Abstract
Purpose
Anterior cervical decompression and fusion is a well-established procedure for the treatment of cervical spinal canal stenosis. In this study, we evaluated the necessity of spinal instrumentation after four-level anterior cervical decompression and cage fusion.
Methods
From January 2006 until August 2008, 25 patients (8 females and 17 males) (mean age 63.9 ± 7.9 years) suffering from spinal stenosis C3–C7 underwent anterior decompression and interbody fusion. The patients were divided into two groups. Four-level discectomy and cage fusion was performed in all patients. In group A including nine patients, posterior instrumentation with a lateral mass screw-rod system was added, while in group B including 16 patients, additional instrumentation was not performed. The mean duration of follow-up was 48.6 months (average 25–67 months).
Results
Clinically, the mean value for the Neck Disability Index improved from 40 ± 23.25 at presentation to 16.31 ± 15.09 at the final follow-up. The difference between the two groups was statistically not significant. Radiologically, the criteria for solid bony fusion were achieved successfully in all patients of group A, and in 87.5 % of patients in group B. The difference between the two groups was statistically not significant. The fused segment was then evaluated in the sagittal radiographs as regards the height and the lordosis angle. The loss in the height as well as the loss in the lordosis angle was more when posterior instrumentation was not added. However, the difference between the two groups was not statistically significant.
Conclusion
Stand-alone intersomatic cage fusion is an acceptable line of treatment for four-level cervical disc disease, both clinically and radiologically. Although the addition of posterior instrumentation yields better radiological results, the difference does not reach the statistical significance level.
Keywords: Cervical, Four-level, Cage, Fusion, Instrumentation
Introduction
Cervical spondylosis is a progressive degenerative disease of the intervertebral discs and adjacent vertebrae. Multilevel affection of the cervical spine represents a challenging problem [3, 15]. A variety of anterior, posterior and combined approaches with and without instrumentation has been advocated [3]. As advanced cervical spondylosis most typically involves compression of the cord by anterior structures, the anterior approach allows for direct decompression of the spinal cord and excision of these pathologic elements [19]. The aim of surgery is to achieve an adequate decompression of the spinal cord, restore or maintain sagittal alignment, and avoid kyphosis [3]. Reconstruction of the defect after discectomy is still a matter of debate among spine surgeons. Autogenous tricortical iliac graft, femoral ring allograft, bone cement, artificial disc, PEEK cages and titanium cages have all been applied [2, 4, 7, 12, 13, 17, 23]. However, the choices become limited in four-level disease. Furthermore, the necessity of adding anterior and/or posterior instrumentation in multilevel disease is still debatable [3]. Recently, stand-alone cages have been widely applied in mono- and bisegmental pathologies [8, 16]. More recently, spine surgeons started to use the stand-alone cage construct in multilevel cervical disc disease [2, 7, 12]. The aim of this study was to evaluate if there are differences between cage-assisted fusion in four-level cervical arthrodesis with and without additional posterior stabilisation.
Materials and methods
Patients
A case series in which retrospective review of all patients undergoing a primary four-level anterior cervical decompression and fusion between 2006 and 2008 in our department was performed. Patients with the diagnosis of cervical spondylosis affecting four levels C3–7 and follow-up of more than 2 years were included in the study (Fig. 1). Patients with a history of rheumatoid arthritis or previous cervical spine surgery as well as patients undergoing corpectomy at any of the intervening levels were excluded from the analysis. The search in the surgical database revealed a total of 52 patients fulfilling these criteria. These patients were again reanalysed in order to obtain a homogenous group in whom a single type of implant was used, that is, all hybrid constructs were excluded. At the end, a total number of 25 patients could be identified (8 females and 17 males) (mean age 63.9 ± 7.9 years). In these patients, anterior cervical decompression and fusion was performed at the levels from C3/4 to C6/C7 using a titanium rectangular cage, which was developed in 2005 by the senior author (H.B.) (Fig. 2). These 25 patients representing the material of this study were divided into two groups. The first group (group A) included nine patients undergoing intersomatic decompression and cage-assisted fusion C3–7, together with posterior lateral mass fixation using lateral mass screw-rod system. In the second group (group B) including 16 patients, stand-alone interbody cages C3–7 without posterior fixation were applied. The choice of the treatment modality was according to the surgeon’s preference.
