Abstract
Purpose
Although the predictive value of Böhler’s angle on outcome remains subject of debate, the initial angle at the time of trauma still guides treatment. Changes in Böhler’s angle during follow-up are frequently reported following surgical treatment of displaced intra-articular calcaneal fractures (DIACF). The aim of the present study was to determine the changes in Böhler’s angle as a measure of secondary fracture displacement following conservative management of DIACF.
Methods
Thirty-eight patients with a total of 44 displaced intra-articular calcaneal fractures treated conservatively with a minimum of two lateral radiographs during follow-up were analysed. Böhler’s angle at different follow-up times was measured by three observers. The change in angle was compared with the angle at trauma, and influence of trauma mechanism and common calcaneal fracture classifications were determined.
Results
The results showed a significant decline over time of the Böhler’s angle in conservatively-treated patients of more than 11° on average at a mean follow-up of 29.2 weeks. This decrease was not related to gender, the initial angle, or the Essex-Lopresti or Sanders classification. A statistically significantly higher decrease was detected in high energetic trauma compared with low energetic trauma.
Conclusion
The conservative treatment of displaced intra-articular calcaneal fractures is still a viable option, yet a significant secondary displacement in time should be taken into account, as reflected in a decrease of Böhler’s angle of 11° up to one year following trauma.
Introduction
The surgical treatment of displaced intra-articular fractures has gained much interest in the last few decades. However, the conservative treatment, either functional or using Plaster-of-Paris, is still the treatment of choice in specific cases. Especially in patients with a fracture with minimal or without displacement, or in case of a polytrauma patient with life-threatening concomitant injuries, or those with severely compromised soft-tissues who might fare just as well with conservative as with operative management. Certain physical or psychological patient characteristics like diabetes, peripheral vascular disease, low anticipated compliance or substance abuse may put the patient at an unacceptable increased risk of surgical complications; in those patients a conservative treatment is justified [1, 2]. Currently, approximately 40 % of displaced intra-articular calcaneal fractures are treated conservatively in the Netherlands [3].
In the decision-making process on the best treatment strategy, the fracture characteristics that should be assessed are the articular involvement, varus/valgus malalignment, increase in width, and loss of height. The loss of height is directly derived from the Tuber angle as described by Böhler in the early 1930s [4]. Although the predictive value of Böhler’s angle on outcome remains a subject of debate, the initial angle at the time of trauma still guides treatment [5, 6]. There is a considerable amount of literature on the change of Böhler’s angle following surgically treated displaced intra-articular calcaneal fractures throughout the follow-up (Table 1) [7–17]. Data on Böhler’s angle in conservatively-treated fractures, however, are limited.
Table 1.
Böhler’s angle following operatively-treated displaced intra-articular calcaneal fractures
| Author | N, treatment | Follow-up (months) | Böhler’s angle (°) | |||
|---|---|---|---|---|---|---|
| Trauma | Post-op | Follow-up | Decrease | |||
| Kurozumi et al. 2003 [12] | 67, ORIF | 20 | 5.5 | 27.1 | 22.6 | 4.5 |
| Schepers et al. 2007 [14] | 37, Perc | 35 | −2 | 19 | 14 | 5 |
| Jiang et al. 2008 [10] | 74, β-TCP | 15 | 6.4 | 29.3 | 25.6 | 1.7 |
| Johal et al. 2009 [11] | 28, ORIF | 12 | −0.6 | 32.6 | 22.2 | 10.4 |
| 24, + α-BSM | 12 | −1.2 | 31.1 | 24.9 | 6.2 | |
| Rak et al. 2009 [13] | 42, ORIF | 24 | 4.9 | 26.2 | 23.7 | 2.5 |
| DeWall et al. 2010 [8] | 42, ORIF | 24 | 0 | 22.4 | 18.4 | 4 |
| 83, Perc | 22 | −3.3 | 22 | 19.9 | 2.1 | |
| Hyer et al. 2010 [9] | 17, ORIF lp | 17 | NS | 30.1 | 28.5 | 1.6 |
| Chen et al. 2011 [7] | 40, ORIF | 24 | 1.4 | 30.6 | 28.9 | 1.7 |
| 38, Perc | 24 | 1.5 | 32.1 | 30.4 | 1,7 | |
| Tomesen et al. 2011 [15] | 39, Perc | 66 | 3.4 | 21.8 | 20.1 | 1.7 |
| Woon et al. 2011 [16] | 22, Perc | 24 | 4.2 | 21.3 | 20.1 | 1.2 |
| Zhang et al. 2011 [17] | 58, Bio-abs | 23 | 7.5 | 32.7 | 31.5 | 1.2 |
| Present study | 44, Cons | 2 | −0.5 | N.A. | −11.7 | 11.2 |
α-BSM bone substitute material (calcium-phosphate), β-TCP tricalcium phosphate, ORIF open reduction and internal fixation, Perc percutaneous treatment, Cons conservative treatment, lp locking plate, Bio-abs bio-absorbable screws, NS not specified
Therefore the aim of this study was to determine the changes in Böhler’s angle of displaced intra-articular calcaneal fractures (DIACF) as a measure of secondary fracture displacement following conservative management.
