Abstract
Aim:
Emerging racial/ethnic disparities in tobacco use behaviors and resulting long-term health outcomes highlight the importance of developing culturally tailored/targeted tobacco prevention and cessation interventions. This manuscript describes the efficacy and the components of prevention and cessation interventions developed for minority adolescents.
Methods:
Thirteen studies focused on culturally tailoring and targeting tobacco prevention/cessation interventions were selected and information on intervention design (type, number of sessions), setting (school or community), theoretical constructs, culture-specific components (surface/deep structures), and treatment outcomes were extracted.
Results:
Of the 13 studies, 5 focused on prevention, 4 on cessation, and 4 combined prevention and cessation, and most of the studies were primarily school-based, while a few used community locations. Although diverse minority groups were targeted, a majority of the studies (n = 6) worked with Hispanic adolescents. The most common theoretical construct examined was the Social Influence Model (n = 5). The overall findings indicated that culturally tailoring cessation interventions did not appear to improve tobacco quit rates among minority adolescents, but culturally tailored prevention interventions appeared to produce lower tobacco initiation rates among minority adolescents than control conditions.
Conclusions:
The results of review suggest that there is a critical need to develop better interventions to reduce tobacco use among minority adolescents and that developing a better understanding of cultural issues related to both cessation and initiation of tobacco use among minority populations is a key component of this endeavor.
Introduction
Despite the decrease in overall cigarette smoking rates among adolescents, smoking rates among minority adolescents have remained constant and may have even risen in recent years (Centers for Disease Control and Prevention, 2009). These discrepant rates are known to extend into adulthood and may explain disproportionate rates of tobacco-related diseases that affect minority populations (Wong, Shapiro, Boscardin, & Ettner, 2002). To address this major health burden, interventions aimed at minority adolescents that preclude smoking initiation among nonsmokers and cease smoking among smokers are critical.
In the United States, epidemiological evidence suggests that African American adolescents have lower levels of smoking initiation and current smoking than White and Hispanic adolescents (Griesler & Kandel, 1998; Kandel, Kiros, Schaffran, & Hu, 2004). However, smoking rates among African Americans grow and even surpass that of their White counterparts during adulthood (25.6% versus 23.5%; Garrett, Dube, Trosclair, Caraballo, & Pechacek, 2011). Importantly, 68.1% of African American adolescent smokers want to quit, but the actual quit rate is at 8.7% (Centers for Disease Control and Prevention, 2009). Similar disparities exist among Hispanic adolescents; for example, Hispanic adolescents have smoking rates that are as high as or higher than those of White adolescents (Ellickson, Orlando, Tucker, & Klein, 2004), and although smoking rates in White adolescents decreased from 2006 to 2009 (9.2% to 7.1%), Hispanic adolescents showed trends of increased use in this same time period (10.9% to 11.1%) and exceeded the rates of use among White adolescents (Centers for Disease Control and Prevention, 2009).
Less examined but still of considerate concern are smoking behaviors of Asian Americans, American Indians, and Hawaiian/Pacific Islanders. Evidence from the National Youth Tobacco Survey indicates that even though Asian American youth smoke at a lower rate than other minority groups, this rate grows in late adolescence; as 12th graders, 42.5% initiated smoking and 33.0% smoked in the past 30 days; these rates are higher than the rates of other racial/ethnic minority groups (Appleyard, Messeri, & Haviland, 2001). American Indian youth show high rates tobacco use at an early age; cigarette use is 30.6% in 5th grade, 60.4% in 7th grade, and smokeless tobacco use is 19.0% in 5th grade and 32.6% in 7th grade (Davis, Lambert, Cunningham-Sabo, & Skipper, 1995). In addition to these major ethnic/racial groups, tobacco use behaviors of other minority groups are beginning to be examined. For example, Arab American adolescents are more likely to use other forms of tobacco, such as water pipes compared with non-Arab American adolescents (38% versus 22%; Rice, Weglicki, Templin, Jamil, & Hammad, 2010). These alarming tobacco use incidences and rates among minority adolescents further demonstrate the need to culturally target and tailor tobacco interventions.
Tobacco interventions aimed at adolescents are crucial because smoking is initiated, and progression to regular smoking and nicotine dependence are established in this developmental period. Even smoking an average of two cigarettes per day is predictive of symptoms of nicotine dependence and long-term tobacco use among adolescents (DiFranza et al., 2002). Furthermore, among high school students who smoke daily, 60.9% report having made a quit attempt (Centers for Disease Control and Prevention, 2009), but the majority of them are unsuccessful, with 12% quit rate when aided by an intervention and 7% quit rate when unaided (Sussman, 2002). Unfortunately, despite the desire to quit smoking, minority smokers are even less likely than White smokers to join smoking cessation interventions (Levinson, Pérez-Stable, Espinoza, Flores, & Byers, 2004; Zhu, Melcer, Sun, Rosbrook, & Pierce, 2000).
To enhance the efficacy of tobacco interventions for minority adolescents, researchers have called for culturally targeting and tailoring tobacco interventions. Targeted interventions focus on expanding the generalizability of an intervention (developed in other populations) to minority groups, and while these interventions may have embedded dominant cultural values, they do not take the values and experiences of a minority group into consideration. In contrast, tailored interventions focus on ensuring that the intervention meets the unique needs of the minority group by including ethnic/cultural experiences, norms, and values. Another way to culturally tailor an intervention is to start from the culture and then subsequently build on the cultural values, which is also known as culturally grounded approach (Pasick, D’Onofrio, & Otero-Sabogal, 1996; Resnicow, Soler, Braithwaite, Ahluwalia, & Butler, 2000).
Cultural targeting and tailoring can be further categorized into two dimensions: “surface” and “deep structure” (Resnicow, Braithwaite, Ahluwalia, & Baranowski, 1999; Resnicow et al., 2000). Surface structure refers to matching the intervention materials to the preferred characteristics of a target population, such as matching the race/ethnicity of the staff to the group and using culturally relevant settings/channels, music, foods, and language. In contrast, deep structure reflects integrating the cultural, social, historical, and psychological influences of the behaviors (i.e., tobacco use) in the target populations.
To our knowledge, existing reviews of adolescent tobacco prevention and cessation studies have not addressed cultural values and experiences of the minority group (Christakis, Garrison, Ebel, Wiehe, & Rivara, 2003; Garrison, Christakis, Ebel, Wiehe, & Rivara, 2003; Wiehe, Garrison, Christakis, Ebel, & Rivara, 2005). Additionally, we are not aware of any reviews that have examined tobacco prevention and cessation studies together. This is important because these two types of interventions contain overlapping program materials, and they are often offered simultaneously in schools. To fill these gaps in the literature, we conducted a comprehensive review of tobacco prevention and cessation interventions for minority adolescents and based on this review, have also provided some directions for future research.
