Abstract
Objective
To identify primary care providers’ (PCPs) perceived barriers to educating patients about chronic kidney disease (CKD) during routine clinical visits.
Methods
We conducted three focus groups of eighteen PCPs in Baltimore, Maryland (MD), USA. Focus groups began with the presentation of a hypothetical case of a patient with CKD, followed by open-ended questions to assess providers’ perceived barriers to delivering education about CKD. Groups were audiotaped, transcribed, and coded independently by two investigators who identified major themes.
Results
PCPs reported on several patient, provider and system level barriers contributing to poor education about CKD in primary care that were both common and unique to barriers previously reported in educating patients regarding other chronic diseases.
Conclusions
Interventions designed to address barriers to CKD education identified by PCPs could improve the delivery of education about CKD in primary care settings.
Keywords: chronic kidney disease, primary care providers, patient education, barriers
Introduction
Most patients with chronic kidney disease (CKD) in the United States receive most of their medical care in primary care settings (Colleges, 2008, USRDS, 2011, Shahinian and Saran, 2010). As such, the primary care visit has been identified as a key venue through which intervention strategies to decrease the incidence and progression of CKD should be implemented (Shahinian and Saran, 2010, Tuot and Powe, 2011, Narva and Briggs, 2009, Plantinga et al., 2010) The majority of patients with CKD are not aware of their CKD diagnosis or the effect of poor risk factor control (such as hypertension and diabetes) on their health.(Waterman et al., 2008, Plantinga et al., 2010, Plantinga et al., 2008, Coresh et al., 2005, Nickolas et al., 2004).
The routine primary care visit represents an important opportunity for patients with CKD to learn about CKD and how to manage their risks of CKD incidence or progression. However, evidence suggests primary care providers discuss CKD with their patients infrequently and that the quality of patient-physician discussions about CKD in primary care is poor (Greer et al., 2011).
Recent studies of the quality of CKD care in primary care settings have employed questionnaires and medical record reviews to identify barriers to the diagnosis and treatment of CKD (Charles et al., 2009, Israni et al., 2009, Boulware et al., 2006, Allen et al., 2010, Fox et al., 2006, Lea et al., 2006, Lenz and Fornoni, 2006). However, these studies have provided limited information regarding reasons for ineffective CKD education in primary care. Qualitative studies allow participants to describe, in great detail, their experiences with delivering health care services, and provide an excellent opportunity to explore, in-depth, the nature of issues providers face in achieving desirable health care outcomes. Although qualitative studies may be less generalisable than population based studies, they allow providers to offer greater insight into the context of problems they face and can therefore offer insights that quantitative studies may not uncover. To date, very little is known about why patients in primary care settings have low awareness of their CKD despite significant efforts to improve patients’ and providers’ knowledge and awareness. We performed a qualitative study to identify primary care providers’ views regarding common barriers they face in educating their patients with CKD.
Methods
Three focus groups of eighteen primary care providers were performed to assess providers’ perceived barriers to educating patients about CKD during routine clinical visits.
Participants
A convenience sample of participants was recruited between April and October 2009 from Baltimore, Maryland area practices in the United States (USA). Recruitment efforts were targeted at the Maryland Chapter of the American College of Physicians and the Johns Hopkins Community Physicians practice sites to identify primary care providers working in various settings (i.e. community and academic medical center affiliated clinics) and serving adult patient populations with diverse socioeconomic and demographic backgrounds. To be included in the study, participants had to
be in active practice (at least 50% of the time) as a licensed primary care provider (e.g. internist, family physician, physician assistant, or nurse practitioner) who provided comprehensive, longitudinal care for patients and
provide clinical care for patients with CKD in their practice.
Oral and/or written consent was obtained from all participants. The study protocol was approved by the Johns Hopkins Medicine Institutional Review Board, the institutional ethics committee.