Fig. 1.

Cervical spondylosis and stenosis affecting four levels of the cervical spine C3–7
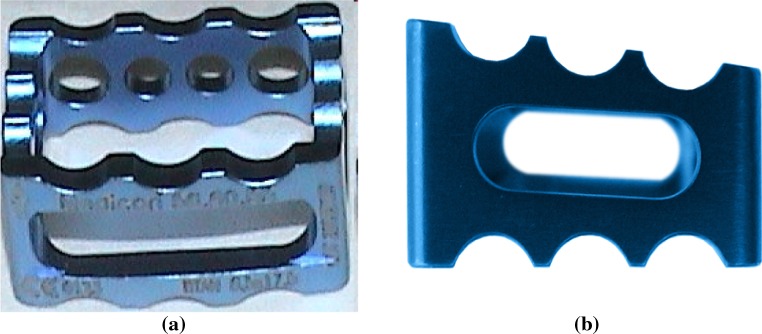
Fig. 2.
The titanium rectangular cage used in this study. a Its anterior aspect is opened to allow decortication of the endplates after application as well as insertion of the bone graft for fusion. The circular holes at its posterior aspect allow visualisation of the dural sac during insertion. b The same cage seen from the side to show its lordotic profile
Surgical technique
The primary goal of surgical management of patients enrolled in this study was decompression of the spinal cord. Secondary surgical goals included stabilisation of the cervical spine and realignment of the sagittal profile together with correction of spinal deformity.
The patient was placed supine with mild neck extension after induction of general endotracheal anaesthesia. A right-sided approach was performed via a transverse or longitudinal incision. The platysma was splitted in line with its fibres. The prevertebral fascia and longus coli muscles were mobilised to visualise the uncovertebral joints. The operative levels were confirmed using fluoroscopy and appropriate discectomy was performed starting from the most cranial level C3/4. Caspar pins were used to apply distraction as needed. With the aid of an operating microscope, the posterior longitudinal ligament was excised. This was followed by removal of the posterior osteophytes to decompress the spinal cord. The nerve roots were decompressed with meticulous foraminotomies. The endplates were not decorticated in order to provide a stable hard bed for the titanium cage avoiding its subsidence in the subchondral bone. After adequate decompression, a titanium rectangular cage (Medicage cervical, MEDICON) (Fig. 2) was placed in the distracted intervertebral space under microscopic visualisation of the dura facilitated by the open design of the cage with multiple holes. After verification of the cage position with fluoroscopy, the end plate areas not in contact with the edges of the cage were decorticated to provide a highly vascular fusion bed. Thereafter, the cages were filled with autogenous iliac bone graft harvested in a minimally invasive technique with the aid of a special drill-trocar instrument.
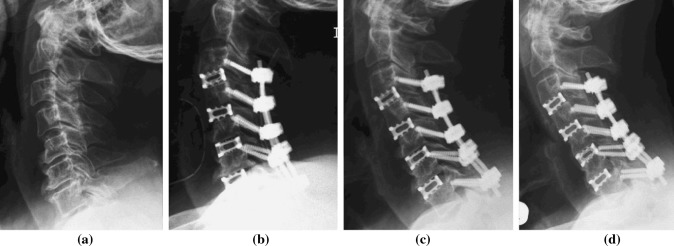
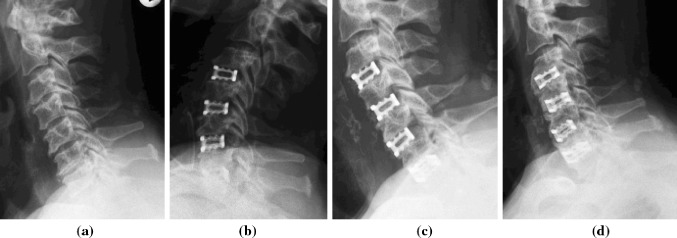
In group A, the nine patients underwent simultaneous posterior supplemental instrumentation with lateral mass screw-rod system C3–7 in the same surgical setting (Fig. 3), while in group B the operation was terminated after the anterior surgery without internal fixation (Fig. 4). After surgery, all patients were instructed to use a Philadelphia cervical collar for external immobilisation for a period of 3 weeks.
