Abstract
Purpose
The ergonomic problems for surgeons during spine surgery are an awkward body posture, repetitive movements, increased muscle activity, an overflexed spine, and a protracted time in a standing posture. The authors analyzed whole spine angles during discectomy. The objective of this study is to assess differences in surgeon whole spines angles according to operating table height and the methods used to visualize surgical field.
Materials and methods
A cohort of 12 experienced spine surgeons was enrolled. Twelve experienced spine surgeons performed discectomy using a spine surgery simulator. Three different methods were used to visualize the surgical field (naked eye, loupe, and out of loupe) and three different operating table heights. Whole spine angles were compared for three different views during discectomy simulation; midline, ipsilateral, and contralateral. A 16-camera optoelectronic motion analysis system was used, and 16 markers were placed from head to pelvis. Lumbar lordosis, thoracic kyphosis, cervical lordosis, and occipital angle were compared at the different operating table heights, while using the three visualization methods, with natural standing position.
Results
Whole spine angles were significantly different for visualization methods. Lumbar lordosis, cervical lordosis, and occipital angle were closer to natural standing values when discectomy was performed with a loupe, but most measures differed from natural standing values when performed out of loupe. Thoracic kyphosis was also similar to the natural standing position during discectomy using a loupe, but differed from the natural standing position when performed with naked eye. Whole spine angles were also found to differ from the natural standing position according to operating table height, and became closer to natural standing position values as operating table height increased, when simulation was conducted with loupe.
Conclusion
This study suggests that loupe use and a table height midpoint between the umbilicus and sternum are optimal for reducing surgeon musculoskeletal fatigue.
Keywords: Spine, Surgeon, Kinematics, Discectomy
Introduction
Ergonomics is defined as “the science that deals with the consideration of human characteristics, expectations, and behaviors in the design of things people use in their work and everyday lives and of the environments in which they work and lives” [1]. It is well known that maintaining a correct posture is an important ergonomic factor for minimizing physical fatigue [2, 3]. An awkward working posture can increase stress on certain body parts, and result in musculoskeletal disorders and nerve problems [4].
Ergonomic stress during surgery is of considerable importance. Due to patient positions, surgeons tend to lean forward toward or even over the surgical field to see and manipulate tissues, and this results in increased muscle activity to balance the upper body [5]. Furthermore, maintaining an awkward body position for longer periods of time results in musculoskeletal fatigue and physical complaints [5]. To maintain proper balance during surgery, the body requires continuous active control and because two-thirds of body mass is located in the upper two-thirds of the body, not surprisingly, the human body has been described as an unstable balanced system [2]. For this reason, the pains complained of by surgeons are usually concentrated at the body axis. In a previous study, it was reported that 30 % of surgeons complain of pain and stiffness of the shoulder, neck, and lower back, and thus, spinal axis and angle are important parameters for assessing the physical stress surgeons are exposed to during surgery [6]. Generally, surgeons should operate repeatedly during several decades, so if awkward body position during operation was accumulated, ergonomic stress will be make big problem.
The main purpose of spine surgery is to resolve axial pain, such as, the neck and back pain, complained of by patients. However, the authors have also experienced neck and back pain during and after spine surgery. A literature search failed to reveal any study on ergonomics regarding different operating environments during spine surgery. The aim of this study was to analyze spine angles during different ergonomic conditions faced by surgeons during discectomy, and in particular, to investigate differences in head and whole spine motion patterns and angles with respect to operating table height, and the methods used to visualize the surgical field.
Materials and methods
Subjects
This study used a randomized crossover design to examine relationships between head and whole spine angles and methods used to visualize the surgical field and different operating heights during discectomy. The study protocol was reviewed and approved by the institutional review board of Gangnam Severance Hospital, Yonsei University College of Medicine (No 3-2011-0127). A cohort of 12 experienced spine surgeons was enrolled to study the motion characteristics of heads and whole spines during discectomy simulation. All of these surgeons had more than 4 years’ experience in spine surgery.
Experimental setup
Twelve experienced spine surgeons performed discectomy using a spine surgery simulator (Spine Surgery Simulator 1-Lumbo-sacral, CREAPLAST, Verton, FR) using three visualization methods (naked eye, loupe, and out of loupe) and three operating table heights; the anterior superior iliac spine (ASIS), umbilicus (U), the midpoint between the umbilicus and sternum (U–S). When surgeons simulated discectomy using naked eye, a part of the spectacles except the eye was covered to minimize eye movement. Whole spine and head motions and angles were examined in three different views, namely, midline, ipsilateral, and contralateral views during simulations (Fig. 1). Data were acquired using a Vicon 3-D motion analysis 16-camera system (Model MX-T40, Vicon Motion Systems, Oxford, UK) operating at sample rate of 100 Hz.
