Abstract
In our recent publication, we describe the local anesthetic (LA) inhibition of the prokaryotic voltage gated sodium channel NaChBac. Despite the numerous functional and putative structural differences with the mammalian sodium channels, the data show that LA compounds effectively and reversibly inhibit NaChBac channels in a concentration range similar to resting blockade on eukaryotic Navs. In addition to current reduction, LA application accelerated channel inactivation kinetics of NaChBac which could be accounted for in a simple state-model whereby local anesthetics increase the probability of entering the inactivated state. We have further explored what state (or states) local anesthetic blockade of NaChBac could pertain to eukaryotic sodium channels, and what molecular similarities exist between these disparate channel families. Here we show that the rate of recovery from inactivation remains unaffected in the presence of local anesthetics. Further, we show that two sites that support use-dependent inhibition in eukaryotic channels, do not affect block to the same extent when mutated in NaChBac channels. The data indicate that the molecular determinants and the inherent mechanisms for LA block are likely to be divergent between bacterial and eukaryotic Navs, but future experiments will help define possible similarities.
Keywords: sodium channel pharmacology, structure-based drug design, NaChBac, local anesthetic binding sites
Introduction
Voltage-gated sodium channels are key regulators of electrical signaling in the cells of nerve and muscle excitable cells.1 These channels display sub-millisecond activation kinetics, and the resultant rapid influx of sodium ions drives the initiation of the action potential making them key players in maintaining electrical excitability and stability in the cells of cardiac and neuronal tissues. Seemingly modest alternations in Nav channel gating parameters can result in a myriad of pathological conditions including lethal cardiac arrhythmia, severe epilepsy and debilitating pain syndromes, conditions which can be effectively managed by therapeutics that inhibit sodium ion conductance.2-6
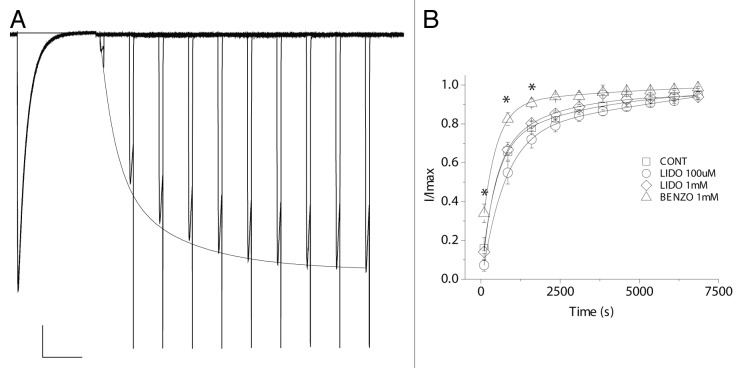
The prokaryotic family of voltage-gated sodium channels, including NaChBac from Bacillus halodurans, are homotetramers with modest sodium ion selectivity and voltage-dependent gating.7-9 Recent crystallographic breakthroughs with the bacterial Nav homologs NavAb and NavRh have begun to shed light on the details of sodium ion selectivity and to capture conformations which may represent functional gating states of the channel.10-12 The molecular determinants of NaChBac inactivation remain undescribed but could involve conformational changes in the selectivity filter, akin to slow inactivation in potassium channels,13 or could be due to re-closure or “slippage” of the S6 activation gate.14 In terms of pharmacology, these structures depict a large cytoplasmic cavity that could accommodate a large blocker such as a local anesthetic molecule, but one of the most intriguing aspects of these new structures is the presence of fenestrations that could, in theory, allow direct access of drugs to the inner vestibule from the membrane. While such portals can be found in the potassium channel structures of KcsA15 and K2P,16,17 their presence here could provide a molecular explanation for putative “hydrophobic pathways” that could allow for closed-state blockade of eukaryotic channels.18 In our recent publication, we reported that the eukaryotic sodium channel blockers benzocaine, lidocaine and ranolazine inhibit NaChBac current with an affinity comparable to the resting block of the mammalian channels.19 Sidedness of blockade by the impermeant blocker QX-314 suggested the receptor for the charged form of the blockers was cytoplasmic. Further, a novel mutation, T220A, in the pore-lining S6 segment, was shown to abolish channel inactivation and was employed to reveal that blocking kinetics were fast or reached equilibrium in the closed state, producing an instantaneous reduction in current upon channel opening. We also observed a concentration-dependent increase in the rate of inactivation in WT channels upon drug exposure, which may be explained by a simple kinetic scheme whereby the drug binding promotes entry into the inactivated state. We now show that the rate of recovery from inactivation in the presence of lidocaine was not affected (Fig. 1). This observation is in contrast to the significant stabilization of the fast-inactivated state which can manifest as a slowing of recovery from fast inactivation seen in eukaryotic Navs in the presence of local anesthetic compounds.20 Thus, it is likely that NaChBac adopts an alternative blocking mode, or mechanism, compared with eukaryotic Nav channels which could underlie differences in drug effects on inactivation properties.
