Abstract
Introduction
Dynamic stabilization of the spine was developed as an alternative to rigid fusion in chronic back pain to reduce the risk of adjacent segment degeneration. Dynamic neutralization system (Dynesys, Zimmer CH) is one of the most popular systems available, but some midterm studies show revision rates as high as 30 %. Some late infectious complications in our patients prompted us to review them systematically. Propionibacterium recently has been shown to cause subtle infections of prosthetic material.
Materials and methods
Here, we report on a consecutive series of 50 Dynesys implants. In a median follow-up of 51 months (range 0–91), we identified 12 infectious and 11 non-infectious complications necessitating reoperation or removal of the implant in 17 patients.
Results
Material infections occurred after a median of 52 months (2–77) and were due to Propionibacterium alone (n = 4) or in combination (n = 3) in seven out of 11 patients. Clinical presentation combines new or increasing pain associated with signs of screw loosening on conventional X-rays; however, as many as 73.5 % of patients present some degree of screw loosening without being at all symptomatic of infection.
Conclusion
The high rate of late infections with low-grade germs and the frequency of screw loosening signs made us suspect a lack of integration at the bone-screw interface. Surgeons should be suspicious if the patient presents a combination of new or increasing pain and signs of screw loosening, and aggressive revision is recommended in these cases.
Keywords: Infection, Propionibacterium, Dynesys, Complications
Introduction
In the past 20 years, dynamic stabilization of the spine has arisen as an alternative concept to rigid fusion in chronic back pain due to lumbar degenerative spinal disease or segmental hypermotility [2, 11, 12, 14, 17]. Dynamic neutralization system (Dynesys, Zimmer CH) was developed as an alternative to rigid fusion to prevent adjacent level disc degeneration, presumably due to adjacent segment hypermotility; to avoid donor site pain as well as other well-known complications of fusion surgery; and is one of the most popular systems available [1, 9, 15]. Many short- and mid-term follow-up studies have shown good results [18, 19]. However, some authors reported revision surgery rates as high as 30 % [3, 6, 8, 21]. No study has proven a restoration of physiologic weight balance or a protective effect on adjacent segments degeneration [13, 15, 19, 20].
Propionibacterium has been identified as a cause of prosthetic joint infections with subtle clinical presentation [22]. In a 10-year retrospective audit on instrumented spinal fusion, Collins et al. [4] showed that almost half of all the material infections were due to Propionibacterium and occurred as late as 5 years after surgery, exclusively after a posterior approach to the spine. However, the global incidence of infection remained low at 3.7 % (74/1,980 patients). Propionibacterium acnes is a slow-growing, aerotolerant anaerobic gram-positive bacterium. It is part of the normal skin flora and is known to be linked to skin condition acne. We were confronted with a series of late infectious complications in our patients, which prompted us to review them systematically.
Materials and methods
We identified all patients who had a dynamic stabilization of the lumbar spine with the Dynesys system. Two senior spine surgeons in two hospitals did all operations and performed most of these together. Basic demographic data from the patients were collected. Their case notes and X-ray files were reviewed. Each patient completed a visual analogue scale for back pain (VAS-BP) and leg pain (VAS-LP), as well as the Oswestry disability index (ODI) at their last clinical follow-up or by direct phone contact. Radiologic follow-up and clinical follow-up times were noted separately. All patients presenting with either new or increasing lumbar pain with a halo on their X-ray were re-operated on to remove implants and to perform bacteriological analysis. All microbiology findings were reported. All tissue samples were bred for up to 14 days to allow slow-growing bacteria to be identified, especially the Propionibacterium species.