Data Collection
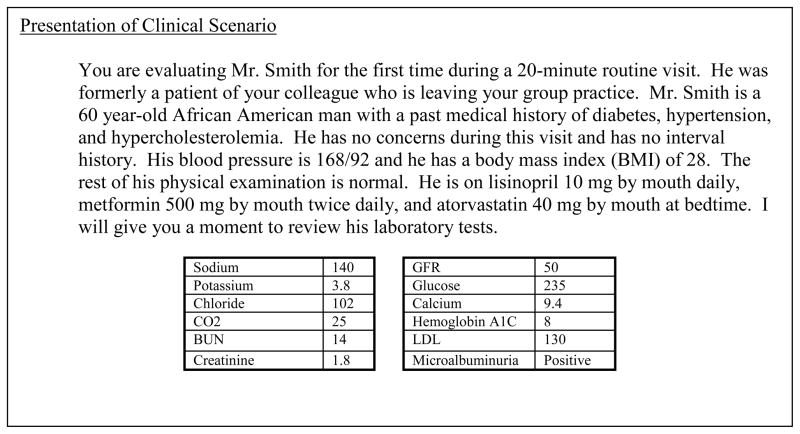
The focus groups were conducted in April, May, and October 2009. Each participating primary care provider completed a self-administered questionnaire at the beginning of the session, which included questions to assess their personal demographic (e.g. age, gender, race) and their clinical practice characteristics (e.g. years in practice and primary care specialty). All focus group sessions were 90 minutes and were facilitated by a trained moderator using a discussion guide. To provide primary care providers with a common context for their discussions about CKD education, focus group sessions were initiated by presenting primary care providers with a hypothetical patient scenario developed by the authors describing a 60 year-old African American man presenting as a new patient. The hypothetical patient had poorly controlled hypertension and diabetes, elevated cholesterol, obesity, and laboratory values consistent with CKD (see Figure 1).
Figure 1.
Text Box: Hypothetical Patient Scenario
After presenting the scenario, primary care providers were asked open-ended follow-up questions to identify their perceptions regarding the importance of educating their patients about CKD and their perceived barriers to educating patients similar to the hypothetical patient about CKD. Participants were asked:
in the context of a routine follow-up visit, what medical conditions they would educate this patient about
do they believe that their patients, similar to the one in the scenario, would be able to list CKD as a medical problem
what are the barriers to educating a patient about CKD, like the patient in the scenario with diabetes and hypertension
what items could be added to their clinic setting that would be helpful in educating their patients about CKD.
Providers were encouraged to participate freely in discussions, responding either to questions posed by the moderator or to questions or ideas posed by other focus group participants. As planned prior to beginning the study, data collection was continued until thematic saturation (i.e. no new themes identified among the group members) was achieved.
Analysis
The focus group discussions were audio-taped and transcribed verbatim. The grounded theory approach was used for content analysis.(Strauss and Corbin, 1990, Glaser and Strauss, 1967) Using the constant comparative method, transcripts were independently reviewed by two study investigators to develop a coding scheme representing the relevant concepts addressed during the discussions. These concepts were further refined and categorised to develop a list of key themes regarding perceptions of barriers and attitudes towards educating patients about CKD. The two investigators arrived at a consensus on a final list of themes, and differences in interpretation of emergent themes were adjudicated by a third investigator. ATLAS.ti version 5.0. (ATLAS.ti GmbH, Berlin, Germany) was used for data management.
Results
Participant Characteristics
Of the 22 primary care providers who responded during recruitment, all were eligible to participate in the study. Four providers were unable to attend a focus group due to a scheduling conflict. Eighteen primary care providers participated in the 3 focus group sessions (consisting of 7, 6, and 5 participants each). Most primary care providers (15 physicians and 3 nurse practitioners) were female, practiced in non-academic settings, and had greater than 10 years practice experience. (Table 1)
Table 1.
Participant Characteristics
| Characteristics | N=18 |
|---|---|
| Age, mean year (SD) | 48 (9) |
| Female, n (%) | 11 (61) |
| Race, n (%) | |
| African American | 2 (11) |
| White | 6 (33) |
| Asian | 10 (56) |
| Specialty, n (%) | |
| Internal Medicine | 15 (83) |
| Family Medicine | 3 (17) |
| Provider Type, n (%) | |
| Physician | 15 (83) |
| Nurse Practitioner | 3 (17) |
| Practice Type, n (%)* | |
| Community Practice | 18 (100) |
| Academic | 1 (8) |
| Years in Practice, mean (SD) | 16 (13) |
Category not mutually exclusive
Perceived Barriers to Patient Education about CKD
Primary care providers identified several barriers to the provision of education about CKD to patients, encompassed by six main themes.
