Abstract
Purpose
We determined the efficacy, biological activity, pharmacokinetics and safety of the hypomethylating agent 5-azacitidine (Celgene Corp., Summit, New Jersey) in dogs with naturally occurring invasive urothelial carcinoma.
Materials and Methods
We performed a preclinical phase I trial in dogs with naturally occurring invasive urothelial carcinoma to examine once daily subcutaneous administration of 5-azacitidine in 28-day cycles at doses of 0.10 to 0.30 mg/kg per day according to 2 dose schedules, including days 1 to 5 (28-day cohort) or days 1 to 5 and 15 to 19 (14-day cohort). Clinical efficacy was assessed by serial cystosonography, radiography and cystoscopy. Urinary 5-azacitidine pharmacokinetic analysis was also done. Pretreatment and posttreatment peripheral blood mononuclear cell and invasive urothelial carcinoma DNA, respectively, was analyzed for global and gene specific [CDKN2A (p14ARF)] methylation changes.
Results
Enrolled in the study were 19 dogs with naturally occurring invasive urothelial carcinoma. In the 28-day cohort the maximum tolerated dose was 0.20 mg/kg per day with higher doses resulting in grade 3 or 4 neutropenia in 4 of 6 dogs. In the 14-day cohort the maximum tolerated dose was 0.10 mg/kg per day with grade 3 or 4 neutropenia seen in 2 of 3 dogs treated at higher doses. No grade 3 or 4 nonhematological toxicity was observed during either dosing schedule. Of 18 dogs evaluable for tumor response partial remission, stable disease and progressive disease were observed in 4 (22.2%), 9 (50.0%) and 4 (22.2%), respectively. Consistent 5-azacitidine levels (205 to 857 ng/ml) were detected in urine. Pretreatment and posttreatment methylation analysis revealed no significant correlation with clinical response.
Conclusions
Subcutaneous 5-azacitidine showed promising clinical activity in a canine invasive urothelial carcinoma model, thus meriting further development in humans with urothelial carcinoma.
Keywords: urinary bladder, urothelium, carcinoma, azacitidine, dogs
Urothelial carcinoma of the bladder and urinary tract is a common human malignancy. Tumors of these organs rank as the fifth most common site of new human cancer diagnoses with bladder UC accounting for 70,000 new diagnoses and more than 14,000 deaths in 2010.1 Despite survival advancements for other malignancies improvements in UC outcomes have been lacking. Consequently a need exists to develop new approaches that provide patients with UC with rapid access to personalized, effective therapies.
UC carcinogenesis is a multistep process involving the dysregulation of multiple oncogenes and tumor suppressor genes, including FGFR3, HRAS, CDH1, CDKN2A (p16INK4a and p14ARF), HOXB2, RASSF1A, SFRP2 and WAF1.2–6 Often these genes are transcriptionally silenced by hypermethylation of CpG rich repeat sequences (CpG islands) in their promoter regions. While CpG islands are usually unmethylated in normal cells, during tumorigenesis these promoter associated regions typically undergo increasing methylation, ultimately resulting in transcriptional silencing.2,7 Several studies of humans with UC have shown potential DNA methylation biomarkers for detection, staging and survival outcomes.2,3,8,9
Demethylation and re-expression of tumor suppressor genes using DNA methyltransferase inhibitors is now under extensive study.10 The DNA methyltransferase inhibitor 5-azaC is a nonmethylatable cytidine analogue that is incorporated into DNA during S-phase (Vidaza package insert 2007). At high doses 5-azaC shows cytotoxicity while lower doses elicit DNA hypomethylation, silenced tumor suppressor re-expression and cellular differentiation. 11 Due to its significant renal excretion and subcutaneous administration 5-azaC represents a rational, patient friendly opportunity for UC therapeutic development.
Naturally occurring iUC in pet dogs is an ideal platform in which to study the preclinical efficacy and safety of potential human UC therapeutic agents. Canine iUC is similar to human invasive UC in its histopathology, aneuploidy, disease progression, prognostic factors and response to platinum based chemotherapy.12 Also, the molecular pathogenesis of canine iUC emulates that of human UC with over expression of bFGF, COX1 (PTGS1), COX2 (PTGS2) and mutated TP53.12
Based on this strong rationale we performed a preclinical phase I study in dogs with iUC to test the experimental hypothesis that subcutaneous 5-azaC has clinical activity sufficient for further development in human UC trials.
MATERIALS AND METHODS
Study Subjects
The dog trial was performed at the Purdue University Veterinary Teaching Hospital and approved by the Purdue University animal care and use committee. Consent for study participation was obtained from all dog owners. All dogs were required to have life expectancy greater than 2 months and histologically documented measurable iUC. Invasive UC was defined as T stage T2 or greater, any N or any M stage according to WHO TNM canine staging criteria, in which canine T2 lesions are equivalent to T3 lesions using human bladder cancer criteria.13 Prior therapies were allowed without limit.