Methods
Two independent reviewers searched tobacco intervention studies that were targeted and tailored to minority adolescents and published between 1990 and 2011 on Medline. Search terms for racial/ethnic minorities were “minority,” “Black,” “African American,” “Caucasian,” “White,” “Hispanic,” “Latino,” “Latina,” “American Indian,” “Native American,” “Native Hawaiian,” “Pacific Islander,” “Asian,” “multiethnicity,” and “mixed ethnicity.” Search terms for tobacco interventions combined “smoking” “tobacco” “cigarette” with “cessation” and “prevention.” Words for racial/ethnic minority and tobacco intervention were paired with “adolescent”, “youth,” and “student” to ensure that the searches identified middle and high school-aged adolescents. Other inclusion criteria were (a) at least 50% of the sample comprised racial/ethnic minority, (b) at least 50% of the intervention focused on tobacco outcomes, (c) the intervention had more than one session, (d) the intervention was conducted in the United States, and (e) the treatment outcomes were initiation or reduction/cessation of smoking behaviors.
Results
Figure 1 shows a flow chart of the articles identified through the initial search to the final articles included in the review. Of the initial 694 articles identified, 164 abstracts and articles were retrieved for further screening. Of these, 30.4% did not meet 1–2 inclusion criteria, 63.6% did not meet 3–4, and 6.0% did not meet all. The use of a noninterventional study design (80.1%) was the most common reason for exclusion. The 12 articles that met the inclusion criteria were coded on the type of intervention (prevention or cessation), demographic characteristics (age, grade, race/ethnicity), setting (school or community), number of sessions, and number of participants that received the intervention (See Table 1). Table 2 presents the theoretical constructs and culture-specific components (surface and deep structures) and Table 3 presents the intervention and control/standard conditions and end-of-treatment (EOT) and follow-up outcomes.
Figure 1.
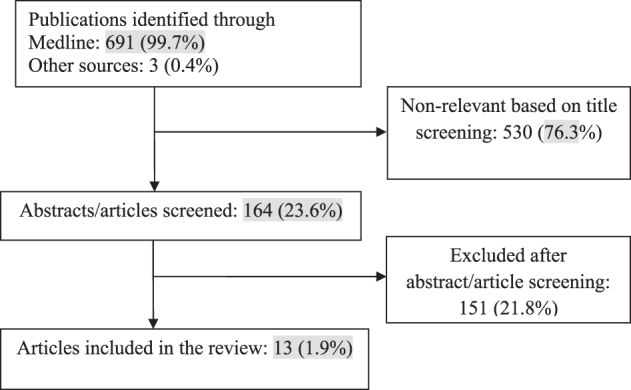
Flow chart of article selection.
Table 1.
Description of Participants and Culturally Targeted/Tailored Tobacco Interventions Characteristics
| Author/year | Race/ethnicity | Location | Age/grade | Prevention/cessation | Setting | Number of sessions | N |
| Albrecht et al. (1998) | African American 63%, White 37% | N/A | Ages 12–20 | Cessation | School-based, clinics | 8 | 84 |
| Botvin et al. (1992) | Hispanic 56%, African American 19%, White 14%, Other 12% | New York City, NY | Grade 7 (M age = 13) | Prevention | School-based, classroom | 15 | 3,153 |
| Elder et al. (2002) | Hispanic 100% | San Diego, CA | Ages 11–16 (M = 13) | Prevention | Community-based, group | 8 | 660 adolescent–caregiverdyads |
| Guilamo-Ramos et al. (2010) | Hispanic 74%, African American 24%, Other 2% | New York City, NY | Grades 6–7 | Prevention | School-based | 2 | 1,386 adolescent–mother dyads |
| Horn et al. (2005) | American Indian 82%, Other 18% | NC | Ages 14–19 (M = 16) | Cessation | School-based, classroom | 10 | 74 |
| Joffe et al. (2009) | African-American 56%, White 29%, Not reported 15% | Baltimore/Howard County, MD | Grades 9–12 | Cessation | School-based, group, classroom | 15 (N-O-T), 20 (Kickin’ Butt) | 407 |
| Johnson et al. (2005) | Hispanic 58%–61%, Asian 22%–24%, White 6%–8%, Multiethnic 9%–11%, African-American 1%–2% | Southern California | Grades 6–8 | Prevention/cessation | School-based, classroom | 8 | 3,157 |
| Kaufman et al. (1994) | African American 100% | Chicago, IL | Grades 6-7 (M age = 11.7) | Prevention | School and community-based | 7 | 276 |
| Ma et al. (2004) | Chinese-American 100% | Delaware region, PA/NJ | Ages 14–19 (M = 17.7) | Cessation | Community-based | 10 | 17 |
| Prokhorov et al. (2008) | Hispanic 51%, African-American 39%, Other 10% | Houston, TX | Grade 10 | Prevention/cessation | School-based, individual | 7 | 1,160 |
| Rice et al. (2010) | Arab-American 62%–66%, Other 38%–34% | Mid-West | Grade 9 (M age = 15.2) | Prevention/cessation | School-based, classroom | N/A | 616 |
| Schinke et al. (1996) | Native American 100% | Northeast | Grades 4–6 (M age = 10.6) | Prevention | Community | 15 | 117 |
| Sun et al. (2007) | Hispanic 71%, White 16%. African-American 5%, Other 4%, Asian 4% | Southern California | Ages 13–19 (M = 16.5) | Prevention/cessation | School-based, classroom | 8 | 1,097 |
Note. N/A = not available.
Table 2.
