Abstract
Background and Objectives
Both emotional reactivity to traumatic event cues and difficulties regulating emotion have been linked to posttraumatic stress symptom severity. The current study uniquely extended these two lines of research by examining the degree to which these two factors alone, and in combination, account for variability in posttraumatic stress symptom severity.
Method
Self-reported emotion regulation difficulties, and both subjective and physiological reactivity in response to a script-driven imagery procedure, were assessed among a community sample of 21 adult women with a history of interpersonal assault. Relationships with an interview-based measure of posttraumatic stress symptom severity were examined.
Results
Results were consistent with hypotheses. Both traumatic event-related emotional reactivity and emotion regulation difficulties independently predicted posttraumatic stress symptom severity. A significant interaction also emerged such that traumatic event-related emotional reactivity and posttraumatic stress symptom severity were only significantly associated at relatively elevated levels of emotion regulation difficulties.
Limitations
Limitations included the use of a self-report questionnaire to assess emotion regulation difficulties, relatively small sample size, and lack of evidence regarding generalizability across gender or other traumatic event types.
Conclusions
These results highlight that the interaction of heightened emotional reactivity and difficulties regulating emotion may be particularly influential in posttraumatic stress symptom severity.
Keywords: Posttraumatic Stress, PTSD, Emotion, Emotion Regulation, Imagery
1. Introduction
Reexperiencing symptoms, including unwanted and intrusive memories of a traumatic event, flashbacks, nightmares and emotional and physiological reactivity to traumatic event reminders, have been considered hallmark symptoms of posttraumatic stress disorder (PTSD; Foa, Zinbarg, & Rothbaum, 1992). Conditioning-based theories suggest powerful associative learning occurs during a traumatic event, such that fear responses become paired via classical conditioning with stimuli present during the event (e.g., Foa & Kozak, 1986; Keane, Zimering, & Caddell, 1985). As a result of this pairing, previously neutral cues associated with the traumatic event become capable of eliciting anxious reactions, even in the absence of present danger. The experience of increased emotional reactivity to traumatic event cues immediately following traumatic event exposure is an expected and normative response (Riggs, Rothbaum, & Foa, 1995; Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992) that decreases over time with repeated exposure to traumatic event cues via extinction learning (Foa & Kozak, 1986; Keane et al., 1985). However, persistent traumatic event-related emotional reactivity is a well-documented phenomenon among individuals exhibiting sustained posttraumatic stress reactions including those with PTSD.
Research demonstrates that compared to traumatic event-exposed individuals without elevated posttraumatic stress symptoms, those with higher symptom levels (Badour et al., 2011; McDonagh-Coyle et al., 2001; Pitman et al., 2001), including those with a diagnosis of PTSD (Lanius et al., 2003; Liberzon et al., 1999; Orr, Pitman, Lasko, & Herz, 1993; Pitman et al., 1990; Pitman, Orr, Forgue, de Jong, & Claiborn, 1987; Shin et al., 1999, 2004; Wolfe et al., 2000), display greater emotional reactivity in response to traumatic event cues. For example, male veterans with PTSD display significantly greater subjective distress and skin conductance responses when presented with combat sounds as compared to those without PTSD (Liberzon et al., 1999). Similarly, Wolfe and colleagues (2000) found female veterans with a current diagnosis of PTSD respond to combat-related images and sounds with increased subjective distress, skin conductance response, and systolic blood pressure compared to those with no history of PTSD. Moreover, skin conductance response positively correlates with severity of each of the three symptom clusters of PTSD (i.e., re-experiencing, avoidance-numbing, hyperarousal).
Several studies in this area have moved beyond the use of generalized traumatic event stimuli to utilize more ecologically valid methods of eliciting emotional responding to traumatic event cues. The script-driven imagery procedure, which involves the development and presentation of individualized narratives of traumatic event experiences, allows for a more refined assessment of traumatic event-related emotional reactivity while maintaining the internal validity associated with a controlled laboratory study. Studies employing this procedure have established links between posttraumatic stress symptom levels and both self-reported increases in negative affect (e.g., fear/anxiety; Badour et al., 2011; Pitman et al., 1987, 1990; Shin et al., 2004) and heightened physiological reactivity (e.g., skin conductance, heart rate, facial electromyography [EMG]; see Orr and Roth [2000] for a review). For example, in response to individualized combat scripts, Vietnam veterans with PTSD evidence increased skin conductance and facial EMG activity, as well as higher ratings of fear (and other negative emotions) as compared to veterans without PTSD (Pitman et al., 1987; Shin et al., 2004) and those with other anxiety disorders (Pitman et al., 1990). Similarly, posttraumatic stress symptom severity significantly correlates with increased heart-rate and self-reported negative affect in response to individualized sexual abuse scripts (McDonagh-Coyle et al., 2001) and self-reported anxious reactivity in response to a range of individualized traumatic event scripts (e.g., interpersonal victimization, motor vehicle accidents, natural disasters), even after accounting for general negative affect (Badour et al., 2011).
A second process likely to be critical in understanding posttraumatic stress reactions is ineffective regulation of emotion (Etkin & Wager, 2007; Liberzon & Garfinkel, 2009; Tull, Barrett, McMillan, & Roemer, 2007). People with PTSD devote significant resources to the regulation of negative emotions (Kashdan, Breen, & Julian, 2010) and frequently exhibit difficulties with this process (Chemtob, Novaco, Hamada, Gross, & Smith, 1997; Cloitre, Miranda, Stovall-McClough, & Han, 2005; Ehring, & Quack, 2010; Klemanski, Mennin, Borelli, Morrissey, & Aikins, 2012; Price, Monson, Callahan, & Rodriguez, 2006; Tull et al., 2007). Emotion regulation is broadly defined as the ability to identify, evaluate, and modify the experience and expression of affect (Gratz & Roemer, 2004; Gross, 1998). Skills for identifying, accepting, processing, and down-regulating arousal and distress are thought to be essential to the effective management of heightened emotional reactivity resulting from exposure to reminders of traumatic events (Tull et al., 2007).
