Abstract
Background
Increases in multimorbidity and obesity have been noted in HIV infected populations in the current treatment era. Patterns of multimorbid disease clustering as well as the impact of obesity on multimorbidity are understudied in this population.
Methods
We examined obesity and multimorbidity patterns among 1844 HIV-infected patients in the UAB 1917 Clinic. Exploratory factor analysis (EFA) was used to identify the underlying factor structure responsible for clustering. Patterns among the resulting morbidity factors by body mass index (BMI) category were explored. Multivariable logistic regression models were fit to identify predictors of multimorbidity cluster patterns.
Results
The prevalence of multimorbidity was 65% (1205/1844). Prevalence increased with progressive BMI categories from underweight (64%) to obese (79%). Three multimorbidity clusters were identified: “Metabolic” including hypertension (HTN), gout, diabetes mellitus, and chronic kidney disease (CKD) (range: 0.41 to 0.84; P<0.001); “Behavioral“ including mood disorders, dyslipidemia, chronic obstructive pulmonary disease (COPD), chronic ulcer disease, osteoarthritis, obstructive sleep apnea (OSA), and cardiac disorders (range: 0.32 to 0.57; P<0.001); “Substance Use” including alcohol abuse, substance abuse, tobacco abuse, and hepatitis C (range: 0.53 to 0.89; P<0.001). Obesity was associated with increased odds of multimorbidity (Obese vs. Normal BMI category: OR=1.52, 95%CI=1.15-2.00).
Conclusions
Three patterns of disease clustering were identified. Obesity was associated with a higher likelihood of multimorbidity. The management of multimorbidity and obesity will need to be addressed in future clinical practice guidelines to enhance long term outcomes of HIV-infected patients in the current treatment era.
Keywords: Multimorbidity, Obesity, HIV, Factor Analysis, Tetrachoric
Introduction
Effective antiretroviral therapy (ART) has significantly prolonged the life expectancy of people living with HIV/AIDS [1]. Estimates indicate that by 2015, over 50% of HIV-infected patients will be over the age of 50 years [2]. Multimorbidity, defined as the co-occurrence of two or more chronic conditions, is increasingly common in the aging population. In non-HIV-infected populations, the presence of multimorbidity has significant clinical implications due to its association with decreased functional status and quality of life, and increased adverse drug events, medical costs, disability, and mortality [3-7]. Few studies have addressed the issue of multimorbidity in HIV-infected patients.
Another emerging and understudied issue in contemporary HIV care is obesity [8]. In our practice setting, we found that 45% of patients were either overweight (body mass index (BMI) 25-29.9 kg/m2) or obese (BMI >30 kg/m2) prior to initiation of ART, consistent with results obtained from similar studies done in other demographic regions of the US [9]. Overweight or obese status confers increased risks for chronic conditions such as hypertension (HTN), cardiovascular disease, and diabetes, potentially adding significantly to the disease burden of an HIV-infected person [8, 10, 11].
In order to explore the impact of obesity on multimorbidity and to determine its effect on disease clustering among HIV-infected patients we sought to: (1) Use exploratory factor methods to identify patterns of multimorbidity in HIV-infected patients [5]; (2) Characterize the resulting factor patterns by BMI category; (3) Determine the association between obesity and the likelihood of having conditions in more than one factor group (which for the purposes of this study was defined as “multimorbidity”) while controlling for other sociodemographic and clinical variables. We hypothesized that multimorbidity disease clusters would be identified, and that increasing BMI would be associated with a higher risk of multimorbidity.