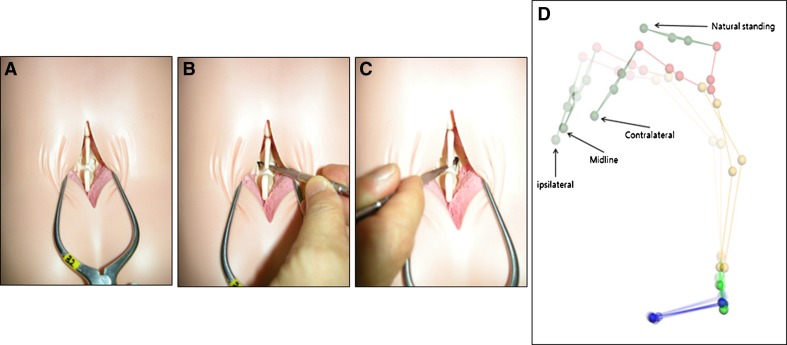
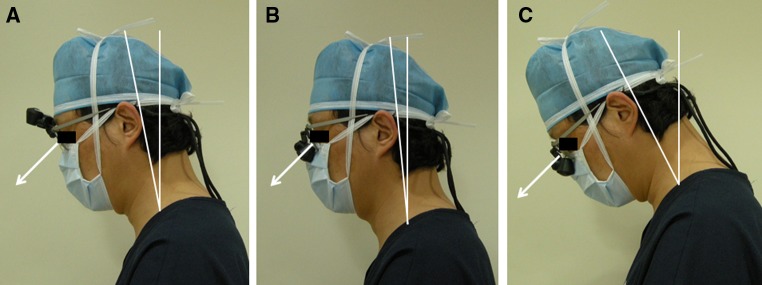
Fig. 1.
Spine surgeons performed discectomy using a simulator (Spine Surgery Simulator 1-Lumbo-sacral, CREAPLAST, Verton, FR) in three views, namely, midline (a), ipsilateral (b), and contralateral (c). Three-dimensional model at motion analysis system in the three different views (d)
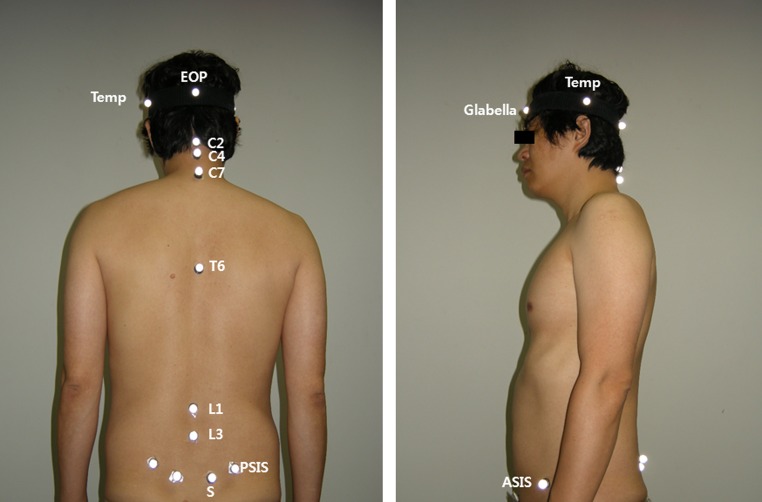
Sixteen markers were placed on skin from head to pelvis (Fig. 2): one on the glabella, two on the most prominent parts of the temporal line (Temp), one on the external occipital protuberance (EOP), three on spinous processes of the cervical vertebrae (C2, C4, and C7), one on the spinous process of T6, two on spinous processes of L1 and L3, two on the most prominent parts of the lateral sacral crest (S), two on the posterior superior iliac spine (PSIS), and two on the ASIS.
Fig. 2.