Material and methods
All consecutive patients with unilateral or bilateral displaced intra-articular calcaneal fractures (DIACF) treated conservatively between 2004 and 2011 were included in this study, which was approved by the local Medical Research Ethics Committee. Patient characteristics (i.e., age, gender, and affected side), trauma mechanism, and fracture characteristics (i.e., Essex-Lopresti and Sanders classification) were collected from the electronic hospital records. The Essex-Lopresti classification [2] and the Sanders classification [18] were determined based on an initial CT-scan. Conventional digital lateral radiographs of the fractured calcaneus were collected. Patients for whom radiographs were present for no more than one time point were excluded. For each patient all available radiographs up to two years follow-up were collected. Böhler’s angle was measured using the Picture Archiving and Communication System (iSite PACS–Philips–Philips Healthcare, Eindhoven, the Netherlands) tool for angle measurement; Böhler’s tuber joint angle was measured using the highest points of the calcaneal tuberosity, the subtalar joint and the anterior process and was taken as a relative measurement of the degree of compression and deformity in calcaneal fractures [4]. The Böhler angle was measured by three observers independently. The three recordings were averaged. Any measurement discrepancy of more than 5° was settled in a consensus meeting.
Statistical analysis
Analyses were performed using SPSS (version 16.0, SPSS Inc., Chicago, IL, USA). Normality of continuous data was checked by inspecting the frequency distributions (histograms) and normal Q-Q plots. They were found not to escape the standard normal distribution and were therefore considered as parametric. Continuous variables are presented as mean with standard deviation (SD), categorical variables as numbers and percentage. Böhler’s angle at trauma and follow-up as well as the change in angle and time since trauma were related to the Böhler’s angle at trauma (i.e., <0° versus ≥0°) using a Student’s t-test with unequal variance. Similarly, the (change in) angle was related to gender, the trauma mechanism (i.e., HET versus LET), Sanders classification (with or without a c-type fracture-line [19] (i.e., 2A, 2B, or 3AB versus 2C, 3AC, 3BC, or 4), and Essex-Lopresti classification (i.e., joint-depression versus tongue-type). Finally, multivariable linear regression models were developed with the different angles as dependent outcome and trauma mechanism, fracture class, and initial Böhler’s angle as covariables. A P-value <0.05 (two-sided) was taken as threshold of statistical significance.
Results
Patient characteristics
A total of 59 patients with a displaced intra-articular calcaneus fracture were treated conservatively in the period between 2004 and 2011. Twenty-one patients were excluded because no follow-up conventional radiographs were available. Thirty-eight patients were available for analysis, of which six patients suffered fractures bilaterally (total of 44 calcaneal fractures). The mean age was 40.5 years (SD 11.3 years), and the majority of patients was male (30/38, 79 %). Fractures occurred in the right foot in 21 and the left in 23 patients. Of the fractures, 26 were sustained during a low energetic trauma (LET) and 18 during a high energetic trauma (HET). The mean follow-up was 29.2 weeks (SD 26.6; range 3.0–105.6 weeks).
Radiographic data
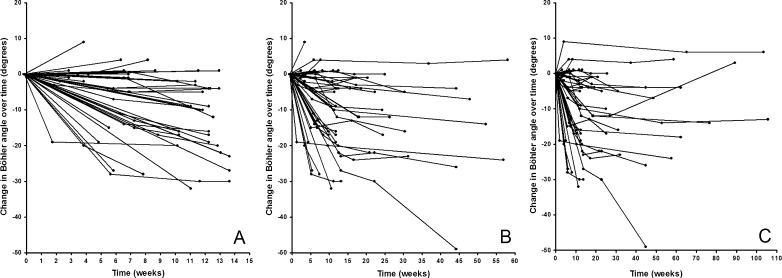
Eighteen fractures were classified as tongue type and 26 as joint-depression type according to the Essex-Lopresti classification. Sanders classification showed 40 type-2 fractures, three type-3 fractures and one type-4 fracture. The mean angle of Böhler measured at trauma was −0.5° (SD 14.4; range −34 to 24). At final follow-up the mean Böhler’s angle was −11.7° (SD 17.2; range −44 to 28). The average decrease in Böhler’s angle during follow-up was 11.2° (SD 11.8; range −49 to 6; Fig. 1).