Methods
Data were obtained from the University of Alabama at Birmingham (UAB) 1917 HIV/AIDS Clinic Cohort Observational Database Project, an ongoing Institutional Review Board (IRB)-approved clinical cohort study. The UAB 1917 Clinic Cohort database includes detailed sociodemographic, psychosocial, and clinical information from over 6,000 HIV-infected patients dating back to 1988. Currently, over 1,900 patients receive primary and subspecialty HIV care at the clinic. The UAB 1917 Clinic uses a locally developed electronic health record (EHR) that imports all laboratory values from the central UAB laboratory, requires electronic prescription for all medications, and contains detailed provider encounter notes. The EHR and database are quality controlled, with all provider notes reviewed to ensure appropriate data capture regarding changes (additions or deletions) in diagnoses, allergies, and medications, including start and stop dates for antiretroviral and all other prescribed medications. New and ongoing diagnoses are maintained in patients’ active problem lists, whereas resolved diagnoses discontinued by providers are removed from active problem lists and remain part of patients’ electronic records. The UAB IRB approved this cross-sectional, retrospective study nested in the UAB 1917 Clinic Cohort.
Participants
We retrieved data from 1844 HIV-infected patients who attended a primary HIV care visit at the 1917 Clinic between July 1, 2010 and June 30, 2011. Inclusion criteria were (1) age 19 years or older, (2) currently receiving ART, with (3) plasma HIV viral load, CD4 count, height, and weight measured between June 31, 2010 and July 1, 2011. All data were acquired through queries (MS SQL®) of the electronic database.
Generation of diagnosis list
An initial list of 28 common non-AIDS related chronic conditions was compiled after review of contemporary multimorbidity literature in both the general and HIV-infected populations [1, 5, 12]. Three providers (MM, JR, JW) reviewed this initial list for relevance and clinical significance to HIV-infected patients. When possible, diagnoses were collapsed into related groups (e.g. mania, bipolar disorder and depression were collapsed under the term “mood disorders”). In addition, we combined individual diagnoses with a prevalence of < 2% into groups (e.g., chronic ischemic heart disease, cardiac insufficiency, and myocardial infarction were grouped as “cardiac disorders”). A patient was considered to have a condition if the diagnosis was ever entered in the EHR. Since empty cells adversely affect the factor modeling of correlations among categorical variables, conditions otherwise not collapsed into larger diagnosis groups were excluded from analyses if present in < 2% of our study sample. Table 1 displays the final list of conditions (n=15) included in the factor analysis model.
Table 1.
Prevalence of conditions in descending order for 1844 HIV infected patients receiving care at the UAB 1917 Clinic as of July 1, 2011.
| Condition | Prevalence (%) |
|---|---|
| Mood Disorders1 | 48 |
| Tobacco abuse/dependence | 43 |
| Hypertension | 40 |
| Dyslipidemia | 36 |
| Osteoarthritis | 26 |
| Substance abuse/dependence2 | 26 |
| Alcohol abuse/dependence | 15 |
| Hepatitis C | 12 |
| Chronic Obstructive Pulmonary Disease (COPD) | 12 |
| Ulcer disease 3 | 11 |
| Diabetes mellitus | 9 |
| Chronic kidney disease (CKD) | 7 |
| Cardiac disorders4 | 7 |
| Obstructive sleep apnea (OSA) | 4 |
Hypomania, mania, depression, cyclothymia, mood disorder, bipolar disorder, dysthymia
Cocaine, heroin, methamphetamine, LSD, opioid abuse, marijuana
Gastroesophageal reflux disease, chronic duodenal ulcer, gastric ulcer, peptic ulcer disease
Chronic ischemic heart disease, cardiac insufficiency, myocardial infarction
Independent variables
Patient-level sociodemographic and laboratory information included: age, gender, race (white, non-white), HIV transmission risk factor (heterosexual, men who have sex with men (MSM), or intravenous drug use (IVDU)), health insurance status (public, private, or uninsured), most recent plasma HIV viral load (VL), CD4 count, and BMI (weight in kg/height in m2). Patients were grouped into four different BMI categories according to the National Institute of Health criteria: underweight (BMI < 18.5), normal weight (BMI = 18.5 to 24.9), overweight (BMI = 25 to 29.9), and obese (BMI ≥ 30) [13]. Race and gender were subsequently modeled as a four level interaction term (white males/females; non-white males/females).