Sixteen markers were placed on the skin from head to pelvis: one on the glabella, two on the most prominent part of the temporal line (Temp), one on external occipital protuberance (EOP), six on spine spinous processes of the cervical vertebrae (C2, C4, C7, T6, L1 and L3), two on most prominent part of the lateral sacral crest (S), two on the posterior superior iliac spine (PSIS) and two on the anterior superior iliac spine (ASIS)
Modeling and data processing
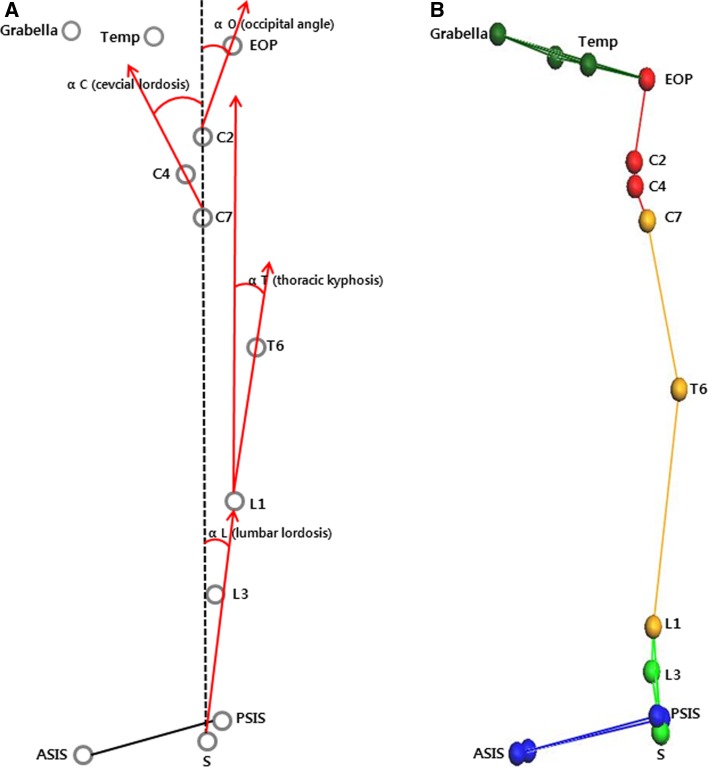
Three-dimensional data from the optoelectronic system were processed using Vicon Nexus 1.7 software (Vicon Motion Systems, Oxford, UK). Lumbar lordosis (αL) was defined by the angle formed by the intersection between the line joining C2 to S and line joining L1 to S, thoracic kyphosis (αT) as the angle formed by the intersection between the line joining C2 to S and the line joining L1 to T6, cervical lordosis (αC) the angle formed by the intersection between the line joining C2 to S and the line joining C7 to C4, and the occipital angle (αO) was defined as the angle formed by the intersection between the line joining C2 to S and line joining C2 to EOP (Fig. 3). We measured αL, αT, αC, and αO in a natural standing position, and when the naked eye, loupe, and out of loupe were used to visualize the surgical field and at three operating table heights (ASIS, U, U–S) during three surgical views (midline, ipsilateral, and contralateral) (Fig. 1).
Fig. 3.
Lumbar lordosis (αL) was defined as the angle between the line from C2 to S and line from L1 to S. Thoracic kyphosis (αT) was defined as the angle between the line from C2 to S and line from L1 to T6. Cervical lordosis (αC) was defined as the angle between the line from C2 to S and line from C7 to C4. Occipital angle (αO) was defined as the angle between the line from C2 to S and line from C2 to EOP (a). Skin marker on 3-dimensional model from motion analysis system also showed at b
Mean values for all parameters were computed, and SPSS for Windows (Version 15.0K; SPSS, Chicago, IL) was used for the statistical analysis. A 3 × 3 × 3 (operating table height × methods × tasks) analysis of variance with repeated measures was obtained. Kruskal–Wallis ANOVA and the Friedman test were used for comparison between nine variations (operating table height × methods × tasks) with natural standing position, and p values of <0.05 were considered significant.