Figure 1. The rate of recovery from inactivation is unaffected by lidocaine. Channels were held at holding potential of -120 mV and activated by 750 ms of depolarizing pulses to -20 mV every 20 sec. (A) A representative family of current traces of WT NaChBac, showing the step-wise recovery from inactivation. Scale bar represents 1 sec and 2 nA. (B) Normalized peak currents are plotted as a function of recovery time interval. The rate of recovery from inactivation is significantly increased in the presence of 1 mM benzocaine, where asterisks indicate (p < 0.05).
The Putative LA-Binding Sites Are Not Conserved in NaChBac
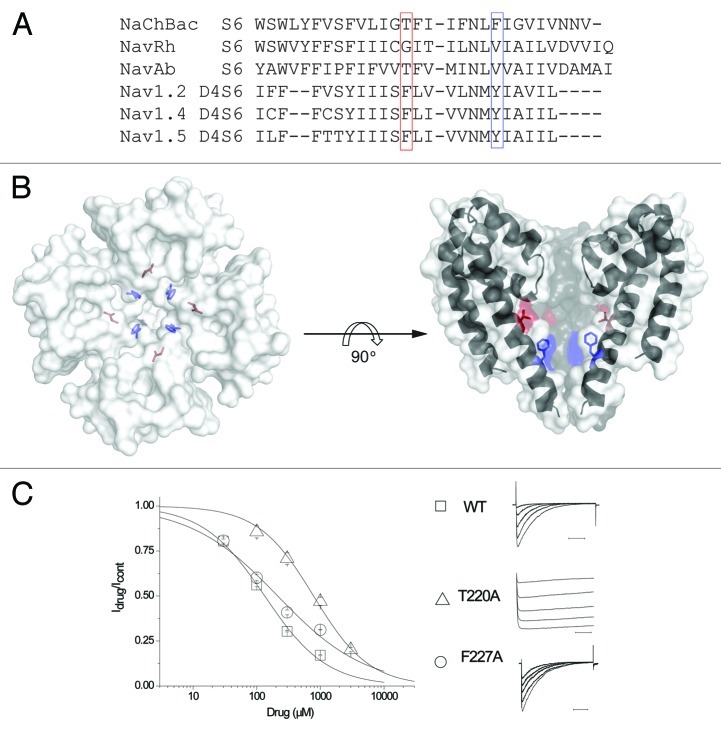
Do bacterial channels provide a long-sought solution for structure-based drug design in sodium channels? Resting blockade and use-dependent inhibition of eukaryotic sodium channels each rely on distinct molecular interactions with different amino acids in the local anesthetic receptor. We aimed to determine which residues support inhibition of NaChBac channels, and if these sites corresponded to those essential for use-dependent inhibition of eukaryotic channels. The sequence comparison between the S6 pore-lining segments of NaChBac and those from eukaryotic sodium channels are shown in Figure 2A, illustrating the partial conservation of residues implicated in supporting use-dependent inhibition in eukaryotic Nav’s. Point mutations of F1764 and Y1771 in Nav1.2, and the corresponding residues in all eukaryotic Nav isoforms, ameliorate use-dependent inhibition by local anesthetic, anti-arrhythmic and anti-epileptic compounds.21,22 It is noteworthy that the aromatic, highlighted by the red box in Figure 2A, which supports lidocaine use-dependent block in eukaryotic channels through a cation-pi interaction,23,24 is entirely unconserved in bacterial channels. To gain more information on the nature of drug block in NaChBac, we examined lidocaine inhibition in T220A and F227A mutant channels (Fig. 2A and B). Surprisingly, alanine mutation of the two residues T220 and F227 in NaChBac showed little variation in lidocaine inhibition IC50s, with ~6-fold and ~2-fold loss of affinity, respectively (Fig. 2C). For comparison, the homologous mutations in Nav1.2 nearly abolish or severely impair use-dependent inhibition for F1764A or Y1771A, respectively.21 Attempts to study the “rescued” pharmacology T220F channel were not possible as this mutant displayed a non-expressing phenotype. Ongoing and future mutagenic studies will serve to further define the determinants of bacterial sodium channel inhibition, and if these coordinates are shared with sites previously identified to support resting block of eukaryotic channels.