Fig. 1.
Change in Böhler’s angle over time. a Trend over 15 weeks. b Trend over 60 weeks. c Trend over 110 weeks
The decrease in Böhler’s angle was not related to the angle at trauma, as the mean (± SD) decrease was similar in fractures with an initial Böhler above zero degrees (−13.4 ± 13.1°) and in fractures with an angle below or equal zero (−9.1 ± 10.2°; p = 0.235). This difference was not statistically different over a comparable duration of follow-up (Fig. 2a).
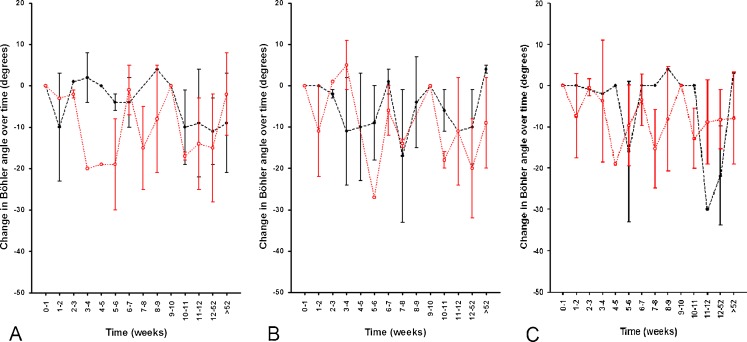
Fig. 2.
Influence of various factors on the change in Böhler’s angle over time. a Initial Böhler on presentation (black line initial Böhler < zero, red line ≥ zero). b Trauma mechanism (black line LET, red line HET). c Gender (black line female, red line male)
With respect to the trauma mechanism Böhler’s angle decreased statistically significantly more after a HET (−15.8 ± 13.0°) than after a LET (−8.0 ± 10.0°; p = 0.040). The follow-up duration was similar in both groups (Fig. 2b). Considering gender, the decrease in Böhler’s angle in women was 14.2° ± 18.2° and in male patients 10.5° ± 9.6°. This difference, with a similar follow-up, was not statistically different (p = 0.569) (Fig. 2c).
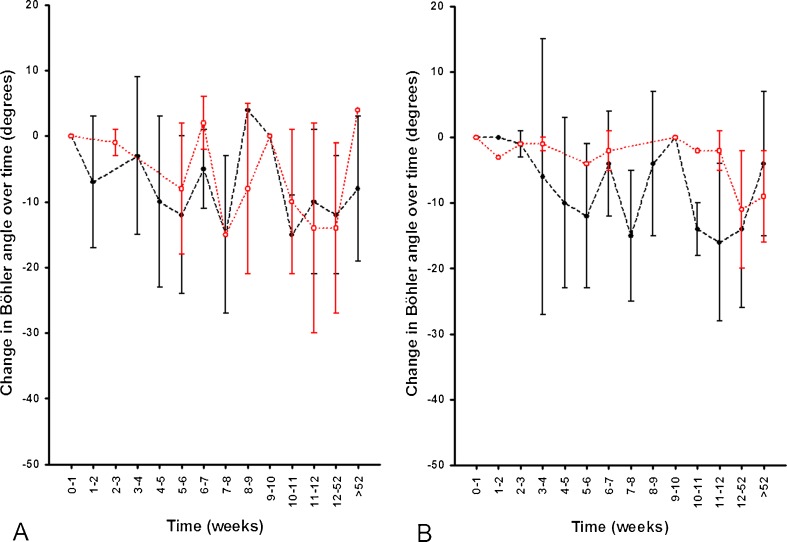
With respect to the Essex-Lopresti classification, the mean change in Böhler’s angle was similar in tongue-type fractures (−12.4 ± 13.8°) and in joint-depression-type fractures (−10.4 ± 10.4°; p = 0.596) (Fig. 3a). No association could be detected with respect to the Sanders classification (p = 0.402) (Fig. 3b).
Fig. 3.
Influence of various factors on the change in Böhler’s angle over time. a Essex-Lopresti classification (black line joint-depression, red line tongue-type). b Sanders classification (black line without c-fracture line [2a, 2b, 3ab], red with c-fracture line [2c, 3ac, 3bc, 4])
In the multivariable model, the change in Böhler’s angle was statistically significantly related to the trauma mechanism (B = −8.726; 95 % CI −15.995 to −1.457; p = 0.020), but not to the angle at trauma (B = −0.197; 95 % CI −0.480–0.086; p = 0.168), the Essex-Lopresti classification (B = 2.441; 95 % CI −4.696–9.578; p = 0.493) or the Sanders classification (B = 1.523; 95 % CI −7.277–10.323; p = 0.728).