Results
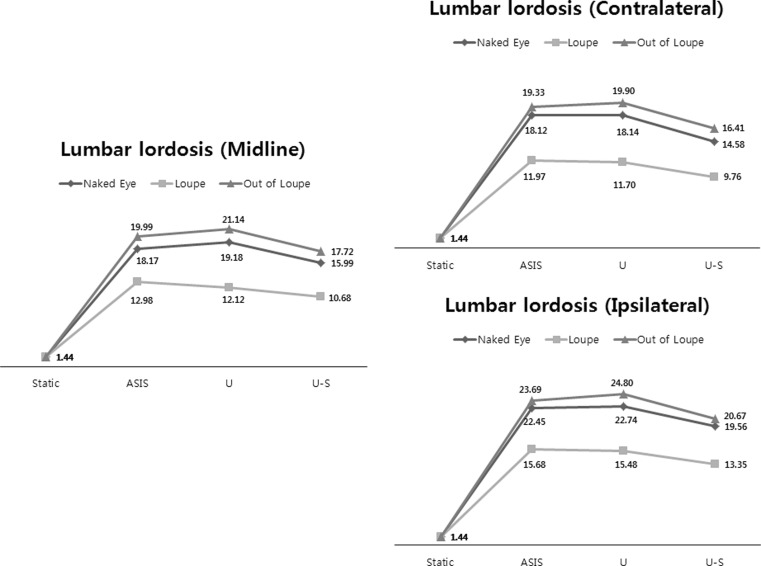
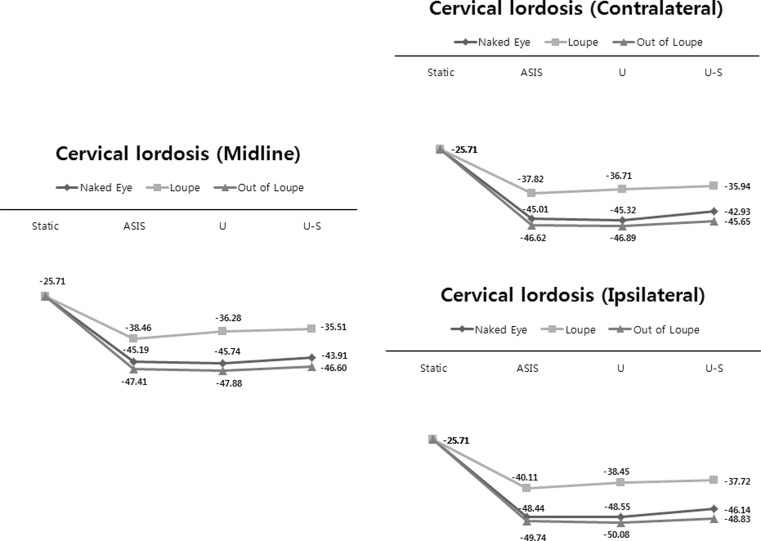
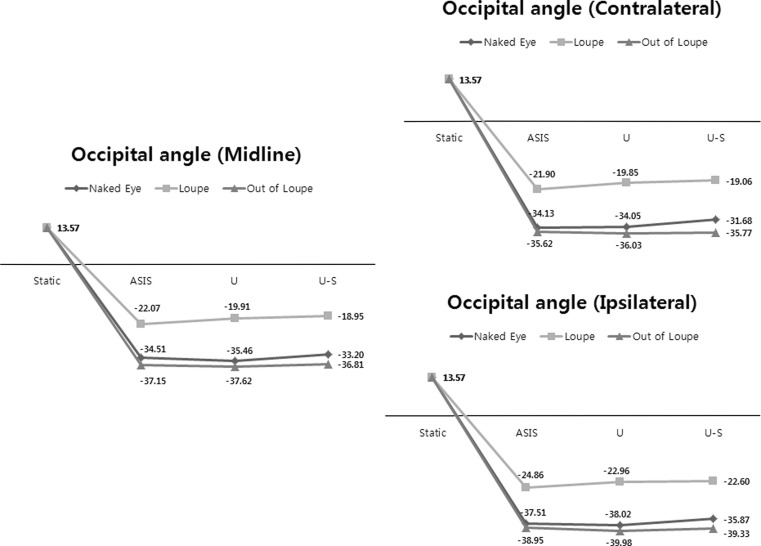
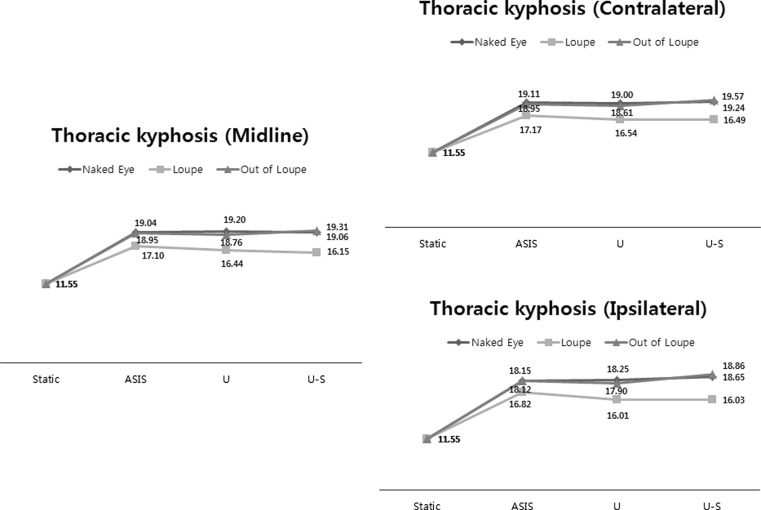
The mean values and standard deviations of all studied parameters are listed in Table 1. Head and whole spine angles were significantly different according to methods to visualize (naked eye, loupe, and out of loupe) during all surgical field views (midline, ipsilateral, and contralateral). The head and whole spine angles were different significantly for the different views with or without a loupe (Table 1). Lumbar lordosis (αL) with a loupe was closer to the natural standing position, but out of loupe was beyond the natural standing position (p < 0.05) (Fig. 4) (Table 1). Cervical lordosis (αC) and occipital angle (αO) with a loupe showed the same pattern as αL (p < 0.05) (Figs. 5, 6) (Table 1), and thoracic kyphosis (αT) with a loupe also was closer to the natural standing position, but beyond the natural standing position when discectomy was done with naked eye (p < 0.01) (Fig. 7; Table 1).