The implantation of the Dynesys system is systematically performed with the patient in prone position through a midline incision or a Wiltse approach. The patients receive general anaesthesia, and a prophylactic antibiotic therapy with Cefuroxime is started at the induction of anaesthesia and is continued for 48 h. Intraoperative protection of the implant was applied to reduce skin contamination. The technical aspects of implantation followed the surgical technique recommended by the manufacturer without inter-somatic cages. All screws used were of first generation (non coated) and at least 6 mm in diameter. Patients were allowed to walk on day one under physiotherapeutic coaching. Regular radiologic and clinical follow-ups are mandatory at 3, 6, 12, 18 and 24 months or on demand. All patients were contacted at the time of study. Only those with new or increasing pain were recruited for clinical and radiological exams.
Descriptive statistics was used to present basic demographic data. The student’s t test and the Fisher’s exact test were used as required.
Results
Between May 2002 and September 2008, 50 consecutive Dynesys implants were performed in 49 patients (one patient received a second operation with Dynesys 1 year after removal of implant due to early infection). All operated patients had low back pain resistant to at least 6 months of conservative treatment. Indication for surgery was lumbar low-grade instability in 16 patients and discopathy in 34 patients. Sixteen patients (32 %) had prior lumbar surgery, most of them micro-discectomy for disc herniation or fusion of neighbouring segments. The total number of implanted screws was 342 and the median screw diameter was 6 mm (range 6–7.2 mm). Thirty screws (8.77 %) in 21 patients (42 %) needed to be corrected with respect to deepness after fluoroscopic control during their initial operation. The total clinical follow-up was 57.5 months (range 6–91 months). There were seven patients (14 %), whom we could not reach to assess VAS-BP, VAS-LP and ODI scores. For those patients, we used the information obtained and X-rays performed at the last clinical control. Demographic data are summarized in Table 1.
Table 1.
Demographics
| Number of operations | 50 | 1 patient operated twice |
| Number of patients | 49 | |
| Sex ratio: women/men (%) | 24 (48)/26 (52) | |
| Age at operation (years) | 49 (29–72) | Median (range) |
| BMI | 26 kg/m2 (19.4–37.6) | Median (range) |
| Smoker status (0/1/2) (one missing data) | 25/05/19 | 0 = never, 1 = <10/day, 2 = >10/day |
| Total clinical follow-up | 57.5 months (6–91) | Median (range) |
| Last follow-upa | 51 months (0–91) | Median (range) |
| Indication | ||
| Instability | 16 patients (32 %) | |
| Discopathy | 34 patients (68 %) | |
| Operation time | 135 min (70–295) | Median (range) |
| Previous lumbar surgery | 16 patients (32 %) | |
| Number of segments | ||
| 1 segment | 14 patients | |
| 2 segments | 16 patients | |
| 3+ segments | 20 patients | |
| Lowest segment | ||
| S1 | 32 patients | Median 3 segments (1–6) |
| L5 | 13 patients | Median 1 segment (1–4) |
| L3–4 | 5 patients | Median 1 segment (1–2) |
| Total screws | 342 (6 mm = 272, 6.4 mm = 68, 7.2 mm = 2) | |
| Deepness correction of screw | 30 screws (8.77 %) in 21 patients (42 %) | |
| Radiological follow-up | 24 months (1–77) | 1 patient lost X-rays |
| Analyzed screws | 328 | 1 patient lost to follow-up |
| Signs of loosening (halo) | 103 screws/328 (31.4 %) | 36 patients/49 (73.5 %) |
a Until first complication or last consultation (completion of VAS-BP, VAS-LP pain, and ODI scores)
Thirty-three patients had no complications at last follow-up; 23 complications necessitated operative revision among 17 patients; 12 complications (11 patients) were infectious and 11 (seven patients) non-infectious (see Tables 2 and 3). One patient had a mechanical complication after 10 months and a material infection after 65 months and, therefore, was counted in both groups but analyzed with the infection group. The infectious problems were diagnosed after a median period of 52 months, compared with a median of 13 months for the non-infectious complications. Four patients needed two follow-up operations, and one patient underwent three follow-up operations due to subsequent complications. One infectious complication necessitating removal of material occurred 2 months after the first operation and 1 month after wound debridement. The bacterium found was Staphylococcus aureus. In two cases material infection (Staphylococcus epidermidis at 54 months/Propionibacterium at 18 months) followed repetitive steroid infiltrations. The other infections occurred much later and had an insidious clinical presentation, mostly recurrent or increasing pain in combination with signs of screw loosening on follow-up radiological exams (see Fig. 1). Only one patient had classical signs of infection with fever, night sweats, high white blood cell counts and elevated C-reactive protein. The germs isolated during implant removal are summarized in Table 4.