Treatment
Dogs received subcutaneous 5-azaC once daily for 5 consecutive days according to 2 dose schedule cohorts, including 28d—5-azaC administered on days 1 to 5 and 14d—5- azaC administered on days 1 to 5 and 15 to 19. Cycles were repeated every 28 days. Treatment was initiated in the 28d cohort starting at a 5-azaC dose of 0.2 mg/kg per day subcutaneously administered on days 1 to 5 based on 10% of the Food and Drug Administration approved human 5-azaC dose for myelodysplastic syndrome (Vidaza package insert 2007).14
DLT was defined as any grade 3 or 4 adverse event, as assessed by Veterinary Cooperative Oncology Group Common Toxicity Criteria, that was noted within the first 2 therapy cycles.15 In the absence of DLT the 5-azaC dose was increased for each subsequent dog in the 28d cohort until toxicity was observed. When DLT was observed, the cohort was expanded from 1 to a maximum of 6 dogs to determine MTD, defined as the dose at which a DLT occurred in no more than 1 of 6 dogs enrolled in a specific dose cohort. Enrollment in the 14d cohorts began at the 28d cohort MTD and was decreased for each subsequent dog according to observed DLTs until the MTD in the 14d cohort was established. No maximum number of treatment cycles was stipulated for dogs in remission or with stable disease.
Dog and Disease Evaluations
Tumors were staged before treatment and monthly during treatment by cystosonography, full abdominal ultrasound, and thoracic and abdominal radiography. Cystosonography was used to map and measure bladder lesions similarly to that described by Chun et al.16 Ultrasound was done by the same operator on each dog at each visit and the bladder was distended to a similar degree for each examination. Briefly, the dogs were placed in right lateral recumbency and the area of the bladder lesions was recorded in the sagittal plane. The dorsal-ventral dimension of each lesion from the transverse plane was multiplied by the area from the sagittal plane to determine estimated tumor volume. CR was defined as complete resolution of all clinical and pathological evidence of iUC, PR was defined as a 50% or greater reduction in tumor volume, SD was defined as less than a 50% increase or reduction in tumor volume for at least 8 weeks and progressive disease was defined as a 50% or greater increase in tumor volume or the development of new lesions.17
PBMCs and bladder tumor biopsy specimens were collected before and after treatment for methylation analysis at baseline in the 2 cohorts as well as on cycle 2, day 5 of the 28d cohort and on cycle 2, day 19 of the 14d cohort dosing schedules. Complete blood count and a comprehensive serum biochemistry profile were performed at baseline and on day 1 of each cycle.
Pharmacokinetic Evaluations
All dogs that received at least 1 day of 5-azaC therapy were eligible for inclusion in urinary pharmacokinetic analysis. Midstream, free catch urine samples were obtained after cycle 1, day 1. Samples were collected between 2 time points, including 0 to 6 hours after 5-azaC treatment and 6 to 24 hours after 5-azaC treatment. Using gemcitabine as the internal standard 5-azaC was extracted by solid phase extraction using an MCX device (Waters®). The eluant was evaporated, reconstituted with mobile phase and injected into an API 4000HPLC-MS/MS (Applied Biosystems™). Polar and nonpolar constituents were separated using a C8 250 × 4.6 mm analytical Zorbax® high performance liquid chromatography column and a gradient mobile phase (acetonitrile containing 5 mM ammonium acetate). Quadropole 1/3 mass spectrometry settings for 5-azaC and gemcitabine were 245/113 and 264/112, respectively. The lower limit of accurate quantification for 1 ml urine was 1.0 ng/ml.
DNA Methylation Assessments
For all dogs that completed 2 cycles of 5-azaC therapy and had sufficient pretreatment and posttreatment bladder biopsy tissue, and/or PBMC samples available the samples were analyzed for CDKN2A (p14ARF) gene specific and global methylation changes. DNA was extracted from 200 µl buffy coat or cystoscopy tumor samples using a QIAamp® DNA Blood Mini Kit according to manufacturer instructions. Sodium bisulfite conversion of genomic DNA and cleanup were done with an EZ DNA Methylation™ kit according to manufacturer instructions. After bisulfite conversion of unmethylated cytosine deamination to uracil CDKN2A (p14ARF) methylation status was assessed by MSP using the methylated and unmethylated MSP primers CDKN2A (p14ARF) unmethylated (F) 5′-GTTTTTTGTTTAGTTGGAGTTATGT-3′, (R) 5′-ATAATAAATAAACTTTCCCAAACTCACT-3′, CDKN2A (p14ARF) methylated (F) 5′-GGTTTTTCGTTTAGTCGGAGGTTAC-3′and (R) 5′-GTAATAAATAAACTTTCCCGAACTCG-3′. Primers were designed using the Web based tool MSPPrimer (Division of Tumor Biology, Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University, Baltimore, Maryland, http://www.mspprimer.org/cgi-mspprimer/design.cgi).18
Changes in global methylation were assessed by LUMA, as previously described.19 The assay was done in duplicate.