Table 1.
The mean values and the standard deviations of all parameters
| Anterior superior iliac spine | Umbilicus | Midpoint between umbilicus and sternum | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Contralateral | Midline | Ipsilateral | Contralateral | Midline | Ipsilateral | Contralateral | Midline | Ipsilateral | |||
| Lumbar lordosis (1.44 ± 2.65)† | |||||||||||
| Naked eye | 18.12 ± 3.47 | 18.17 ± 3.78 | 22.45 ± 3.87 | 18.14 ± 3.97 | 19.18 ± 3.46 | 22.74 ± 3.74 | 14.58 ± 3.37*b | 15.99 ± 3.43*b | 19.56 ± 3.72*b | ||
| Loupe*a | 11.97 ± 5.84 | 12.98 ± 5.70 | 15.68 ± 5.33 | 11.70 ± 6.67 | 12.12 ± 5.11 | 15.48 ± 5.21 | 9.76 ± 5.78**b | 10.68 ± 4.62*b | 13.35 ± 4.18 | ||
| Out of loupe | 19.33 ± 4.78 | 19.99 ± 4.97 | 23.69 ± 4.53 | 19.90 ± 5.78 | 21.14 ± 4.41 | 24.80 ± 4.90 | 16.41 ± 4.90**b | 17.72 ± 4.43**b | 20.67 ± 4.43**b | ||
| Thoracic kyphosis (11.55 ± 2.37)† | |||||||||||
| Naked eye | 19.11 ± 2.76 | 19.04 ± 2.87 | 18.15 ± 2.69 | 19.00 ± 2.36 | 19.20 ± 2.50 | 18.25 ± 2.04 | 19.24 ± 2.26 | 19.06 ± 2.16 | 18.65 ± 2.01 | ||
| Loupe**a | 17.17 ± 1.81 | 17.10 ± 1.79 | 16.82 ± 1.60 | 16.54 ± 1.59 | 16.44 ± 1.51 | 16.01 ± 1.28**b | 16.49 ± 1.51 | 16.15 ± 1.34 | 16.03 ± 1.22 | ||
| Out of loupe | 18.95 ± 3.38 | 18.95 ± 3.18 | 18.12 ± 2.99 | 18.61 ± 3.34**b | 18.76 ± 2.97**b | 17.90 ± 2.57**b | 19.57 ± 3.29 | 19.31 ± 2.94 | 18.86 ± 2.67 | ||
| Cervical lordosis (−25.71 ± 2.02)† | |||||||||||
| Naked eye | −45.01 ± 6.24 | −45.19 ± 6.55 | −48.44 ± 6.93 | −45.32 ± 5.79 | −45.74 ± 5.89 | −48.55 ± 6.49 | −42.93 ± 4.98**b | −43.91 ± 4.98 | −46.14 ± 4.60**b | ||
| Loupe*a | −37.82 ± 4.87 | −38.46 ± 4.67 | −40.11 ± 5.76 | −36.71 ± 4.59 | −36.28 ± 4.17 | −38.45 ± 5.16 | −35.94 ± 5.04**b | −35.51 ± 5.03*b | −37.72 ± 5.35**b | ||
| Out of loupe | −46.62 ± 5.71 | −47.41 ± 6.16 | −49.74 ± 6.90 | −46.89 ± 5.34 | −47.88 ± 5.48 | −50.08 ± 6.23 | −45.65 ± 5.02 | −46.60 ± 6.22 | −48.83 ± 5.67 | ||
| Occipital angle (13.57 ± 1.85)† | |||||||||||
| Naked eye | −34.13 ± 5.59 | −34.51 ± 5.60 | −37.51 ± 5.45 | −34.05 ± 4.48 | −35.46 ± 4.24 | −38.02 ± 3.87 | −31.68 ± 3.89 | −33.20 ± 3.18**b | −35.87 ± 2.70 | ||
| Loupe*a | −21.90 ± 5.82 | −22.07 ± 5.42 | −24.86 ± 5.87 | −19.85 ± 4.56 | −19.91 ± 3.96 | −22.96 ± 4.60 | −19.06 ± 5.26**b | −18.95 ± 5.15**b | −22.60 ± 4.61 | ||
| Out of loupe | −35.62 ± 4.72 | −37.15 ± 3.92 | −38.95 ± 4.37 | −36.03 ± 5.23 | −37.62 ± 4.35 | −39.98 ± 4.37 | −35.77 ± 4.52 | −36.81 ± 5.25 | −39.33 ± 3.85 | ||
aDifferences according to methods to see surgical field
bDifferences according to operating table height
* p < 0.01
** p < 0.05
† Static values
Fig. 4.