Table 2.
Patients and timing of complications
| Compl. no | Pat. no | Indications for revision | Time to reop. (months) |
|---|---|---|---|
| 1 | 2 | Screw loosening and migration (L3 right, L5 bilateral) | 41 |
| 2 | 6 | Pseudarthrosis of operated segment (L4–L5) | 13 |
| 3 | Decompensation of adjacent segment (L3–L4) | 58 | |
| 4 | 7 | Root compression of operated segment (L5 left) | 2 |
| 5 | Pseudarthrosis of operated segment (L4–L5) | 26 | |
| 6 | 8 | Wound infection | 1 |
| 7 | Material infection (L2 right) | 2 | |
| 8 | 10 | Material infection (Dynesys cord right) | 52 |
| 9 | 14 | Decompensation of operated segment (L5–S1 right) | 0 |
| 10 | Root compression of operated segment (L5 right) | 1 | |
| 11 | Instability of operated segment (L4–S1) | 15 | |
| 12 | 16 | Cortical perforation of operated segment (L4 right) | 1 |
| 13 | 20 | Material infection | 52 |
| 14 | 21 | Material infection (L3–S1 and Dynesys cord) | 44 |
| 15 | 24 | Material infection (Dynesys cord left) | 60 |
| 16 | 28 | Screw fracture (L2 left) | 10 |
| 17 | Material infection (L2–L5) | 65 | |
| 18 | 34 | Material infection (L5 right) | 57 |
| 19 | 35 | Screw fracture and suspicion of infection (L4 right) | 52 |
| 20 | 36 | Material infection with migration of screw (S1 left) | 47 |
| 21 | 37 | Material infection (S1 left) | 54 |
| 22 | 46 | Material infection (L4–S1 and Dynesys cord) | 77 |
| 23 | 48 | Material infection (L2–S1 and Dynesys cord) | 18 |
Compl complication, no number, pat patient, reop reoperation
Table 3.
Indications for revision surgery
| Number of complications (number of patients) | Postoperative time (months in range) | |
|---|---|---|
| 23 complications in 17 patientsb | ||
| Infectious | 12 (11)b | Median 52 (1–77) |
| Wound infection | 1 patient (Staphylococcus aureus) | 1 month |
| Material infection | 11 patients | Median 52 (2–77) |
| Non-infectious | 11 (7)b | Median 13 (0–58) |
| Screw loosening and migration | 1 | 41 |
| Pseudarthrosis | 2 | 13 and 26 |
| Decompensation of adjacent segment | 1 | 58 |
| Decompensation of operated segment | 1 | 0 |
| Root compression | 2 | 1 and 2 |
| Cortical perforation | 1 | 1 |
| Screw fracture | 1 | 10 |
| Screw fracture with suspicion of infection | 1 | 52a |
| Instability | 1 | 15 |
a Indication for revision surgery given, patient not re-operated
b Patient 28 had first a mechanical complication, followed by an infectious complication (see Table 2)
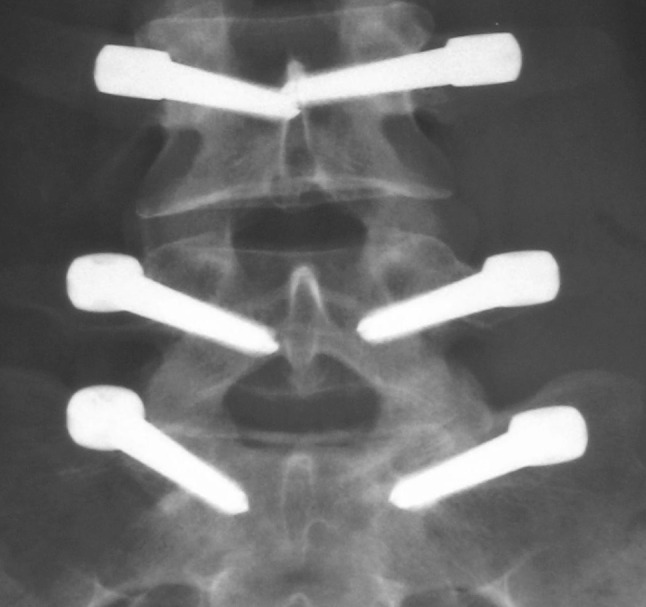
Fig. 1.