Discussion
The results of the present investigation show a significant decline over time of the Böhler’s angle in conservatively-treated patients of more than 11° on average. This decrease was not related to gender, the initial angle, Essex-Lopresti, or Sanders classification. A statistically significant difference was detected when comparing low energetic trauma with high energetic trauma.
This is the first study in which the trends in Böhler’s angle, in a consecutive series of conservatively-treated patients, were assessed. Only one small sample of 19 conservatively-treated patients could be identified from the literature in which an initial Tuber angle and an angle at final follow-up were presented [20]. In this study the initial angle of Böhler measured +2° (range, −10 to +20), and at follow-up −1° (range, −20 to +20).
From Böhler’s original paper, the Tuber angle in non fractured calcanei ranges from 25 to 40° [4]. Single digit Böhler angles are common in fractured calcaneus (Table 1), which agrees with the findings in our study. There were no calcaneal fractures with an initial Böhler’s angle of over 15°. So the results of the present study might not be translated to this subpopulation of ‘minor’ fractures.
The main limitation of the present study is its retrospective nature. Follow-up appointments varied between patients and follow-up radiographs were made depending upon the surgeon’s preference or the patient’s complaints. The significantly longer follow-up in HET patients can be explained by the possible prolonged treatment for the concomitant injuries. This in turn might explain the lower angle at final follow-up, as Rak and Hyer showed an ongoing minor decrease in Böhler’s angle even after one year [9, 13], which was significant before weight-bearing and not significant after weight-bearing in surgically treated patients [9]. The conservative treatment protocol for displaced intra-articular calcaneal fractures in our institution consisted of 10–12 weeks non weight-bearing mobilization. We can however, not account for patient compliance and lack thereof during this period and realize this to be a possible limitation of the present study, as too early weight-bearing might have a negative effect on secondary dislocation and loss of height.
Inaccuracy of measurements for Böhler’s angle may be a second limitation. Inaccuracy may arise from difference in the quality of the radiographs (e.g., rotation) that occurs from suboptimal positioning in a trauma screening setting for patients with high energy trauma mechanism. This may explain the few cases in which the Böhler’s angle at follow-up was higher than the initial angle at trauma. Little is known about the interobserver agreement in the measurement of Böhler’s angle in calcaneal fractures; it is, however, high in the non-fractured population [21, 22]. Interobserver bias for the measurements of Böhler’s angle was minimized as much as possible; three observers performed the measurements independently, and any discrepancies in excess of 5° were settled by consensus between all three observers.
In summary, there is a significant decline over time of the Böhler’s angle in conservatively-treated patients of more than 11° on average, especially in high energy traumas. As the conservative treatment of displaced intra-articular calcaneal fractures is still a viable option, future research on conservatively-treated calcaneal fractures should be encouraged not only to report initial Böhler’s angle, but also the angle at follow-up, especially in high energetic trauma fractures. In the choice of treatment option the fate of Böhler’s angle should be taken into account. Whether or not this secondary decrease has an effect on outcome needs to be subject of further investigation.
