Abstract
Much research has focused on the possible overuse of health care services within Medicare, but there is also substantial evidence of underuse. In recent years, Congress has added a “welcome to Medicare” physician visit and a number of preventive services with no cost sharing to the Medicare benefit package to encourage early and appropriate use of services. We examined national longitudinal data on first claims for Part B services—the portion of Medicare that covers physician visits—to learn how people used these benefits. We found that 12 percent of people, or about one in eight, who enrolled in Medicare at age sixty-five waited more than two years before making their first use of care covered by Part B. In part, this delay reflected patterns of use before enrollment, in that people who sought preventive care before turning sixty-five continued to do so after enrolling in Medicare. Enrollees with Medigap coverage, higher household wealth, and a higher level of education typically received care under Part B sooner than others, whereas having greater tolerance for risk was more likely to lead enrollees to delay use of Part B services. Men had a lower probability of using Part B services early than women; blacks and members of other minority groups were less likely to use services early than whites. Although the “welcome to Medicare” checkup does not appear to have had a positive effect on use of services soon after enrollment, the percentage of beneficiaries receiving Part B services in the first two years after enrollment has steadily increased over time. Whether or not delays in receipt of care should be a considerable public policy concern may depend on what factors are leading specific categories of enrollees to delay care and how such delays affect health.
Constraining the rate of growth in spending for Medicare, a public insurance program with uniform benefits, is a widely acknowledged goal for federal fiscal policy. At the same time, there has long been empirical evidence of differences in use of Medicare by different enrollees. This evidence first emerged soon after Medicare was implemented in 1966,1 and the differences have persisted.2–6
One might expect there to be overuse by Medicare beneficiaries for various reasons, such as what is called moral hazard—which in this context means higher use of services when patient cost sharing is reduced. However, there is also substantial evidence of underuse.7–9 Underuse of preventive and diagnostic services may lead to more expensive care and a higher cost burden on Medicare in later years.
A provision of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, which took effect January 1, 2005, sought to increase newly enrolled beneficiaries’ immediate use of benefits. The legislation included a “welcome to Medicare” check-up within the first six months of enrollment with no beneficiary cost sharing. This initial preventive physical examination was intended to give new beneficiaries up-to-date screenings and vaccinations, and to allow providers to learn about the patient’s medical history.
Reasons for differences in use and for under-use are complex, involving decisions by not only health professionals but also beneficiaries.10 For example, the timing of a Medicare beneficiary’s initial visit is likely to be largely driven by that beneficiary.
Using a nationally representative sample of people who turned sixty-five, we found that 12 percent of new beneficiaries did not have an encounter resulting in a Medicare claim for Part B services within the first two years of enrollment. Some beneficiaries waited five or more years after enrollment before having an initial encounter. This study used data from a longitudinal survey of people that tracked them before and after Medicare eligibility. Our purpose was to analyze the transition into eligibility and to assess the determinants of time between enrollment and an initial encounter.
Study Data And Methods
DATA
We used data from the Health and Retirement Study11 to identify a nationally representative sample of people who enrolled in Medicare at age sixty-five. A national, longitudinal household survey, the study measures health, functional, and cognitive status; demographic characteristics; insurance coverage; and income and wealth among five cohorts of US near-elderly and elderly people.
Members of the initial cohort, consisting of people born during the period 1931–41 and their spouses, who could be of any age, were first interviewed in 1992 and then in every even-numbered year. The most recent interviews were conducted in 2010. For these beneficiaries, Medicare claims and data on dates of death and enrollment in Medicare risk plans (health maintenance organizations) have been merged with the survey data.
We included people in our analysis if they first enrolled in Medicare in the period 1993–2005 and if they were never enrolled before age sixty-five and never enrolled in a Medicare Advantage (managed care) plan after reaching age sixty-five. This exclusion was necessary because there are no claims data for Medicare Advantage enrollees. We excluded beneficiaries who died within two years of enrollment without filing a claim (n = 5).
ANALYSIS OF TIME TO FIRST MEDICARE PART B ENCOUNTER
We used survival analysis (Cox proportional hazard) to assess time from Medicare enrollment to the date of beneficiaries’ first encounter covered by Part B. Survival models relate the time that elapses before an outcome occurs, reflected in the dependent variable, to one or more explanatory variables. We excluded people not interviewed in the most recent Health and Retirement Study wave before they enrolled in Medicare and people with missing values on covariates. Of the 4,534 people in the original sample, 1,693 had not been interviewed before Medicare enrollment or had missing data on covariates, yielding an analysis sample of 2,841.