Fig. 3.
Plain radiography of a patient in group A with cervical stenosis C3–7 treated by anterior decompression and cage-augmented fusion together with posterior stabilisation. a Preoperative, b immediately postoperative, c 2 weeks after surgery, d at the final follow-up
Fig. 4.
Plain radiography of a patient in group B with cervical stenosis C3–7 treated by anterior decompression and cage-augmented fusion without stabilisation. a Preoperative, b immediately postoperative, c 2 weeks after surgery, d at the final follow-up
Outcomes assessment
Clinical and radiographic follow-up was maintained for a mean period of 48.6 months (average 25–67 months). Clinical outcome was determined on the basis of a subjective pain questionnaire according to the Neck Disability Index (NDI). The questionnaire was completed immediately before surgery and at the final follow-up. The improvement in symptoms was evaluated by calculating the difference between the NDI at the final follow-up and at presentation. Radiographic fusion was determined according to anteroposterior and lateral cervical spine X-rays. Fusion was defined by the presence of trabecular bone across the interfaces without lucencies between the cage and vertebral endplates, and bony bridging formation between superior and inferior endplates [6]. The radiological analysis was performed by two independent radiologists in a blinded manner. Furthermore, the height as well as the angle of the fused segment C3–7 were measured and compared between the two groups preoperatively, immediately after surgery and at the final follow-up.
Statistical analysis
Statistical tests used to analyse statistical significance included the Fisher exact and χ2 tests as well as the Student’s t test. Statistical significance was established at a p value of less than 0.05. All statistical analyses were performed using the SPSS program, version 11.5, on an IBM compatible computer.
Results
Clinical outcome
Table 1 describes the two groups as regards gender, age and follow-up time. The mean value for the NDI improved from 40 ± 23.25 at presentation to 16.31 ± 15.09 at the final follow-up. This improvement in the NDI reported a mean value of 29.43 ± 17.95 in group A and a mean value of 20.83 ± 18.86 in group B. The difference between the two groups was statistically not significant (t = 1.02, p = 0.33). Regarding the complications, one patient in group A developed a right C5 palsy postoperatively on one side. This was manifested by deltoid weakness grade 2 together with biceps weakness grade 4. However, full recovery of the muscle power was reported 6 months postoperatively. In group B, no complications were reported.
Table 1.
Gender, age, and follow-up time in the two groups
| Gender | Percent males | Group A | Group B | p value |
|---|---|---|---|---|
| 57.1 | 64.3 | 0.557 | ||
| Age | Range | 57–73 years | 48–74 years | 0.107 |
| Mean | 67.9 ± 5.336 | 61.9 ± 8.389 | ||
| Follow-up time | Range | 25–27 months | 29–55 months | 0.266 |
| Mean | 53.3 ± 19.155 | 46.3 ± 9.244 |
Radiographic outcome
All nine patients in group A had demonstrable radiographic fusion at the last follow-up examination, as demonstrated by bridging bone between the vertebral bodies and the absence of motion on dynamic X-rays. In group B, two patients did not fulfil the criteria for solid bony fusion (12.5 %). In the first patient, pseudoarthrosis was reported between C4 and C6, while in the second patient, pseudoarthrosis occurred between C5 and C7. However, in both patients no revision surgery was necessary due to the lack of symptoms necessitating surgical intervention. The difference between the two groups as regards bony fusion did not reach the statistical significance level (χ2 = 1.105, p = 0.533). Regarding the lordosis angle of the fused segment C3–7, there was no statistically significant difference between the two groups preoperatively. Comparing the values reported at the final follow-up with those obtained immediately after surgery revealed a loss of 10o in group A. The amount of loss when posterior instrumentation was not added reported a value of 10.1o in group B. The difference between the two groups was not statistically significant (t = 0.023, p = 0.982). The same measurements were reported for the height of the fused segment C3–7. The amount of loss in segmental height was markedly higher when posterior instrumentation was not added (1.1 mm in group A and 5.14 mm in group B), but again without statistical significance between the two groups (t = 1.763, p = 0.094) (Fig. 5).
Fig. 5.