At least two lines of evidence suggest emotion regulation ability may be involved in the maintenance of posttraumatic stress reactions. First, it has been suggested that non-acceptance of negative emotions, a subtype of emotion regulation linked to severity of PTSD symptoms (Ehring & Quack, 2010; Tull et al., 2007), may actually increase traumatic event-related distress by leading to the development of secondary emotions such as guilt or shame associated with one’s initial response to the event (Tull et al., 2007). It has further been suggested that non-acceptance of emotion may result in the expenditure of additional resources for the regulation of negative emotions at the cost of reducing engagement in goal-directed adaptive behaviors which may improve general well-being (Kashdan et al., 2010). Second, emotion regulation difficulties have been linked to a relative reliance on avoidant regulation strategies. For example, emotion regulation difficulties predict behavioral avoidance and functional impairment among victims of childhood abuse (Cloitre et al., 2005; Gratz, Bornovalova, Delany-Brumsey, Nick, & Lejuez, 2007), and improvement in emotion regulation ability predicts greater symptom reduction during exposure-based PTSD treatment, which specifically targets engagement with traumatic event cues in an effort to extinguish associated emotional reactivity (Cloitre, Koenen, Cohen, & Han, 2002; Price et al., 2006). Specific difficulty in identifying, describing, and distinguishing between emotion states following exposure to a traumatic event (i.e., secondary alexithymia; Hendryx, Haviland, & Shaw, 1991; Taylor, Bagby, & Parker, 1991) has been linked to PTSD (Badura, 2003; Hyer, Woods, Summers, Boudewyns, & Harrison, 1990; Monson, Price, Rodriguez, Ripley, & Warner, 2004), and has been conceptualized as a form of avoidance employed to help an individual cope with the experience of aversive emotional states. This is critical given that avoidance and escape in the face of traumatic event reminders serves to maintain posttraumatic stress reactions by interfering with extinction learning needed to reduce traumatic event-related emotional reactivity (Foa & Kozak, 1986; Foa & Rothbaum, 1998; Keane & Barlow, 2002; Keane et al., 1985; Pineles et al., 2011). Collectively, this work suggests emotion regulation difficulties may serve as a maintaining factor for posttraumatic stress reactions.
While these distinctive literatures converge to suggest that both persistent heightened emotional reactivity to traumatic event cues and difficulties regulating emotion should be linked to elevated posttraumatic stress symptomatology, empirical research has yet to examine the potential combined effects of these factors. When presented with distress associated with exposure to traumatic event cues, we might expect individuals equipped with the ability to effectively manage emotional experiences to be better able to appropriately identify and respond to the heightened traumatic event-related emotional reactivity that emerges as a consequence of fear conditioning during a traumatic event (Foa & Kozak, 1986; Keane et al., 1985). Conversely, we would expect those with difficulties regulating emotional experiences to engage in less adaptive strategies for coping with emotional reactivity elicited by traumatic event cues (e.g., cognitive/behavioral avoidance; Cloitre et al., 2005; Gratz et al., 2007) thus interfering with natural extinction processes and serving to maintain elevated posttraumatic stress reactions. The current study sought to provide a preliminary test of this model. Specifically, we examined the impact of emotion regulation difficulties on the association between subjective (i.e., self-reported anxiety) and physiological (i.e., skin conductance) reactivity to individualized traumatic event cues and posttraumatic stress symptom severity in the controlled environment of the laboratory using the well-established script-driven imagery procedure. This method was chosen based on a wealth of research linking posttraumatic stress symptomatology to both subjective and physiological arousal in response to the script-driven imagery procedure (Badour et al., 2011; Lanius et al., 2003; Liberzon et al., 1999; McDonagh-Coyle et al., 2001; Orr et al., 1993; Pitman et al., 1987, 1990, 2001; Shin et al., 1999, 2004; Wolfe et al., 2000). It was hypothesized that, consistent with prior research, positive associations would emerge between posttraumatic stress symptom severity and both emotion regulation difficulties and traumatic event-related emotional reactivity. It was further hypothesized that a stronger relation between reactivity to traumatic event cues and posttraumatic stress symptom severity would emerge among individuals exhibiting relatively high levels of emotion regulation difficulties.
2. Method
2.1. Participants
Twenty-one adult women (Mage = 33.24, SD = 16.19) with a history of at least one sexual or physical assault meeting criteria for a traumatic event, defined as satisfying Criterion A of the PTSD diagnosis (i.e., A1: an event involving life threat, threatened or actual serious injury, or threat to one’s physical integrity, A2: that is accompanied by intense feelings of either fear, helplessness, or horror; American Psychiatric Association [APA], 2000), were recruited from the community as part of a study examining affective reactivity associated with traumatic interpersonal violence. Participants were excluded from the study based on 1) inability to provide written, informed consent, 2) current suicidality, 3) experience of a traumatic event during the past month, 4) endorsement of an index traumatic event other than a sexual or physical assault, or 5) endorsement of a history of separate instances of both sexual and physical assault (due to methodological considerations not related to the current investigation).
Of the total sample, 4.8% (n = 1) of participants identified themselves as ethnically Hispanic, 85.7% (n = 18) as Caucasian, 9.5% (n = 2) as American Indian/Alaska Native, and 4.8% (n = 1) as multi-racial. There were no African American participants in the current sample. Mean annual income was $31,777 (SD = $27.346). Of the total sample, 57.1% (n = 12) had a history of sexual assault and 42.9% had a history of physical assault (n = 9). Time since the assault ranged from less than 1 year to 58 years (M = 15.38, SD = 18.65). In addition, 28.6% of the sample (n = 6) met criteria for a current diagnosis of PTSD based on the Clinician-Administered PTSD Scale (Blake et al., 1995).
2.2. Measures
2.2.1. Posttraumatic stress symptoms
The Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) is a well-established semi-structured interview with excellent psychometric properties that is considered a gold standard of PTSD assessment (Weathers, Keane, & Davidson, 2001). The CAPS provides a diagnosis of PTSD as well as a continuous index of posttraumatic stress symptom severity based on frequency and intensity of 17 symptoms experienced in the past month. The continuous index of posttraumatic stress symptom severity was used in the current study based upon research suggesting posttraumatic psychopathology is best represented by a dimensional (as opposed to taxonic) symptom structure, with PTSD at the upper end of this continuum (Broman-Fulks et al., 2009; Ruscio, Ruscio, & Keane, 2002). Diagnostic status was obtained for descriptive purposes, using established scoring rules (1, 2 scoring rule; Weathers, Ruscio, & Keane, 1999). A graduate-level researcher trained in administration of the CAPS administered all CAPS interviews. Reliability checks of 25% of CAPS interviews conducted by a second graduate student trained in administration of the interview yielded 100% diagnostic agreement.