Statistical Considerations
The number of dogs to be enrolled in the study depended on the observed safety profile of each dose cohort. Using a 6-dog cohort the probability of failing to observe DLT toxicity at least 40% of the time was less than 5%. Descriptive statistics were used to summarize the dog characteristics of treatment efficacy, safety and pharmacokinetics. Associations of urinary 5-azaC with dose schedules and response outcomes were analyzed by Student’s t test. Pretreatment and posttreatment LUMA methylation changes were analyzed by the paired t test. Associations between the frequency of methylation reduction and 5-azaC dose schedules were assessed by Fisher’s exact test.
RESULTS
Subjects
From April 7, 2008 through September 9, 2009 we enrolled 11 dogs in the 28d cohort and 8 in the 14d cohort. All dogs were included in toxicity analysis and 18 were evaluable for tumor response. One dog concurrently received firocoxib during 5-azaC administration and, thus, was not evaluable for tumor response. Various dog breeds were represented with Scottish Terriers and mixed as the most common breeds (4 dogs each). Median age was 11.0 years (range 8.0 to 14.1) and median weight was 19.2 kg (range 7.0 to 51.0). Distant metastasis was detected in 16% of dogs. Of the dogs 73% had received prior cyclooxygenase inhibitor treatment. Table 1 lists demographic features.
Table 1.
Subject characteristics
| No. Dogs (%) | |
|---|---|
| Breed: | |
| Mixed | 4 (21) |
| Scottish Terrier | 4 (21) |
| Shetland Sheepdog | 3 (16) |
| Golden Retriever | 2 (11) |
| Other | 6 (32) |
| Gender: | |
| Spayed F | 11 (58) |
| Neutered M | 8 (42) |
| WHO stage:13 | |
| T2N0M0 | 15 (79) |
| T3N0M0 | 1 (5) |
| T2N0M1* | 1 (5) |
| T3N0M1* | 1 (5) |
| T3N1M1* | 1 (5) |
| No. prior therapies: | |
| 0 | 5 (26) |
| 1 | 13 (68) |
| 2 | 1 (5) |
Lung metastasis in 3 dogs and bone metastasis in 1.
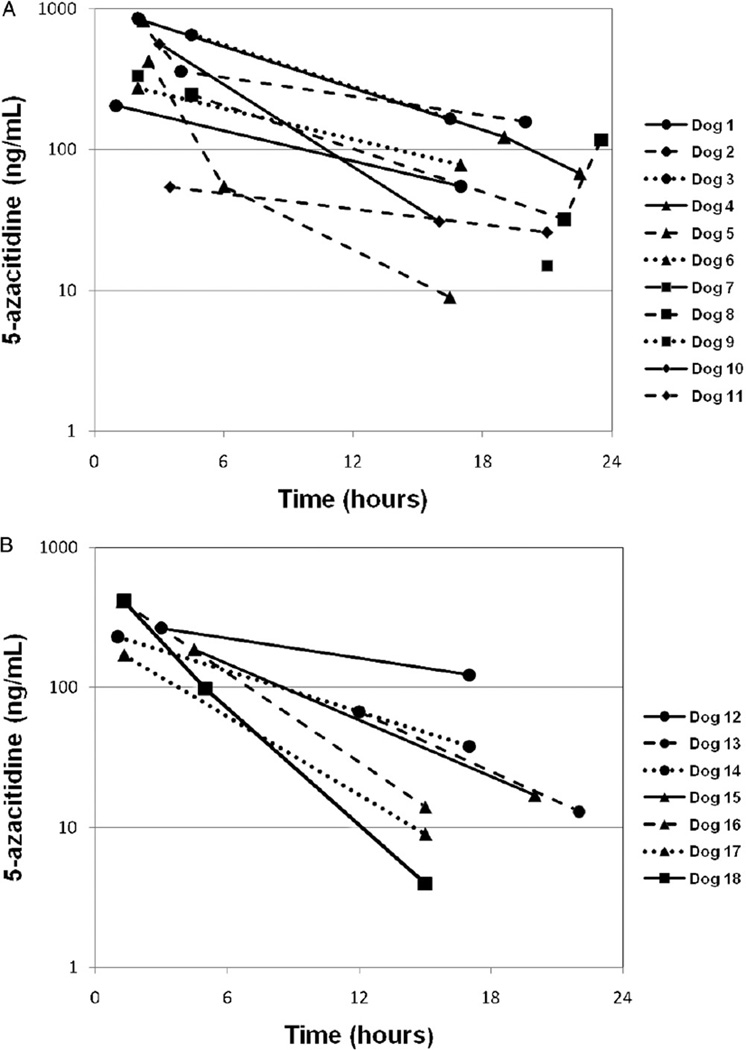
Pharmacokinetic Analysis
Cycle 1, day 1 posttreatment urine samples from 11 and 7 dogs in the 28d and 14d cohorts, respectively, were available for quantitative 5-azaC pharmacokinetic analysis. Detectable 5-azaC was observed within the first 6 hours after treatment in 10 of 11 dogs in the 28d cohort and in 6 of 7 in the 14d cohort (fig. 1). In the 28d and 14d cohorts the mean ± standard deviation observed 5-azaC urine concentration within the first 6 hours after treatment was 401 ± 245 and 254 ± 85 ng/ml, respectively (p = 0.01). Similarly the mean 12 to 24-hour 5-azaC urine concentration in the 28d and 14d cohorts was 71 ± 56 and 31 ± 42 ng/ml, respectively.