The segmental lordosis (a) and segmental height (b) improved significantly after surgery in both groups. A loss in the gained sagittal lordosis occurred in both groups over the follow-up period. This loss was more when instrumentation was not added but without statistically significant difference. Fact is that the values at the final follow-up remained better in comparison to the preoperative values in both groups
In order to evaluate the effect of age and accompanying osteoporosis on the radiological results and whether this factor should play a role in choosing the method of treatment in long-segment cervical fusion, the patients were divided into two subgroups: the first one included 10 cases presenting all patients 65 years old and younger. The second subgroup included 15 cases presenting all patients older than 65 years. Again, the same radiological parameters were reported and compared as shown in Tables 1 and 2. No statistically significant difference was found between the two treatment methods as regards segmental lordosis and segmental height in the two age groups, denoting that additional posterior stabilisation after long-segment cervical fusion in older patients is of no statistically significant advantage.
Table 3.
The radiological parameters reported in the subgroup of patients >65 years
| Group | Preoperative | Postoperative | Last follow-up | Correction loss |
|---|---|---|---|---|
| Lordosis of the fused segment | ||||
| A | −5.5o | 22.5o | 12o | 10.5o |
| B | 5.29o | 21.71o | 8.71o | 13o |
| t test | −1.369 | 0.156 | 0.644 | 0.607 |
| p value | 0.198 | 0.879 | 0.533 | 0.556 |
| Height of the fused segment | ||||
| A | 96.17 mm | 110.17 mm | 110.2 mm | 0 mm |
| B | 100.57 mm | 109.71 mm | 103.86 mm | 5.86 mm |
| t test | −0.546 | 0.073 | 0.888 | 1.903 |
| p value | 0.596 | 0.943 | 0.393 | 0.084 |
Both Tables 2 and 3 demonstrate the values of segmental lordosis and segmental height in both groups preoperatively, immediately after surgery and at the final follow-up. The last column shows the amount of correction loss calculated as the difference between the value at the final follow-up and immediately after surgery
Table 2.
The radiological parameters reported in the subgroup of patients ≤65 years
| Group | Preoperative | Postoperative | Last follow-up | Correction loss |
|---|---|---|---|---|
| Lordosis of the fused segment | ||||
| A | 5o | 20o | 13o | 7o |
| B | 4.86o | 17.14o | 10o | 7.14o |
| t test | 0.009 | 0.349 | 0.414 | 0.033 |
| p value | 0.993 | 0.739 | 0.693 | 0.975 |
| Height of the fused segment | ||||
| A | 107 mm | 122 mm | 113 mm | 9 mm |
| B | 104.86 mm | 114.14 mm | 109.71 mm | 4.43 mm |
| t test | 0.187 | 1.063 | 0.39 | −1.86 |
| p value | 0.858 | 0.329 | 0.71 | 0.112 |
Discussion
Why four-level cervical fusion
Anterior cervical discectomy and fusion has proved to be a safe and effective procedure for the treatment of degenerative disc disease [12]. Performing this technique in cases with multilevel cervical spinal canal stenosis is still debatable as regards the type of implant applied and the necessity of supplemental fixation. Studies dealing with four-level cervical discectomy and fusion are scanty and the published reports usually include a limited number of patients [1, 2, 5, 12, 13].
Why posterior and not anterior instrumentation
Reviewing the literature as regards multilevel anterior cervical fusion supplemented by stabilisation revealed a tendency towards the application of anterior plating rather than posterior instrumentation [1, 5, 7, 12, 13, 18]. This is of course advantageous in terms of avoiding performing an additional surgery with a new posterior wound. However, posterior instrumentation was chosen in this study for several reasons. First, anterior plating after four-level discectomy and fusion is known to have a higher rate of implant related complications than for short segment fusion. The problem of screw breakage and screw pullout is well known and has been reported by several investigators [7, 12]. This can lead in extreme cases to oesophageal problems ranging from dysphagia to oesophageal perforation [7, 10]. Second and from a biomechanical point of view, the posterior instrumentation’s greater distance from the instantaneous axis of rotation relative to the anterior plate’s distance provides a greater moment arm and enhances the stability of the construct in flexion and compression [14].