Double halo L2 left + right, L5 left, S1 right, simple halo L3 left; posterior–anterior view; left on right side of picture
Table 4.
Microbiology results in material infections
| Number of patients | Postoperative time (months in range) | |
|---|---|---|
| All material infections | 11 | Median 52 (2–77) |
| Staphylococcus aureus | 1 | 2a |
| Staphylococcus epidermidis | 2 | 47 and 54 |
| Propionibacterium acnes | 4 | 18, 52, 57 and 77 |
| Propionibacterium acnes and mixed infectionb | 3 | 44, 52 and 65 |
| Gram positive Coccic | 1 | 60 |
a This patient had a wound infection at 1 month postoperation
b Concomitant infections were Staphylococcus epidermidis, Staphylococcus haemolyticus, Streptococcus oralis and Staphylococcus coagulase negative
c Identification of bacteria was not possible
Seven out of 11 patients (63.6 %) had single or combined infections with Propionibacterium acnes. One late infection (60 months) was probably also due to Propionibacterium: The gram coloration was positive, but the culture was unable to identify the bacterium, even after a 14-day breeding period. Other germs involved in late infections were Staphylococcus epidermidis, alone or in combination, as well as Staphylococcus haemolyticus, Streptococcus oralis and Staphylococcus coagulase negative in combination with Propionibacterium.
Mechanical complications are summarized in Table 3.
The re-operated group (all causes) was significantly younger (Mage = 43 vs. 50.5 years), and the duration of the initial operation skin to skin was significantly longer (M = 163 vs. 135 min., see Table 5). This difference in operation length also was seen in the comparison between infected and non-infected patients (168 vs. 138 min., see Table 6). The number of segments operated was equal (M = 2.4 levels) and did not explain this difference in duration. All other preoperative parameters were similar, especially smoker status, body mass index, indication for surgery and previous lumbar operation status. As expected, the re-operated and infected group performed worse in regards to VAS-BP, VAS-LP and ODI scores at the last clinical follow-up, but the difference was only significant for VAS-BP between re-operated and non-operated patients (p = 0.035).
Table 5.
Comparison between revised and non-revised cases
| Non-re-operated (n = 33) | Re-operated (n = 17) | p | |
|---|---|---|---|
| Male/female | 16/17 | 10/7 | 0.559b |
| Age (mean) years | 50.5 | 43 | 0.028a |
| OP-time (mean) min. | 135 | 163 | 0.041a |
| Indication (instability/discopathy) | 11/22 | 5/12 | 1.000b |
| Previous lumbar operation (year/n) | 11/22 | 5/12 | 0.723b |
| Screw corrections (year/n) | 13/20 | 8/9 | 0.412b |
| Number of segments (mean) | 2.42 | 2.41 | 0.974a |
| BMI (mean) | 27.5 | 27 | 0.719a |
| Smoker status (year/n) | 19/13c | 5/12 | 0.989b |
| VAS-BP (mean) | 4.18 | 6.2 | 0.035a |
| VAS-LP (mean) | 3.89 | 4.73 | 0.398a |
| ODI score (mean) | 31.75 | 46 | 0.068a |
| Halo on X-ray (year/n) | 22/10c | 14/3 | 0.249b |
| Mean follow-up (months) | 47.5 | 34.2 | 0.063a |
Significant p-values are in italics
at test, b Fisher’s exact test, c one missing data
Table 6.