Figure 1.
Urinary 5-azaC pharmacokinetics. First data point per dog was obtained after first dose. A, 28d cohort. B, 14d cohort.
Toxicity
The 5-azaC treatment was generally well tolerated with myelosuppression and gastrointestinal side effects as the most common clinically relevant toxicities. One episode of grade 1 hand-foot syndrome was observed. Grade 3 or 4 neutropenia developed in 4 dogs (21.1%, 95% CI 6.1– 45.6) in the 28d cohort at a dose of 0.2 to 0.3 mg/kg per day but in none in the 14d cohort. Grade 3 or 4 nausea or anorexia developed in 1 dog on 0.3 mg/kg per day in the 28d cohort and in 2 (15.8%, 95% CI 3.3–39.6) in the 14d cohort after more than 2 cycles of therapy, which did not represent DLT events at the 0.1 mg/kg per day dose. In the 28d cohort none of the 6 dogs on the 0.20 mg/kg dose showed hematological toxicity. In the 14d cohort none of the 6 dogs on the 0.10 mg/kg dose showed thrombocytopenia, neither of the 2 on the 0.15 mg/kg dose showed nausea and none of the 6 on the 0.10 mg/kg dose showed diarrhea. No treatment related deaths were observed. Tables 2 and 3 list all treatment related toxicities. MTD in the 28d and 14d cohorts was 0.20 and 0.10 mg/kg per day, respectively.
Table 2.
Dose toxicity profile of 28d 5-azaC cohort
| Grade |
|||||
|---|---|---|---|---|---|
| Dose (event) (mg/kg) | No. Dogs | 1 | 2 | 3 | 4 |
| Hematological | |||||
| 0.3: | 2 | ||||
| Neutropenia | 0 | 0 | 0 | 2* | |
| Thrombocytopenia | 0 | 1 | 0 | 0 | |
| 0.25: | 6 | ||||
| Neutropenia | 1 | 1 | 1* | 1* | |
| Thrombocytopenia | 0 | 1 | 0 | 0 | |
| Nonhematological | |||||
| 0.3: | 2 | ||||
| Diarrhea | 1 | 0 | 1* | 0 | |
| Nausea | 1 | 1 | 0 | 0 | |
| Anorexia | 1 | 0 | 0 | 0 | |
| 0.25: | 6 | ||||
| Diarrhea | 2 | 0 | 0 | 0 | |
| Nausea | 2 | 0 | 0 | 0 | |
| Anorexia | 1 | 0 | 0 | 0 | |
| 0.20: | 6 | ||||
| Diarrhea | 2 | 0 | 0 | 0 | |
| Nausea | 3 | 0 | 0 | 0 | |
During cycles 1 and 2.
Table 3.
Dose toxicity profile of 14d 5-azaC cohort
| Grade |
|||||
|---|---|---|---|---|---|
| Dose (event) (mg/kg) | No. Dogs | 1 | 2 | 3 | 4 |
| Hematological | |||||
| 0.20: | 3 | ||||
| Neutropenia | 0 | 0 | 0 | 1* | |
| Thrombocytopenia | 1 | 0 | 0 | 0 | |
| 0.15: | 2 | ||||
| Neutropenia | 0 | 1 | 0 | 0 | |
| Thrombocytopenia | 1 | 0 | 0 | 0 | |
| 0.10 (neutropenia) | 6 | 1 | 2 | 1† | 0 |
| Nonhematological | |||||
| 0.20: | 3 | ||||
| Nausea | 3 | 0 | 0 | 0 | |
| Anorexia | 1 | 0 | 0 | 0 | |
| Hand-foot | 1 | 0 | 0 | 0 | |
| syndrome | |||||
| 0.15: | 2 | ||||
| Diarrhea | 1 | 0 | 0 | 0 | |
| Anorexia | 1 | 0 | 0 | 0 | |
| 0.10: | |||||
| Nausea | 2 | 0 | 0 | 0 | |
| Anorexia | 3 | 1 | 2† | 0 | |
During cycles 1 and 2.
After cycle 2.