1. Patients’ low awareness of CKD and poor recognition of CKD as a medical problem
Some providers believed that while most patients are aware of CKD risk factors, they are less aware of CKD itself, making it difficult for providers to educate patients regarding the importance of CKD to their health. Due to patients’ lack of awareness of CKD, a number of providers commented that patients often come to their primary care visits with questions and concerns that frequently do not include CKD. This makes it more difficult to add a discussion about CKD during visits. A provider commented,
“I think the biggest barrier is that he’s not going to come and talk to you about it…it’s not on his agenda….”
Also, since patients were not directly being treated or receiving a medication for CKD, some providers believed that patients were not likely to recognise or list CKD as a medical problem. Some providers suggested improved public education about CKD could help address the problem of low patient awareness.
2. Primary care providers’ views of CKD as not a distinct medical problem
A number of providers viewed CKD as a medical problem so closely linked to diabetes or hypertension that they did not distinguish it as a separate chronic disease requiring additional management, and they were therefore less likely to discuss CKD with patients. Some providers also recognised that the way they present CKD to patients may be less effective in helping the patient recognize CKD as a distinct medical problem. A provider stated
“They have diabetic nephropathy; they have hypertensive nephropathy. So I’ve been trained that way. I think we all have. …And there’s a tendency to speak about and focus on practical problems that we can direct therapy to and measure changes rapidly, like measuring your blood pressure, measuring your sugar, and getting patients to do that themselves.”
In addition, some providers noted that CKD often does not make it onto the problem list and is therefore, less likely to be addressed during the visit.
3. Primary care providers’ own lack of adequate knowledge or skills to educate patients about CKD
A number of primary care providers acknowledged that they lacked adequate knowledge and/or necessary skills to educate their patients about CKD. Providers listed a range of areas in which they felt their knowledge and skills could improve, including their understanding of CKD treatment, their abilities to educate patients with low education or reading levels, their abilities to motivate patients to alter their chronic disease management behaviors, and their knowledge of the appropriate timing of educating patients about CKD. With regard to their own knowledge of CKD, a few providers’ felt they had limited knowledge of CKD. Some primary care providers seeing patients with low education and reading levels felt ill-equipped to teach patients at an appropriate literacy level, particularly more complex concepts regarding kidney function or making dietary adjustments. One provider noted:
“I think the kidney is very complex…and I think patients have a hard time grasping kidney disease because they don’t feel it at all, they just don’t…. When you start talking pathophys to patients who are mostly, in my patient population, working class, blue collar, a lot of them have not finished high school, you just need to keep things very simple and I don’t think the kidney is simple.”
However, even when providers felt confident in their ability to educate patients, they felt unskilled in motivating their patients toward important behavior changes.
Many providers were also uncertain about the appropriate timing for CKD education. Although providers reported they more frequently diagnosed CKD given the increased laboratory reporting of estimated glomerular filtration rate (GFR), they reported feeling unsure about burdening patients with an additional diagnosis unless it was absolutely necessary. Providers felt this was particularly true when patients were at low risk of CKD progression. However, a number of providers were concerned about potentially waiting “too late” to tell their patients about their CKD status.
To help address their own perceived lack of skills, some primary care providers suggested that patient education about CKD might be best delivered when patients are initially seen by nephrologists, who they believed might be more effective CKD educators. While most providers did not report deferring CKD education to the nephrologist, many agreed that sending patients to a nephrologist may have a greater effect on improving patients’ recognition of CKD as a problem and motivate patients to modify their behaviors.
4. Fear of emotionally overwhelming patients
Many providers described themselves as feeling hesitant to overwhelm their patients with an additional diagnosis of CKD. Providers reported they often defer discussing CKD with their patients in order to avoid eliciting patients’ fears about the potential consequences of CKD. One provider stated,
“…it’s [kidney disease] a bit like saying insulin to a diabetic. It’s like, oh my god, my uncle was on insulin, and then he died. Insulin… his leg got chopped off.”