Comparison between infected and non-infected material cases
| Non-infected (n=39) | Infected (n=11) | p | |
|---|---|---|---|
| Male/female | 18/21 | 8/3 | 0.175b |
| Age (mean) years | 49.6 | 42.1 | 0.055a |
| OP-time (mean) min. | 138 | 168 | 0.048a |
| Indication (instability/discopathy) | 12/27 | 4/7 | 0.728b |
| Previous lumbar operation (year/n) | 12/27 | 4/7 | 0.767b |
| Screw corrections (year/n) | 16/23 | 5/6 | 0.529b |
| Number of segments (mean) | 2.41 | 2.45 | 0.920a |
| BMI (mean) | 27.7 | 26.1 | 0.391a |
| Smoker status (year/n) | 20/18c | 4/7 | 0.273a |
| VAS-BP (mean) | 4.55 | 6 | 0.186a |
| VAS-LP (mean) | 4.18 | 4.2 | 0.987a |
| ODI score (mean) | 33.9 | 45.8 | 0.184a |
| Halo on X-ray (year/n) | 27/11c | 9/2 | 0.866b |
| Mean follow-up (months) | 43 | 42.9 | 0.989a |
Significant p-value is in italics
at test, b Fisher’s exact test, c one missing data
Most of the patients had clinical improvement after removal of material and resolution of infection, which necessitated long antibiotic therapy and no need for new instrumentation.
Median radiological follow-up after implantation of Dynesys with conventional X-rays was 24 months, with a broad range from 1 to 77 months. This is explained by the fact that some patients were re-operated on early, others were missing at follow-up and some patients had other radiologic modalities at follow-up. A total of 328 screws were analyzed, and 103 showed signs of loosening (simple or double halo sign, see Fig. 1). Thirty six out of 49 patients (73.5 %) had at least one loose screw on follow-up X-rays, and only 13 patients had all screws well integrated (see Fig. 2).
Fig. 2.
No halo; posterior–anterior view; left on right side of picture
Discussion
This retrospective study achieved good data retrieval with only seven patients out of 50 (14 %) who were not available for clinical or telephonic assessment at last follow-up. The total observation time of nearly 5 years (Median = 57.5 months) also allows us to draw long-term conclusions. Our results at last follow-up (MODI = 36.7 %) were comparable to results after rigid fusion [7], and our VAS-BP of 4.8 and VAS-LP of 4.2 were similar to results obtained by Grob et al. after Dynesys implant [8]. Nevertheless, we could confirm our initial supposition of high incidence of late material infections in our patients.
Our revision rate of 34 % (17/50 patients), even if in the upper range, was comparable to that in the literature [3, 6, 8] and was explained by the long follow-up time in our study. What is new, to our knowledge, is the high incidence of infections (22 %) and especially their late presentation with a median of 52 months, peaking at 77 months. Excluding one early infection at 2 months that classically followed a wound infection with Staphylococcus aureus, and one mid-term infection with Propionibacterium at 18 months following repetitive infiltrations of the iliosacral joint, all other infections occurred after almost 4 years. Our clinical experience and case management is similar to that of Collins et al.. [4]. In most cases, a combination of recurrent or persistent lumbar pain with radiological signs of material loosening or a broken screw prompted the indication for revision surgery. Only one patient presented with classical symptoms of infection (night sweats, elevated white blood cells count, and C-reactive protein). The proportion of Propionibacterium infections was high (7/11 patients), but the spectrum of pathogens was still comparable to Collins et al.’s work. Additionally, in our experience, Propionibacterium is not only a contaminant, but also a germ with a clear pathogenicity for spinal implants, as confirmed by Gram-positive probe staining in this study. Interestingly, another study about deep surgical infections after spinal fusion [16] did not find Propionibacterium as a causative organism, confirming the difficulty of breeding this germ [22]. We found the same correlation between infectious risk and length of operation, but not with smoking habits or the number of operated levels [16]. And, in opposition to our results, almost all infections occurred early with a median postoperative time of 13.5 days.