Lumbar lordosis (αL) measured during the three different visualize methods (naked eye, loupe, out of loupe) and during three different operating table heights (ASIS anterior superior iliac spine, U umbilicus, U–S midpoint of umbilicus and sternum) under three different views (midline, ipsilateral, and contralateral)
Fig. 5.
Cervical lordosis (αC) measured during the three different visualize methods (naked eye, loupe, out of loupe) and during three different operating table heights (ASIS anterior superior iliac spine, U umbilicus, U–S midpoint of umbilicus and sternum) under three different views (midline, ipsilateral, and contralateral)
Fig. 6.
Occipital angles (αO) measured during the three different visualize methods (naked eye, loupe, out of loupe) and during three different operating table heights (ASIS anterior superior iliac spine, U umbilicus, U–S midpoint of umbilicus and sternum) under three different views (midline, ipsilateral, and contralateral)
Fig. 7.
Thoracic kyphosis (αT) measured during the three different visualize methods (naked eye, loupe, out of loupe) and during three different operating table heights (ASIS anterior superior iliac spine, U umbilicus, U–S midpoint of umbilicus and sternum) under three different views (midline, ipsilateral, and contralateral)
In terms of operating table height, lumbar lordosis (αL) showed significant changes according to operation table height. As operating table height increased, lumbar lordosis (αL) was closer to the natural standing position during all three surgical field views (midline, ipsilateral, and contralateral) and during all methods to visualize (Fig. 4; Table 1). As operating table height increased, thoracic kyphosis (αT) was also closer to natural standing position, when simulation was conducted by loupe, but there was no statistical difference (Fig. 7; Table 1). If simulation was conducted by naked eye and out of loupe, thoracic kyphosis (αT) was closer to natural standing position, when operating table height was umbilicus. Cervical lordosis (αC) and occipital angle (αO) were significantly close to natural standing position as operating table height increased, but not when simulation was performed out of loupe (Figs. 5, 6; Table 1). As a result in operating table height increased, lumbar lordosis (αL), thoracic kyphosis (αT), cervical lordosis (αC), and occipital angle (αO) approached natural standing position values when simulation was conducted with loupe.
Discussion
Ergonomics during surgery has moved to the forefront during the last 20 years largely because of laparoscopic surgery, which is now commonly used because of its minimally invasive nature. In contrast to open surgery, during laparoscopic surgery surgeons usually use much longer instruments [7, 8] and tend to complain of musculoskeletal discomfort and fatigue of the lower back, neck, and shoulder because of the maintenance of a prolonged static posture and continuous isometric muscle contraction, which reduce muscle perfusion and cause muscle fatigue and pain [1, 9, 10]. Many studies have been conducted on the ergonomics of laparoscopic surgery, and the subject of ergonomics has been considered by surgeons in many fields [2, 3, 5, 11–14]. Previous studies have usually focused on leg fatigue, a large working area, extreme movements of the upper limbs and wrists, and stiffness of the neck [1, 2, 10, 15]. However, no study has been conducted on surgeon’s spine or head motion, although they are importantly associated with surgeons’ complaints of musculoskeletal discomfort and fatigue of the lower back, neck, and shoulder [1, 6]. Accordingly, this is the first study to be conducted on the motion and disposition of the whole spine and head during surgery during different operating situations.
Technologies that function in three dimensions and use multiple sensors allow for the simultaneous measurements of motions across multiple spine levels. Furthermore, the reliability of 3-D optoelectronic system data has already been demonstrated [16, 17]. In the present study, we used 3-D motion analysis, a 16-camera system, and 16 skin markers to determine whole spine and head motion changes during different operating situations during spinal surgery.