Cultural Components and Theoretical Constructs of the Culturally Targeted/Tailored Adolescent Tobacco Prevention/Cessation Interventions
| Author/year | Surface structure | Deep structure | Theoretical foundation |
| Albrecht et al. (1998) | Targeted African American pregnant girls | Added peer component to the program | CBT/peer component |
| Botvin et al. (1992) | Targeted mostly African American/Hispanic adolescents | N/A | CBT/social resistance skills training |
| Lowered the reading level | |||
| Elder et al. (2002) | Targeted migrant Hispanic adolescents and parents | Incorporated values of familismo (interdependence of family members) and respecto (respect for others) | SI/parental component |
| Bilingual, bicultural staff conducted surveys and groups | Themes of role plays represented experiences common to migrant Hispanic adolescents | ||
| Groups conducted in evening hours to facilitate parents’ schedules | |||
| Offered Spanish version of the survey to adolescents and parents | |||
| Guilamo-Ramos et al. (2010) | Targeted mostly Hispanic/African American adolescents and mothers | Added parent component to the program | SI |
| Bilingual callers recruited parents | Tailored the English manual separately for Hispanic and African American parents | ||
| Program materials were in either English or Spanish | |||
| Horn et al. (2005) | Targeted American Indian adolescents | Provided facts about tobacco-use rates, addiction, and health consequences specific to American Indian populations | SCT |
| Recruitment and intervention materials used program logos, audio media graphics, themes, and text relevant for American Indian youth | Provided history of tobacco use among American Indians | ||
| Recruitments held in churches, powwows, tribal council meetings, and youth groups | Focused on group identity and cohesion rather than individual efforts | ||
| American Indians conducted the program and comprised the advisory board | Focused on the impact of a teenager’s smoking on family and community | ||
| Used culturally appropriate interactive problem-solving methods and activities | |||
| Included activity options that involved family members | |||
| Joffe et al. (2009) | Targeting mostly African American adolescents | N/A | SCT/SI |
| Johnson et al. (2005) | Targeted mostly Hispanic and Asian adolescents | Incorporated Hispanic values: familisim and simpatia (harmonious interpersonal relations) | SI |
| Ethnically diverse staff distributed the surveys | Incorporated Asian values: filial piety (respect of ancestors), saving face (prevent dishonoring the family), and health as a balanced body, mind, and spirit | ||
| Multicultural experiences included acculturative stress, discrimination, and family conflicts that can occur during the acculturation process | |||
| Activities included: role play in the style of a telenovela (a soap opera format on Spanish-language television), Chinese yin-yang symbol, tai chi as stress management, culturally relevant scenarios such as quinceanera (15th birthday party) | |||
| Kaufman et al. (1994) | Targeted African American adolescents | Smoking prevention program curriculum printed on the weekly children's page of a newspaper with predominantly African American readership. It included interactive exercises for the children to complete with their parents | SI |
| Conducted a smoking prevention rap contest | Radio station ran smoking prevention service announcements and aired a call-in talk show with a focus on helping parents to increase their communication with their children | ||
| Conducted a smoking prevention poster contest and 5 winning posters were displayed in billboards in 5 different locations in the Chicago area | |||
| Used radio and newspaper as channels of intervention delivery | |||
| Ma et al. (2004) | Targeted Chinese American adolescents | Included Asian cultural themes of interdependency and collective orientation, harmony (parent | SCT |
| Handouts and visual media featured Asian youth | Used trivia questions on the achievements of famous Asian | ||
| Prokhorov et al. (2008) | Targeted mostly Hispanic/African American adolescents | N/A | TTM/SCT |
| Rice et al. (2010) | Targeted Arab-American adolescents | N/A | SI |
| Intervention offered in Arabic and English | |||
| Bilingual educators administered the intervention | |||
| Both Middle Eastern and non-Middle Eastern figures included in program materials | |||
| Schinke et al. (1996) | Targeted Native American adolescents | Included spiritual and cultural values related to health behaviors | N/A |
| Native American staff delivered the intervention | Increased knowledge of ancestral tobacco use and modern-day abuse | ||
| Used Native American food, arts and crafts, music, movement and storytelling methods to relay cultural messages | Emphasized the importance of negative peer and social influence and positive influence of family | ||
| Native American role models including visual artists and theater performers | |||
| Examined commercialization of tobacco in the media | |||
| Sun et al. (2007) | Targeted mostly Hispanic adolescents | N/A | SI |
Note. CBT = Cognitive Behavioral Theory; SI = Social Influence Model; SCT = Social Cognitive Theory; TTM = Transtheoretical Model of Change.
Table 3.
Treatment Outcomes of Tobacco Interventions
| Author/year | Conditions | Smoking measure | Initiation/cessation/reduction | Intervention group rates | Control/standard group rates |
| Albrecht et al. (1998) a | Intervention 1: Teen Fresh Start (TFS), a standardized cognitive behavioral group model designed for adolescents. | Current smoking | Cessation | Intervention 2: EOT: 30.0% | Intervention 1 + control group: EOT: 16.6% |
| Intervention 2: Teen Fresh Start Plus Buddy (TFSB), TFS+peer component | |||||
| Control: Usual care (UC), a 30-minute individual educational session with the nurse | |||||
| Botvin et al. (1992) a | Intervention: CBT/social resistance skills training | 30-day smoking | Initiation | BL: 4.86%, 4-mo: 5.19%* | BL: 5.03%, 4-mo: 7.15%* |
| Control: no contact control group | |||||
| Elder et al. (2002) a | Intervention: Sembrando Salud (Sowing the Seeds of Health), tobacco and alcohol use prevention | 30-day smoking | Initiation | BL: 3.0%, EOT: 2.5%, 1-yr: 3.3%, 2-yr: 2.9% | BL: 3.1%, EOT: 4.6%, 1-yr: 4.7%, 2-yr: 3.5% |
| Control: first aid/home safety prevention | |||||
| Guilamo-Ramos et al. (2010) | All adolescents received Project TNT and parents were randomized to either The Linking Lives Health Education Program, focused on effective communication and parental monitoring strategies for preventing adolescent tobacco use or control curriculum about how to choose a high school | Ever tried smoking | Initiation | BL: 5.0%, 15-mo: 5.0%* | BL: 5.0%, 15-mo: 10.0%* |
| Horn et al. (2005) a | Intervention: American Indian N-O-T. Control: Brief 15-minute intervention with quit-smoking advice and the Center for Disease Control (CDC) brochure on quitting smoking | 24-hr abstinence | Cessation | 3-mo: 18-29% males quit, no females quit | 3-mo: 14.3% males quit, no females quit |
| Joffe et al. (2009) a | Intervention 1: Kickin’ Butts | Quit smoking | Cessation | Intervention 1: EOT 14%, 1-mo: 9%, 6-mo: 10%, 12-mo: 9% | Control: EOT: 13%, 1-mo: 6%, 6-mo: 15%, 12-mo: 12% |
| Intervention 2: N-O-T | Intervention 2: EOT: 18%, 1-mo: 13%b, 6-mo: 5%, 12-mo: 7% | Control: EOT: 17%, 1-mo: 9%b, 6-mo: 9%, 12-mo: 6% | |||
| Control: participants in each intervention arm were randomized to intervention or a single session intervention that encouraged students to quit and provided smoking-cessation pamphlets. | |||||