5. Patient visit time constraints and lack of reimbursement for CKD patient education
The most commonly reported barrier was time constraints of a routine clinic visit as a barrier to education. With limited time available to address many clinical issues, providers often reported CKD education as a lower priority among a long list of other clinical issues to address during visits. Providers attributed the current reimbursement system, which does not facilitate spending more time educating patients about CKD, as a major contributor to time constraints.
One provider commented
“I look at [the patient] and I see three different numbers that don’t look right, I’ve got to fix those numbers. And where am I going to start fitting in CKD, because I’ve got to give him three med changes probably to get his numbers to look right, and I’ve got to talk about those med changes, do I have enough room to talk about something else?”
6. Lack of educational resources
Many providers were not aware of good educational resources to assist them with educating patients about CKD (i.e. print materials or website). In addition, they noted a lack of health educators dedicated to discussing kidney disease with patients. A provider stated
“There’s no kidney educator to send them to.”
Providers identified several strategies they believed would help facilitate more discussions about CKD in primary care, including the availability of health educators to assist with CKD education, the availability of high-quality educational materials presented in different formats (i.e. written materials, DVDs, websites, and educational aids to assist providers), using group educational visits, and updating electronic medical record systems to identify patients with CKD.
Discussion
In this qualitative study primary care providers identified six major barriers to effectively educating their patients about CKD at the patient, provider and health care system levels. Some barriers (e.g., visit time constraints) have been identified previously as barriers to patient education about other chronic diseases (Yarnall et al., 2003, Elliott et al., 2011) and may reflect global issues regarding the delivery of all types of chronic disease education during primary care visits. However, other barriers (e.g., providers’ lack of identification of CKD as a distinct medical condition warranting tailored education) may be unique to CKD and may contribute to the lower occurrence of education about CKD in primary care relative to other topics.(Greer et al., 2011)
This study examines US primary care providers’ detailed views regarding the barriers they face in trying to educate their patients about CKD. Prior research on patient education about CKD has focused primarily on nephrology clinic-based strategies(Devins et al., 2000, Devins et al., 2003, Pagels et al., 2008, Manns et al., 2005, Khosla et al., 2010), with limited studies focused on the delivery of education about CKD in primary care settings (Crinson et al., 2010) Findings from this study emphasise the challenge of providing comprehensive CKD care in primary care settings and provide valuable insight for potential strategies to enhance the delivery of education about CKD in primary care.
Greater need for recognition of CKD as a distinct medical problem by primary care providers
Perhaps the most unique barrier our primary care providers reported was their own difficulty with distinguishing the value of educating patients about CKD when they were already providing related education on risk factors for CKD such as diabetes and hypertension. This finding is supported by a prior study describing primary care providers’ challenge with recognizing CKD as a discrete diagnosis. (Crinson et al., 2010). While discussion of CKD within the context of these common risk factors for CKD progression is appropriate, primary care physicians’ failure to think about and address CKD as a distinct clinical entity may contribute to their neglect of very important aspects of clinical care that could significantly impact patients’ clinical outcomes (i.e. CKD-tailored blood pressure treatment goals or counseling patients to avoid potentially nephrotoxic over-the-counter non-steroidal anti-inflammatory drugs)(National Kidney Foundation, 2002, Shahinian and Saran, 2010, Levey et al., 2009, Fink et al., 2009, Chobanian et al., 2003). Efforts are needed to further raise primary care providers’ awareness regarding these unique considerations with regard to CKD care.
Greater infrastructural and collaborative support for CKD education in primary care practices
Primary care providers’ reported lack of self-efficacy with educating patients about CKD and lack of resources or payment structures which promote patient education about CKD in primary care. These findings suggest training of primary care providers in CKD care and infrastructure to facilitate CKD care and patient education in US primary care settings is lacking. While more integrated models for CKD care (incorporating dieticians, health educators, and social workers) have been proposed both within and outside the US (Chen et al., 2006, Rastogi et al., 2008, Beaulieu and Levin, 2009), a majority of US-based multidisciplinary CKD education programmes have been based primarily within nephrology clinics (Khosla et al., 2010, Spry, 2008, Dixon et al., 2011).