Dependent variables
The primary outcome was multimorbidity, defined in our study as the presence of at least one condition in two or more disease clusters in addition to HIV infection.
Statistical analysis
Descriptive statistics were used to calculate the distributions of all study variables and to ensure that assumptions of statistical tests were met. The term factor analysis encompasses a family of statistical methods used to investigate patterns of correlations. In this study, we used Exploratory Structural Equation Modeling (ESEM), a recently developed variation of Exploratory Factor Analysis (EFA) to identify patterns of disease clustering among our patients. Eigenvalues were calculated to decide how many factors to extract in the overall factor analysis (first five results were: 3.22, 2.60, 1.38, 1.04, and 0.98). ESEM combines the advantages of both exploratory and confirmatory factor analysis. We used the Horn parallel test, Velicer MAP criterion and Very simple structure (VSS) complexity to determine that a three-factor model fit the data best (see supplementary electronic table). Tetrachoric correlations were measured using Weighted Least Square with Mean and Variance adjustment estimation and oblique rotation [14]. Adequacy of model fit was determined by the chi-square test and several other descriptive models discussed in previous literature [15]. These analyses were completed with MPlus computer software (version 6) [16] and the module ‘psych’ of the statistical package R.
A multivariable logistic regression model was fit to evaluate the association between obesity and the presence of multimorbidity while controlling for covariates. Statistical significance for all tests was defined as a 2-tailed P value < 0.05. Descriptive and logistic regression statistical analyses were performed using SAS software, version 9.2.
Results
Among 1833 patients meeting inclusion criteria the mean age (±SD) was 44 ± 10.9 years, 46% were white (n=837), 77% male (n=1408), and MSM constituted the largest HIV transmission risk group (59%, n=992). Most patients had a CD4 count > 350 cells/mm3 (71%, n=1,313), and 65% of patients had an elevated BMI (36% overweight, 29% obese). Multimorbidity, defined in our study as the presence of conditions in more than one cluster, was prevalent in 65% of the study sample (Table 2), and increased with each progressive BMI category: underweight (n=41 of 73, 56%), normal weight (n=351 of 566, 62%), overweight (n=443 of 661, 67%), obese (n=370 of 536, 69%).
Table 2.
Demographic characteristics for 1844 HIV infected patients receiving care at the UAB 1917 Clinic as of July 1, 2011.
| Characteristics | N (%) |
|---|---|
| Age (years), mean (sd) | 44.3 (10.9) |
| Multimorbidity | 1205 (65.3) |
| Race/Gender5 | |
| White male | 725 (39.6) |
| White female | 112 (6.1) |
| Non-white male | 683 (37.3) |
| Non-white female | 313 (17.1) |
| BMI category | |
| Underweight | 73 (4.0) |
| Normal weight | 567 (30.8) |
| Overweight | 665 (36.1) |
| Obese | 539 (29.2) |
| Insurance type | |
| Private | 579 (31.4) |
| Public | 684 (37.1) |
| Uninsured | 581 (31.5) |
| CD4 count cells/mm3 | |
| < 200 | 221 (12.0) |
| 200-350 | 310 (16.8) |
| >350 | 1313 (71.2) |