| Johnson et al. (2005) | Intervention: Project FLAVOR (Fun Learning About Vitality, Origins, and Respect), a multicultural tobacco prevention curriculum | Ever tried smoking | Initiation | Intervention vs. Control: 1-yr: 8%c, 2-yr: OR = 0.77d , e | Standard vs. Control: 1-yr: 11%c, 2-yr: OR= 0.97d |
| Standard curriculum: Project CHIPS (Choosing Healthy Influences for a Positive Self), tobacco prevention without culture specific values | |||||
| Waitlist control | 30-day smoking | Cessation | 2-yr: OR = 0.40 d , e | 2-yr: OR = 0.74d | |
| Kaufman et al. (1994) | Intervention: School curriculum + media. | Composite score of cigarette usef | Reduction | BL: M = 13.0 (SD = 2.3), EOT: M = 13.6 (SD = 1.8), 6-mo: M = 11.6 (SD = 4.0) | BL: M = 12.3, (SD = 1.9), EOT: M = 13.3 (SD = 1.9), 6-mo: 11.0 (SD = 2.5) |
| Comparison group: media only | |||||
| Ma et al. (2004) | Intervention: Asian Adolescents Choose Tobacco Free (ACT) | Quit smoking | Cessation, | EOT: 0.0%, 3-mo: 18.2% | EOT: 22.0%, 3-mo: 23.1% |
| Standard care: N-O-T as standard curriculum | |||||
| Prokhorov et al. (2008) | Intervention: A Smoking Prevention InteractiveExperience (ASPIRE) | Current smoking | Initiation | 18-mo: 1.9%* | 18-mo: 5.8%* |
| Standard-care: provided National Cancer Institute’s Clearing the Air self-help booklet | Past week smoking | Cessation | 18-mo: 60.7% | 18-mo: 61.8% | |
| Rice et al. (2010) a | Intervention: 9th graders received Arab-American Tobacco Use (AATU) | Ever tried smoking | Initiation | 1-yr: 23.3%* | Control group 1: 1-yr: 30.5%* Control group 2: 1-yr: 26.5%* |
| Control 1: 10th graders who did not receive intervention | current smoking | Cessation | 1-yr: 8.1%* | Control group 1: 1-yr: 10.6%* Control group 2: 1-yr: 11.3%* | |
| Control 2: 10th graders assessed one year after the end of intervention as a second comparison group to control for historic effects | Regular smoking | 1-yr: 5.6% | Control group 1: 1-yr: 7.3% Control group 2: 1-yr: 6.5% | ||
| Schinke et al. (1996) a | Intervention 1: Tobacco prevention only | Ever tried smoking | Initiation | Intervention 1 BL: 28% EOT: 28% 6-mo: 26% | Control BL: 20% EOT: 30% 6-mo: 43%* |
| Intervention 2: Diet only | Intervention 2 BL: 24% EOT: 30% 6-mo: 40% | ||||
| Intervention 3: Tobacco and diet | Intervention 3 BL: 18% EOT: 18% 6-mo: 18%* | ||||
| Control: no treatment | Current smoking | Intervention 1 BL: 0% EOT: 0% 6-mo: 0% | Control BL: 11%* EOT: 43% 6-mo: 25% | ||
| Intervention 2 BL: 30%* EOT: 30% 6-mo: 30% | |||||
| Intervention 3 BL: 0% EOT: 0% 6-mo: 0% | |||||
| Sun et al. (2007) | Intervention: Project EX (adapted from TNT). | Past week smoking | Reduction | BL: 32.5%, EOT: 25.6%, 6-mo: OR = 0.33e , g, 1-yr: OR = 0.59e , g | BL: 33.3%, EOT: 32.6% |
| Standard-care: students received tobacco prevention or cessation activities offered at the schools |
Note. *Statistically significant differences between intervention and control condition(s). BL = baseline; EOT = end-of-treatment; CO = expired-air carbon monoxide; Mo = month; Yr = year.
Other smoking measures are not included in this table.
Self-reported quit rate not confirmed by cotinine at 1-month follow up in the intervention group was significantly greater than the control group.
1-year follow-up outcomes reported in Unger et al. (2004).
Percentages were not reported.
The odds ratio is significantly different from that of the control group.
Smoking composite score consisted of personal use of cigarettes, family/peer use, experiencing difficulty as a result of smoking cigarettes, parents would be angry if they found out about smoking, what student would do if a friend offered them cigarettes. Scores ranged from 6 to 32, with higher scores indicating higher level of use.
The odds ratios of follow-up assessments were reported in Sussman et al. (2007).
The included studies targeted diverse ethnic/racial groups: four (31%) targeted single racial/ethnic group: African American (Kaufman, Jason, Sawlski, & Halpert, 1994), Chinese-American (Ma, Shive, Tan, Thomas, & Man, 2004), Hispanic (Elder et al., 2002), and Native American (Schinke, Singer, Cole, & Contento, 1996), and the rest targeted more than one minority group, which included, but was not limited to, predominantly Hispanic (Botvin et al., 1992; Guilamo-Ramos et al., 2010; Johnson et al., 2005; Prokhorov et al., 2008; Sun, Miyano, Rohrbach, Dent, & Sussman, 2007), African American (Albrecht, Payne, Stone, & Reynolds, 1998; Joffe et al., 2009), American Indian (Horn et al., 2005), and Arab American adolescents (Rice et al., 2010).
Different age groups were represented: five (38%) primarily focused on middle school ages (Botvin et al., 1992; Guilamo-Ramos et al., 2010; Johnson et al., 2005; Kaufman et al., 1994; Schinke et al., 1996), six (46%) on high school ages (Horn et al., 2005; Joffe et al., 2009; Ma et al., 2004; Prokhorov et al., 2008; Rice et al., 2010; Sun et al., 2007), and two (9%) combined middle and high school ages (Albrecht et al., 1998; Elder et al., 2002).
Five (38%) focused on tobacco prevention, four (31%) on cessation, and four (31%) on both prevention and cessation. The majority (n = 9, 69%) was based in school settings, using mostly classroom-based activities (Botvin et al., 1992; Guilamo-Ramos et al., 2010; Horn et al., 2005; Joffe et al., 2009; Johnson et al., 2005; Rice et al., 2010; Sun et al., 2007), one used an individualized intervention during school hours (Prokhorov et al., 2008), and another used school-based clinic (Albrecht et al., 1998). Three (23%; Elder et al., 2002; Ma et al., 2004; Schinke et al., 1996) were based in community organizations and one was conducted in both school and community settings (Kaufman et al., 1994). Most studies (85%) targeted only tobacco use behavior with the exception of one study that also targeted alcohol use behaviors (Elder et al., 2002) and another study targeted dietary behaviors (Schinke et al., 1996).
The sample sizes used varied considerably depending on the type of intervention, with smoking cessation studies having smaller sizes (e.g., n = 17; Ma et al., 2004) and multisite school-based prevention studies having larger samples sizes (e.g., n > 3,000; Johnson et al., 2005). The number and duration of sessions were also wide ranging; interventions with fewer sessions tended to have longer session durations (e.g., two sessions—each 2.5 hr long; Guilamo-Ramos et al., 2010) and those with more sessions were shorter (e.g., 15–20 sessions—each 25–30 min long; Joffe et al., 2009). Ten (77%) reported follow-up assessment periods that varied from 3 months (e.g., Horn et al., 2005) to 2 years (e.g., Elder et al., 2002), and three (23%) did not report any follow-up data. One of the two studies that did not include follow-up data (i.e., Sun et al., 2007) reported them in a different article (See Sussman, Miyano, Rohrbach, Dent, & Sun, 2007).
Cultural Components
The cultural components included in the interventions are summarized in Table 2. Five (38%) targeted the intervention to minority groups without culturally modifying its contents (Albrecht et al., 1998; Botvin et al., 1992; Joffe et al., 2009; Prokhorov et al., 2008; Sun et al., 2007), and eight (62%) tailored the intervention to specific minority populations (Elder et al., 2002; Guilamo-Ramos et al., 2010; Horn et al., 2005; Johnson et al., 2005; Kaufman et al., 1994; Ma et al., 2004; Rice et al., 2010; Schinke et al., 1996).
Of the eight culturally tailored interventions, two (15%; Johnson et al., 2005; Schinke et al., 1996) used a culturally grounded approach. Cultural modification of preexisting interventions was more common: two (15%; Horn et al., 2005; Ma et al., 2004) culturally adapted the American Lung Association’s (ALA) Not on Tobacco (N-O-T) program, and two (15%; Guilamo-Ramos et al., 2010; Rice et al., 2010) modified Project Towards No Tobacco Use (TNT; Sussman, Dent, Burton, Stacy, & Flay, 1995).