The dependent variable measured time from enrollment to first encounter in days. The first set of explanatory variables measured insurance coverage and use of services immediately prior to enrollment.
There are reasons why prior insurance coverage would lead to an earlier Part B encounter and why lack of coverage would lead to a later encounter. If people who were insured before enrolling in Medicare were persistent heavy users of services because they had a low threshold for seeking care, then the first Medicare encounter could be earlier.12
However, this seems unlikely to be the case because our two explanatory variables for prior insurance were binary variables for employer-provided coverage and Medicaid—with the value of 1 if a person was covered and 0 if he or she was not. Such insurance tends to be provided to people regardless of their care-seeking thresholds. Thus, having had such insurance coverage immediately prior to Medicare enrollment should increase time to first encounter after enrollment.
A binary variable for use of preventive services prior to enrollment was set to 1 if a beneficiary reported at the Health and Retirement Study interview immediately prior to becoming sixty-five that he or she had had at least one of the following services in the previous two years: a cholesterol test, flu shot, breast exam, prostate exam, mammogram, and pap smear. These procedures are recommended to be performed every year or every other year. People with such prior use are more prevention-oriented, and they may have been less likely to postpone a Part B encounter following Medicare enrollment.
We included a binary variable for private supplemental insurance following enrollment, set to 1 if a beneficiary had such insurance. The variable excluded employer-provided supplemental coverage. Such supplemental coverage was expected to decrease time to first encounter.13
People’s beliefs about their own longevity have two potentially offsetting effects. Those who think that they have a higher probability of surviving a decade tend to be healthier; thus, they may be expected to demand less care immediately following enrollment. However, people who are very pessimistic about living long also may eschew care. We defined a variable for a person’s stated probability of living to age seventy-five at the interview immediately prior to his or her Medicare enrollment. As a probability, the minimum value was 0 and the maximum 1, with fractions representing probabilities in between.
People who are risk tolerant, or not averse to taking risks, may be more likely to defer care. To measure this phenomenon, we used a measure from the survey, which posed various financial trade-offs to distinguish between people who were risk-tolerant and those who were not.14 The scale consisted of four values increasing in risk tolerance, with 0.57 being most risk-tolerant and 0.15 the least risk-tolerant. This scale is correlated with a variety of health and other behaviors.14,15
Another factor we considered was whether the person had a short- or long-term perspective in decision making. The survey asked people about the length of their financial planning horizons in years. People with shorter planning horizons in our study context should be less likely to consider the long-term benefits of health care services.
We included several explanatory variables for health and functional status at the interview immediately before Medicare enrollment. We expected people in worse health to use care more quickly after enrolling. We defined binary variables for the following conditions: a work-related disability—that is, a disability limiting the person’s ability to work; fair or poor health; diabetes mellitus; cancer; lung problems; heart problems; stroke; arthritis; and obesity. The survey’s questions on diagnoses referred to whether or not a doctor had told the respondent that she or he had the condition. Obesity was defined as a body mass index of greater than 30.
Limitations in activities in daily living (such as getting into or out of bed or using the toilet) and in instrumental activities in daily living (such as shopping or managing money) ranged from zero (no limitations) to a maximum of five for each type of activity. We used a modified Center for Epidemiologic Studies depression scale16 with a range of zero to eight—the highest number of symptoms of depression.
We included the following demographic characteristics: sex, race, educational attainment, marital status, and veteran status. We measured wealth as the household’s total assets, in scaled units of $100,000s. In other words, we divided the person’s assets by 100,000.
Finally, binary variables for year (1 if the observation came from a given year and 0 if it did not) measured the influence of long-term trends in care seeking and, for 2005, changes in time to visit caused by the Medicare Modernization Act. The coefficients on the year binary variables allowed us to compare care seeking in a particular year with care seeking at the baseline period 1993–95 (that is, the omitted reference group was 1993–95).
OTHER STATISTICAL ANALYSIS
To further assess the nature of the delays to the first Part B encounter, we used Part B Medicare claim files to identify the first eligible health care provider seen by sample beneficiaries after Medicare enrollment. The analysis sample was larger than in the previously described analysis of time to a first Part B encounter because we did not require information on explanatory variables (n = 4,534).
We excluded claims from providers in specialties that typically do not involve face-to-face interaction: anesthesiology, pathology, diagnostic radiology, and clinical laboratory. With the remaining claims, we searched for the first Part B encounter, documenting the type of specialist visited. We divided beneficiaries with Part B claims for care filed within the first fourteen years of enrollment into the following three groups: those with a claim within their first two years of enrollment; those whose first claim was in years 3–4; and those whose first claim was in years 5–14.