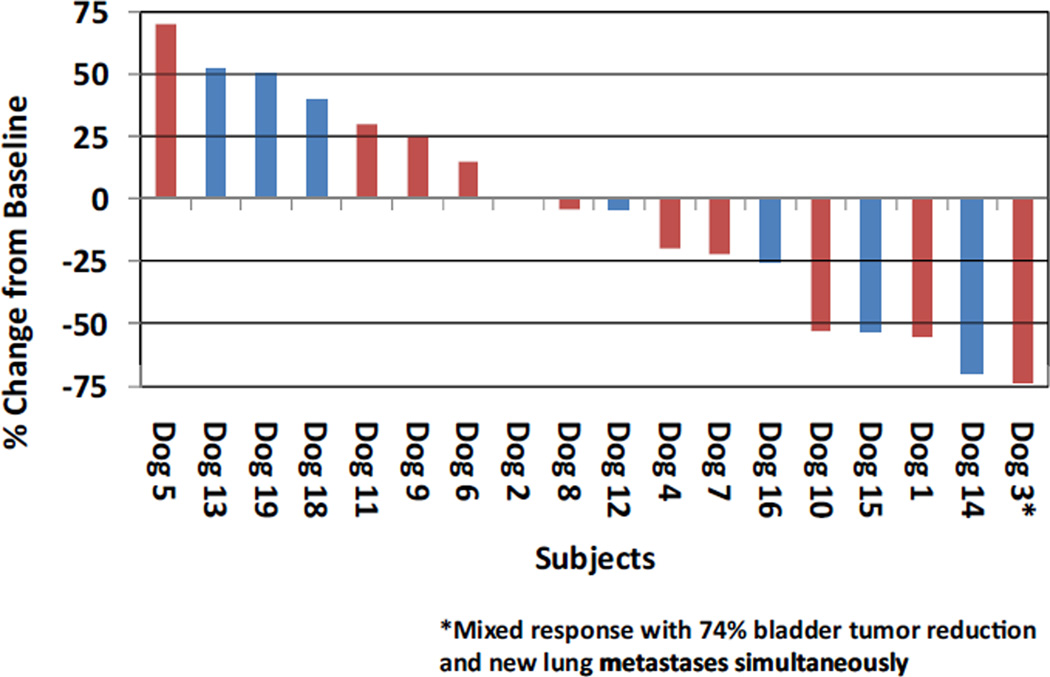
Tumor Response
Demonstrable size reductions in bladder tumors were observed in 10 of 18 dogs (55.6%, 95% CI 30.8–78.5, fig. 2). No CR was noted, PR was noted in 4 dogs (22.2%, 95% CI 6.4–47.6) and SD greater than 8 weeks in duration was noted in 9 (50.0%, 95% CI 26.0–74.0). Progressive disease developed in 4 dogs (22.2%, 95% CI 6.4–47.6). A mixed response with a 74% reduction of primary tumor and metastatic growth was observed in 1 dog. The observed disease control rate across all doses and schedules (CR plus PR plus SD) was 72.2% (95% CI 46.5–90.3). In the 28d and 14d cohorts the disease control rate was 81.8% and 57.1%, respectively (Fisher’s exact test p = 0.33). No significant association was noted between urinary 5-azaC and response.
Figure 2.
Maximum bladder tumor volume reduction. Red bars represent 28d cohort. Blue bars represent 14d cohort.
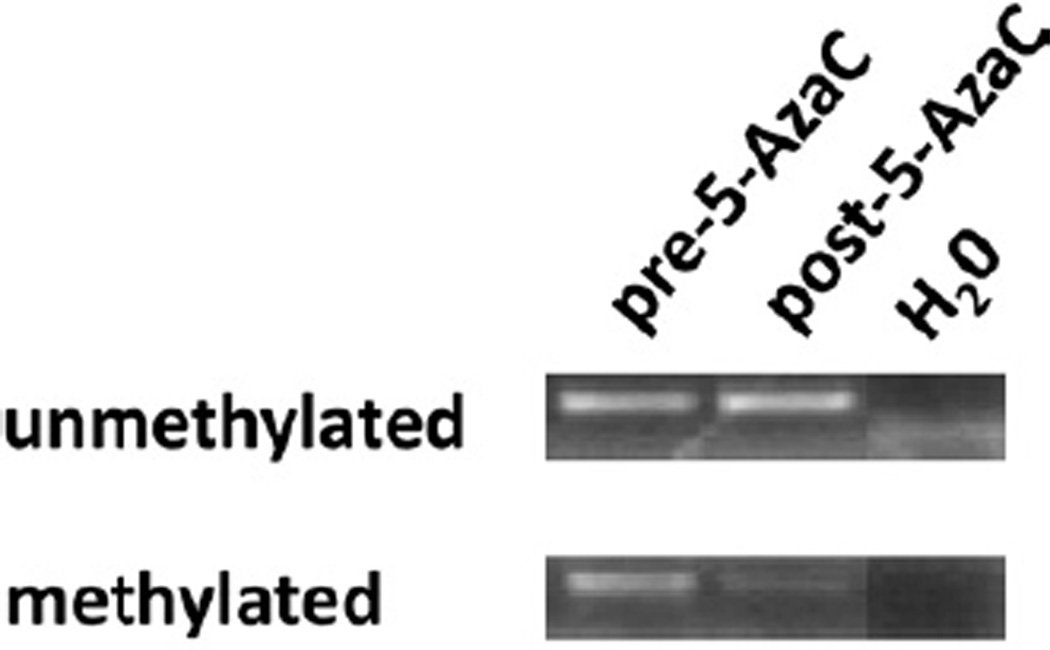
Tumor Methylation Analysis
Paired pretreatment and posttreatment PBMC samples were available from 8 and 4 dogs in the 28d and 14d cohorts, respectively. As assessed by LUMA, mean PBMC global methylation before and after 5-azaC was 72.1% and 73.6%, respectively (p = 0.47). However, 6 dogs (50%) showed a minor decrease of 0.74% to 8.43% in posttreatment PBMC global DNA methylation independent of the 5-azaC dose schedule (p = 0.54).