Surface Structure
The most common surface structural change was the use of bicultural/bilingual staff; for example, ethnically diverse staff or staff whose ethnicity matched the ethnicity of the target group conducted assessments (Elder et al., 2002; Johnson et al., 2005) or provided the tobacco cessation intervention (Rice et al., 2010; Schinke et al., 1996). Other surface structure changes included the use of program materials in the language of the target population (Guilamo-Ramos et al., 2010), culturally relevant graphics in print and audio visual media in recruitment and counseling materials (Horn et al., 2005; Johnson et al., 2005; Ma et al., 2004; Schinke et al., 1996), recruitment from specific settings like minority churches, powwows, tribal council meetings, and community-based youth groups (Horn et al., 2005; Schinke et al., 1996). Surface structure change was also introduced by the channel in which the intervention was delivered. For example, Kaufman et al. (1994) disseminated the smoking prevention curriculum using radio and newspaper services with predominantly African American listening audience and readership; specifically, the radio was used for smoking prevention service announcements, as well as for a call-in talk show designed to help parents to increase communication with their children about not smoking, and the newspaper advertisements included interactive exercises for parents and children. They also conducted a billboard contest of smoking prevention poster and a rap contest.
Deep Structure
Deep structural changes involved incorporating culture specific values into tobacco interventions. For instance, tobacco prevention interventions (Elder et al., 2002; Johnson et al., 2005) tailored to Hispanic youth have incorporated cultural themes of “familism” (interdependence of family members), “simpatia” (harmonious interpersonal relations), and “respecto” (showing respect to elders). These themes were used to frame tobacco refusal skills without offending others and to increase motivation to quit by thinking about the ways in which smoking hurts family members.
Two interventions (15%), Project FLAVOR, developed to prevent smoking among Hispanic and Asian middle school students, and Asian Adolescents Choose Tobacco-Free (ACT), a smoking cessation intervention tailored to Chinese American youth (Ma et al., 2004), discussed themes of Asian culture, such as filial piety (respect of ancestors), “saving face” (prevent embarrassing or dishonoring the family unit), interdependency and collective orientation, maintenance of harmony in terms of parent–child dynamics, and the effects of smoking on both body and mind. Other core cultural values, such as persistence, hard work, success, and emphasis on education, as well as the negative effects of smoking on academic performance framed antitobacco messages.
Finally, two smoking cessation interventions tailored to American Indian high school students used historical context of tobacco use among American Indians and Alaskan Natives to motivate students to quit tobacco use; specifically, the educational materials discussed how commercialization and mass manufacturing of tobacco replaced aboriginal botanicals and traditions related to tobacco use among American Indian communities, which ultimately led to high tobacco use rates (Dino et al., 2001; Schinke et al., 1996).
Most of these interventions also included themes that encompassed unifying minority experiences, such as acculturative stress, discrimination, family conflicts that can occur during the acculturation process, and increased emphasis on group identity and cohesion rather than individual efforts.
Another theme integrated in culturally tailored intervention was parental involvement (Elder et al., 2002; Guilamo-Ramos et al., 2010; Horn et al., 2005; Johnson et al., 2005; Kaufman et al., 1994). Parental influence has shown to be effective in reducing tobacco use in adolescents (den Exter Blokland, Engels, Hale Iii, Meeus, & Willemsen, 2004), including those from minority groups by expressing disapproval of smoking (Kong et al., 2012) and through engaging in effective communication about tobacco use and implementing antismoking rules at home (Clark, Scarisbrick-Hauser, Gautam, & Wirk, 1999; Skinner, Haggerty, & Catalano, 2009). For example, Guilamo-Ramos et al. (2010) added parental involvement to TNT; specially, mothers of African American and Hispanic adolescents in this group were taught communication and monitoring strategies for preventing adolescent tobacco use.
Theoretical Framework
The theoretical construct that underlay all interventions was psychosocial (see Table 2). Six (46%; Elder et al., 2002; Guilamo-Ramos et al., 2010; Joffe et al., 2009; Johnson et al., 2005; Kaufman et al., 1994; Rice et al., 2010) were based on social influence model (SI) and addressed short- and long-term social and health consequences of smoking, social norms, refusal and social skills training using modeling, role plays, and group practices. Project TNT (Sussman et al., 1995) is an example of an intervention based on SI; it is composed of three sections: basic information (engage adolescents in the treatment and present information on the consequences of substance use), normative social influence lessons (address social pressures to use substances), and informational social influence lessons (challenge favorable opinions about substance use shared among peers). Two (15%) studies have modified Project TNT: Rice et al. (2010) culturally tailored Project TNT for Arab American youth by offering the program in both Arabic and English and also used Middle Eastern figures in the counseling materials. Sun et al. (2007) enhanced Project TNT by adding enjoyable components for teens including a talk show game and yoga to increase motivation and personal commitment to quitting smoking. Although the enhancement was not culture specific, they implemented this intervention in predominantly Hispanic adolescent sample.
Four (31%; Horn et al., 2005; Joffe et al., 2009; Ma et al., 2004; Prokhorov et al., 2008) were based on social cognitive theory (SCT) and included a variety of smoking cessation skills, such as stimulus control, social skills, relapse prevention, nicotine withdrawal, stress and weight management, and strategies to deal with family and peer pressure (Dino et al., 2001; Dino, Horn, Zedosky, & Monaco, 1998). Additional skills included setting goals for change, monitoring progress, and self-reinforcement. The N-O-T program, a gender-specific, school-based program with an overall EOT quit rate of 26% is an example of intervention based on SCT (Horn & Dino, 2009).
Two (15%; Albrecht et al., 1998; Botvin et al., 1992) were based on cognitive behavioral theory (CBT) and included psychoeducation on the consequences of smoking and addictive nature of smoking and skill building, such as problem solving, decision making, anxiety management, and self-control. In addition to these skills, the two CBT interventions differed in that Albrecht et al. (1998) included a peer component and Botvin et al. (1992) included social resistance skills training.
Prokhorov et al. (2010) developed a computer-based program called ASPIRE (A Smoking Prevention Interactive Experience), which combined SCT with Transtheoretical Model of Change (TTM; Prochaska & DiClemente, 1983). TTM focuses on changing motivation to reduce smoking through movement in a series of five stages: precontemplation, contemplation, preparation, action, and maintenance (Velicer, Norman, Fava, & Prochaska, 1999). Finally, Schinke et al. (1996) used psychosocial approach in their tobacco curriculum but did not specify which theoretical modality.
Treatment Outcomes
The definition of treatment outcome varied depending on the type of study; cessation studies defined it as abstinence or reduction of smoking and prevention studies as initiation of smoking. The self-reported questions used to assess smoking behaviors included, lifetime smoking (i.e., “ever tried cigarettes”), smoking in the past 30 days, susceptibility to smoking, smoking in the past week/day, current smoking, and quitting smoking. Only two (15%) studies validated self-reported abstinence with biochemical tests using expired-air carbon monoxide (CO) breath test (Albrecht et al., 1998) and cotinine levels (Joffe et al., 2009).