2.2.2. Emotion regulation difficulties
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item questionnaire designed to measure difficulties in 6 domains of emotion regulation. These domains include awareness/understanding, clarity, and acceptance of emotions; ability to continue engaging in goal-directed behaviors while in a negative mood; refraining from engaging in impulsive behaviors while in a negative mood; and access to effective strategies for regulating emotion. Respondents endorse the frequency with which items apply to them on a 5-point Likert-type scale (1 = almost never to 5 = always). Higher scores suggest greater difficulties regulating emotions. The DERS has evidenced strong internal consistency (α = .93 for the overall scale, and α > .80 for each of the subscales; Gratz & Roemer, 2004) as well as convergent validity with other emotion regulation measures (e.g., the Negative Mood Regulation Scale; Catanzaro & Mearns, 1990). The global score on the DERS was employed to measure emotion regulation difficulties (as opposed to specific subscales) due to the relatively underdeveloped nature of this literature that precluded more specific predictions (α = .87 in the current sample). The global score has been shown to uniquely predict posttraumatic stress symptom severity even after accounting for negative affect (Tull et al., 2007).
2.2.3. Subjective reactivity to the script procedure
Subjective anxious reactivity to the script-driven imagery procedure was measured using a Visual Analog Scale (VAS; Freyd, 1923). This method is well established for measuring subjective anxiety in response to script-driven imagery procedures (e.g., Orr et al., 1990; Pitman et al., 1987). Participants were asked to rate current anxiety levels by placing a single straight line on a 100 mm VAS ranging from 0 (no anxiety) to 100 (extreme anxiety) following the presentation of the neutral and traumatic event scripts. Change in anxiety to the traumatic event script (i.e., anxious reactivity) was calculated by creating a change score (subtracting VAS ratings following the neutral script from VAS ratings following the traumatic event script). This approach provides a relatively conservative estimate of anxious reactivity by taking into account general emotional reactivity (i.e., anxiety following an individualized neutral script; Olatunji, Babson, Smith, Feldner, & Connolly, 2009).
2.2.4. Physiological reactivity to the script procedure
Physiological reactivity to the script-driven imagery procedure was measured using a J&J Engineering I-330-C2 system to digitally record skin conductance data on-line at a sample rate of 1024 samples per second using J&J Engineering Physiolab Software. Consistent with previous research (Brunet et al., 2008; Carson et al., 2000; Pitman et al., 1990), continuous monitoring of skin conductance converted to microsiemens (μS) was obtained using disposable electrodes placed on the medial phalange of the index and ring finger of the participants’ non-dominant hand. Electrode preparation included the use of an alcohol swab to reduce inter-electrode impedance. A measure of skin conductance was created by calculating the mean of the data collected during the 30-sec imaginal rehearsal period following the presentation of each script (described in greater detail below). Physiological reactivity to the traumatic event script was defined as change in skin conductance to the traumatic event script relative to the neutral event script (calculated via a change score as described above).
2.3. Procedure
All laboratory procedures were conducted in a 12′ × 14′ experimental room that contained a chair, desk, computer, and audio recorder. The experimenter was located in an adjacent room throughout the entire procedure. An intercom system and closed-circuit surveillance system were in place to allow for monitoring and communication between the experimenter and participant. During the laboratory session, participants were informed of any potential risks associated with the study (e.g., temporary psychological distress associated with the script-driven imagery procedure) and written informed consent was obtained. Participants completed the CAPS, followed by a demographics questionnaire, the DERS, and additional questionnaires not related to the current study. During the CAPS, participants identified the most distressing traumatic event (i.e., index event) that would be used for developing the individualized traumatic event script. Next, participants generated a detailed written description of both an individualized neutral and traumatic event (e.g., description of the location, sensory experiences, thoughts, feelings). Consistent with previously employed script-driven imagery procedures (Orr et al., 1990; Pitman et al., 1987), participants also completed a checklist of physiological sensations experienced during each event. The experimenter then generated 30-sec scripts based on the written description and physiological sensations checklist, which were audiotaped and presented to participants during the script-driven imagery procedure.
2.3.1. Script-driven imagery procedure
Participants were fitted with the physiological recording equipment, during which time the experimenter explained electrode placement procedures to minimize participant discomfort. Following a 10-min baseline during which participants sat quietly, the script-driven imagery procedure was administered (e.g., Pitman et al., 1987). This consisted of presenting the neutral script followed by the traumatic event script. During presentation of each script, participants were instructed to imagine the scenario described as vividly as possible. Each script included the following 30-sec periods: baseline, script presentation, imaginal rehearsal, and recovery. Following each recovery period, participants provided VAS anxiety ratings. After this procedure participants were fully debriefed, thanked for their time, and compensated $30.
2.4. Data Analytic Approach
First, descriptive statistics for, and zero-order correlations among, all primary variables were examined. Relations between age and time since traumatic event exposure and all primary variables were also examined to determine if these variables, which have been linked to posttraumatic stress symptom severity (Amir, Kaplan, & Kotler, 1996; Maercker, Michael, Fehm, Becker, & Margraf, 2004) should be included as covariates in the primary analyses. Second, hypotheses were tested via two separate hierarchical linear regression analyses. Subjective and physiological reactivity were examined in independent analyses, as opposed to multivariate methods, due to documented discordance between self-report and physiological indicators of emotion in response to script-driven imagery procedures among participants with PTSD (Orr et al., 1993) and anxiety disorders more broadly (Craske, 1999; Cuthbert et al., 2003; Hodgson & Rachman, 1974). Predictors were mean-centered prior to entry in the regression models (Cohen & Cohen, 1983). Indices of emotional reactivity to the traumatic event script (VAS anxiety ratings or skin conductance) and emotion regulation difficulties were entered into step 1 of each model. The interaction between emotional reactivity and emotion regulation were entered into step 2 of each model. Significant interactions were probed as recommended (Aiken & West, 1991; Holmbeck, 2002). Squared semi-partial correlations (sr2) were used to index effect size of individual predictors (Kirk, 1996; Tabachnick & Fidell, 2007).