In addition to PBMCs, paired pretreatment and post-5-azaC treatment tumor samples were available for 6 and 4 dogs in the 28d and 14d cohorts, respectively. As assessed by LUMA, mean tumor global methylation before and after 5-azaC was 57.5% and 55.0%, respectively (p = 0.31). Seven dogs (70%) showed a minor decrease of 1.55% to 17.00% in tumor global methylation after therapy. All 4 dogs (100%) on the 14d dose schedule showed some decrease in tumor global DNA methylation after 5-azaC vs 3 of 6 (50%) on the 28d dose schedule, although the difference was not statistically significant (p = 0.20). Notably in dog 15, the single dog that achieved a confirmed partial remission with paired tumor tissue available, a 6.8% absolute decrease in CDKN2A (p14ARF) methylation was observed (fig. 3).
Figure 3.
Dog 15. CDKN2A (p14ARF) MSP results before and after 5-azaC.
DISCUSSION
In humans UC is a chemosensitive malignancy and a significant tumor reduction is seen in half of the patients with metastasis who are treated with platinum based chemotherapy regimens.20 However, despite initial responses almost all patients with metastatic UC die of the disease. While traditional human UC models permit the rapid study of cell lines with specific phenotypes (ie cisplatin resistant and/or multidrug resistant) and combination epigenetic agent regimens, no significant advances have been made in UC clinical outcomes in patients in the last 20 years.21 Thus, a critical need exists to identify new therapeutic development strategies in this understudied cancer population.
The development of novel therapeutic and biomarker strategies through translational investigations in dogs with naturally occurring iUC represents an attractive new model.22 This approach is particularly relevant for iUC, in which the canine and human diseases have similar histopathology, oncogene and tumor suppressor gene expression, patterns of invasion and metastasis, prognostic factors and response to platinum based chemotherapy.12 With this background a phase I study was performed of subcutaneous 5-azaC for naturally occurring iUC in dogs.11,12
Pharmacokinetic assessment of urinary 5-azaC using 2 drug administration schedules (28d and 14d) revealed detectable 5-azaC in 16 of the 18 dogs (89%) tested. The 5-azaC concentrations observed were within the biologically active concentrations reported for humans (Vidaza package insert 2007). In the 28d and 14d dose cohorts 24-hour pharmacokinetic profiles were characterized by a rapid peak concentration, quick clearance and a low, persistent 5-azaC concentration. These profiles are similar to the pharmacokinetics of 5-azaC in humans (Vidaza package insert 2007).23
Myelosuppression and gastrointestinal toxicity, including nausea, diarrhea and anorexia, in dogs on 5-azaC was observed at higher doses in each dose cohort. All were dose related and reversible. The toxicity profile in this canine study reflects a side effect profile similar to that in humans on 5-azaC (Vidaza package insert 2007).23
We observed promising antitumor activity in this study with a 22% partial remission rate and disease control at least 8 weeks in duration in 72% of dogs. These results compare favorably to an approximately 20% partial remission rate and 50% disease control rate in dogs with iUC that received cisplatin intravenously as a single agent in prior studies.24,25 Also, tumor reductions were seen in 56% of dogs. No significant differences were observed in the tumor response rate between the 28d and 14d dose cohorts. The antitumor activity in this trial is notable in the study population, in which 73% of dogs had received systemic therapy before 5-azaC. Thus, the current findings of 5-azaC clinical activity for canine iUC provide strong justification for its evaluation as a potential anti-UC therapy in humans.
This canine study revealed no significant change in global or CDKN2A (p14ARF) specific methylation in pretreatment and post-5-azaC PBMC or iUC samples, as assessed by LUMA and MSP. Possible explanations for the observed clinical efficacy in the absence of biological hypomethylation include insufficient duration of 5-azaC drug exposure, suboptimal timing of PBMC and urothelial carcinoma sample collection, and cross-species or crossbreed incompatibility of the LUMA and MSP platforms. A lack of correlation between hypomethylation and clinical response was also reported in several human 5-azaC studies.26,27 Lastly, while using 5-azaC as an epigenetic modifier of tumor suppressor gene function represents an attractive novel anticancer mechanistic approach, the presence of myelosuppression in the absence of consistent gene specific methylation changes may indicate clinical efficacy through a traditional cytotoxic mechanism in our canine model. To our knowledge the optimal 5-azaC dose has not been established for solid tumors in humans. However, the maximal frequency of tumor responses was observed at a 5-azaC dose of 60 to 75 mg/m2 per day, similar to the drug exposures used in our canine model and far below the maximum tolerated human 5-azaC dose.28
The findings of this canine trial support further study of naturally occurring iUC in dogs as a relevant tumor model for human UC drug development. The benefits of using the naturally occurring canine iUC model for translational therapeutic studies are substantial. Specifically the known association of specific canine breeds, ie Scottish Terrier, with an increased incidence of iUC provides a unique opportunity to define genes critical to the carcinogenesis process.29 By identifying putative candidate genes in canine breeds the confirmation and testing of prevention strategies in humans may be optimized. In contrast to human UC studies, which have been plagued by poor accrual, therapeutic studies in dogs with iUC can accrue quickly. Even partial financial assistance for canine clinical trial therapy acts as a strong accrual motivator. Lastly but perhaps of utmost relevance to the personalized medicine model, given the innumerable candidate compounds available for therapeutic development, the canine model can provide a less expensive means to test several promising agents compared to similarly designed human phase I/II studies, which typically investigate a single candidate drug.