References
- 1.Buckley R, Tough S, McCormack R, Pate G, Leighton R, Petrie D, Galpin R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84-A:1733–1744. doi: 10.2106/00004623-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Essex-Lopresti P. Mechanism, reduction technique and results in fractures of os calcis. Br J Surg. 1952;39:395–419. doi: 10.1002/bjs.18003915704. [DOI] [PubMed] [Google Scholar]
- 3.Schepers T, Lieshout EM, Ginhoven TM, Heetveld MJ, Patka P. Current concepts in the treatment of intra-articular calcaneal fractures: results of a nationwide survey. Int Orthop. 2008;32:711–715. doi: 10.1007/s00264-007-0385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Böhler L. Diagnosis, pathology and treatment of fractures of the os calcis. J Bone Joint Surg. 1931;13:75–89. [Google Scholar]
- 5.Loucks C, Buckley R. Bohler’s angle: correlation with outcome in displaced intra-articular calcaneal fractures. J Orthop Trauma. 1999;13:554–558. doi: 10.1097/00005131-199911000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Shuler FD, Conti SF, Gruen GS, Abidi NA. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures: does correction of Bohler’s angle alter outcomes? Orthop Clin N Am. 2001;32:187–192. doi: 10.1016/S0030-5898(05)70202-9. [DOI] [PubMed] [Google Scholar]
- 7.Chen L, Zhang G, Hong J, Lu X, Yuan W. Comparison of percutaneous screw fixation and calcium sulfate cement grafting versus open treatment of displaced intra-articular calcaneal fractures. Foot Ankle Int. 2011;32:979–985. doi: 10.3113/FAI.2011.0979. [DOI] [PubMed] [Google Scholar]
- 8.DeWall M, Henderson CE, McKinley TO, Phelps T, Dolan L, Marsh JL. Percutaneous reduction and fixation of displaced intra-articular calcaneus fractures. J Orthop Trauma. 2010;24:466–472. doi: 10.1097/BOT.0b013e3181defd74. [DOI] [PubMed] [Google Scholar]
- 9.Hyer CF, Atway S, Berlet GC, Lee TH. Early weight bearing of calcaneal fractures fixated with locked plates: a radiographic review. Foot Ankle Spec. 2010;3:320–323. doi: 10.1177/1938640010374121. [DOI] [PubMed] [Google Scholar]
- 10.Jiang SD, Jiang LS, Dai LY. Surgical treatment of calcaneal fractures with use of beta-tricalcium phosphate ceramic grafting. Foot Ankle Int. 2008;29:1015–1019. doi: 10.3113/FAI.2008.1015. [DOI] [PubMed] [Google Scholar]
- 11.Johal HS, Buckley RE, Le IL, Leighton RK. A prospective randomized controlled trial of a bioresorbable calcium phosphate paste (alpha-BSM) in treatment of displaced intra-articular calcaneal fractures. J Trauma. 2009;67:875–882. doi: 10.1097/TA.0b013e3181ae2d50. [DOI] [PubMed] [Google Scholar]
- 12.Kurozumi T, Jinno Y, Sato T, Inoue H, Aitani T, Okuda K. Open reduction for intra-articular calcaneal fractures: evaluation using computed tomography. Foot Ankle Int. 2003;24:942–948. doi: 10.1177/107110070302401214. [DOI] [PubMed] [Google Scholar]
- 13.Rak V, Ira D, Masek M. Operative treatment of intra-articular calcaneal fractures with calcaneal plates and its complications. Indian J Orthop. 2009;43:271–280. doi: 10.4103/0019-5413.49388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schepers T, Schipper IB, Vogels LM, Ginai AZ, Mulder PG, Heetveld MJ, Patka P. Percutaneous treatment of displaced intra-articular calcaneal fractures. J Orthop Sci. 2007;12:22–27. doi: 10.1007/s00776-006-1076-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tomesen T, Biert J, Frolke JP. Treatment of displaced intra-articular calcaneal fractures with closed reduction and percutaneous screw fixation. J Bone Joint Surg Am. 2011;93:920–928. doi: 10.2106/JBJS.H.01834. [DOI] [PubMed] [Google Scholar]
- 16.Woon CY, Chong KW, Yeo W, Eng-Meng Yeo N, Wong MK (2011) Subtalar arthroscopy and flurosocopy in percutaneous fixation of intra-articular calcaneal fractures: the best of both worlds. J Trauma 71(4):917–925 [DOI] [PubMed]
- 17.Zhang J, Xiao B, Wu Z. Surgical treatment of calcaneal fractures with bioabsorbable screws. Int Orthop. 2011;35:529–533. doi: 10.1007/s00264-010-1183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanders R, Fortin P, DiPasquale T, Walling A (1993) Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop 290:87–95 [PubMed]
- 19.Ogut T, Ayhan E, Kantarci F, Unlu MC, Salih M. Medial fracture line significance in calcaneus fracture. J Foot Ankle Surg. 2011;50:517–521. doi: 10.1053/j.jfas.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 20.Jarvholm U, Korner L, Thoren O, Wiklund LM. Fractures of the calcaneus. A comparison of open and closed treatment. Acta Orthop Scand. 1984;55:652–656. doi: 10.3109/17453678408992416. [DOI] [PubMed] [Google Scholar]
- 21.Clint SA, Morris TP, Shaw OM, Oddy MJ, Rudge B, Barry M. The reliability and variation of measurements of the os calcis angles in children. J Bone Joint Surg Br. 2010;92:571–575. doi: 10.1302/0301-620X.92B4.22565. [DOI] [PubMed] [Google Scholar]
- 22.Willmott H, Stanton J, Southgate C. Bohler’s angle—what is normal in the uninjured British population? Foot Ankle Surg. 2012;18:187–189. doi: 10.1016/j.fas.2011.10.005. [DOI] [PubMed] [Google Scholar]