LIMITATIONS
This study has various limitations. First, although we assessed the importance of various factors in determining time to the first Part B encounter, the underlying factors are undoubtedly more complex than the ones we could document with this database of household interviews and claims.
Second, many health care episodes involve multiple diagnoses and providers. We relied on the initial claim filed, in effect counting the initial transaction that may have occurred in a given episode of utilization, although multiple claims from various specialties might have been filed later.
Third, specialty type might not reflect the actual training of the provider delivering care. For example, a physician assistant may be the primary care provider, but claims processing is done via the physician.
Fourth, we excluded encounters involving a few specialty types. Although there was a rationale for these exclusions, eliminating those specialties also had disadvantages. For example, initial claims filed by an anesthesiologist—an excluded group—could have been related to pain-related services in a face-to-face encounter.
Study Results
Beneficiaries with private health insurance supplemental to Medicare received care covered under Part B sooner after enrollment on average than other beneficiaries did (Exhibit 1). The probability of receipt of care was 34 percent higher if the person had Medigap insurance, a supplemental policy, than if he or she did not.
EXHIBIT 1.
New Medicare Beneficiaries’ Time To First Use Of Care Covered By Part B, 1993–2005
| Variable | Hazard ratioa |
|---|---|
| COVERAGE AND USE OF SERVICES BEFORE ENROLLMENT | |
| Employer-provided insurance | 1.03 |
| Medicaid | 1.02 |
| Preventive testing | 1.32*** |
| RISK PREFERENCE AND TIME HORIZON | |
| Risk tolerance | 0.64*** |
| Financial planning horizon, by year | 1.01 |
| HEALTH AND FUNCTIONAL STATUS | |
| Work-related disability | 1.23** |
| ADL limitations | 1.00 |
| IADL limitations | 1.07 |
| Fair/poor health | 1.08 |
| Diabetes mellitus | 1.25*** |
| Cancer | 1.12* |
| Lung problems | 1.19** |
| Heart problems | 1.13** |
| Stroke | 0.95 |
| Emotional problems | 1.01 |
| Arthritis | 1.10** |
| Obesity | 1.04 |
| DEMOGRAPHIC CHARACTERISTICS AND WEALTH | |
| Male | 0.89** |
| Black race | 0.85** |
| Other raceb | 0.75** |
| Educational attainment, by year | 1.02** |
| Married | 1.14*** |
| Veteran | 0.94 |
| Total assets, by $100,000s | 1.09*** |
| OTHER VARIABLES | |
| Private supplemental insurance (Medigap) | 1.34*** |
| Probability of living to age 75 | 0.86** |
| YEAR OF ENROLLMENT | |
| 1996 | 1.19 |
| 1997 | 0.99 |
| 1998 | 1.00 |
| 1999 | 1.35** |
| 2000 | 1.31** |
| 2001 | 1.17 |
| 2002 | 1.23 |
| 2003 | 1.55*** |
| 2004 | 1.61*** |
| 2005 | 1.52*** |
SOURCE Authors’ analysis of Health and Retirement Study data with linked Medicare claims files.
NOTES Binary variables for 1993–95 were omitted. ADL is activity of daily living. IADL is instrumental activity of daily living. For examples, see the text.
The hazard ratio shows how the probability of an outcome’s occurring changes when the explanatory variable changes by 1.
“Other race” is defined as nonwhite and nonblack.
p < 0.10
p < 0.05
p < 0.01
There were no significant relationships between having had employer-provided insurance or Medicaid prior to Medicare enrollment and time to first Part B encounter (Exhibit 1). However, people who sought preventive care before enrollment in Medicare and had low risk tolerance were significantly more likely than others to have a shorter time to their first encounter.
An increase in the subjective probability of living to age seventy-five decreased the probability of using Part B care (Exhibit 1). Even after we considered other health measures, including fair or poor health and the chronic conditions we studied, we found that people who projected longer survival for themselves tended to defer care use.
Among the twelve health and functional status variables, six were significant: work-related disability; diabetes mellitus; cancer; lung problems; heart problems; and arthritis (Exhibit 1). And except for veteran status, all demographic and wealth variables were significant. For example, men had a lower probability of using Part B services than women, and blacks and people who indicated “other race” had a lower probability than whites. Each additional year of schooling added 2 percent to the probability of using Part B care.