The United Kingdom has successfully implemented primary care-based CKD disease management programmes, in which all patients with advanced CKD are identified and referred to multidisciplinary CKD care teams focused on enhancing CKD care and education (Stevens and O’Donoghue, 2009, Richards et al., 2008). Implementation of similar programs in the US or implementation of practice models such as the patient-centered medical home, which incorporate collaborative care to meet the complex care and educational needs of patients with chronic illness (such as CKD), could address concerns raised by primary care providers in this study. Additionally, increased dissemination of new and existing educational tools (such as those made available by the National Kidney Disease Education Program)(Narva and Briggs, 2009) to facilitate education of patients with CKD in primary care settings could also help address these needs. Enhanced early education of primary care trainees regarding key aspects of CKD may also be needed.
Limitations
The limitations of this study deserve mention. First, qualitative findings from the small convenience sample of community-based primary care providers we studied may not be generalisable to primary care providers in other geographic areas or practice settings. However, many of our findings were consistent with findings from other studies demonstrating inadequate knowledge regarding CKD among primary care providers.(Agrawal et al., 2008, Boulware et al., 2006, Charles et al., 2009, Israni et al., 2009, Lenz and Fornoni, 2006, Johnson et al., 2006, Fox et al., 2006) Second, we provided participants with a hypothetical patient scenario to spur focus group discussion. It is possible the content of discussions could have differed if alternative hypothetical scenarios had been presented. Third, the qualitative nature of our study did not allow us to quantify which attitudes were most prevalent among primary care providers and may therefore pose the most formidable barriers to CKD education. Quantitative population-based studies estimating the rates of perceived barriers to CKD education that we identified in this study could yield valuable information regarding the most powerful interventions that could be implemented to improve CKD education in primary care.
Conclusion
Primary care providers identified patient, provider and system level barriers to providing their patients with education about CKD. Efforts to improve primary care providers’ recognition of the unique aspects of CKD care could enhance CKD education in primary care. Better infrastructural support for education, including the greater use of multidisciplinary team-based approaches to CKD education within primary care settings and improved primary care provider training in CKD education may also be needed to better support patients’ educational needs regarding CKD, and to ultimately improve patients’ clinical outcomes.
Acknowledgments
Funding Statement: National Kidney Foundation of Maryland, Research Supplement to Promote Diversity in Health-Related Research (Grant# R01DK079682) from the National Institute of Diabetes and Digestive and Kidney Diseases and the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and the NIH Roadmap for Medical Research (5KL2RR025006) (Dr. Greer); Harold Amos Medical Faculty Development Award of the Robert Wood Johnson Foundation (Dr. Crews); and Grant#K23DK070757 from the National Center for Minority Health and Health Disparities and the National Institute of Diabetes and Digestive and Kidney Diseases (Dr. Boulware).
We thank Nisa Maruthur for her assistance with moderating the focus groups
Footnotes
Contributors/authors: All listed authors have made an important contribution and met each of the three authorship requirements as stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals, including 1) conception and design of the study (RG and LEB) and data collection (RG), analysis and interpretation (RG, DC, and LEB); 2) drafting and revision of the manuscript (RG, DC, LEB); and read and approved the submission of the manuscript (RG, DC, LEB).
Conflicting and Competing Interests: None declared.
References
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–266. [PubMed] [Google Scholar]
- Agrawal V, Ghosh AK, Barnes MA, et al. Awareness and knowledge of clinical practice guidelines for CKD among internal medicine residents: a national online survey. Am J Kidney Dis. 2008;52:1061–9. doi: 10.1053/j.ajkd.2008.06.022. [DOI] [PubMed] [Google Scholar]
- Allen AS, Forman JP, Orav EJ, et al. Primary Care Management of Chronic Kidney Disease. J Gen Intern Med. 2011;26:386–92. doi: 10.1007/s11606-010-1523-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaulieu M, Levin A. Analysis of multidisciplinary care models and interface with primary care in management of chronic kidney disease. Semin Nephrol. 2009;29:467–74. doi: 10.1016/j.semnephrol.2009.06.003. [DOI] [PubMed] [Google Scholar]
- Boulware LE, Troll MU, Jaar BG, et al. Identification and referral of patients with progressive CKD: a national study. Am J Kidney Dis. 2006;48:192–204. doi: 10.1053/j.ajkd.2006.04.073. [DOI] [PubMed] [Google Scholar]
- Charles RF, Powe NR, Jaar BG, et al. Clinical testing patterns and cost implications of variation in the evaluation of CKD among US physicians. Am J Kidney Dis. 2009;54:227–37. doi: 10.1053/j.ajkd.2008.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen RA, Scott S, Mattern WD, et al. The case for disease management in chronic kidney disease. Dis Manag. 2006;9:86–92. doi: 10.1089/dis.2006.9.86. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- Colleges, A. O. a. M. [Accessed November 5 2010];2008 Physician Specialty Data: Center for workforce studies. 2008 [Online]. Available: https://www.aamc.org/linkableblob/47352-5/data/specialtydata-data.pdf.