Previous laparoscopic and dental studies have established that a surgeon’s posture is affected by five factors, that is, the height of the operating table, the magnification method used, instrument design, monitor position, and foot pedal position [12, 14, 18]. Of these factors, both operating table height and magnification method associated with general spine surgery, and we analyzed whole spine and head motions and angles according to visualization methods (naked eye with or without spectacles, loupe, and out of loupe) (Fig. 8) at three operating table heights (ASIS, U and U–S). It was found that lumbar lordosis (αL), thoracic kyphosis (αT), cervical lordosis (αC), and occipital angle (αO) were close to those in a natural standing position when discectomy was performed with a loupe. Branson et al. previously reported that the use of magnification lenses while performing dental procedures may increase quality of work and that their use has the potential to prevent, or in some cases eliminate, chronic neck and back pain [12, 19, 20]. Furthermore, a strong relationship exists between head working angle and neck muscle fatigue, and when a surgeon uses a magnification loupe head tilt angle decreases (Fig. 8) [21]. The present study shows that the use of a loupe during spine surgery also directly influences cervical, lumbar, and thoracic angles.
Fig. 8.
Head tilt angle during discectomy simulation during the three different methods used to visualize the surgical field: naked eye (a), loupe (b), out of loupe (c)
In terms of operating table height, an optimum table height for laparoscopic surgery should position the laparoscopic instrument handles close to the surgeon’s elbow level to minimize discomfort and upper arm and shoulder muscle work [11, 22]. In this study, we set the highest table height at the midpoint between the umbilicus and sternum (U–S), which is usually at elbow level. Thus, based on our findings, we recommend that the operating table height should be located at the midpoint between the umbilicus and sternum during spine surgery. Upper arm and shoulder muscle stress are also importantly associated with fatigue and pain during surgery, and thus, to determine optimum table heights for spinal surgery, additional studies are required on arm and shoulder motions.
This study has several limitations. We decided to define lumbar lordosis (αL) as the angle formed by the intersection between the line from C2 to S and line from L1 to S, thoracic kyphosis (αT) as the angle formed by the intersection between the line from C2 to S and the line from L1 to T6, cervical lordosis (αC) as the angle formed by the intersection between the line from C2 to S and the line from C7 to C4, and occipital angle (αO) as the angle formed by the intersection between the line from C2 to S and line from C2 to EOP (Fig. 3). Actually, these measurements differ from real lumbar lordosis, thoracic kyphosis, cervical lordosis, and occipital angle. In order to decide spines and head angles at 3-D optoelectronic system, we selected marker attachment sites, after considering whole spine radiographs and skin surface anatomy which we can touch bony structures. To determine precise cervical, thoracic, and lumbar angles, spine endplate angles are needed, but it is impossible to measure endplate angles in real time during spine surgery simulation. Although cervical, thoracic, and lumbar angles using 3-D data obtained from optoelectronic systems may differ from real bony spine angles, they can reflect changes in spinal angle during spinal surgery simulations. To determine more precisely spinal and occipital angles, we need new methods which can measure exact spine motion and angle with real time. In addition, we do not include the microscope to analysis. During using microscope, surgeon’s neck positions can be adjusted to close with natural standing position. However, to include microscope, we must install 16 motion analysis cameras at operating room or move the microscope to lap. IRB did not accept to install camera at operating room due to contamination, so we will do additional study including the microscope after move the microscope to lap.
Conclusions
We suggest that the use of a loupe and a table height at the midpoint between the umbilicus and sternum is good for surgeon during spine operation. The table height was good as higher in aspect of ergonomically until midpoint between umbilicus and sternum, and spine operation with loupe was also good in aspect of whole spine angle. This simulation can be used as a guide for young surgeons to protect their spinal alignment during surgery.
Acknowledgments
This work was supported by a faculty research grant from Yonsei University College of Medicine in 2011 (Grant No. 6-2011-0118).