| Viral Load: HIV RNA copies/mL | |
| < 50 | 1231 (66.8) |
| ≥ 50 | 613 (33.2) |
| HIV risk factor6 | |
| IVDU | 149 (8.8) |
| MSM | 927 (54.5) |
| Heterosexual | 625 (36.7) |
Data for 11 patients were missing; Racial distribution among non whites (n=996, 54.3%) is as follows: American Indian or Alaska Native (n=2, 0.11%), Asian (n=4, 0.22%), Black or African American (n=963, 52.55%), Hispanic (n=21, 1.14%), Multiracial (n=3, 0.16%), Other (n=3, 0.16%)
Risk factor is missing for 143 patients
The overall prevalence of specific conditions ranged from a low of 2% (gout) to a high of 48% (mood disorders, see Table 1). Results indicated that a three-factor model provided the most interpretable solution for our data set (chi-square test of goodness-of-fit, P<0.001; RMSEA, 0.020; TLI, 0.957; CFL, 0.974). Each of the three factors is comprised of a number of diagnoses that were grouped together by a data-driven computer model based on frequency of co-occurrence. To simplify nomenclature, we labeled each cluster of diagnoses based on the diagnosis that had the highest prevalence within each factor. In our case, the three most common conditions in our population were mood disorders (48%), tobacco dependence/abuse (43%), and hypertension (40%). Factor one, labeled “Metabolic”, loaded HTN, gout, diabetes mellitus, and chronic kidney disease (CKD) (range of standardized loadings: 0.41 to 0.84; P<0.001); Factor two, labeled “Behavioral”, loaded mood disorders, dyslipidemia, chronic obstructive pulmonary disease (COPD), peptic ulcer disease, osteoarthritis, obstructive sleep apnea (OSA), and cardiac disorders (range of standardized loadings: 0.32 to 0.57; P<0.001); Factor 3, labeled “Substance use”, loaded alcohol abuse, substance abuse, tobacco abuse, and hepatitis C (range of standardized loadings: 0.53 to 0.89; P<0.001).
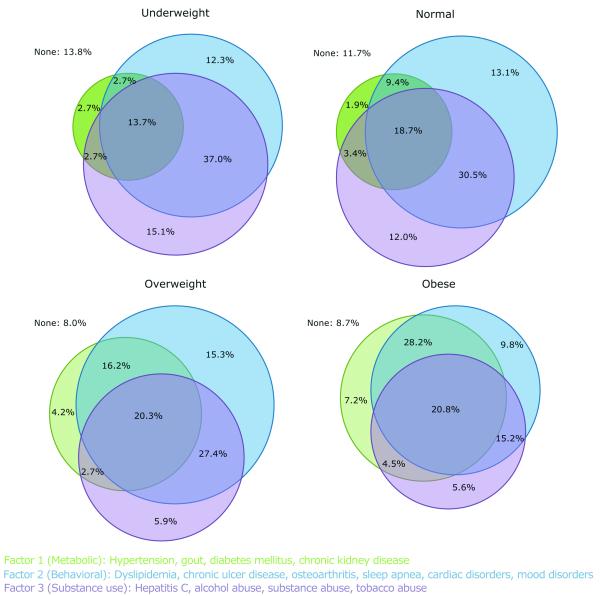
Multimorbidity patterns showing overlapping distributions of factors stratified by BMI category are shown in Figure 1. The proportion of patients with a Factor 1 (Metabolic) condition increased with BMI: Underweight (22%), normal weight (33%), overweight (44%), obese (61%). The presence of Factor 2 (Behavioral) conditions were roughly proportional across all BMI categories: Underweight (66%), normal weight (72%), overweight (79%), obese (74%). The frequency of Factor 3 (Substance use) conditions decreased as BMI category increased: Underweight (69%), normal weight (65%), overweight (56%), obese (46%). Overall, overlap among factors increased with BMI category, with the most notable overlap occurring between Factors 1 (Metabolic) and 2 (Behavioral): Underweight (3%), normal weight (9%), overweight (16%), obese (28%).
Figure 1.
In the multivariable logistic regression model, obesity (obese vs. normal weight OR=1.52, 95%CI=1.15-2.00), white males (white male vs. non-white male OR= 1.60, 95%CI=1.25-2.05), insurance status (public vs. private insurance OR=2.06, 95% CI =1.57-2.69; uninsured vs. private insurance OR=1.34, 95% CI =1.03-1.74), CD4 >350 (CD4>350 vs. <200 OR=1.62, 95%CI=1.18-2.24) and increased age (per 10 year increase, OR=1.81, 95% CI 1.62-2.02) were associated with increased odds of multimorbidity (Table 3).