3. Results
Table 1 includes means, standard deviations, and zero-order correlations. As hypothesized, emotion regulation difficulties and both subjective and physiological reactivity to the traumatic event script were significantly positively correlated with posttraumatic stress symptom severity. Emotion regulation difficulties were not significantly associated with either traumatic event-related subjective or physiological reactivity, suggesting that these measures assessed distinct factors. Other factors, including age and time since traumatic event exposure, were not significantly correlated with posttraumatic stress symptom severity. Accordingly, these factors were not included in the regression models testing the primary hypotheses.
Table 1.
Zero-Order Relations among Continuous Factors
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. Age | 33.24 | 16.19 | -- | .87** | −.20 | −.37 | .09 | .09 |
| 2. Time Since Traumatic Event Exposure | 15.38 | 18.65 | -- | -- | −.38 | −.49* | −.11 | .08 |
| 3. Posttraumatic Stress Symptom Severity | 30.76 | 22.66 | -- | -- | -- | .63** | .59** | .44* |
| 4. Difficulties with Emotion Regulation | 80.10 | 20.39 | -- | -- | -- | -- | .09 | .18 |
| 5. Anxious Reactivity | 32.43 | 27.90 | -- | -- | -- | -- | -- | .21 |
| 6. Skin Conductance Reactivity | 0.78 | 1.62 | -- | -- | -- | -- | -- | -- |
Note:
p < .05;
p < .01.
Table 2 provides an overview of regression analyses. First, results of the model examining subjective reactivity revealed a significant omnibus regression model [F(3, 17) = 17.71, p < .001]. As expected, in step 1 both emotion regulation difficulties and self-reported anxious reactivity to the traumatic event script significantly accounted for unique variability in posttraumatic stress symptom severity. In step 2, the interaction between emotion regulation difficulties and self-reported anxious reactivity accounted for an additional 8.3% of the total variance in symptom severity. Collectively, the model accounted for 71.5% of the variability in posttraumatic stress symptom severity.
Table 2.
Emotion Regulation Difficulties and Traumatic Event-Related Emotional Reactivity in Predicting Posttraumatic Stress Symptom Severity
| R2 | t | β | sr2 | |
|---|---|---|---|---|
| Model 1: Emotion Regulation Difficulties and Anxious Reactivity | ||||
| Step 1 | 0.64*** | |||
| Emotion Regulation Difficulties | 4.30 | 0.58 | 0.33*** | |
| Anxious Reactivity | 3.95 | 0.53 | 0.28** | |
| Step 2 | 0.72* | |||
| Emotion Regulation Difficulties | ||||
| By Anxious Reactivity | 2.42 | 0.30 | 0.08* | |
| Model 2: Emotion Regulation Difficulties and Skin Conductance Reactivity | ||||
| Step 1 | 0.50** | |||
| Emotion Regulation Difficulties | 3.35 | 0.57 | 0.31** | |
| Skin Conductance Reactivity | 1.99 | 0.34 | 0.11 | |
| Step 2 | 0.61* | |||
| Emotion Regulation Difficulties | ||||
| By Skin Conductance Reactivity | 2.13 | 0.35 | 0.10* | |
p < .001;
p < .01;
p < .05
A significant omnibus regression also emerged when examining skin conductance reactivity to the traumatic event script [F(3, 17) = 8.73, p < .01]. In step 1 of the model, emotion regulation difficulties accounted for significant variability in posttraumatic stress symptom severity, while change in skin conductance did not reach significance. The interaction between emotion regulation difficulties and skin conductance reactivity entered into step 2 significantly accounted for an additional 10.5% of the total variance in posttraumatic stress symptoms. In combination, the model accounted for a total of 60.6% of the variability in posttraumatic stress symptom severity.
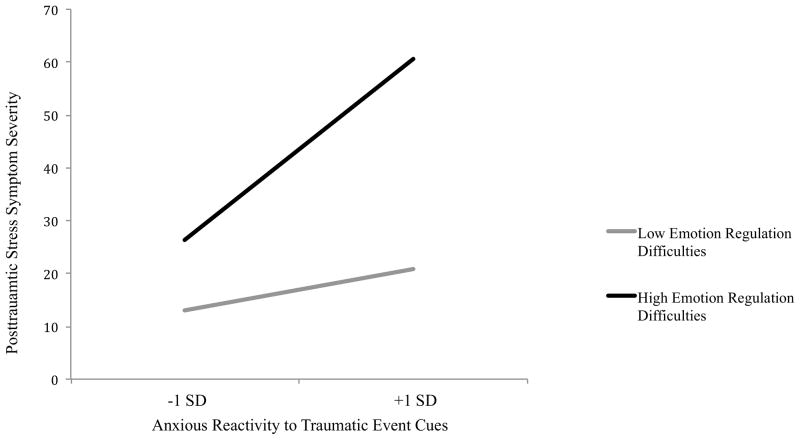
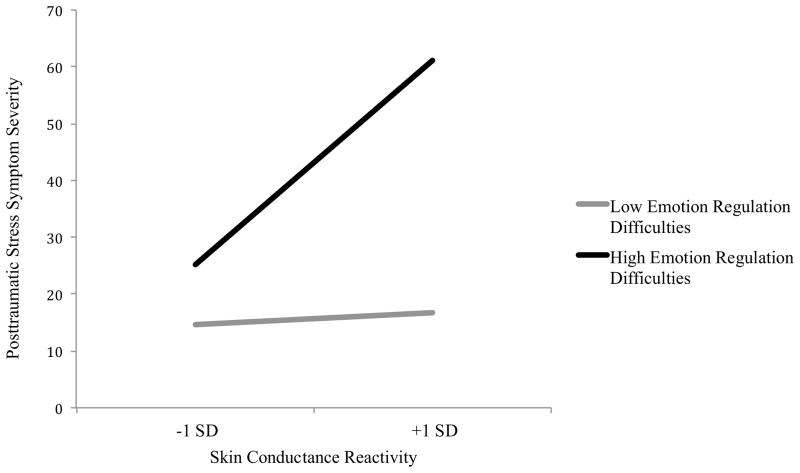
Post hoc probing analyses suggested (as depicted in Figure 1) that self-reported anxious reactivity to the traumatic event script was significantly positively associated with posttraumatic stress symptom severity among individuals with elevated emotion regulation difficulties (β = .76, t = 4.99, p < .001, sr2 = .36), but not among those low in emotion regulation difficulties (β = .15, t = .91, p = .37, sr2 = .01). A similar pattern emerged with respect to skin conductance reactivity (Figure 2). Skin conductance reactivity to the traumatic event script was significantly positively associated with posttraumatic stress symptom severity among individuals with relatively elevated emotion regulation difficulties (β = .80, t = 3.00, p < .01, sr2 = .21), but not among those relatively low in emotion regulation difficulties (β = .10, t = 0.53, p = .60, sr2 = .01).