In addition, each additional $100,000 in assets raised the probability of Part B use by 9 percent (Exhibit 1). Given that mean assets were $38,000, this result implies important differences in the use of Part B benefits according to household wealth.
Relative to 1993–95, probabilities of use were significantly higher in 1999, 2000, and 2003–05 (Exhibit 1). These results imply that newly eligible beneficiaries had higher probabilities of use over time. However, although the estimated difference in probabilities between 2005 and 1993–95 was large and significant, the hazard ratio for 2005 was similar to the ratios for 2003 and 2004.
The percentage of beneficiaries receiving services covered by Part B within first two years of enrolling increased over time (Exhibit 2). A regression of the percentage receiving such services on the year of Medicare enrollment implies that the percentage receiving such services rose by 0.48 percent per year over the period 1993–2005. The 2005 observation lies above the regression line, implying an above-trend percentage in first use of Part B services in that year. However, the observation for 2002, before the Medicare Modernization Act was enacted and its provisions implemented, was almost as high.
EXHIBIT 2.
Trend In Percentage Of Beneficiaries Filing First Claims Within Two Years Of Medicare Enrollment
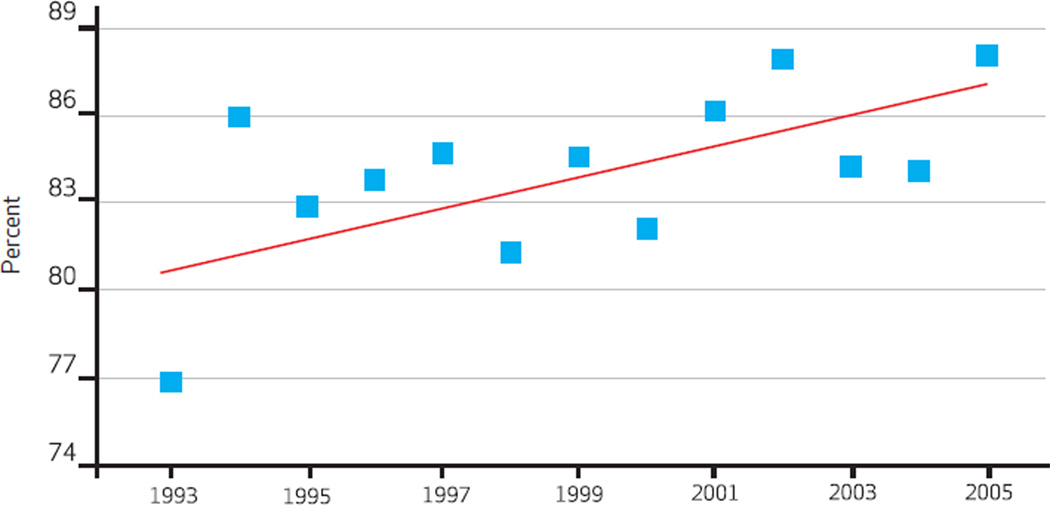 |
SOURCE Authors’ analysis of Health and Retirement Study data with linked Medicare claims files.
NOTES Slope is 0.48. Standard error is 0.20.
REASONS FOR FIRST ENCOUNTER WITH SERVICES COVERED BY PART B
Of the beneficiaries who filed their first Part B claim for care provided within fourteen years of enrollment in Medicare at age sixty-five, 88 percent—3,984 (Exhibit 3) out of the total sample of 4,534—filed their first claim within the first two years of enrollment. The primary diagnosis on the first claim differed according to how long after enrollment the claim was filed.
EXHIBIT 3.
Medicare Beneficiaries’ Primary Diagnosis At First Encounter Covered By Part B, 1993–2005
| Time after enrollment for first encounter |
|||
|---|---|---|---|
| Diagnosis/reason for visit | Years 1–2 (n = 3,984) |
Years 3–4 (n = 349) |
Years 5–14 (n = 201) |
| Acute bronchitis/bronchiolitis | 1.0% | 0.3% | 2.0% |
| Cardiac dysrhythmia | 0.9 | 1.7 | 2.0* |
| Cataract | 3.8 | 6.9*** | 6.5* |
| Chronic airway obstruction | 0.7 | 0.6 | 2.0** |
| Coronary atherosclerosis | 1.8 | 0.3** | 2.0 |
| Diabetes melitus | 4.5 | 2.6* | 3.0 |
| Hyperlipidemiaa | 4.1 | 2.6 | 1.0** |
| General symptoms | 1.5 | 1.4 | 2.5 |
| Glaucoma | 1.8 | 1.1 | 2.0 |
| Heart failure | 0.3 | 0.0 | 2.0*** |
| Hypertension | 10.4 | 12.3 | 4.5*** |
| Nonallopathic lesions, not classified | 1.7 | 2.0 | 0.0 |
| Osteoarthrosis/allied disorders | 1.9 | 2.3 | 1.0 |
| Respiratory and chest symptoms | 2.4 | 3.7 | 6.0*** |
| Vaccination | 4.6 | 3.7 | 5.5 |
| Total | 41.4 | 41.5 | 42.0 |
SOURCE Authors’ analysis of Health and Retirement Study data with linked Medicare claims files.