Among the preoperative parameters evaluated, we found no criteria that could help restrict the indication for Dynesys to a more favourable subgroup. Predictive factors are difficult to assess [10]. Bothmann et al. [3] described a tendency toward more screw loosening in younger patients. In our study, younger age was associated with a less favourable outcome without showing more screw loosening on conventional X-rays. Dakhil-Jerew et al. [5] suggested using the “double halo sign” to describe screw loosening. Even if they showed that this sign was associated with better inter-observer reliability, we think that, in the presence of new or increasing pain, every sign of screw loosening must be scrutinized and confirmed with a computed tomography or SPECT.
We do not have an explanation for the high rate of long-term infections observed in our patients. In view of the frequency of signs of screw loosening observed (73.5 %, 36/49 patients), we hypothesize that there is a biomechanical lack of integration at the bone-screw interface probably due to the screw design. This could eventually lead to a chronic inflammation with a “dead space” prone to opportunistic skin-flora super infection and should be cleared in further animal or experimental studies. Meanwhile, new screws coated with hydroxyapatite have been developed by the same manufacturer to achieve better tissue integration, and they may reduce the risk of screw loosening. This needs further study to confirm.
Finally, systematic implant removal after a 3-year period remains an open question in our group.
Conclusion
In this small series of patients, we detected an abnormal level of late infections. We did not find any correlation with the screw diameter or operated levels. We found a slightly longer operation time in the infected group, but we do not think that a perioperative contamination explained those late infections.
Biomechanical design of the screw could be the main factor of poor screw-bone integration.
We strongly advise performing long-term follow-up on patients implanted with Dynesys and removing implants in patients with new or increasing pain and radiological signs of screw loosening.
Conflict of interest
None.
References
- 1.Beastall J, Karadimas E, Siddiqui M, Nicol M, Hughes J, Smith F, Wardlaw D. The Dynesys lumbar spinal stabilization system: a preliminary report on positional magnetic resonance imaging findings. Spine (Phila Pa 1976) 2007;32:685–690. doi: 10.1097/01.brs.0000257578.44134.fb. [DOI] [PubMed] [Google Scholar]
- 2.Benezech J, Mitulescu A. Retrospective patient outcome evaluation after semi-rigid stabilization without fusion for degenerative lumbar instability. Eur J Orthop Surg Traumatol. 2007;17:227–234. doi: 10.1007/s00590-006-0186-9. [DOI] [Google Scholar]
- 3.Bothmann M, Kast E, Boldt GJ, Oberle J. Dynesys fixation for lumbar spine degeneration. Neurosurg Rev. 2008;31:189–196. doi: 10.1007/s10143-007-0101-9. [DOI] [PubMed] [Google Scholar]
- 4.Collins I, Wilson-MacDonald J, Chami G, Burgoyne W, Vineyakam P, Berendt T, Fairbank J. The diagnosis and management of infection following instrumented spinal fusion. Eur Spine J. 2008;17:445–450. doi: 10.1007/s00586-007-0559-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dakhil-Jerew F, Jadeja H, Cohen A, Shepperd JAN. Inter-observer reliability of detecting Dynesys pedicle screw using plain X-rays: a study on 50 post-operative patients. Eur Spine J. 2009;18:1486–1493. doi: 10.1007/s00586-009-1071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davis R, Delamarter R, Maxwell J, Welch W, Wingate J, Sherman J (2009) Preliminary 3-year results from a prospective, randomized, controlled IDE study of the Dynesys dynamic stabilization system. In: Abstracts of the 24th annual meeting of the North American spine society, San Francisco, 10–17 Nov 2009, The Spine J, 86S