CONCLUSIONS
The naturally occurring canine iUC model used in this preclinical phase I investigation of 5-azaC represents a novel platform for the translation and design of human UC clinical trials that is justified by the tolerability and marked clinical antitumor efficacy observed in this pilot study. After success against human hematological neoplasms azanucleosides are now being extensively investigated in solid tumor clinical trials as monotherapy and combined with other epigenetic or chemotherapeutic agents. The current 5-azaC preclinical UC results suggest optimism for treating this highly fatal malignancy.
ACKNOWLEDGMENTS
Dr. Michael House, Indiana University School of Medicine, provided discussion on MSP primer design techniques. Analysis was done at the laboratory of the Clinical Pharmacology Analytical Core, Indiana University Melvin and Bren Simon Cancer Center.
Supported by Indiana University Melvin and Bren Simon Cancer Center Translational Research Acceleration Collaboration grant funding, Celgene Corp., Summit, New Jersey and National Cancer Institute Grant P30 CA082709.
Abbreviations and Acronyms
- 14d
14-day
- 28d
28-day
- 5-azaC
5-azacitidine
- CpG
cytosine-guanine
- CR
complete remission
- DLT
dose limiting toxicity
- iUC
invasive UC
- LUMA
luminometric methylation assay
- MSP
methylation specific polymerase chain reaction
- MTD
maximum tolerated dose
- PBMC
peripheral blood mononuclear cell
- PR
partial remission
- SD
stable disease
- UC
urothelial carcinoma
Footnotes
Financial interest and/or other relationship with Celgene, Sanofi-Aventis, GlaxoSmithKline and Centocor Ortho Biotech.
REFERENCES
- 1.Jemal A, Siegel R, Xu J, et al. Cancer Statistics, 2010. CA Cancer J Clin. 2010;60:277. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Marsit CJ, Houseman EA, Christensen BC, et al. Identification of methylated genes associated with aggressive bladder cancer. PLoS One. 2010;5:e12334. doi: 10.1371/journal.pone.0012334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Serizawa RR, Ralfkiaer U, Steven K, et al. Integrated genetic and epigenetic analysis of bladder cancer reveals an additive diagnostic value of FGFR3 mutations and hypermethylation events. Int J Cancer. 2010;129:78. doi: 10.1002/ijc.25651. [DOI] [PubMed] [Google Scholar]
- 4.Mitra AP, Datar RH, Cote RJ. Molecular pathways in invasive bladder cancer: new insights into mechanisms, progression, and target identification. J Clin Oncol. 2006;24:5552. doi: 10.1200/JCO.2006.08.2073. [DOI] [PubMed] [Google Scholar]
- 5.Stein JP, Ginsberg DA, Grossfeld GD, et al. Effect of p21WAF1/CIP1 expression on tumor progression in bladder cancer. JNCI. 1998;90:1072. doi: 10.1093/jnci/90.14.1072. [DOI] [PubMed] [Google Scholar]
- 6.Wu XR. Urothelial tumorigenesis: a tale of divergent pathways. Nat Rev Cancer. 2005;5:713. doi: 10.1038/nrc1697. [DOI] [PubMed] [Google Scholar]
- 7.Esteller M. Epigenetics in cancer. N Engl J Med. 2008;358:1148. doi: 10.1056/NEJMra072067. [DOI] [PubMed] [Google Scholar]
- 8.Dulaimi E, Uzzo RG, Greenberg RE, et al. Detection of bladder cancer in urine by a tumor suppressor gene hypermethylation panel. Clin Cancer Res. 2004;10:1887. doi: 10.1158/1078-0432.ccr-03-0127. [DOI] [PubMed] [Google Scholar]
- 9.Maruyama R, Toyooka S, Toyooka KO, et al. Aberrant promoter methylation profile of bladder cancer and its relationship to clinicopathological features. Cancer Res. 2001;61:8659. [PubMed] [Google Scholar]
- 10.Jones PA, Baylin SB. The epigenomics of cancer. Cell. 2007;128:683. doi: 10.1016/j.cell.2007.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Issa JP, Kantarjian HM, Kirkpatrick P. Azacitidine. Nat Rev Drug Discov. 2005;4:275. doi: 10.1038/nrd1698. [DOI] [PubMed] [Google Scholar]