NOTES We used t tests to compare years 3–4 and years 5–14 with years 1–2. Not all diagnoses met the 2 percent threshold for inclusion in the table.
A disorder of lipid metabolism.
p < 0.10
p < 0.05
p < 0.01
For new enrollees with encounters in the first two years, hypertension was the most frequent diagnosis. Nineteen percent of initial claims filed for care in that period were for hypertension, diabetes mellitus, and hyperlipidemia—some of the most prevalent (and dependent on follow-up care) chronic illnesses. Almost 18 percent of initial claims filed in years 3–4 were for the same conditions. These results are broadly consistent with those shown in Exhibit 1, which identified particular preexisting chronic conditions as leading to a higher probability of receipt of services covered in Part B. Of initial encounters in years 5–14, only 7.5 percent were for hypertension and diabetes mellitus, and none were for hyperlipidemia.
The longer the beneficiary waited to see a provider for Part B care, the less likely the primary diagnosis was to be related to chronic disease or prevention, and the more likely it was to relate to acute respiratory symptoms and cataract (Exhibit 3). However, the overall results do not support the view that delayed use resulted in beneficiaries’ being more likely to use Part B care for severe acute illnesses. Cardiac dysrhythmias and acute bronchitis each constituted only 2 percent of diagnoses on the first claim for the group filing initial claims in years 5–14. This does not eliminate the possibility that visits requiring immediate attention existed. However, such visits do not dominate those made by the subsample.
TYPE OF PROVIDER SEEN AT FIRST ENCOUNTER
The type of provider seen also differed according to the time between enrollment and the first encounter for Plan B care (Exhibit 4). Even people who delayed obtaining Part B services were more likely to see a primary care provider than a specialist. Emergency medicine ranked third among beneficiaries who waited 3–4 years and those who waited 5–14 years to have their first encounter.
EXHIBIT 4.
Type Of Provider Seen By Medicare Beneficiaries At First Encounter Covered By Part B, 1993–2005
| Years 1–2 | Years 3–4 | Years 5–14 | |
|---|---|---|---|
| TYPE OF PROVIDER | |||
| Ambulance services | 0.5% | 1.7%*** | 5.5%*** |
| Cardiology | 4.4 | 5.2 | 8.5*** |
| Chiropractic | 3.0 | 4.3 | 0.0** |
| Dermatology | 3.2 | 1.1** | 0.5** |
| Emergency medicine | 2.6 | 7.4*** | 10.9*** |
| Family practice | 20.4 | 18.6 | 15.9 |
| General practice | 4.8 | 5.4 | 5.5 |
| General surgery | 2.0 | 2.3 | 2.5 |
| Internal medicine | 19.8 | 19.5 | 14.9* |
| Multispecialty clinic or group practice | 2.9 | 1.7 | 1.0 |
| Neurology | 0.6 | 0.6 | 2.5*** |
| Oncology | 0.4 | 1.1** | 2.5*** |
| Ophthalmology | 6.7 | 7.4 | 5.5 |
| Optometry | 3.9 | 5.2 | 6.5* |
| Orthopedic surgery | 2.6 | 2.9 | 3.5 |
| Urology | 2.4 | 2.6 | 2.0 |
| CATEGORY OF PROVIDER | |||
| Emergency carea | 3.4% | 9.5%*** | 12.0%*** |
| MD specialist | 37.9 | 32.1** | 35.3 |
| Non-MD specialist | 13.6 | 14.9 | 16.4 |
| Primary careb | 45.1 | 43.5 | 36.3** |
SOURCE Authors’ analysis of Health and Retirement Study data with linked Medicare claims files.
NOTES We used t tests to compare years 3–4 and years 5–14 with years 1–2. Specialties included were in the top ten first visits for at least one category. Sample sizes for each year category are provided in Exhibit 3.
Emergency care is emergency medicine and ambulatory services.