Figure 2. The canonical local anesthetic-binding sites are not conserved in NaChBac. (A) The sequence alignment of S6 of bacterial and eukaryotic S6 segments, highlighting two sites implicated in use-dependent inhibition of eukaryotic channels. (B) Top-down view of the highlighted residues shown on the right. (C) A concentration response curve was generated with the mean of Idrug/Icontrol obtained from the peak currents after exposing cells to 30 μM, 100 μM, 300 μM, 1 mM and 3 mM (for T220A only) lidocaine. The IC50 for lidocaine, according to the concentration response curve, is ~135 μM for WT(), ~788 μM for T220A() and ~214 μM for F227A (). Representative current traces are obtained after depolarization from the holding potential -120 to -20 mV in the presence of various lidocaine concentrations, peak current sizes were reduced upon application of increasing lidocaine concentrations (right).
Materials and Methods
The wild-type and mutant NaChBac channels were transiently expressed via calcium phosphate transfection in HEK-293 cells for patch clamp recordings. The patch pipette contained (in mmol/L): 60 CsCl2, 13 NaCl, 80 K-L-Aspartic Acid, 11 EGTA, 1 MgCl2, 1 CaCl2, 10 HEPES (pH 7.2), the bath contained (in mmol/L) 150 NaCl, 2 KCl, 1.5 CaCl2, 1 MgCl2 and 10 HEPES (pH 7.4). Electrode resistance was in the range of 1.0–1.5 MΩ voltage errors due to series resistance was always < 3 mV after compensation and liquid junction potentials were corrected. All experiments were performed at room temperature.
Conclusions
In addition to the inhibition of the bacterial sodium channel described here, lidocaine can rapidly and reversibly block a variety of channels and receptor types, including KATP, K2P, T-type Ca2+, hyperpolarization activated channels in addition to nicotinic acetylcholine receptors as well as eukaryotic sodium channels, suggesting that a minimal common molecular architecture is shared among these channel types.25-29 However, the recent appearance of bacterial sodium channel structures represents a significant step toward the long-held goal of structure-based drug design in sodium channels. The pharmacological and functional commonalities shared between bacterial and eukaryotic channels have been, thus far, limited by lack of detailed information on bacterial gating and pharmacological parameters. In this light, our data on local anesthetic inhibition of NaChBac has begun to highlight potential similarities and differences between these disparate channels.
Footnotes
Previously published online: www.landesbioscience.com/journals/channels/article/21807
References
- 1.Hille B. Ion channels of excitable membranes. 3rd ed2001, Sunderland, Mass.: Sinauer. xviii, 814 p. [Google Scholar]
- 2.Ruan Y, Liu N, Priori SG. Sodium channel mutations and arrhythmias. Nat Rev Cardiol. 2009;6:337–48. doi: 10.1038/nrcardio.2009.44. [DOI] [PubMed] [Google Scholar]
- 3.Roden DM, George AL., Jr. The cardiac ion channels: relevance to management of arrhythmias. Annu Rev Med. 1996;47:135–48. doi: 10.1146/annurev.med.47.1.135. [DOI] [PubMed] [Google Scholar]
- 4.Waxman SG, Hains BC. Fire and phantoms after spinal cord injury: Na+ channels and central pain. Trends Neurosci. 2006;29:207–15. doi: 10.1016/j.tins.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Waxman SG, Dib-Hajj S, Cummins TR, Black JA. Sodium channels and pain. Proc Natl Acad Sci USA. 1999;96:7635–9. doi: 10.1073/pnas.96.14.7635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meisler MH, Kearney JA. Sodium channel mutations in epilepsy and other neurological disorders. J Clin Invest. 2005;115:2010–7. doi: 10.1172/JCI25466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ren D, Navarro B, Xu H, Yue L, Shi Q, Clapham DE. A prokaryotic voltage-gated sodium channel. Science. 2001;294:2372–5. doi: 10.1126/science.1065635. [DOI] [PubMed] [Google Scholar]