Figure 1.
Interaction between anxious reactivity in response to the traumatic event script and emotion regulation difficulties in predicting posttraumatic stress symptom severity.
Figure 2.
Interaction between skin conductance reactivity in response to the traumatic event script and emotion regulation difficulties in predicting posttraumatic stress symptoms.
4. Discussion
There is increasing recognition of the link between emotion regulation difficulties and posttraumatic stress symptom severity (Chemtob et al., 1997; Cloitre et al., 2005; Price et al., 2006; Tull et al., 2007). However, there has been a dearth of research examining the nature of this association. The current study was the first to explore the interaction between emotion regulation difficulties and traumatic event-related emotional reactivity in predicting posttraumatic stress symptom severity. Results were consistent with hypotheses.
A significant association between emotion regulation difficulties and posttraumatic stress symptom severity emerged. This supports prior research (Chemtob et al., 1997; Cloitre et al., 2005; Pickett, Bardeen, & Orcutt, 2011; Price et al., 2006; Tull et al., 2007) and extended it by demonstrating that the association held even after either subjective or physiological reactivity to the traumatic event script was simultaneously entered into the regression. As such, this pattern suggests a unique association between difficulty regulating emotion and posttraumatic stress symptom severity above and beyond self-reported anxious reactivity to traumatic event cues. Moreover, the magnitude of the observed association was large (Cohen, 1988; Kirk, 1996).
A large association between self-reported anxious reactivity to the traumatic event script and posttraumatic stress symptom severity also emerged. The association between skin conductance reactivity to the traumatic event script was below the statistical significance threshold, but the medium to large effect size, and the breadth of research that has documented increased emotional reactivity as assessed by peripheral (see Orr and Roth [2000] for a review) and central (Britton, Phan, Taylor, Fig, & Liberzon, 2005; Shin et al., 1999, 2004) measures of physiological reactivity among individuals with PTSD, it is likely that the current study was insufficiently powered to detect a main effect. However, non-significant associations between physiological reactivity to traumatic event cues and continuous measures of posttraumatic stress severity have also been observed in some larger samples (e.g., Pineles et al., 2011). Thus, while additional research is needed that extends the current study via a larger sample size, alternative possibilities for this null result should also be considered. For example, Cuthbert and colleagues (2003) have observed greater discordance between self-reported distress and physiological reactivity in response to imagery among persons with PTSD as compared to some other anxiety disorders. Specifically, as compared to those with specific phobias or social anxiety disorder, individuals with PTSD evidence higher levels of self-reported arousal and negative valence, while physiological reactivity is generally dampened in response to individualized fear cues. Dissociation or emotional numbing as means to disengage from the traumatic memory has been offered as one possibility to account for dampened physiological responding among some individuals with PTSD (see Lanius et al. [2006, 2010] for reviews). While approximately 70% of individuals with PTSD respond to individualized traumatic event imagery with a pattern of increased subjective and physiological reactivity, the other 30% display dampened physiological arousal that is accompanied by unique patterns of brain activation consistent with self-reported feelings of depersonalization and derealization (Lanius et al., 2001, 2002). Future research in this area should factor in individual differences in dissociation when examining relations between traumatic event-related physiological reactivity and posttraumatic stress.
Finally, significant interactions emerged between emotion regulation difficulties and both self-reported anxious and physiological reactivity to the traumatic event script in predicting posttraumatic stress symptom severity. The direction of these interactions was as expected; measures of traumatic event-related subjective and physiological reactivity were both associated with posttraumatic stress symptom severity, but only among those relatively high in emotion regulation difficulties. Associations between measures of emotional reactivity and posttraumatic stress symptom severity were medium/large to large (Cohen, 1998; Kirk, 1996) among individuals relatively high in emotion regulation difficulties. These can be contrasted to the small and non-significant associations observed among individuals relatively low in emotion regulation difficulties. Taken together these results suggest the pattern of interactions observed here is likely reliable despite the relatively small sample.
These results are consistent with the supposition that emotional reactivity to traumatic event cues may contribute to the maintenance of posttraumatic stress symptom severity when combined with relative difficulties regulating such increased reactivity. In addition, the observed pattern parallels the results of Pineles and colleagues (2011) in which avoidance coping was found to moderate the association between traumatic event-related emotional reactivity and posttraumatic stress symptom severity. Use of the well-established script-driven imagery procedure (Orr et al., 1990; Pitman et al., 1987) was considered a methodological strength of the current study, allowing for a real-time assessment of traumatic event-related emotional reactivity in response to an individualized traumatic event script in the controlled environment of the laboratory. Moreover, use of multi-modal assessment of emotional reactivity in the current study (i.e., self-report, physiological) represents an important and novel extension to prior work examining emotion regulation in the context of posttraumatic emotional reactivity. Evidence of desynchrony between self-report and physiological indicators of emotion in response to traumatic event-related cues in the laboratory (e.g., Orr et al., 1993) highlights that patterns observed within a single mode of response cannot be assumed to generalize across modes.
In light of evidence suggesting emotion regulation difficulties may lead to increased behavioral avoidance among traumatic event-exposed individuals (Gratz et al., 2007), future research is now needed to investigates a potential mediating role for both general and traumatic event-specific avoidance coping in the association between emotion regulation difficulties and posttraumatic stress symptom severity. Importantly, the cross-sectional nature of the current study precludes conclusions regarding the specific role of emotion regulation difficulties in the maintenance of posttraumatic stress symptoms per se. Additional longitudinal research is needed to address the temporal patterning among emotion regulation difficulties, emotional reactivity to traumatic event cues, and posttraumatic stress symptoms.