Table 3.
Multivariable Logistic Regression Model Relationship between multimorbidity and sociodemographic and laboratory values in 1844 HIV-infected patients receiving care at the UAB 1917 Clinic as of July 1, 2011
| Univariate OR (95% CI) |
Multi-variable OR (95% CI) |
|
|---|---|---|
| Age (per 10 years) | 1.93 (1.75-2.13) | 1.81 (1.62-2.02) |
| BMI category | ||
| Normal weight | 1.00 | 1.00 |
| Obese | 1.35 (1.05-1.73) | 1.51 (1.15-1.99) |
| Overweight | 1.23 (0.97-1.55) | 1.14 (0.88-1.46) |
| Underweight | 0.79 (0.48-1.29) | 0.86 (0.50-1.50) |
| Race/Gender | ||
| Non-white male | 1.00 | 1.00 |
| White male | 1.93 (1.54-2.41) | 1.59 (1.24-2.04) |
| Non-white female | 1.26 (0.95-1.65) | 0.82 (0.61-1.12) |
| White female | 1.82 (1.18-2.82) | 1.36 (0.85-2.17) |
| Insurance type | ||
| Private insurance | 1.00 | 1.00 |
| Public insurance | 1.80 (1.41-2.29) | 2.06 (1.58-2.70) |
| Uninsured | 0.77 (0.61-0.98) | 1.34 (1.03-1.74) |
| CD4 value, cells/mm3 | ||
| <200 | 1.00 | 1.00 |
| 200-350 | 1.24 (0.87-1.76) | 1.05 (0.72-1.53) |
| >350 | 1.65 (1.24-2.21) | 1.56 (1.12-2.18) |
| Viral Load: HIV RNA copies/mL | ||
| < 50 | 1.00 | 1.00 |
| ≥ 50 | 0.63 (0.52-0.77) | 0.89 (0.71 - 1.12) |
Discussion
Our study represents one of the first efforts to characterize multimorbidity patterns in an HIV-infected population. Factor analysis and hierarchical item cluster analysis were used to take a data driven approach to how common chronic conditions clustered together based on frequency of co-occurrence alone, irrespective mechanisms or shared similarities in pathophysiology. These factor groups or disease clusters were then stratified per BMI category in an effort to see how weight gain and obesity affected patterns of multimorbidity. In our study population, the majority of patients (65%) met our criteria for multimorbidity overall, which required patients to have conditions in more than one of the three clusters we described. In addition, our model of multimorbidity did not include 11% of the study sample that had multiple conditions within a single factor. Taken together, these data suggest our estimate of the association between multimorbidity and obesity in the present study is likely conservative.
In concordance with our hypothesis and consistent with existing literature [6], obesity was associated with a significantly higher likelihood of multimorbidity (OR 1.51, 95% CI 1.15-1.99). In addition to increasing the odds of having conditions in multiple disease clusters, it is interesting to observe the impact of higher BMI categories on the patterns of disease clustering in our patients. For instance, the prevalence of overlap among conditions in both Factor 1 (Metabolic) and Factor 2 (Behavioral) was higher in obese patients compared to underweight patients (28.2% vs. 2.7%). In addition, underweight patients were three times as likely to have at least one Factor 3 (Substance use) related condition. Overall, the degree of overlap among all disease clusters was greater as BMI increased.
Conditions such as obesity and dyslipidemia in particular, once considered to be a side effect of ART, are now observed as baseline conditions for treatment-naïve HIV-infected patients [17] [18] and play a key role in multimorbidity. In our practice setting, we found that 45% of patients were either overweight or obese prior to initiation of ART [19]. The prevalence of obesity among our patients (29.2%) is similar to the general population averages for Alabama (32%) and the United States (30%) [20]. Thus, the issue of weight management must be stressed in longitudinal care in order to diminish its impact on multimorbidity among HIV-infected patients.