Table 3 presents a summary of major treatment outcomes. Overall, culturally tailored tobacco prevention interventions yielded lower tobacco initiation rates among all adolescents compared with their respective control or standard conditions, but for the most part, culturally tailored tobacco cessation interventions did not yield higher abstinence rates than control/standard-care conditions; the exception was the culturally tailored intervention conducted by Johnson et al. (2005), who observed that the culturally tailored intervention lowered the risk for past month smoking among smokers. Although cessation rates did not differ between intervention and control groups in most studies, changes in other smoking-related behaviors were noted. For instance, Ma et al. (2004) compared standard care (SC) curriculum (N-O-T program) with culturally sensitive ACT program, and the EOT results yielded 0% quit rate in the ACT group and 22.2% quit rate in the SC group, and these rates did not improve at follow-up. Despite the lack of between-group differences in the abstinence outcomes, the participants in the ACT condition reported greater reduction of cigarette smoking and higher ability to quit compared with those in the SC group. Additionally, Horn et al.’s (2005) enhanced N-O-T program for American Indian adolescents, compared with a 15-min brief intervention control group, did not produce a higher quit rate. However, the intervention condition yielded a stronger intervention effect size for males and reduced smoking among all adolescents who did not quit smoking.
Discussion
In this review, we have summarized and discussed tobacco prevention and cessation interventions that were targeted and tailored to minority adolescents. We observed that although culturally tailored prevention interventions appeared to reduce the tobacco use initiations rates among all adolescents, culturally tailored cessation interventions did not appear to produce a similar effect. While more research needs to be conducted in this area, this lack of efficacy could be due to several reasons; first, using absolute abstinence as a treatment outcome among adolescents, and in particular minority adolescent smokers, may be too stringent. The measure of dichotomous abstinence has been adapted from the adult literature, and smoking patterns among adolescents vary from adult smoking patterns in both rates and frequencies (Mermelstein et al., 2002). Adolescents have more external restraints put on their smoking behaviors from authority figures at home and at school, and therefore, their smoking behavior is less regimented and stable. Other measures of treatment outcome that can capture subtle changes in smoking behaviors, such as number of cigarettes smoked per day and number of days abstinent should be used to determine treatment outcome (Mermelstein et al., 2002). This issue may be even more relevant among minority adolescent smokers where cigarette smoking patterns differ from White adolescents. Consistent with this notion, although the tobacco cessation interventions that we examined did not yield higher abstinence rates than the control interventions, they influenced other important outcomes such as greater reduction in smoking and ability to quit.
Second, the definition of cultural tailoring may need to be expanded from our current understanding. Other important factors that may affect the smoking behaviors of minority adolescents, such as the level of acculturation, ethnic identity, and perceived discrimination, may need to be considered; these are complex factors that are influenced by broader structural systems such as the racial/ethnic composition of the school and the neighborhood. For example, Johnson et al.’s (2005) Project FLAVOR lowered the risk of smoking for all adolescents, but the effect was greater among Hispanic students in predominantly Hispanic schools compared with Hispanic students in predominantly Asian/multicultural schools. Additionally, Prokhorov et al.’s (2008) ASPIRE program that targeted both nonsmoking and smoking African American and Hispanic adolescents showed that although all adolescents were less likely to initiate smoking at the follow-up assessment, this effect was stronger among less-acculturated Hispanic adolescents, indicating that this intervention may not be equally effective for all minority groups. These study findings suggest that factors such as the racial/ethnic composition of the schools and levels of acculturation of minority students may moderate treatment outcomes and need to be examined in future research.
Interestingly, and appropriately, all the studies included in this review took place in diverse ethnic/racial populations or in geographic locations with high concentration of minority populations. Although minority adolescents who live in these areas are important to target, minority smokers who live in locations in which they are truly a minority population should also be examined.
Existing research indicates that when the balance shifts from Whites being the numerical majority to minority, factors such as higher ethnic pride that are known to protect minority adolescents from substance use may also protect White adolescents (Marsiglia, Kulis, Hecht, & Sills, 2004), suggesting that regardless of ethnicity/race, when an individual is the numerical minority in school or other community locations, their sense of self may develop differently because they have to negotiate their sense of minority membership within the majority culture. Specific to tobacco use, we have shown that among racial/ethnic minority adolescents in a suburban high school (where they are the numerical minority), having high ethnic pride heightened the protective effect against smoking behaviors (Kong et al., 2012). Given the evidence that tobacco interventions may work differently depending on the ethnic/racial composition of the school, the level of acculturation and ethnic identity of minority adolescents, incorporating culturally targeted and tailored tobacco interventions into the mainstream culture in diverse geographic locations may be important.
Our review also points to specific areas in the field of adolescent tobacco intervention that needs further development and research. For instance, a recent comprehensive review of 64 adolescent smoking cessations studies showed that only 27 (42%) studies even reported ethnicity of subjects (Sussman & Sun, 2009). Even in this present review where smoking interventions targeted 50% or greater minority adolescents, three (23%; Joffe et al., 2009; Prokhorov et al., 2008; Sun et al., 2007) did not take into account culture specific values. These evidence indicate that although developing culturally sensitive tobacco intervention is a long-term goal, perhaps, the first viable goal is to start collecting more specific information like ethnicity/race, and other cultural values such as level of acculturation to begin to assess whether these programs are generalizable to ethnic/racial minority adolescents and whether culturally tailoring would improve intervention effects. Another area for future research is tailoring tobacco interventions for African American youth; much to our surprise, there were few tobacco interventions for African American youth. This is surprising, given that the majority of culturally sensitive tobacco cessation interventions for adults were aimed at African Americans (Lawrence, Graber, Mills, Meissner, & Warnecke, 2003). Only one study (Kaufman et al., 1994) in this review tailored the intervention to adolescents in African American community. In order to better understand possible surface and deep structural changes that can be applied to tobacco interventions for African American adolescents, examining culturally tailored interventions to address other risky behaviors among African American youth may be informative. For example, The Aban Aya Youth Project (Flay, Graumlich, Segawa, Burns, & Holliday, 2004), a prevention program for violence and substance use, incorporated cultural themes of self and cultural pride and family and community ties through storytelling and proverbs drawn from African and African American history and literature and homework assignments involving parents. Another drug prevention program targeting African American girls (Corneille, Ashcraft, & Belgrave, 2005) included cultural component that emphasized Afrocentric values, such as a sense of communalism and collectiveness, spirituality and connectedness to the past and future, as well as issues surrounding race and gender. These values were reinforced through team building and problem solving activities as well as music, poetry, and dance. Taken from the adult literature, Kick It! Program (Resnicow et al., 1997), a self-help smoking prevention program developed for African American adult smokers used video stories about African American smokers as well as examples from Black history (e.g., Marcus Garvey, Martin Luther King, Malcolm X) to motivate quitting smoking. These cultural components can be used as an initial guide to begin developing culturally tailored tobacco interventions for African American youth.