Limitations of the current study (in addition to those considered above) and future directions for research in this area warrant discussion. First, the current results need to be replicated in larger and more diverse samples. The current sample was comprised of predominately Caucasian women with a history of sexual or physical assault. Replication of the current findings among individuals with a range of traumatic event experiences as well as among men and racial/ethnic minorities is needed. Future research would also benefit from expanding the measurement of traumatic event-related emotional reactivity to include additional indices of physiological (e.g., heart rate, facial electromyography) and self-reported (e.g., VAS ratings of anger, shame, guilt, and disgust) reactivity (Badour et al., 2011; Olatunji et al., 2009; Orr et al., 1990; Shin et al., 1999). Research is needed that measures specific domains of emotion regulation, as opposed to the measure of general emotion regulation difficulties adopted herein. Both self-report and measures of real-time emotion regulation including behavioral, physiological, and neuroimaging assessment strategies should be adopted. Also, the generalizability of the current results to a sample of people meeting diagnostic criteria for PTSD needs to be tested. The fact that nearly 30% of participants in the current sample met criteria for PTSD increases confidence in such generalizability. Moreover, taxometric research suggests posttraumatic stress symptomatology is dimensional in nature (as opposed to categorical; Broman-Fulks et al., 2009; Ruscio et al., 2002) and sampling a range of symptom severity circumvents restriction of variability in the criterion variables of interest. Nonetheless, it will be important to empirically test whether the current findings generalize to a sample of individuals meeting criteria for PTSD. Sampling exclusively for PTSD would oversample one end of the distribution of symptoms, which may lead to a different pattern of results than observed here.
Limitations notwithstanding, the present findings offer tentative clinical implications. Although existing empirically supported treatments for PTSD specifically aim to reduce traumatic event-related emotional reactivity through exposure and extinction processes, this study highlights the importance of considering the influence of emotion regulation difficulties within this context. Specifically, those with difficulties recognizing and appropriately regulating aversive emotional states elicited by traumatic event cues may benefit from treatment aimed at improving these skills prior to engaging in exposure-based treatment. Indeed, emerging research suggests improvement in emotion regulation abilities predicts greater reduction in PTSD symptoms (Cloitre et al., 2002; Price et al., 2006) across the course of exposure-based treatment. However, others have argued that a focus on enhancing emotion regulation skills may interfere with the efficacy of exposure by introducing the use of safety signals or behaviors (Sloan & Telch, 2002). Additional research in this area is clearly needed.
Taken as a whole, the current study offers a novel and important contribution to furthering our understanding of the interplay among traumatic event-related emotional reactivity, emotion regulation difficulties, and posttraumatic stress symptom severity. These findings highlight the need for further elaboration of the unique and combined contributions of these factors to understanding the etiology and maintenance of PTSD.
Reactivity to traumatic event cues have been related to posttraumatic stress.
Emotion regulation difficulties have also been linked to posttraumatic stress.
This study examined how these factors interact to predict posttraumatic stress.
Physiological and subjective reactivity predicted posttraumatic stress.
This relation was only significant for those with difficulties regulating emotion.
Acknowledgments
Role of Funding Organizations
This research was supported, in part, by a NIMH National Research Service Award (F31 MH092994-01) as well as a grant from the Marie Wilson Howells Foundation in the Department of Psychological Science at the University of Arkansas, both awarded to the first author.
Footnotes
Declaration of Interest
There are no conflicts of interest to be declared for either author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Amir M, Kaplan Z, Kotler M. Type of trauma, severity of posttraumatic stress disorder core symptoms, and associated features. The Journal of General Psychology. 1996;123:341–351. doi: 10.1080/00221309.1996.9921286. [DOI] [PubMed] [Google Scholar]
- Badour CL, Feldner MT, Babson KA, Smith RC, Blumenthal H, Trainor CD, Bunaciu L, Olatunji BO. Differential emotional responding to ideographic cues of traumatic interpersonal violence compared to non-interpersonal traumatic experiences. Journal of Experimental Psychopathology. 2011;2:400–417. doi: 10.5127/jep.014711. [DOI] [Google Scholar]
- Badura AS. Journal of Anxiety Disorders. Vol. 17. Hillsdale, NJ: Erlbaum; 2003. Theoretical and empirical exploration of the similarities between emotional numbing in posttraumatic stress disorder and alexithymia; pp. 349–360. behavioral sciences. [DOI] [PubMed] [Google Scholar]
- Blake D, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Britton JC, Phan KL, Taylor SF, Fig LM, Liberzon I. Corticolimbic blood flow in posttraumatic stress disorder during script-driven imagery. Biological Psychiatry. 2005;8:832–840. doi: 10.1016/j.biopsych.2004.12.025. doi: dx.doi.org/10.1016/j.biopsych.2004.12.025. [DOI] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Ruggiero KJ, Green BA, Smith DW, Hanson RF, Kilpatrick DG, Saunders BE. The latent structure of posttraumatic stress disorder among adolescents. Journal of Traumatic Stress. 2009;22:146–152. doi: 10.1002/jts.20399. [DOI] [PubMed] [Google Scholar]
- Brunet A, Orr SP, Tremblay J, Robertson K, Nader K, Pitman RK. Effect of post-retrieval propranolol on psychophysiologic responding during subsequent script-driven traumatic imagery in post-traumatic stress disorder. Journal of Psychiatric Research. 2008;42:503–506. doi: 10.1016/j.jpsychires.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Carson MA, Paulus LA, Lasko NB, Metzger LJ, Wolfe J, Orr SP, Pitman RK. Psychophysiologic assessment of posttraumatic stress disorder in Vietnam nurse veterans who witnessed injury or death. Journal of Consulting and Clinical Psychology. 2000;68:890–897. doi: 10.1037/0022-006X.68.5.890. [DOI] [PubMed] [Google Scholar]