Older HIV-infected patients have higher odds of multimorbidity than older non-HIV infected patients with similar baseline characteristics [12]. Consistent with existing medical literature [21], we determined older age to be significantly associated with multimorbidity (OR = 1.81, 95% CI = 1.62-2.02 per 10 years) among our HIV-infected patients. Increased longevity among well-managed HIV-infected patients will likely contribute to higher rates of multimorbidity in the future and will play a key role in the evolving care needs of our patient population. Higher CD4 values increase the risk for multimorbidity. This finding is in concordance with previously published results and underscores the growing importance of non-HIV related morbidities among those successfully treated for HIV [22].
The impact of aging, obesity and increasing prevalence of multimorbidity in the HIV-infected population will have far reaching implications. First, clinical practice guidelines are often based on results from clinical trials with strict entry criteria, that frequently exclude patients with significant co-morbid disease and even more so those with multimorbidity. With such variability between patient populations in clinical trials and clinical practice, the applicability of data derived from prior and similarly exclusive future trial populations must be carefully considered. Looking beyond isolated co-morbidity and accounting for multimorbidity in trial design will be an integral part of optimized HIV management in the future. [23] In addition, though guidelines often exist to address management of co-morbid conditions in isolation (i.e., hepatitis C infection or dyslipidemia), guidelines rarely address multimorbidity and its associated impact on drug-drug interactions, functional status, quality of life and mortality for those managing the care of complex HIV-infected patients burdened with multiple chronic diseases [24]. As the healthcare needs of the HIV-infected population continue to evolve, our field will need to formally address this challenge.
Limitations
This study has several limitations. This paper used EFA, a data driven approach, and different results may have been found using a different specification of the model, such as a rotational strategy. Replication would be important to assure generalizability of these findings in other study samples. There is no established list of diagnoses used to define multimorbidity, and definitions of multimorbidity vary in the medical literature. Since it was not possible to include every potential diagnosis in the factor analysis model, we combined clinical judgment with statistical analysis to determine the conditions that best described our study population. Furthermore, we were guided by data from the general population where multimorbidity has been better defined [25]. Though the 1917 Clinic draws from a broad referral area, our study is composed of a sample from one site in the Southeastern US. Since our region has historically seen a higher incidence of obesity and chronic diseases, our findings may not be generalizable to other HIV-infected populations. However, other studies have shown that the overweight/obese epidemic among HIV infected individuals is equally prevalent in other regions of the US [9]. Finally, this study used a cross-sectional sample of adults who attended the UAB 1917 Clinic between June 2010 and July 2011 regardless of the duration of care or cumulative ART exposure. Therefore, it is difficult to characterize the role that such factors might have had on existing co-morbidities in this cross-sectional study.
Conclusion
We are in the midst of several demographic shifts among people living with HIV/AIDS, with aging and obesity becoming concomitantly more prevalent. In our analysis of HIV-infected patients we determined both aging and obesity as risk factors for multimorbidity. Our attempt to characterize multimorbidity patterns and observe commonly co-occurring conditions will provide critical first steps in further defining the scope of the problem, and inform interventions to address the management of multimorbidity in the context of HIV. Our focus as HIV care providers must extend beyond CD4 counts, viral load, and traditional AIDS-defining illnesses to embrace HIV care as complex chronic disease management of multiple overlapping conditions within the context of primary care. Attention to these changing needs across the field, from trial design to guideline development will allow us to dynamically adapt to the changing care needs of people living with HIV/AIDS.