Union and pseudoarthrosis
Because of increased biomechanical stress and the number of bony interfaces, the pseudoarthrosis rate after a multisegmental anterior cervical fusion is directly correlated with the number of levels treated [11, 22]. In 1997, Emery et al. retrospectively reviewed 16 patients undergoing anterior cervical discectomy and stand-alone graft fusion for three-level disease. They reported a pseudoarthrosis rate of 44 % and recommended that these patients should undergo additional or alternative measures to achieve arthrodesis consistently [9]. Anterior cervical plating with tricortical iliac graft became in the later years the gold standard for cervical fusion and was applied for multilevel disease by several authors. The rate of fusion obtained was more than 90 % in most of the series [5, 18]. Hwang et al. studied multilevel cervical disc disease treated with titanium cage fusion with and without addition of anterior plating. Bony union could be achieved in more than 90 % of their patients without significant intergroup difference [12]. In 2008, Bucciero et al. reported about 10 patients undergoing anterior cervical discectomy and stand-alone PEEK cage fusion performed at four levels. They reported 97.5 % fusion rate and concluded that this method of treatment could be safely applied in multilevel disease [2]. In the current study, patients undergoing four-level anterior cervical discectomy and stand-alone cage fusion achieved 87.5 % fusion rate. On the other hand, patients in whom supplemental posterior stabilisation was undertaken achieved a fusion rate of 100 %. Despite this difference, no statistically significant difference could be found between the two groups as regards bony union. Although the results obtained in the current work are not fully comparable with the available publications; because we did not perform anterior cervical plating and we did not use PEEK cages, however fact is that with the use of titanium cages and autogenous bone graft, solid bony arthrodesis in multilevel cervical spine surgery could be achieved whether supplemental instrumentation is added or not.
Cage design and subsidence
Over the preceding years, the use of cages in the cervical spine has increased because of their higher rate of success and their ability to prevent disc space collapse, with the potential advantages of indirect foraminal decompression by restoration and preservation of disc height and lordosis [20, 21]. Several designs of intervertebral cervical cages have been developed in the last years. The interbody cage used in this study is a rectangular one with posterior holes and an anterior open window (Fig. 2). Furthermore, the anterior aspect of the cage is higher than its posterior aspect to facilitate the restoration of segmental lordosis. The rectangular shape matches the vertebral bodies and allows press-fitting of the implant against the uncovertebral joints, safely resisting expulsion or retropulsion of the cage and allowing fibrous union and osseous growth. The open design with posterior holes allows visualisation of the dura during insertion to ensure appropriate positioning of the cage under direct vision. In order to minimise cage subsidence, the cage is designed to be inserted without removal of the endplate in order to provide a solid bed for the edges of the cage. Only after placement, the central area of the endplates not in contact with the edges of the cage could be reamed through the open window at its anterior aspect. Although the height of the fused segment at the final follow-up was always diminished in comparison to immediately after surgery regardless the method of treatment applied, this value was always higher than preoperatively, denoting that the final result is a gain in the height of the fused segment. The non significant loss in segmental height is surely due to some amount of cage subsidence. However, this minimal settling of the cage and the contained bone graft may even be beneficial leading to faster healing. This opinion has also been adopted by Hwang et al. [12].
Necessity of instrumentation in cage fusion
The main aim of this work was to evaluate the necessity of supplemental instrumentation after four-level cervical spine fusion. From the clinical point of view, no intergroup difference has been identified. Radiologically and in terms of bony union, although the addition of posterior stabilisation yields to a higher rate of bony fusion in comparison to stand-alone cages, the difference between the two methods of surgery is not statistically significant. Another point is still of importance in the radiographic evaluation; namely the sagittal profile. The amount of loss in segmental height and in segmental lordosis was indeed higher when posterior instrumentation was not added; however, the difference between the two groups again did not reach the statistical significance level. A similar result has been obtained by Hwang et al., who evaluated titanium cage-augmented fusion in three-level and four-level anterior cervical discectomies with and without anterior plate fixation. They even reported a lower complication rate and a shorter hospital stay in the group without plate fixation and concluded that stand-alone cages in multilevel cervical disc disease are better than with plate fixation [12]. These results have been also confirmed by Cho et al., who included in their work a group of 26 patients with three-level disease undergoing stand-alone PEEK cage fusion and reported also satisfactory results comparable with graft-plate construct [7]. The same subject has been studied by Bucciero et al., who applied stand-alone PEEK cage fusion in four-level cervical disc disease. They concluded that this method of treatment is an effective procedure for the treatment of such cases [2].