- 8.Blanchet J, Pilote S, Chahine M. Acidic residues on the voltage-sensor domain determine the activation of the NaChBac sodium channel. Biophys J. 2007;92:3513–23. doi: 10.1529/biophysj.106.090464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yue L, Navarro B, Ren D, Ramos A, Clapham DE. The cation selectivity filter of the bacterial sodium channel, NaChBac. J Gen Physiol. 2002;120:845–53. doi: 10.1085/jgp.20028699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang X, Ren W, DeCaen P, Yan C, Tao X, Tang L, et al. Crystal structure of an orthologue of the NaChBac voltage-gated sodium channel. Nature. 2012;486:130–4. doi: 10.1038/nature11054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Payandeh J, Gamal El-Din TM, Scheuer T, Zheng N, Catterall WA. Crystal structure of a voltage-gated sodium channel in two potentially inactivated states. Nature. 2012;486:135–9. doi: 10.1038/nature11077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Payandeh J, Scheuer T, Zheng N, Catterall WA. The crystal structure of a voltage-gated sodium channel. Nature. 2011;475:353–8. doi: 10.1038/nature10238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pavlov E, Bladen C, Winkfein R, Diao C, Dhaliwal P, French RJ. The pore, not cytoplasmic domains, underlies inactivation in a prokaryotic sodium channel. Biophys J. 2005;89:232–42. doi: 10.1529/biophysj.104.056994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shin KS, Maertens C, Proenza C, Rothberg BS, Yellen G. Inactivation in HCN channels results from reclosure of the activation gate: desensitization to voltage. Neuron. 2004;41:737–44. doi: 10.1016/S0896-6273(04)00083-2. [DOI] [PubMed] [Google Scholar]
- 15.Doyle DA, Morais Cabral J, Pfuetzner RA, Kuo A, Gulbis JM, Cohen SL, et al. The structure of the potassium channel: molecular basis of K+ conduction and selectivity. Science. 1998;280:69–77. doi: 10.1126/science.280.5360.69. [DOI] [PubMed] [Google Scholar]
- 16.Miller AN, Long SB. Crystal structure of the human two-pore domain potassium channel K2P1. Science. 2012;335:432–6. doi: 10.1126/science.1213274. [DOI] [PubMed] [Google Scholar]
- 17.Brohawn SG, del Mármol J, MacKinnon R. Crystal structure of the human K2P TRAAK, a lipid- and mechano-sensitive K+ ion channel. Science. 2012;335:436–41. doi: 10.1126/science.1213808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hille B. Local anesthetics: hydrophilic and hydrophobic pathways for the drug-receptor reaction. J Gen Physiol. 1977;69:497–515. doi: 10.1085/jgp.69.4.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee S, Goodchild SJ, Ahern CA. Local anesthetic inhibition of a bacterial sodium channel. J Gen Physiol. 2012;139:507–16. doi: 10.1085/jgp.201210779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bean BP, Cohen CJ, Tsien RW. Lidocaine block of cardiac sodium channels. J Gen Physiol. 1983;81:613–42. doi: 10.1085/jgp.81.5.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ragsdale DS, McPhee JC, Scheuer T, Catterall WA. Molecular determinants of state-dependent block of Na+ channels by local anesthetics. Science. 1994;265:1724–8. doi: 10.1126/science.8085162. [DOI] [PubMed] [Google Scholar]
- 22.Ragsdale DS, McPhee JC, Scheuer T, Catterall WA. Common molecular determinants of local anesthetic, antiarrhythmic, and anticonvulsant block of voltage-gated Na+ channels. Proc Natl Acad Sci USA. 1996;93:9270–5. doi: 10.1073/pnas.93.17.9270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pless SA, Galpin JD, Frankel A, Ahern CA. Molecular basis for class Ib anti-arrhythmic inhibition of cardiac sodium channels. Nat Commun. 2011;2:351. doi: 10.1038/ncomms1351. [DOI] [PubMed] [Google Scholar]
- 24.Ahern CA, Eastwood AL, Dougherty DA, Horn R. Electrostatic contributions of aromatic residues in the local anesthetic receptor of voltage-gated sodium channels. Circ Res. 2008;102:86–94. doi: 10.1161/CIRCRESAHA.107.160663. [DOI] [PubMed] [Google Scholar]
- 25.Olschewski A, Bräu ME, Olschewski H, Hempelmann G, Vogel W. ATP-dependent potassium channel in rat cardiomyocytes is blocked by lidocaine. Possible impact on the antiarrhythmic action of lidocaine. Circulation. 1996;93:656–9. doi: 10.1161/01.CIR.93.4.656. [DOI] [PubMed] [Google Scholar]
- 26.Kindler CH, Paul M, Zou H, Liu C, Winegar BD, Gray AT, et al. Amide local anesthetics potently inhibit the human tandem pore domain background K+ channel TASK-2 (KCNK5) J Pharmacol Exp Ther. 2003;306:84–92. doi: 10.1124/jpet.103.049809. [DOI] [PubMed] [Google Scholar]
- 27.Alberola-Die A, Martinez-Pinna J, González-Ros JM, Ivorra I, Morales A. Multiple inhibitory actions of lidocaine on Torpedo nicotinic acetylcholine receptors transplanted to Xenopus oocytes. J Neurochem. 2011;117:1009–19. doi: 10.1111/j.1471-4159.2011.07271.x. [DOI] [PubMed] [Google Scholar]
- 28.Bladen C, Zamponi GW. Common mechanisms of drug interactions with sodium and T-type calcium channels. Mol Pharmacol. 2012;82:481–7. doi: 10.1124/mol.112.079715. [DOI] [PubMed] [Google Scholar]
- 29.Meng QT, Xia ZY, Liu J, Bayliss DA, Chen X. Local anesthetic inhibits hyperpolarization-activated cationic currents. Mol Pharmacol. 2011;79:866–73. doi: 10.1124/mol.110.070227. [DOI] [PMC free article] [PubMed] [Google Scholar]