clinical experiences with the DUROM hip resurfacing system using a lateral approach. Oper Orthop Traumatol. 2009;21(6):586–601. doi: 10.1007/s00064-009-2007-x. [DOI] [PubMed] [Google Scholar]
- 25.Gross TP, Liu F. The first 100 fully porous-coated femoral components in hip resurfacing. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S30–S35. [PubMed] [Google Scholar]
- 26.Heilpern GNA, Shah NN, Fordyce MJF. Birmingham hip resurfacing arthroplasty: a series of 110 consecutive hips with a minimum five-year clinical and radiological follow-up. J Bone Joint Surg Br. 2008;90(9):1137–1142. doi: 10.1302/0301-620X.90B9.20524. [DOI] [PubMed] [Google Scholar]
- 27.Hing CB, Back DL, Bailey M, Young DA, Dalziel RE, Shimmin AJ. The results of primary Birmingham hip resurfacings at a mean of five years. An independent prospective review of the first 230 hips. J Bone Joint Surg Br. 2007;89(11):1431–1438. doi: 10.1302/0301-620X.89B11.19336. [DOI] [PubMed] [Google Scholar]
- 28.Hulst JB, Ball ST, Wu G, Duff MJ, Woon RP, Amstutz HC. Survivorship of Conserve® Plus monoblock metal-on-metal hip resurfacing sockets: radiographic midterm results of 580 patients. Orthop Clin North Am. 2011;42(2):153–159. doi: 10.1016/j.ocl.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 29.Jameson SS, Langton DJ, Nargol AVF. Articular surface replacement of the hip: a prospective single-surgeon series. J Bone Joint Surg Br. 2010;92(1):28–37. doi: 10.1302/0301-620X.92B1.22769. [DOI] [PubMed] [Google Scholar]
- 30.Khan M, Kuiper J-H, Edwards D, Robinson E, Richardson JB. Birmingham hip arthroplasty: five to eight years of prospective multicenter results. J Arthroplasty. 2009;24(7):1044–1050. doi: 10.1016/j.arth.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 31.Killampalli VV, Hayes A, Parsons N, Costa ML, Prakash U. Hip resurfacing using the trochanteric flip osteotomy. Hip Int. 2009;19(2):131–135. doi: 10.1177/112070000901900209. [DOI] [PubMed] [Google Scholar]
- 32.Kim PR, Beaulé PE, Laflamme GY, Dunbar M. Causes of early failure in a multicenter clinical trial of hip resurfacing. J Arthroplasty. 2008;23(6 Suppl 1):44–49. doi: 10.1016/j.arth.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 33.Klein M, Scherger B, Bernd H, Ostermann PA. Complications after hip resurfacing using the ASR prosthesis in patients with osteoarthritis. Z Orthop Unfall. 2008;146(2):179–184. doi: 10.1055/s-2008-1038397. [DOI] [PubMed] [Google Scholar]
- 34.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AVF. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: A consequence of excess wear. J Bone Joint Surg Br. 2010;92(1):38–46. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- 35.Larbpaiboonpong V, Turajane T, Pragtong P. The early outcome of Birmingham hip resurfacing: an independent Thai surgeon experiences. J Med Assoc Thai. 2009;92(Suppl 6):S134–S140. [PubMed] [Google Scholar]
- 36.Lei M, Yang S, Xu W, Ye S, Ze R, Fan L. Metal-on-metal total hip resurfacing arthroplasty for treatment of advanced osteonecrosis of femoral head in young and middle-aged patients. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2010;24(3):262–265. [PubMed] [Google Scholar]