Supplementary Material
Acknowledgments
Funding
This work was supported by the UAB Center for AIDS Research [P30-AI27767], CNICS [1R24 AI067039-1], and the Mary Fisher CARE Fund. Dr. Christine Ritchie is supported by a Geriatric Academic Leadership Award (Advanced Illness and Multimorbidity Research Program) from the National Institute on Aging [1K07AG31779 R01 AG015062], UB4HP19045 (National Cancer Institute), and R18-HS017786-02 (AHRQ). G.A.B. is supported in part by the Agency for Healthcare Research and Quality [5 T32 HS013852]. Dr. Crane is supported by AHRQ 1R21HS019516-01.
M.S.S. has received grants and/or is a consultant for: Ardea Biosciences, Inc, Avexa Ltd, Boehringer Ingelheim Pharmaceuticals, Inc, Bristol-Myers Squibb, Gilead Sciences, Inc, GlaxoSmithKline, Merck & Co, Inc,, Pfizer Inc, Tibotec Therapeutics, Vertex Pharmaceuticals, Inc, and ViiV Healthcare
M.J.M. has received recent research support (to UAB) from Bristol-Myers Squibb, Tibotec Therapeutics, Definicare, and Pfizer, and has consulted (advisory board) for Merck Foundation, Bristol-Myers Squibb and Gilead Sciences.
J.H.W. has received research support from the Bristol-Myers Squibb, Pfizer, Tibotec Therapeutics, and Definicare, and has consulted for Bristol-Myers Squibb and Gilead Sciences.
Footnotes
Potential Conflicts of Interest:
D. J. K. No conflict
A.O.W. No conflict
E.C. No conflict
A. L. W. No conflict
C.R. is on the Board of the American Academy of Hospice and Palliative Medicine
G.A.B. has received research support from the Bristol-Myers Squibb Virology Fellows Research Training Program for the 2010-2012 academic years.
H.M.C No conflict
J.L.R. No conflict
Hypomania, mania, depression, cyclothymia, mood disorder, bipolar disorder, dysthymia
Cocaine, heroin, methamphetamine, LSD, opioid abuse, marijuana
Gastroesophageal reflux disease, chronic duodenal ulcer, gastric ulcer, peptic ulcer disease
Chronic ischemic heart disease, cardiac insufficiency, myocardial infarction
Data for 11 patients were missing; Racial distribution among non whites (n=996, 54.3%) is as follows: American Indian or Alaska Native (n=2, 0.11%), Asian (n=4, 0.22%), Black or African American (n=963, 52.55%), Hispanic (n=21, 1.14%), Multiracial (n=3, 0.16%), Other (n=3, 0.16%)
Risk factor is missing for 143 patients
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Justice AC. HIV and aging: time for a new paradigm. Curr HIV/AIDS Rep. 2010;7:69–76. doi: 10.1007/s11904-010-0041-9. [DOI] [PubMed] [Google Scholar]
- 2.Effros RB, Fletcher CV, Gebo K, et al. Aging and infectious diseases: workshop on HIV infection and aging: what is known and future research directions. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2008;47:542–53. doi: 10.1086/590150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fortin M, Hudon C, Haggerty J, Akker M, Almirall J. Prevalence estimates of multimorbidity: a comparative study of two sources. BMC health services research. 2010;10:111. doi: 10.1186/1472-6963-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salter ML, Lau B, Go VF, Mehta SH, Kirk GD. HIV Infection, Immune Suppression, and Uncontrolled Viremia Are Associated With Increased Multimorbidity Among Aging Injection Drug Users. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2011;53:1256–64. doi: 10.1093/cid/cir673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schafer I, von Leitner EC, Schon G, et al. Multimorbidity patterns in the elderly: a new approach of disease clustering identifies complex interrelations between chronic conditions. PloS one. 2010;5:e15941. doi: 10.1371/journal.pone.0015941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van den Bussche H, Koller D, Kolonko T, et al. Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. BMC public health. 2011;11:101. doi: 10.1186/1471-2458-11-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Archives of internal medicine. 2002;162:2269–76. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 8.Bogers RP, Bemelmans WJ, Hoogenveen RT, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Archives of internal medicine. 2007;167:1720–8. doi: 10.1001/archinte.167.16.1720. [DOI] [PubMed] [Google Scholar]