This study summarized major components of tobacco prevention and cessation interventions for minority youth with the goal of developing a better understanding of cultural and other associated factors that may lead to more effective intervention to reduce tobacco rates for all adolescents. The advantage of this study is broad inclusion criteria that allowed us to examine diverse studies in regards to study design, sample sizes, treatment formats, control groups, outcome measures, and periods of follow-up. However, the disadvantage is the difficulty unifying these differences by directly comparing treatment outcomes. Therefore, we cannot determine whether culturally tailoring would improve the efficacy of the smoking interventions for minority adolescents. More studies with well-controlled designs that either take or do not take into consideration the cultural needs of the population need to be conducted to determine whether culturally enhanced smoking interventions would be more effective for minority adolescents. Despite this disadvantage, the narrative description of the study findings, including treatment outcome, may help researchers detect areas that need further research.
In conclusion, the path to the development of effective culturally sensitive tobacco prevention and cessation interventions is at a nascent stage and still faces many challenges. In the past two decades, the efforts to develop culturally sensitive tobacco interventions for minority youth has gained some momentum, but much more work needs to be done in this area. Most importantly, complex and yet critical culture specific factors, such as heterogeneity of tobacco products used, cultural beliefs associated with tobacco use and cessation, and within group differences, need to be studied and incorporated into such interventions.
Funding
This work was supported by the National Institute on Drug Abuse at the National Institutes of Health (T32 DA07238 to GK and P50 DA09421, R01 DA0264 to SK).
Declaration of Interests
All authors have no conflict of interest.
References
- Albrecht S, Payne L, Stone CA, Reynolds MD. A preliminary study of the use of peer support in smoking cessation programs for pregnant adolescents. Journal of the American Academy of Nurse Practitioners. 1998;10:119–125. doi: 10.1111/j.1745-7599.1998.tb01205.x. doi:10.1111/j.1745-7599.1998.tb01205.x. [DOI] [PubMed] [Google Scholar]
- Appleyard J, Messeri P, Haviland ML. Smoking among Asian American and Hawaiian/Pacific Islander youth: Data from the 2000 National Youth Tobacco Survey. Asian American and Pacific Islander Journal of Health. 2001;9:5–14. [PubMed] [Google Scholar]
- Botvin GJ, Dusenbury L, Baker E, James-Ortiz S, Botvin EM, Kerner J. Smoking prevention among urban minority youth: Assessing effects on outcome and mediating variables. Health Psychology. 1992;11:290–299. doi: 10.1037//0278-6133.11.5.290. doi:10.1037//0278-6133.11.5.290. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. High school students who tried to quit smoking cigarettes—United States, 2007. Morbidity & Mortality Weekly Report. 2009;58:428–431. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5816a4.htm. [PubMed] [Google Scholar]
- Christakis DA, Garrison MM, Ebel BE, Wiehe SE, Rivara FP. Pediatric smoking prevention interventions delivered by care providers: A systematic review. American Journal of Preventive Medicine. 2003;25:358–362. doi: 10.1016/s0749-3797(03)00214-9. doi:10.1016/S0749-3797(03)00214-9. [DOI] [PubMed] [Google Scholar]
- Clark PI, Scarisbrick-Hauser A, Gautam SP, Wirk SJ. Anti-tobacco socialization in homes of African-American and white parents, and smoking and nonsmoking parents. Journal of Adolescent Health. 1999;24:329–339. doi: 10.1016/s1054-139x(98)00117-7. doi:10.1016/s1054-139x(98)00117-7. [DOI] [PubMed] [Google Scholar]
- Corneille MA, Ashcraft AM, Belgrave FZ. What's culture got to do with it? Prevention programs for African American adolescent girls. Journal of Health Care for the Poor and Underserved. 2005;16:38–47. doi: 10.1353/hpu.2005.0109. doi:10.1353/hpu.2005.0109. [DOI] [PubMed] [Google Scholar]
- Davis SM, Lambert BS, Cunningham-Sabo L, Skipper BJ. Tobacco use: Baseline results from Pathways to Health, a school-based project for southwestern American Indian youth. Preventive Medicine. 1995;24:454–460. doi: 10.1006/pmed.1995.1073. doi:10.1006/pmed.1995.1073. [DOI] [PubMed] [Google Scholar]
- den Exter Blokland EAW, Engels RCME, Hale Iii WW, Meeus W, Willemsen MC. Lifetime parental smoking history and cessation and early adolescent smoking behavior. Preventive Medicine. 2004;38:359–368. doi: 10.1016/j.ypmed.2003.11.008. doi:10.1016/j.ypmed.2003.11.008. [DOI] [PubMed] [Google Scholar]
- DiFranza JR, Savageau JA, Rigotti NA, Fletcher K, Ockene JK, McNeill AD, et al. Development of symptoms of tobacco dependence in youths: 30 month follow up data from the DANDY study. Tobacco Control. 2002;11:228–235. doi: 10.1136/tc.11.3.228. doi:10.1136/tc.11.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dino GA, Horn KA, Goldcamp J, Maniar SD, Fernandes A, Massey CJ. Statewide demonstration of Not on Tobacco: A gender-sensitive teen smoking cessation program. Journal of School Nursing. 2001;17:90–97. doi: 10.1177/105984050101700206. doi:doi:10.1177/105984050101700206. [DOI] [PubMed] [Google Scholar]
- Dino GA, Horn KA, Zedosky L, Monaco K. A positive response to teen smoking: Why N-O-T? NASSP Bulletin. 1998;82(601):46–58. doi:10.1177/019263659808260106. [Google Scholar]
- Elder JP, Litrownik AJ, Slymen DJ, Campbell NR, Parra-Medina D, Choe S, et al. Tobacco and alcohol use-prevention program for Hispanic migrant adolescents. American Journal of Preventive Medicine. 2002;23:269–275. doi: 10.1016/s0749-3797(02)00515-9. doi:10.1016/s0749-3797(02)00515-9. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Orlando M, Tucker JS, Klein DJ. From adolescence to young adulthood: Racial/ethnic disparities in smoking. American Journal of Public Health. 2004;94:293–299. doi: 10.2105/ajph.94.2.293. doi:10.2105/AJPH.94.2.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flay BR, Graumlich S, Segawa E, Burns JL, Holliday MY. Effects of 2 prevention programs on high-risk behaviors among African American youth: A randomized trial. Archives of Pediatrics & Adolescent Medicine. 2004;158:377–384. doi: 10.1001/archpedi.158.4.377. doi:10.1001/archpedi.158.4.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett BE, Dube SR, Trosclair A, Caraballo RS, Pechacek TF. Cigarette smoking—United States, 1965–2008. Morbidity & Mortality Weekly Report. 2011;60:109–113. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/su6001a24.htm. [PubMed] [Google Scholar]