Primary care is family practice, internal medicine, and general practice.
p < 0.10
p < 0.05
p < 0.01
Family practice and internal medicine occupied the top two positions in all three groups (Exhibit 4). We grouped physician types into broader specialty categories, and the primary care category—family practice, internal medicine, and general practice—accounted for 45.1 percent of total encounters.
The frequency of initial encounters involving the use of emergency medicine increased as time between enrollment and filing the first claim did (Exhibit 4). The same is true for the broader category of emergency care, the sum of emergency medicine and ambulance services (encounters were coded as either emergency medicine or ambulance services, but not both, for an individual beneficiary). But emergency care represented only a minor source of care in all three groups.
Discussion
Medicare is a social insurance program offering equal benefits regardless of a beneficiary’s income or wealth. Yet 12 percent of people, or about one in eight, who enrolled in Medicare Part B at age sixty-five did not use this benefit during the first two years following enrollment, and roughly another 4 percent did not file a Part B claim within fourteen years following enrollment (computed from numbers of observations, Exhibit 3). The extent to which this outcome can be viewed as unfavorable depends in large part on the characteristics of beneficiaries who delayed in utilizing services covered by Part B and the types of encounters they had once they did use their coverage.
IS BENEFICIARIES’ DELAY IN USING CARE A PROBLEM?
From the vantage point of honoring consumer preferences, nonuse would be less of an issue if the beneficiaries who did not use services placed a lower value on health and tended to be less averse to taking risks. Indeed, we found that beneficiaries who did not obtain preventive services immediately prior to Medicare enrollment—a plausible indication that they attached a lower value to such services than people who did obtain them—and those who were more risk tolerant were more likely to delay filing their first claim for care covered by Part B.
People who were relatively optimistic about living to age seventy-five were also likely to delay getting Part B care. Here the question is whether or not they were unduly optimistic about their survival prospects, in which case we would not want to place as much weight on their views. However, the empirical evidence suggests that the near-elderly and elderly are quite good at gauging their survival prospects.17 We know that subjective beliefs about longevity take factors into account other than current health. In forming beliefs about their own survival, people consider the longevity of their parents.18
Also, people who before enrolling in Medicare had several chronic conditions that should be monitored by health professionals on a regular and ongoing basis were less likely to delay getting care covered by Part B. The fact that the results for all preexisting chronic disease variables were not significant is probably a by-product of multicollinearity, or correlations among the explanatory variables.
OTHER FINDINGS
Other findings support the view that delays in receipt of care should not be of considerable public policy concern. First, there is a significant positive trend, increasing over time, in the percentage of beneficiaries receiving services covered by Part B in the first two years after enrollment (Exhibit 2). Second, only a minority of beneficiaries who first received such services after the first two years received emergency care as their first Part B services (Exhibit 4). Of course, some beneficiaries might have benefited from care more if they had received it closer to their enrollment in Medicare. Third, consistent with this result, much of the delayed care was with primary care providers.
A few other findings are more troublesome, however. There appears to be a 15 percent differential in the probability of Part B use between whites and blacks (Exhibit 1). Also, even though benefits are uniform, our analysis documented differences in use according to household wealth. Given the high variation in household wealth, finding that the probability of use increased by almost a percentage point per $10,000 increase in wealth is a potential concern. We obtained this finding after controlling for educational attainment and marital status, which are systematically related to household wealth.
POLICY IMPLICATIONS
Two other results are of public policy interest. First, we found no statistical effect of the Medicare Modernization Act’s provisions for early use of Part B benefits, although the “welcome to Medicare” check-up was designed to encourage early and appropriate use of Medicare services.
Second, advocates for covering the uninsured have used potential cost offsets as an argument for extending health insurance to people who are currently uninsured. The argument is that people without coverage defer their use of services, leading to higher spending a few years later. In the context of our study, this would mean that consistent insurance coverage for people prior to enrolling in Medicare cuts down on utilization immediately after enrollment, because new beneficiaries have no need to rush out and get care they put off while they were uninsured. We found no evidence that people with insurance coverage prior to enrollment were more likely to delay receiving care covered by Part B. This lack of evidence does not imply that coverage extensions never produce such offsets. Rather, it suggests that extending coverage does not guarantee that cost offsets will be realized.
Our finding that eliminating a possible financial barrier to seeking care, the “welcome to Medicare” check-up, did not affect how long after enrollment people first sought care covered by Part B may seem counterintuitive, at least at first glance. There are several possible explanations for this result.