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Det MJ, Meijerink WJ, Hoff C, Tott ER, Pierie JP. Optimal ergonomics for laparoscopic surgery in minimally invasive surgery suites: a review and guidelines. Surg Endosc. 2009;23:1279–1285. doi: 10.1007/s00464-008-0148-x. [DOI] [PubMed] [Google Scholar]
- 2.Lee G, Lee T, Dexter D, Godinez C, Meenaghan N, Catania R, Park A. Ergonomic risk associated with assisting in minimally invasive surgery. Surg Endosc. 2009;23:182–188. doi: 10.1007/s00464-008-0141-4. [DOI] [PubMed] [Google Scholar]
- 3.Tse MA, Masters RS, McManus AM, Lo CY, Patil NG. Trunk muscle training, posture fatigue, and performance in laparoscopic surgery. J Endourol. 2008;22:1053–1058. doi: 10.1089/end.2007.0409. [DOI] [PubMed] [Google Scholar]
- 4.Keyserling WM. A computer-aided system to evaluate postural stress in the workplace. AIHA J. 1986;47:641–649. doi: 10.1080/15298668691390377. [DOI] [PubMed] [Google Scholar]
- 5.Albayrak A, Veelen MA, Prins JF, Snijders CJ, Ridder H, Kazemier G. A newly designed ergonomic body support for surgeons. Surg Endosc. 2007;21:1835–1840. doi: 10.1007/s00464-007-9249-1. [DOI] [PubMed] [Google Scholar]
- 6.Mirbod SM, Yoshida H, Miyamoto K, Miyashita K, Inaba R, Iwata H. Subjective complaints in orthopedists and general surgeons. Int Arch Occup Environ Health. 1995;67:179–186. doi: 10.1007/BF00626350. [DOI] [PubMed] [Google Scholar]
- 7.Matern U. Ergonomic deficiencies in the operating room: examples from minimally invasive surgery. Work. 2009;33:165–168. doi: 10.3233/WOR-2009-0862. [DOI] [PubMed] [Google Scholar]
- 8.Berguer R, Forkey DL, Smith WD. Ergonomic problems associated with laparoscopic surgery. Surg Endosc. 1999;13:466–468. doi: 10.1007/PL00009635. [DOI] [PubMed] [Google Scholar]
- 9.McGill SM, Hughson RL, Parks K. Lumbar erector spinae oxygenation during prolonged contractions: implications for prolonged work. Ergonomics. 2000;43:486–493. doi: 10.1080/001401300184369. [DOI] [PubMed] [Google Scholar]
- 10.Kant IJ, Jong LC, Rijssen-Moll M, Borm PJ. A survey of static and dynamic work postures of operating room staff. Int Arch Occup Environ Health. 1992;63:423–428. doi: 10.1007/BF00386939. [DOI] [PubMed] [Google Scholar]
- 11.Berquer R, Smith WD, Davis S. An ergonomic study of the optimum operating table height for laparoscopic surgery. Surg Endosc. 2002;16:416–421. doi: 10.1007/s00464-001-8190-y. [DOI] [PubMed] [Google Scholar]
- 12.Branson BG, Bray KK, Gadbury Amyot C, Holt LA, Keselyak NT, Mitchell TV, Williams KB (2004) Effect of magnification lenses on student operator posture. J Dent Eedu 68:384–389 [PubMed]
- 13.Dajpratham P, Ploypetch T, Kiattavorncharoen S, Boonsiriseth K. Prevalence and associated factors of musculoskeletal pain among the dental personnel in a dental school. Chot Mai Het Thang Phaet. 2010;93:714–721. [PubMed] [Google Scholar]
- 14.Kaya OI, Moran M, Ozkardes AB, Taskin EY, Seker GE, Ozmen M. Ergonomic problems encountered by the surgical team during video endoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2008;18:40–44. doi: 10.1097/SLE.0b013e3181569ee2. [DOI] [PubMed] [Google Scholar]
- 15.Kranenburg Gossot. Ergonomic problems encountered during video-assisted thoracic surgery. Minim Invasive Ther Allied Technol. 2004;13:147–155. doi: 10.1080/13645700410033661. [DOI] [PubMed] [Google Scholar]
- 16.Preuss RA, Popovic MR. Three-dimensional spine kinematics during multidirectional, target-directed trunk movement in sitting. J Electromyogr Kinesiol. 2010;20:823–832. doi: 10.1016/j.jelekin.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 17.Vismara L, Menegoni F, Zaina F, Galli M, Negrini S, Capodaglio P. Effect of obesity and low back pain on spinal mobility: a cross sectional study in women. J Neuroeng Rehabil. 2010;7:3. doi: 10.1186/1743-0003-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van V, Jakimowicz, Kazemier (2004) Improved physical ergonomics of laparoscopic surgery. Minim Invasive Ther Allied Technol 13:161–166 [DOI] [PubMed]
- 19.Mamoun JS. A rationale for the use of high-powered magnification or microscopes in general dentistry. Gen Dent. 2009;57:18–26. [PubMed] [Google Scholar]
- 20.Maggio MP, Villegas H, Blatz MB. The effect of magnification loupes on the performance of preclinical dental students. Quintessence Int. 2011;42:45–55. [PubMed] [Google Scholar]
- 21.Chang BJ. Ergonomic benefits of surgical telescope systems: selection guidelines. J Calif Dent Assoc. 2002;30:161–169. [PubMed] [Google Scholar]
- 22.Veelen MA, Kazemier G, Koopman J, Goossens RH, Meijer DW. Assessment of the ergonomically optimal operating surface height for laparoscopic surgery. J Laparoendosc Adv Surg Tech. 2002;12:47–52. doi: 10.1089/109264202753486920. [DOI] [PubMed] [Google Scholar]