- Catanzaro SJ, Mearns J. Measuring generalized expectancies for negative mood regulation: Initial scale development and implications. Journal of Personality Assessment. 1990;54:546–563. doi: 10.1080/00223891.1990.9674019. [DOI] [PubMed] [Google Scholar]
- Chemtob CM, Novaco RW, Hamada RS, Gross DM, Smith G. Anger regulation deficits in combat-related posttraumatic stress disorder. Journal of Traumatic Stress. 1997;10:17–36. doi: 10.1023/A:1024852228908. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology. 2002;70:1067–1074. doi: 10.1037//0022-006X.70.5.1067. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Miranda R, Stovall-McClough KC, Han H. Beyond PTSD: Emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behavior Therapy. 2005;36:119–124. doi: 10.1016/S0005-7894(05)80060-7. [DOI] [Google Scholar]
- Cohen J. Statistical power analysis for behavioral sciences. 2. Hillsdale NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the. 1983. [Google Scholar]
- Craske MG. Anxiety disorders: Psychological approaches to theory and treatment. Boulder, Colorado: Westview Press; 1999. [Google Scholar]
- Cuthbert BN, Lang PJ, Strauss C, Drobes D, Patrick CJ, Bradley MM. The psychophysiology of anxiety disorder: Fear memory imagery. Psychophysiology. 2003;40:407–422. doi: 10.1111/1469-8986.00043. [DOI] [PubMed] [Google Scholar]
- Ehring T, Quack D. Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy. 2010;41:587–598. doi: 10.1016/j.beth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Etkin A, Wager TD. Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. American Journal of Psychiatry. 2007;164:1476–1488. doi: 10.1016/j.beth.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. doi: 10.1037/0033-2909.99.1.20. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO. Treating the trauma of rape: Cognitive-behavioral therapy for PTSD. New York, NY: Guilford Press; 1998. [Google Scholar]
- Foa EB, Zinbarg R, Rothbaum BO. Uncontrollability and unpredictability in post-traumatic stress disorder: An animal model. Psychological Bulletin. 1992;112:218–238. doi: 10.1037/0033-2909.112.2.218. [DOI] [PubMed] [Google Scholar]
- Freyd M. The graphic rating scale. Journal of Educational Psychology. 1923;14:83–102. doi: 10.1037/h0074329. [DOI] [Google Scholar]
- Gratz KL, Bornovalova MA, Delany-Brumsey A, Nick B, Lejuez CW. A laboratory-based study of the relationship between childhood abuse and experiential avoidance among inner-city substance users: The role of emotional nonacceptance. Behavior Therapy. 2007;38:256–268. doi: 10.1016/j.beth.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004 doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Gross J. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998;2:271–299. [Google Scholar]
- Hendryx MS, Haviland MG, Shaw DG. Dimensions of alexithymia and their relationships to anxiety and depression. Journal of Personality Assessment. 1991;56:227–237. doi: 10.1207/s15327752jpa5602_4. [DOI] [PubMed] [Google Scholar]
- Hodgson R, Rachman S. Desynchrony in measures of fear. Behaviour Research and Therapy. 1974;12:319–326. doi: 10.1016/0005-7967(74)90006-0. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Hyer L, Woods MG, Summers MN, Boudewyns P, Harrison WR. Alexithymia among Vietnam veterans with posttraumatic stress disorder. Journal of Clinical Psychiatry. 1990;51:243–247. [PubMed] [Google Scholar]
- Kashdan TB, Breen WE, Julian T. Everyday strivings in war veterans with posttraumatic stress disorder: Suffering from a hyper-focus on avoidance and emotion regulation. Behavior Therapy. 2010;41:350–363. doi: 10.1016/j.beth.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane TM, Barlow DH. Posttraumatic stress disorder. In: Barlow DH, editor. Anxiety and its disorder: The nature and treatment of anxiety and panic. New York, NY: Guilford Press; 2002. pp. 418–452. [Google Scholar]
- Keane TM, Zimering RT, Caddell JM. A behavioral formulation of posttraumatic stress disorder in Vietnam Veterans. The Behavior Therapist. 1985;8:9–12. [Google Scholar]
- Kirk RE. Practical significance: A concept whose time has come. Educational and Psychological Measurement. 1996;56:746–759. doi: 10.1177/001316449056005002. [DOI] [Google Scholar]
- Klemanski DH, Mennin DS, Borelli JL, Morrissey PM, Aikins DE. Emotion-regulated regulatory difficulties contribute to negative psychological outcomes in active-duty Iraq war soldiers with and without posttraumatic stress disorder. Depression and Anxiety. 2012;29:621–628. doi: 10.1002/da.21914. [DOI] [PubMed] [Google Scholar]
- Lanius RA, Bluhm R, Lanius U, Pain C. A review of neuroimaging studies in PTSD: Heterogeneity of response to symptom provocation. Journal of Psychiatric Research. 2006;40:79–729. doi: 10.1016/j.jpsychires.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, Spiegel D. Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. American Journal of Psychiatry. 2010;167:640–647. doi: 10.1176/appi.ajp.2009.09081168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanius RA, Williamson MD, Densmore M, Boksman K, Gupta MA, Neufeld RW, Menon RS. Neural correlates of traumatic memories in posttraumatic stress disorder. A functional MRI investigation. The American Journal of Psychiatry. 2001;158:1920–1922. doi: 10.1176/appi.ajp.158.11.1920. [DOI] [PubMed] [Google Scholar]
- Lanius RA, Williamson PC, Boksman K, Densmore M, Gupta M, Neufeld RWJ, Menon RS. Brain activation during script-driven imagery induced dissociative responses in PTSD: A functional magnetic resonance imaging investigation. Biological Psychiatry. 2002;52:305–311. doi: 10.1016/S0006-3223(02)01367-7. [DOI] [PubMed] [Google Scholar]
- Lanius RA, Williamson PC, Hopper J, Densmore M, Boksman K, Gupta MA, Menon RS. Recall of emotional states in posttraumatic stress disorder: An fMRI investigation. Biological Psychiatry. 2003;53:204–210. doi: 10.1016/S0006-3223(02)01466-X. [DOI] [PubMed] [Google Scholar]
- Liberzon I, Garfinkel SN. Functional neuroimaging in post-traumatic stress disorder. In: Shiromani PJ, Keane TM, LeDoux JE, editors. Post-traumatic stress disorder: Basic science and clinical practice. New York, NY: Humana Press; 2009. pp. 297–317. [Google Scholar]