First, many new beneficiaries have existing chronic conditions that can be legitimately used as diagnoses to justify Medicare payment. For this reason, providers can record diagnoses for visits, and even check-ups will be viewed by Medicare as the physician monitoring a chronic condition.
Second, many new beneficiaries have existing relationships with their providers. Thus, although they are new to Medicare, the first Part B encounter is often not an encounter with a new provider.
Third, surprisingly, many Medicare beneficiaries have not taken advantage of screening and preventive benefits that Medicare has offered in the past. The reasons for the lack of benefit uptake are not well understood, but they might explain the failure to make use of this benefit.
Fourth, we excluded some beneficiaries who might be more price-sensitive than others from our empirical analysis, such as beneficiaries enrolled in health maintenance organization plans. If these beneficiaries are in fact more price-sensitive and have chosen to join managed care plans for their emphasis on preventive care, we may have underestimated the effect of the “welcome to Medicare” check-up.
Annual visits to a physician for people age sixty-five or older are recommended by the National Institutes of Health and the Department of Health and Human Services.19 In some cases, the barrier to obtaining this visit may be lack of geographic access to care or lack of providers’ willingness to accept Medicare. In addition, people vary in how they rank priorities, including health and health care, and this variance is reflected in differences in use of health care according to demographic and financial characteristics.
Our study has a series of important strengths. First, we tracked the time between Medicare enrollment and initial Part B encounter using data from the period immediately before enrollment. Thus, we could attribute patterns of care after enrollment to factors that preceded the decision to enroll. This linkage cannot be performed with data from more specialized Medicare data sources.
Second, the longitudinal feature of the Health and Retirement Study11 allowed for a follow-up period after enrollment of fourteen years. Third, unlike studies based entirely on claims data, the Health and Retirement Study provides data on variables that are highly related to utilization patterns not contained in claims data. Fourth, having claims data merged with household survey data meant that we did not have to rely on patient self-reports for information on utilization of health services.
In sum, a minority of Medicare beneficiaries delayed making their first use of covered care, which according to some guidelines represents subpar care. Although partly explainable, this type of difference in use, which has roots in care patterns before people become eligible for Medicare, has not been eliminated by a social insurance program that has been in existence for over four decades. Documenting whether or not health outcomes are worse when new beneficiaries delay making use of Medicare would be a useful subject for future research.
Acknowledgments
This research was supported in part by the National Institute on Aging (Grant No. 5R01AG017473-10).
Biographies
In this month’s Health Affairs, Frank Sloan and coauthors discuss their study of use of Part B services under Medicare, and their finding that about one in eight beneficiaries (12 percent) waited more than two years to make their first use of these services. Although use in this area is rising, they note that the “welcome to Medicare” check-up authorized by the Medicare Modernization Act of 2003 does not appear to have had a much of an effect.
Sloan is the J. Alexander McMahon Professor of Health Policy and Management and a professor of economics at Duke University. He is also president-elect of the American Society of Health Economics and chair of the Institute of Medicine committee on the study of geographic adjustment factors in Medicare payment. Sloan’s research interests include medical malpractice, long-term care, and the cost-effectiveness of medical technologies.
Sloan has previously served as chair of the health services research study section for the Agency for Healthcare Research and Quality, and he has chaired several Institute of Medicine committees. He received the National Institutes of Health Merit Award in 2005. Sloan holds a doctorate in economics from Harvard University.
Kofi Acquah is a doctoral student in economics at Brown University. He received a master’s degree in economics from Duke University.

Paul Lee is the F. Bruce Fralick Professor of Ophthalmology, director of the Kellogg Eye Center, and chair of the Department of Ophthalmology and Visual Sciences at the University of Michigan. He has published several papers on glaucoma and eye care delivery. Lee has a medical degree from the University of Michigan and a law degree from Columbia University.

Devdutta Sangvai is chief of the Division of Family Medicine in the Department of Community and Family Medicine, Duke University School of Medicine. Previously, he served as medical director at Duke Student Health. His research interests include quality, ambulatory practice efficiency, care redesign, and leadership development. Sangvai holds a medical degree from the University of Toledo and a master’s degree in business administration from Duke University.