- 37.Alberta Hip Improvement Project. MacKenzie JR, O’Connor GJ, et al. Functional outcomes for 2 years comparing hip resurfacing and total hip arthroplasty. J Arthroplasty. 2012;27(5):750–7.e2. doi: 10.1016/j.arth.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 38.Madadi F, Eajazi A, Kazemi SM, Aalami Harandi A, Madadi F, Sharifzadeh SR. Total hip arthroplasty in advanced osteonecrosis: the short-term results by metal-on-metal hip resurfacing. Med Sci Monit. 2011;17(2):CR78–CR82. doi: 10.12659/MSM.881391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Madhu TS, Akula MR, Raman RN, Sharma HK, Johnson VG. The Birmingham hip resurfacing prosthesis: an independent single surgeon’s experience at 7-year follow-up. J Arthroplasty. 2011;26(1):1–8. doi: 10.1016/j.arth.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 40.Malhotra R, Kannan A, Kumar V, Nagaraj C, Marimuthu K, Khatri D. Hip resurfacing arthroplasty in inflammatory arthritis a 3- to 5-year follow-up study. J Arthroplasty. 2012;27(1):15–20. doi: 10.1016/j.arth.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 41.Marker DR, Zywiel MG, Johnson AJ, Seyler TM, Mont MA. Are component positioning and prosthesis size associated with hip resurfacing failure? BMC Musculoskelet Disord. 2010;11:227. doi: 10.1186/1471-2474-11-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marulanda GA, Wilson MS, Edwards P, Raterman S (2008) Early clinical experience with the use of the Birmingham hip resurfacing system. Orthopedics 31(12 Suppl 2) [PubMed]
- 43.McAndrew AR, Khaleel A, Bloomfield MD, Aweid A. A district general hospital’s experience of hip resurfacing. Hip Int. 2007;17(1):1–3. doi: 10.1177/112070000701700101. [DOI] [PubMed] [Google Scholar]
- 44.McBryde CW, Theivendran K, Thomas AMC, Treacy RBC, Pynsent PB. The influence of head size and sex on the outcome of Birmingham hip resurfacing. J Bone Joint Surg Am. 2010;92(1):105–112. doi: 10.2106/JBJS.I.00197. [DOI] [PubMed] [Google Scholar]
- 45.McMinn DJW, Daniel J, Ziaee H, Pradhan C. Indications and results of hip resurfacing. Int Orthop. 2011;35(2):231–237. doi: 10.1007/s00264-010-1148-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mont MA, Marker DR, Smith JM, Ulrich SD, McGrath MS. Resurfacing is comparable to total hip arthroplasty at short-term follow-up. Clin Orthop Relat Res. 2009;467(1):66–71. doi: 10.1007/s11999-008-0465-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mont MA, Seyler TM, Ulrich SD, et al. Effect of changing indications and techniques on total hip resurfacing. Clin Orthop Relat Res. 2007;465:63–70. doi: 10.1097/BLO.0b013e318159dd60. [DOI] [PubMed] [Google Scholar]
- 48.Naal FD, Pilz R, Munzinger U, Hersche O, Leunig M. High revision rate at 5 years after hip resurfacing with the Durom implant. Clin Orthop Relat Res. 2011;469(9):2598–2604. doi: 10.1007/s11999-011-1792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ollivere B, Duckett S, August A, Porteous M. The Birmingham Hip Resurfacing: 5-year clinical and radiographic results from a District General Hospital. Int Orthop. 2010;34(5):631–634. doi: 10.1007/s00264-009-0821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sandiford NA, Muirhead-Allwood SK, Skinner JA, Hua J. Metal on metal hip resurfacing versus uncemented custom total hip replacement—early results. J Orthop Surg Res. 2010;5:8. doi: 10.1186/1749-799X-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siebel T, Maubach S, Morlock MM. Lessons learned from early clinical experience and results of 300 ASR hip resurfacing implantations. Proc Inst Mech Eng H. 2006;220(2):345–353. doi: 10.1243/095441105X69079. [DOI] [PubMed] [Google Scholar]
- 52.Smolders JMH, Hol A, Rijnberg WJ, Susante JLC. Metal ion levels and functional results after either resurfacing hip arthroplasty or conventional metal-on-metal hip arthroplasty. Acta Orthop. 2011;82(5):559–566. doi: 10.3109/17453674.2011.625533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Steffen RT, Pandit HP, Palan J, Beard DJ, Gundle R, McLardy-Smith P, Murray DW, Gill HS. The five-year results of the Birmingham Hip Resurfacing arthroplasty: an independent series. J Bone Joint Surg Br. 2008;90(4):436–441. doi: 10.1302/0301-620X.90B4.19648. [DOI] [PubMed] [Google Scholar]