- 9.IDSA [Accessed 12/15/11 2011];HIV-Positive People Now Overweight Like Everyone Else - As disease becomes a chronic condition, other health issues arise [Google Scholar]
- 10.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. The New England journal of medicine. 2003;348:1625–38. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan PW, Morrato EH, Ghushchyan V, Wyatt HR, Hill JO. Obesity, inactivity, and the prevalence of diabetes and diabetes-related cardiovascular comorbidities in the U.S., 2000-2002. Diabetes care. 2005;28:1599–603. doi: 10.2337/diacare.28.7.1599. [DOI] [PubMed] [Google Scholar]
- 12.Goulet JL, Fultz SL, Rimland D, et al. Aging and infectious diseases: do patterns of comorbidity vary by HIV status, age, and HIV severity? Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2007;45:1593–601. doi: 10.1086/523577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Institutes of Health NHL . Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. National Institutes of Health; Bethesda, MD: 1998. [PubMed] [Google Scholar]
- 14.Beauducel A, YP H. On the performance of maximum likelihood versus means and variance adjusted least squares estimation in CFA. Structural equation modeling: a multidisciplinary journal. 2006;13:186–203. [Google Scholar]
- 15.Revelle WRT. Very simple structure. An alternative procedure for estimating the optimal number of interpretable factors. Multivariable Behavioral Research. 1979;14:403–14. doi: 10.1207/s15327906mbr1404_2. [DOI] [PubMed] [Google Scholar]
- 16.Muthén B. A general structural equation model with dichotomous, ordered categorical, and continuous latent variable indicators. Psychometrika. 1984;49:115–32. [Google Scholar]
- 17.Feeney ER, Mallon PW. HIV and HAART-Associated Dyslipidemia. Open Cardiovasc Med J. 2011;5:49–63. doi: 10.2174/1874192401105010049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palella FJ, Jr., Baker RK, Buchacz K, et al. Increased mortality among publicly insured participants in the HIV Outpatient Study despite HAART treatment. AIDS. 2011;25:1865–76. doi: 10.1097/QAD.0b013e32834b3537. [DOI] [PubMed] [Google Scholar]
- 19.Tate T, Willig A, Willig J, et al. HIV infection and obesity: Where did all the wasting go? Antiviral therapy. 2012 doi: 10.3851/IMP2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA: the journal of the American Medical Association. 2002;288:1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 21.Vance DE, Mugavero M, Willig J, Raper JL, Saag MS. Aging with HIV: a cross-sectional study of comorbidity prevalence and clinical characteristics across decades of life. J Assoc Nurses AIDS Care. 2011;22:17–25. doi: 10.1016/j.jana.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Mocroft A, Reiss P, Gasiorowski J, et al. Serious fatal and nonfatal non-AIDS-defining illnesses in Europe. J Acquir Immune Defic Syndr. 2010;55:262–70. doi: 10.1097/QAI.0b013e3181e9be6b. [DOI] [PubMed] [Google Scholar]
- 23.O’Kelly FD, Bury G. An analysis of the effects of HIV infection in a cohort of intravenous drug users. Irish medical journal. 1996;89:112–4. [PubMed] [Google Scholar]
- 24.Goulet JL, Fultz SL, McGinnis KA, Justice AC. Relative prevalence of comorbidities and treatment contraindications in HIV-mono-infected and HIV/HCV-co-infected veterans. AIDS. 2005;19(Suppl 3):S99–105. doi: 10.1097/01.aids.0000192077.11067.e5. [DOI] [PubMed] [Google Scholar]
- 25.Marengoni A, Rizzuto D, Wang HX, Winblad B, Fratiglioni L. Patterns of chronic multimorbidity in the elderly population. J Am Geriatr Soc. 2009;57:225–30. doi: 10.1111/j.1532-5415.2008.02109.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.