Contributor Information
Frank A. Sloan, fsloan@duke.edu is the J. Alexander McMahon Professor of Health Policy and Management and a, professor of economics at Duke University
Kofi F. Acquah, Doctoral student in economics at Brown University, in Providence, Rhode Island
Paul P. Lee, F. Bruce Fralick Professor of Ophthalmology, director of the Kellogg Eye Center, and chair of the Department of Ophthalmology and Visual Sciences, all at the University of Michigan, in Ann Arbor
Devdutta G. Sangvai, Chief of the Division of Family Medicine, Department of Community and Family Medicine, at the Duke University School of Medicine, in Durham, North Carolina
NOTES
- 1.Feldstein MS. An econometric model of the Medicare system. Q J Econ. 1971;85(1):1–20. [Google Scholar]
- 2.Adams EK, Thorpe KE, Becker ER, Joski PJ, Flome J. Colorectal cancer screening, 1997–1999: role of income, insurance, and policy. Prev Med. 2004;38(5):551–557. doi: 10.1016/j.ypmed.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Blustein J, Weiss LJ. Visits to specialists under Medicare: socioeconomic advantage and access to care. J Health Care Poor Underserved. 1998;9(2):153–169. doi: 10.1353/hpu.2010.0451. [DOI] [PubMed] [Google Scholar]
- 4.Gross DJ, Alecxih L, Gibson MJ, Corea J, Caplan C, Brangan N. Outof- pocket health spending by poor and near-poor elderly Medicare beneficiaries. Health Serv Res. 1999;34(1 Pt 2):241–254. [PMC free article] [PubMed] [Google Scholar]
- 5.Niefeld MR, Kasper JD. Access to ambulatory medical and long-term care services among elderly Medicare and Medicaid beneficiaries: organizational, financial, and geographic barriers. Med Care Res Rev. 2005;62(3):300–319. doi: 10.1177/1077558705275418. [DOI] [PubMed] [Google Scholar]
- 6.Shea D, Stuart B, Vasey J, Nag S. Medicare physician referral patterns. Health Serv Res. 1999;34(1):331–348. [PMC free article] [PubMed] [Google Scholar]
- 7.Asch SM, Sloss EM, Hogan C, Brook RH, Kravitz RL. Measuring underuse of necessary care among elderly Medicare beneficiaries using inpatient and outpatient claims. JAMA. 2000;284(18):2325–2333. doi: 10.1001/jama.284.18.2325. [DOI] [PubMed] [Google Scholar]
- 8.Culler SD, Parchman ML, Przybylski M. Factors related to potentially preventable hospitalizations among the elderly. Med Care. 1998;36(6):804–817. doi: 10.1097/00005650-199806000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Doubeni CA, Laiyemo AO, Reed G, Field TS, Fletcher RH. Socioeconomic and racial patterns of colorectal cancer screening among Medicare enrollees in 2000 to 2005. Cancer Epidemiol Biomarkers Prev. 2009;18(8):2170–2175. doi: 10.1158/1055-9965.EPI-09-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 11.Health and Retirement Study. About the Health and Retirement Study [Internet] Ann Arbor (MI): The Study; [[cited 2012 May 11]]. Available from: http://hrsonline.isr.umich.edu/ [Google Scholar]
- 12.Einav L, Finkelstein A. Selection in insurance markets: theory and empirics in pictures. J Econ Perspect. 2011;25(1):115–138. doi: 10.1257/jep.25.1.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cartwright WS, Hu TW, Huang LF. Impact of varying Medigap insurance coverage on the use of medical services of the elderly. Appl Econ. 1992;24(5):529–539. [Google Scholar]
- 14.Barsky RB, Juster FT, Kimball MS, Shapiro MD. Preference parameters and behavioral heterogeneity: an experimental approach in the Health and Retirement Study. Q J Econ. 1997;112(2):537–579. [Google Scholar]
- 15.Picone G, Sloan F, Taylor D. Effects of risk and time preference and expected longevity on demand for medical tests. J Risk Uncertain. 2004;28(1):39–53. [Google Scholar]
- 16.Radloff LS. The CES-D scale: a selfreport depression scale for research in the general population. Appl Psychol Meas. 1977;1:285–401. [Google Scholar]
- 17.Smith VK, Taylor DH, Sloan FA. Longevity expectations and death: can people predict their own demise? Am Econ Rev. 2001;91(4):1126–1134. [Google Scholar]
- 18.Hamermesh DS. Expectations, life expectancy, and economic behavior. Q J Econ. 1985;100(2):389–408. [Google Scholar]
- 19.MedlinePlus. Physical exam frequency [Internet] Bethesda (MD): National Library of Medicine; [[last updated 2011 Apr 30; cited 2012 Apr 25]]. Available from: http:// www.nlm.nih.gov/medlineplus/ ency/article/002125.htm. [Google Scholar]