- 12.Mutsaers AJ, Widmer WR, Knapp DW. Canine transitional cell carcinoma. J Vet Intern Med. 2003;17:136. doi: 10.1892/0891-6640(2003)017<0136:ctcc>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 13.TNM Classification of Tumours in Domestic Animals. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 14.Guidance for Industry and Reviewers Estimating the Safe Starting Dose in Clinical Trials for Therapeutics in Adult Healthy Volunteers. Silver Spring: Food And Drug Administration; 2002. [Google Scholar]
- 15.Veterinary Co-operative Oncology Group-Common Terminology Criteria for Adverse Events (VCOGCTCAE) following chemotherapy or biological antineoplastic therapy in dogs and cats, v1.0. Vet Comp Oncol. 2004;2:195. doi: 10.1111/j.1476-5810.2004.0053b.x. [DOI] [PubMed] [Google Scholar]
- 16.Chun R, Knapp DW, Widmer WR, et al. Phase II clinical trial of carboplatin in canine transitional cell carcinoma of the urinary bladder. J Vet Intern Med. 1997;11:279. doi: 10.1111/j.1939-1676.1997.tb00465.x. [DOI] [PubMed] [Google Scholar]
- 17.Hume C, Seiler G, Porat-Mosenco Y, et al. Cystosonographic measurements of canine bladder tumours. Vet Comp Oncol. 2010;8:122. doi: 10.1111/j.1476-5829.2010.00212.x. [DOI] [PubMed] [Google Scholar]
- 18.Brandes JC, Carraway H, Herman JG. Optimal primer design using the novel primer design program: MSPprimer provides accurate methylation analysis of the ATM promoter. Oncogene. 2007;26:6229. doi: 10.1038/sj.onc.1210433. [DOI] [PubMed] [Google Scholar]
- 19.Karimi M, Johansson S, Stach D, et al. LUMA (LUminometric Methylation Assay)—a high throughput method to the analysis of genomic DNA methylation. Exp Cell Res. 2006;312:1989. doi: 10.1016/j.yexcr.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 20.von der Maase H, Hansen SW, Roberts JT, et al. Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol. 2000;18:3068. doi: 10.1200/JCO.2000.18.17.3068. [DOI] [PubMed] [Google Scholar]
- 21.Karam JA, Fan J, Stanfield J, et al. The use of histone deacetylase inhibitor FK228 and DNA hypomethylation agent 5-azacytidine in human bladder cancer therapy. Int J Cancer. 2007;120:1795. doi: 10.1002/ijc.22405. [DOI] [PubMed] [Google Scholar]
- 22.Khanna C, Lindblad-Toh K, Vail D, et al. The dog as a cancer model. Nat Biotechnol. 2006;24:1065. doi: 10.1038/nbt0906-1065b. [DOI] [PubMed] [Google Scholar]
- 23.Rudek MA, Zhao M, He P, et al. Pharmacokinetics of 5-azacitidine administered with phenylbutyrate in patients with refractory solid tumors or hematologic malignancies. J Clin Oncol. 2005;23:3906. doi: 10.1200/JCO.2005.07.450. [DOI] [PubMed] [Google Scholar]
- 24.Moore AS, Cardona A, Shapiro W, et al. Cisplatin (cisdiamminedichloroplatinum) for treatment of transitional cell carcinoma of the urinary bladder or urethra. A retrospective study of 15 dogs. J Vet Intern Med. 1990;4:148. doi: 10.1111/j.1939-1676.1990.tb00888.x. [DOI] [PubMed] [Google Scholar]
- 25.Knapp DW, Glickman NW, Widmer WR, et al. Cisplatin versus cisplatin combined with piroxicam in a canine model of human invasive urinary bladder cancer. Cancer Chemother Pharmacol. 2000;46:221. doi: 10.1007/s002800000147. [DOI] [PubMed] [Google Scholar]
- 26.Issa JP, Kantarjian HM. Targeting DNA methylation. Clin Cancer Res. 2009;15:3938. doi: 10.1158/1078-0432.CCR-08-2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Keating GM. Azacitidine: a review of its use in higher-risk myelodysplastic syndromes/acute myeloid leukaemia. Drugs. 2009;69:2501. doi: 10.2165/11202840-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 28.Cowan LA, Talwar S, Yang AS. Will DNA methylation inhibitors work in solid tumors? A review of the clinical experience with azacitidine and decitabine in solid tumors. (Report) Epigenomics. 2010;2:71. doi: 10.2217/epi.09.44. [DOI] [PubMed] [Google Scholar]
- 29.Shearin AL, Ostrander EA. Canine morphology: hunting for genes and tracking mutations. PLoS Biol. 2010;8:e1000310. doi: 10.1371/journal.pbio.1000310. [DOI] [PMC free article] [PubMed] [Google Scholar]