- Coresh J, Byrd-Holt D, Astor BC, et al. Chronic kidney disease awareness, prevalence, and trends among U.S. adults, 1999 to 2000. J Am Soc Nephrol. 2005;16:180–8. doi: 10.1681/ASN.2004070539. [DOI] [PubMed] [Google Scholar]
- Crinson I, Gallagher H, Thomas N, et al. How ready is general practice to improve quality in chronic kidney disease? A diagnostic analysis. Br J Gen Pract. 2010;60:403–9. doi: 10.3399/bjgp10X502100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devins GM, Hollomby DJ, Barre PE, et al. Long-term knowledge retention following predialysis psychoeducational intervention. Nephron. 2000;86:129–34. doi: 10.1159/000045730. [DOI] [PubMed] [Google Scholar]
- Devins GM, Mendelssohn DC, Barre PE, et al. Predialysis psychoeducational intervention and coping styles influence time to dialysis in chronic kidney disease. Am J Kidney Dis. 2003;42:693–703. doi: 10.1016/s0272-6386(03)00835-7. [DOI] [PubMed] [Google Scholar]
- Dixon J, Borden P, Kaneko TM, et al. Multidisciplinary CKD care enhances outcomes at dialysis initiation. Nephrol Nurs J. 2011;38:165–71. [PubMed] [Google Scholar]
- Elliott DJ, Robinson EJ, Sanford M, et al. Systemic barriers to diabetes management in primary care: a qualitative analysis of Delaware physicians. Am J Med Qual. 2011;26:284–90. doi: 10.1177/1062860610383332. [DOI] [PubMed] [Google Scholar]
- Fink JC, Brown J, Hsu VD, et al. CKD as an underrecognized threat to patient safety. Am J Kidney Dis. 2009;53:681–8. doi: 10.1053/j.ajkd.2008.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox CH, Brooks A, Zayas LE, et al. Primary care physicians’ knowledge and practice patterns in the treatment of chronic kidney disease: an Upstate New York Practice-based Research Network (UNYNET) study. J Am Board Fam Med. 2006;19:54–61. doi: 10.3122/jabfm.19.1.54. [DOI] [PubMed] [Google Scholar]
- Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago: Aldine; 1967. [Google Scholar]
- Greer RC, Cooper LA, Crews DC, et al. Quality of patient-physician discussions about CKD in primary care: a cross-sectional study. Am J Kidney Dis. 2011;57:583–91. doi: 10.1053/j.ajkd.2010.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israni RK, Shea JA, Joffe MM, et al. Physician characteristics and knowledge of CKD management. Am J Kidney Dis. 2009;54:238–47. doi: 10.1053/j.ajkd.2009.01.258. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Tierney EF, Onyemere KU, et al. Who is tested for diabetic kidney disease and who initiates treatment? The Translating Research Into Action For Diabetes (TRIAD) Study. Diabetes Care. 2006;29:1733–8. doi: 10.2337/dc06-0260. [DOI] [PubMed] [Google Scholar]
- Khosla N, Gordon E, Nishi L, et al. Impact of a chronic kidney disease clinic on preemptive kidney transplantation and transplant wait times. Prog Transplant. 2010;20:216–20. doi: 10.1177/152692481002000304. [DOI] [PubMed] [Google Scholar]
- Lea JP, Mcclellan WM, Melcher C, et al. CKD risk factors reported by primary care physicians: do guidelines make a difference? Am J Kidney Dis. 2006;47:72–7. doi: 10.1053/j.ajkd.2005.09.027. [DOI] [PubMed] [Google Scholar]
- Lenz O, Fornoni A. Chronic kidney disease care delivered by US family medicine and internal medicine trainees: results from an online survey. BMC Med. 2006;4:30. doi: 10.1186/1741-7015-4-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levey AS, Stevens LA, Coresh J. Conceptual model of CKD: applications and implications. Am J Kidney Dis. 2009;53:S4–16. doi: 10.1053/j.ajkd.2008.07.048. [DOI] [PubMed] [Google Scholar]