Limitations of this study
In this study a titanium rectangular cage has been applied to accomplish cervical intersomatic fusion. The results obtained might be limited to this implant type. However, other implant designs as well as other implant materials have been used in several other publications with similar results [1, 2, 6, 7, 13]. Another issue was the limited number of patients included in this work. 25 patients were included with a test power of 60 % (one-tailed) or 46 % (two-tailed). Because of its underpower, the study remains limited in its statements. This restriction is due to the rarity of four-level cervical spine affection. Reviewing the available literature revealed scanty publications dealing with four-level cervical intersomatic fusion and the number of patients in each study is usually small [1, 2, 5, 12, 13]. A multicenter study to include a larger number of patients might be the solution to overcome this limitation.
Conclusion
Stand-alone cages filled with autogenous iliac bone graft taken in a minimally invasive method represent a safe technique of arthrodesis after four-level cervical interbody decompression, even in elderly patients. Clinical outcome is not influenced by the addition of posterior instrumentation. Although the loss in segmental lordosis and height as well as the rate of pseudoarthrosis when posterior instrumentation is not added are more at the final follow-up, the difference does not reach the statistical significance level. Furthermore, the presence of radiological signs of pseudoarthrosis does not always reflect a bad clinical situation.
Conflict of interest
None.
References
- 1.Bolesta MJ, Rechtine GR 2nd, Chrin AM (2000) Three- and four-level anterior cervical discectomy and fusion with plate fixation: a prospective study. Spine (Phila Pa 1976) 25(16):2040–2044 (discussion 2045–2046) [DOI] [PubMed]
- 2.Bucciero A, Zorzi T, Piscopo GA. Peek cage-assisted anterior cervical discectomy and fusion at four levels: clinical and radiographic results. J Neurosurg Sci. 2008;52(2):37–40. [PubMed] [Google Scholar]
- 3.Cabraja M, Abbushi A, Koeppen D, Kroppenstedt S, Woiciechowsky C. Comparison between anterior and posterior decompression with instrumentation for cervical spondylotic myelopathy: sagittal alignment and clinical outcome. Neurosurg Focus. 2010;28(3):E15. doi: 10.3171/2010.1.FOCUS09253. [DOI] [PubMed] [Google Scholar]
- 4.Cardoso MJ, Rosner MK. Multilevel cervical arthroplasty with artificial disc replacement. Neurosurg Focus. 2010;28(5):E19. doi: 10.3171/2010.1.FOCUS1031. [DOI] [PubMed] [Google Scholar]
- 5.Chang SW, Kakarla UK, Maughan PH, DeSanto J, Fox D, Theodore N, Dickman CA, Papadopoulos S, Sonntag VK (2010) Four-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Neurosurgery 66(4):639–646 (discussion 646–647) [DOI] [PubMed]
- 6.Chiang CJ, Kuo YJ, Chiang YF, Rau G, Tsuang YH (2008) Anterior cervical fusion using a polyetheretherketone cage containing a bovine xenograft: three to five-year follow-up. Spine (Phila Pa 1976) 33(23):2524–2528 [DOI] [PubMed]
- 7.Cho DY, Lee WY, Sheu PC (2004) Treatment of multilevel cervical fusion with cages. Surg Neurol 62(5):378–385 (discussion 385–386) [DOI] [PubMed]
- 8.Dufour T, Huppert J, Louis C, Beaurain J, Stecken J, Aubourg L, Vila T. Radiological analysis of 37 segments in cervical spine implanted with a peek standalone device, with at least one year follow-up. Br J Neurosurg. 2010;24(6):633–640. doi: 10.3109/02688691003793029. [DOI] [PubMed] [Google Scholar]