- 54.Stulberg BN, Trier KK, Naughton M, Zadzilka JD. Results and lessons learned from a United States hip resurfacing investigational device exemption trial. J Bone Joint Surg Am. 2008;90(Suppl 3):21–26. doi: 10.2106/JBJS.H.00718. [DOI] [PubMed] [Google Scholar]
- 55.Swank ML, Alkire MR. Minimally invasive hip resurfacing compared to minimally invasive total hip arthroplasty. Bull NYU Hosp Jt Dis. 2009;67(2):113–115. [PubMed] [Google Scholar]
- 56.Takamura KM, Yoon J, Ebramzadeh E, Campbell PA, Amstutz HC. Incidence and significance of femoral neck narrowing in the first 500 Conserve® Plus series of hip resurfacing cases: a clinical and histologic study. Orthop Clin North Am. 2011;42(2):181–193. doi: 10.1016/j.ocl.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 57.Treacy RBC, Mcbryde CW, Shears E, Pynsent PB. Birmingham hip resurfacing: a minimum follow-up of ten years. J Bone Joint Surg Br. 2011;93(1):27–33. doi: 10.1302/0301-620X.93B1.24134. [DOI] [PubMed] [Google Scholar]
- 58.Vendittoli P-A, Ganapathi M, Roy AG, Lusignan D, Lavigne M. A comparison of clinical results of hip resurfacing arthroplasty and 28 mm metal on metal total hip arthroplasty: a randomised trial with 3–6 years follow-up. Hip Int. 2010;20(1):1–13. doi: 10.1177/112070001002000101. [DOI] [PubMed] [Google Scholar]
- 59.Wang Q, Zhang XL, Chen YS, Shen H, Shao JJ. Resurfacing arthroplasty for hip dysplasia: a prospective randomised study. J Bone Joint Surg Br. 2012;94(6):768–773. doi: 10.1302/0301-620X.94B6.28522. [DOI] [PubMed] [Google Scholar]
- 60.Witzleb W-C, Arnold M, Krummenauer F, Knecht A, Ranisch H, Günther K-P. Birmingham hip resurfacing arthroplasty: short-term clinical and radiographic outcome. Eur J Med Res. 2008;13(1):39–46. [PubMed] [Google Scholar]
- 61.Johanson P-E, Fenstad AM, Furnes O, Garellick G, Havelin LI, Overgaard S, Pedersen AB, Kärrholm J. Inferior outcome after hip resurfacing arthroplasty than after conventional arthroplasty. Evidence from the Nordic Arthroplasty Register Association (NARA) database, 1995 to 2007. Acta Orthop. 2010;81(5):535–541. doi: 10.3109/17453674.2010.525193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Buergi ML, Walter WL. Hip resurfacing arthroplasty: the Australian experience. J Arthroplasty. 2007;22(7 Suppl 3):61–65. doi: 10.1016/j.arth.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 63.McMinn DJW, Snell KIE, Daniel J, Treacy RBC, Pynsent PB, Riley RD. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ. 2012;344:e3319. doi: 10.1136/bmj.e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Corten K, Macdonald SJ. Hip resurfacing data from national joint registries: what do they tell us? What do they not tell us? Clin Orthop Relat Res. 2010;468(2):351–357. doi: 10.1007/s11999-009-1157-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Goodfellow JW, O’Connor JJ, Murray DW. A critique of revision rate as an outcome measure: re-interpretation of knee joint registry data. J Bone Joint Surg Br. 2010;92(12):1628–1631. doi: 10.1302/0301-620X.92B12.25193. [DOI] [PubMed] [Google Scholar]
- 66.Witjes S, Smolders JMH, Beaulé PE, Pasker P, Susante JLC. Learning from the learning curve in total hip resurfacing: a radiographic analysis. Arch Orthop Trauma Surg. 2009;129(10):1293–1299. doi: 10.1007/s00402-009-0875-z. [DOI] [PubMed] [Google Scholar]
- 67.Berend KR, Lombardi AV, Adams JB, Sneller MA. Unsatisfactory surgical learning curve with hip resurfacing. J Bone Joint Surg Am. 2011;93(Suppl 2):89–92. doi: 10.2106/JBJS.J.01719. [DOI] [PubMed] [Google Scholar]
- 68.Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90(10):1291–1297. doi: 10.1302/0301-620X.90B10.20533. [DOI] [PubMed] [Google Scholar]