- Manns BJ, Taub K, Vanderstraeten C, et al. The impact of education on chronic kidney disease patients’ plans to initiate dialysis with self-care dialysis: a randomized trial. Kidney Int. 2005;68:1777–83. doi: 10.1111/j.1523-1755.2005.00594.x. [DOI] [PubMed] [Google Scholar]
- Narva AS, Briggs M. The National Kidney Disease Education Program: improving understanding, detection, and management of CKD. Am J Kidney Dis. 2009;53:S115–20. doi: 10.1053/j.ajkd.2008.05.038. [DOI] [PubMed] [Google Scholar]
- Nickolas TL, Frisch GD, Opotowsky AR, et al. Awareness of kidney disease in the US population: findings from the National Health and Nutrition Examination Survey (NHANES) 1999 to 2000. Am J Kidney Dis. 2004;44:185–97. doi: 10.1053/j.ajkd.2004.04.023. [DOI] [PubMed] [Google Scholar]
- Pagels AA, Wang M, Wengstrom Y. The impact of a nurse-led clinic on self-care ability, disease-specific knowledge, and home dialysis modality. Nephrol Nurs J. 2008;35:242–8. [PubMed] [Google Scholar]
- Plantinga LC, Boulware LE, Coresh J, et al. Patient awareness of chronic kidney disease: trends and predictors. Arch Intern Med. 2008;168:2268–75. doi: 10.1001/archinte.168.20.2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plantinga LC, Tuot DS, Powe NR. Awareness of chronic kidney disease among patients and providers. Adv Chronic Kidney Dis. 2010;17:225–36. doi: 10.1053/j.ackd.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastogi A, Linden A, Nissenson AR. Disease management in chronic kidney disease. Adv Chronic Kidney Dis. 2008;15:19–28. doi: 10.1053/j.ackd.2007.10.011. [DOI] [PubMed] [Google Scholar]
- Richards N, Harris K, Whitfield M, et al. Primary care-based disease management of chronic kidney disease (CKD), based on estimated glomerular filtration rate (eGFR) reporting, improves patient outcomes. Nephrol Dial Transplant. 2008;23:549–55. doi: 10.1093/ndt/gfm857. [DOI] [PubMed] [Google Scholar]
- Shahinian VB, Saran R. The role of primary care in the management of the chronic kidney disease population. Adv Chronic Kidney Dis. 2010;17:246–53. doi: 10.1053/j.ackd.2010.02.003. [DOI] [PubMed] [Google Scholar]
- Spry L. Building the chronic kidney disease management team. Adv Chronic Kidney Dis. 2008;15:29–36. doi: 10.1053/j.ackd.2007.10.006. [DOI] [PubMed] [Google Scholar]
- Stevens PE, O’donoghue DJ. The UK model for system redesign and chronic kidney disease services. Semin Nephrol. 2009;29:475–82. doi: 10.1016/j.semnephrol.2009.06.004. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park, CA: Sage Publications; 1990. [Google Scholar]
- Tuot DS, Powe NR. Chronic kidney disease in primary care: an opportunity for generalists. J Gen Intern Med. 2011;26:356–8. doi: 10.1007/s11606-011-1650-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usrds. US Renal Data System. USRDS 2011 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. The National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease; Bethesda, MD: 2011. [Google Scholar]
- Waterman AD, Browne T, Waterman BM, et al. Attitudes and behaviors of African Americans regarding early detection of kidney disease. Am J Kidney Dis. 2008;51:554–62. doi: 10.1053/j.ajkd.2007.12.020. [DOI] [PubMed] [Google Scholar]
- Yarnall KS, Pollak KI, Ostbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635–41. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]