- 7.Faundez AA, Schwender JD, Safriel Y, Gilbert ThJ, Mehbod AA, Denis F, Transfeldt EE, Wroblewski JM. Clinical and radiological outcome of anterior-posterior fusion versus trans-foraminal lumbar interbody fusion for symptomatic disc degeneration: a retrospective comparative study of 133 patients. Eur Spine J. 2009;18:203–211. doi: 10.1007/s00586-008-0845-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine. Spine. 2005;30:324–331. doi: 10.1097/01.brs.0000152584.46266.25. [DOI] [PubMed] [Google Scholar]
- 9.Lee ChS, Hwang ChJ, Lee SW, Ahn YJ, Kim YT, Lee DH, Lee MY. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J. 2009;18:1637–1643. doi: 10.1007/s00586-009-1060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mannion AF, Elfering A. Predictors of surgical outcome and their assessment. Eur Spine J. 2006;15:S93–S108. doi: 10.1007/s00586-005-1045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mullholland RC, Sengupta DK. Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J. 2002;11:S198–S205. doi: 10.1007/s00586-002-0422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mullholland RC. The myth of lumbar instability: the importance of abnormal loading as a cause of low back pain. Eur Spine J. 2008;17:619–625. doi: 10.1007/s00586-008-0612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Putzier M, Hoff E, Tohtz S, Gross C, Perka C, Strube P. Dynamic stabilization adjacent to single-level fusion: part II. No clinical benefit for asymptomatic, initially degenerated adjacent segments after 6 years follow-up. Eur Spine J. 2010;19(12):2181–2189. doi: 10.1007/s00586-010-1517-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reyes-Sánchez A, Zárate-Kalfópulos B, Ramírez-Mora I, Rosales-Olivarez LM, Alpizar-Aguirre A, Sánchez-Bringas G. Posterior dynamic stabilization of the lumbar spine with the Accuflex rod system as a stand-alone device: experience in 20 patients with 2-year follow-up. Eur Spine J. 2010 doi: 10.1007/s00586-010-1417-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.St Schaeren, Broger I, Jeanneret B. Minimum 4-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine. 2008;33:E636–E642. doi: 10.1097/BRS.0b013e31817d2435. [DOI] [PubMed] [Google Scholar]
- 16.Schimmel JJP, Horsting PP, Kleuver M, Wonders G, Limbeck J. Risk factors for deep surgical site infections after spinal fusion. Eur Spine J. 2010;19:1711–1719. doi: 10.1007/s00586-010-1421-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwarzenbach O, Berlemann U, Stoll ThM, Dubois G. Posterior dynamic stabilization systems: Dynesys. Orthop Clin N Am. 2005;36:363–372. doi: 10.1016/j.ocl.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Schwarzenbach O, Rohrbach N, Berlemann U. Segment-by-segment stabilization for degenerative disc disease: a hybrid technique. Eur Spine J. 2010;19:1010–1020. doi: 10.1007/s00586-010-1282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stoll ThM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J. 2002;11:S170–S178. doi: 10.1007/s00586-002-0438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Strube P, S Tohtz, Hoff E, Gross C, Perka C, Putzier M. Dynamic stabilization adjacent to single-level fusion: part I. Biomechanical effects on lumbar spinal motion. Eur Spine J. 2010 doi: 10.1007/s00586-010-1549-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Würgler-Hauri CC, Kalbarczyk A, Wiesli M, Landolt H, Fandino J. Dynamic neutralization of the lumbar spine after microsurgical decompression in acquired lumbar spinal stenosis and segmental instability. Spine. 2008;33:E66–E72. doi: 10.1097/BRS.0b013e31816245c0. [DOI] [PubMed] [Google Scholar]
- 22.Zappe B, Graf S, Ochsner PE, Zimmerli W, Sendi P. Propionibacterium spp. in prosthetic joint infections: a diagnostic challenge. Arch Orthop Trauma Surg. 2008;128:1039–1046. doi: 10.1007/s00402-007-0454-0. [DOI] [PubMed] [Google Scholar]