- Liberzon I, Taylor SF, Amdur R, Jung TD, Chamberain KR, Minoshima S, Fig LM. Brain activation in PTSD in response to trauma-related stimuli. Biological Psychiatry. 1999;45:817–826. doi: 10.1016/S0006-3223(98)00246-7. [DOI] [PubMed] [Google Scholar]
- Maercker A, Michael T, Fehm L, Becker ES, Margraf J. Age of traumatisation as a predictor of post-traumatic stress disorder or major depression in young women. British Journal of Psychiatry. 2004;184:482–487. doi: 10.1192/bjp.184.6.482. [DOI] [PubMed] [Google Scholar]
- McDonagh-Coyle A, McHugo GJ, Friedman MJ, Schnurr PP, Zayfert C, Descamps M. Psychological reactivity in female sexual abuse survivors. Journal of Traumatic Stress. 2001;14:667–683. doi: 10.1023/A:1013081803429. [DOI] [PubMed] [Google Scholar]
- Monson CM, Price JL, Rodriguez BF, Ripley MP, Warner RA. Emotional deficits in military-related PTSD: An investigation of content and process disturbances. Journal of Traumatic Stress. 2004;17:275–279. doi: 10.1023/B:JOTS.0000029271.58494.05. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Babson KA, Smith RC, Feldner MT, Connolly KM. Gender as a moderator of the relation between PTSD and disgust: A laboratory test employing individualized script-driven imagery. Journal of Anxiety Disorders. 2009;23:1091–1097. doi: 10.1016/j.janxdis.2009.07.012. [DOI] [PubMed] [Google Scholar]
- Orr SP, Roth WT. Psychophysiological assessment: Clinical applications for PTSD. Journal of Affective Disorders. 2000;61:225–240. doi: 10.1016/S0165-0327(00)00340-2. [DOI] [PubMed] [Google Scholar]
- Orr SP, Claiborn JM, Altman B, Forgue DF, de Jong JB, Pitman RK, Herz LR. Psychometric profile of posttraumatic stress disorder, anxious, and healthy Vietnam veterans: Correlations with psychophysiologic responses. Journal of Consulting and Clinical Psychology. 1990;58:329–335. doi: 10.1037/0022-006X.58.3.329. [DOI] [PubMed] [Google Scholar]
- Orr SP, Pitman RK, Lasko NB, Herz LR. Psychophysiological assessment of posttraumatic stress disorder imagery in World War II and Korean combat veterans. Journal of Abnormal Psychology. 1993;102:152–159. doi: 10.1037/0021-843X.102.152. [DOI] [PubMed] [Google Scholar]
- Pickett SM, Bardeen JR, Orcutt HK. Experiential avoidance as a moderator of the relationship between behavioral inhibition system sensitivity and posttraumatic stress symptoms. Journal of Anxiety Disorders. 2011;25:1038–1045. doi: 10.1016/j.janxdis.2011.06.013. [DOI] [PubMed] [Google Scholar]
- Pineles SL, Mostoufi SM, Ready CB, Street AE, Griffin MG, Resick PA. Trauma reactivity, avoidant coping, and PTSD symptoms: A moderating relationship? Journal of Abnormal Psychology. 2011;120:240–246. doi: 10.1037/a0022123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitman RK, Lanes DM, Williston SK, Guillaume JL, Metzger LJ, Gehr GM, Orr SP. Psychophysiologic assessment of posttraumatic stress disorder in breast cancer patients. Psychosomatics. 2001;42:133–140. doi: 10.1176/appi.psy.42.2.133. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Forgue DF, Altman B, Je Jong JB, Herz LR. Psychophysiologic responses to combat imagery of Vietnam veterans with posttraumatic stress disorder versus other anxiety disorders. Journal of Abnormal Psychology. 1990;99:49–54. doi: 10.1037//0021-843x.99.1.49. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Forgue DF, de Jong J, Claiborn J. Psychophysiologic assessment of posttraumatic stress disorder imagery in Vietnam combat veterans. Archives of General Psychiatry. 1987;44 (11):970–975. doi: 10.1001/archpsyc.1987.01800230050009. [DOI] [PubMed] [Google Scholar]
- Price JL, Monson CM, Callahan K, Rodriguez BF. The role of emotional functioning in military-related PTSD and its treatment. Journal of Anxiety Disorders. 2006;20:661–674. doi: 10.1016/j.janxdis.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Riggs DS, Rothbaum BO, Foa EB. A prospective examination of symptoms of posttraumatic stress disorder in victims of nonsexual assault. Journal of Interpersonal Violence. 1995;10:201–214. doi: 10.1177/0886260595010002005. [DOI] [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress. 1992;5:455–475. doi: 10.1007/BF00977239. [DOI] [Google Scholar]
- Ruscio AM, Ruscio J, Keane TM. The latent structure of posttraumatic stress disorder. A taxometric investigation of reactions to extreme stress. Journal of Abnormal psychology. 2002;111:290–301. doi: 10. 1037//001-843X.111.2.290. [DOI] [PubMed] [Google Scholar]
- Shin LM, McNally RJ, Kosslyn SM, Thompson WL, Rauch SL, Alpert NM, Pitman RK. Regional cerebral blood flow during script-driven imagery in childhood sexual abuse-related PTSD: A PET investigation. American Journal of Psychiatry. 1999;156:575–584. doi: 10.1176/ajp.156.4.575. [DOI] [PubMed] [Google Scholar]
- Shin LM, Orr SP, Carson MA, Rauch SL, Macklin ML, Lasko NB, Pitman RK. Regional cerebral blood flow in the amygdala and medial prefrontal cortex during traumatic imagery in male and female Vietnam veterans with PTSD. Archives of General Psychiatry. 2004;61:168–176. doi: 10.1001/archpsyc.61.2.168. [DOI] [PubMed] [Google Scholar]
- Sloan T, Telch MJ. The effects of safety-seeking behavior and guidedthreat reappraisal on fear reduction during exposure: An experimental investigation. Behaviour Research and Therapy. 2002;40:235–251. doi: 10.1016/S0005-7967(01)00007-9. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5. Boston, MA: Pearson Education, Inc; 2007. [Google Scholar]
- Taylor GJ, Bagby RM, Parker JDA. The alexithymia construct: A potential paradigm for psychosomatic medicine. Psychosomatics. 1991;32:153–164. doi: 10.1016/S0033-3182(91)72086-0. [DOI] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, Roemer L. A preliminary investigation of the relation between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;38:303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JT. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio A, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124–133. doi: 10.1037/1040-3590.11.2.124. [DOI] [Google Scholar]
- Wolfe J, Chrestman KR, Ouimette PC, Kaloupek D, Harley M, Bucsela M. Trauma-related psychophysiological reactivity in women exposed to war-zone stress. Journal of Clinical Psychology. 2000;56:1371–1379. doi: 10.1002/1097-4679(200010)56:10<1371::AID-JCLP8>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]