- 9.Emery SE, Fisher JR, Bohlman HH (1997) Three-level anterior cervical discectomy and fusion: radiographic and clinical results. Spine (Phila Pa 1976) 22(22):2622–2624 (discussion 2625) [DOI] [PubMed]
- 10.Greiner-Perth R, Allam Y, El-Saghir H, Röhl F, Franke J, Böhm H. Analysis of reoperations after surgical treatment of degenerative cervical spine disorders: a report on 900 cases. Cen Eur Neurosurg. 2009;70(1):3–8. doi: 10.1055/s-0028-1082061. [DOI] [PubMed] [Google Scholar]
- 11.Hilibrand AS, Yoo JU, Carlson GD, Bohlman HH (1997) The success of anterior cervical arthrodesis adjacent to a previous fusion. Spine (Phila Pa 1976) 22(14):1574–1579 [DOI] [PubMed]
- 12.Hwang SL, Lin CL, Lieu AS, Lee KS, Kuo TH, Hwang YF, Su YF, Howng SL. Three-level and four-level anterior cervical discectomies and titanium cageaugmented fusion with and without plate fixation. J Neurosurg Spine. 2004;1(2):160–167. doi: 10.3171/spi.2004.1.2.0160. [DOI] [PubMed] [Google Scholar]
- 13.Khoueir P, Oh BC, Dirisio DJ, Wang MY. Multilevel anterior cervical fusion using a collagen-hydroxyapatite matrix with iliac crest bone marrow aspirate: an eighteen-month follow-up study. Neurosurgery. 2007;61(5):963–970. doi: 10.1227/01.neu.0000303192.64802.c6. [DOI] [PubMed] [Google Scholar]
- 14.Kirkpatrick JS, Levy JA, Carillo J, Moeini SR (1999) Reconstruction after multilevel corpectomy in the cervical spine. A sagittal plane biomechanical study. Spine (Phila Pa 1976) 24(12):1186–1190 (discussion 1191) [DOI] [PubMed]
- 15.Kojima T, Waga S, Kubo Y, Kanamaru K, Shimosaka S, Shimizu T. Anterior cervical vertebrectomy and interbody fusion for multi-level spondylosis and ossification of the posterior longitudinal ligament. Neurosurgery. 1989;24(6):864–872. doi: 10.1227/00006123-198906000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Kolstad F, Nygaard ØP, Andresen H, Leivseth G (2010) Anterior cervical arthrodesis using a “stand alone” cylindrical titanium cage: prospective analysis of radiographic parameters. Spine (Phila Pa 1976) 35(16):1545–1550 [DOI] [PubMed]
- 17.Pan HC, Wang YC, Lee CH, Yang DY. Hollow bone cement filled with impacted cancellous bone as a substitute for bone grafts in cervical spine fusion. J Clin Neurosci. 2007;14(2):143–147. doi: 10.1016/j.jocn.2005.11.049. [DOI] [PubMed] [Google Scholar]
- 18.Papadopoulos EC, Huang RC, Girardi FP, Synnott K, Cammisa FP Jr (2006) Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine (Phila Pa 1976) 31(8):897–902 [DOI] [PubMed]
- 19.Tortolani PJ, Yoon ST. Cervical disc disease: cervical spondylotic myelopathy. In: Frymoyer JW, Wiesel SW, An HS, Boden SD, Lauerman WC, Lenke LG, McLain RF, editors. The adult and paediatric spine. 3. Philadelphia: Lippincott Williams & Wilkins; 2004. pp. 701–711. [Google Scholar]
- 20.Türeyen K (2003) Disc height loss after anterior cervical microdiscectomy with titanium intervertebral cage fusion. Acta Neurochir (Wien) 145(7):565–569 (discussion 569–570) [DOI] [PubMed]
- 21.Vavruch L, Hedlund R, Javid D, Leszniewski W, Shalabi A (2002) A prospective randomized comparison between the cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine (Phila Pa 1976) 27(16):1694–1701 [DOI] [PubMed]
- 22.Wang JC, McDonough PW, Kanim LE, Endow KK, Delamarter RB (2001) Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 26(6):643–646 (discussion 646–647) [DOI] [PubMed]
- 23.Wilke HJ, Kettler A, Claes L. Primary stabilizing effect of interbody fusion devices for the cervical spine: an in vitro comparison between three different cage types and bone cement. Eur Spine J. 2000;9(5):410–416. doi: 10.1007/s005860000168. [DOI] [PMC free article] [PubMed] [Google Scholar]