- Garrison MM, Christakis DA, Ebel BE, Wiehe SE, Rivara FP. Smoking cessation interventions for adolescents: A systematic review. American Journal of Preventive Medicine. 2003;25:363–367. doi: 10.1016/s0749-3797(03)00213-7. doi:10.1016/S0749-3797(03)00213-7. [DOI] [PubMed] [Google Scholar]
- Griesler PC, Kandel DB. Ethnic differences in correlates of adolescent cigarette smoking. Journal of Adolescent Health. 1998;23:167–180. doi: 10.1016/s1054-139x(98)00029-9. doi:10.1016/s1054-139x(98)00029-9. [DOI] [PubMed] [Google Scholar]
- Guilamo-Ramos V, Jaccard J, Dittus P, Gonzalez B, Bouris A, Banspach S. The Linking Lives health education program: A randomized clinical trial of a parent-based tobacco use prevention program for African American and Latino youths. American Journal of Public Health. 2010;100:1641–1647. doi: 10.2105/AJPH.2009.171637. doi:10.2105/ajph.2009.171637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn K, McGloin T, Dino G, Manzo K, McCracken L, Shorty L, et al. Quit and reduction rates for a pilot study of the American Indian Not On Tobacco (N-O-T) program. Preventing Chronic Disease. 2005;2:A13. [PMC free article] [PubMed] [Google Scholar]
- Horn KA, Dino G. A comparative review of the effectiveness trial of N-O-T in Alabama: Guideposts for future research. American Journal of Health Education. 2009;40:47–55. [Google Scholar]
- Joffe A, McNeely C, Colantuoni E, An M, Wang W, Scharfstein D. Evaluation of school-based smoking-cessation interventions for self-described adolescent smokers. Pediatrics. 2009;124:e187–e194. doi: 10.1542/peds.2008-2509. doi:10.1542/peds.2008-2509. [DOI] [PubMed] [Google Scholar]
- Johnson CA, Unger JB, Ritt-Olson A, Palmer PH, Cen SY, Gallaher P, et al. Smoking prevention for ethnically diverse adolescents: 2-year outcomes of a multicultural, school-based smoking prevention curriculum in Southern California. Preventive Medicine. 2005;40:842–852. doi: 10.1016/j.ypmed.2004.09.032. doi:10.1016/j.ypmed.2004.09.032. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Kiros G, Schaffran C, Hu M. Racial/ethnic differences in cigarette smoking initiation and progression to daily smoking: A multilevel analysis. American Journal of Public Health. 2004;94:128–135. doi: 10.2105/ajph.94.1.128. doi:10.2105/AJPH.94.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman JS, Jason LA, Sawlski LM, Halpert JA. A comprehensive multi-media program to prevent smoking among black students. Journal of Drug Education. 1994;24:95–108. doi: 10.2190/6NAN-696P-HD0J-9GG9. doi:10.2105/AJPH.94.1.128. [DOI] [PubMed] [Google Scholar]
- Kong G, Camenga D, Cavallo D, Connell CM, Pflieger JC, Krishnan-Sarin S. The role of ethnic pride and parental disapproval of smoking on smoking behaviors among minority and white adolescents in a suburban high school. American Journal on Addictions. 2012;21:424–434. doi: 10.1111/j.1521-0391.2012.00266.x. doi:10.1111/j.1521-0391.2012.00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence D, Graber JE, Mills SL, Meissner HI, Warnecke R. Smoking cessation interventions in U.S. racial/ethnic minority populations: An assessment of the literature. Preventive Medicine. 2003;36:204–216. doi: 10.1016/s0091-7435(02)00023-3. doi:10.1016/s0091-7435(02)00023-3. [DOI] [PubMed] [Google Scholar]
- Levinson AH, Pérez-Stable EJ, Espinoza P, Flores ET, Byers TE. Latinos report less use of pharmaceutical aids when trying to quit smoking. American Journal of Preventive Medicine. 2004;26:105–111. doi: 10.1016/j.amepre.2003.10.012. doi:10.1016/j.amepre.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Tan Y, Thomas P, Man VL. Development of a culturally appropriate smoking cessation program for Chinese-American youth. Journal of Adolescent Health. 2004;35:206–216. doi: 10.1016/j.jadohealth.2003.09.013. doi:10.1016/j.jadohealth.2003.09.013. [DOI] [PubMed] [Google Scholar]
- Marsiglia FF, Kulis S, Hecht ML, Sills S. Ethnicity and ethnic identity as predictors of drug norms and drug use among preadolescents in the US Southwest. Substance Use and Misuse. 2004;39:1061–1094. doi: 10.1081/ja-120038030. doi:10.1081/ja-120038030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mermelstein R, Colby SM, Patten C, Prokhorov A, Brown R, Myers M, et al. Methodological issues in measuring treatment outcome in adolescent smoking cessation studies. Nicotine & Tobacco Research. 2002;4:395–403. doi: 10.1080/1462220021000018470. doi:10.1080/1462220021000018470. [DOI] [PubMed] [Google Scholar]
- Pasick RJ, D’Onofrio CN, Otero-Sabogal R. Similarities and differences across cultures: Questions to inform a third generation for health promotion research. Health Education Quarterly. 1996;23:S142–S161. [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. doi:10.1037//0022-006X.51.3.390. [DOI] [PubMed] [Google Scholar]
- Prokhorov AV, Kelder SH, Shegog R, Murray N, Peters R, Agurcia-Parker C, et al. Impact of A Smoking Prevention Interactive Experience (ASPIRE), an interactive, multimedia smoking prevention and cessation curriculum for culturally diverse high-school students. Nicotine & Tobacco Research. 2008;10:1477–1485. doi: 10.1080/14622200802323183. doi:10.1080/14622200802323183. [DOI] [PubMed] [Google Scholar]
- Prokhorov AV, Kelder SH, Shegog R, Conroy JL, Murray N, Peters R, et al. Project ASPIRE: An interactive, multimedia smoking prevention and cessation curriculum for culturally diverse high school students. Substance Use & Misuse. 2010;45:983–1006. doi: 10.3109/10826080903038050. doi:10.3109/10826080903038050. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Braithwaite R, Ahluwalia J, Baranowski T. Cultural sensitivity in public health: Defined and demystified. Ethnicity and Disease. 1999;9:10–21. [PubMed] [Google Scholar]
- Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J. Cultural sensitivity in substance use prevention. Journal of Community Psychology. 2000;28:271–290. doi:10.1002/(sici)1520-6629(200005)28:3<271::aid-jcop4>3.0.co;2-i. [Google Scholar]
- Resnicow K, Vaughan R, Futterman R, Weston RE, Royce J, Parms C, et al. A self-help smoking cessation program for inner-city African Americans: Results from the Harlem Health Connection Project. Health Education and Behavior. 1997;24:201–217. doi: 10.1177/109019819702400208. doi:10.1177/109019819702400208. [DOI] [PubMed] [Google Scholar]
- Rice VH, Weglicki LS, Templin T, Jamil H, Hammad A. Intervention effects on tobacco use in Arab and non-Arab American adolescents. Addictive Behaviors. 2010;35:46–48. doi: 10.1016/j.addbeh.2009.07.005. doi:10.1016/j.addbeh.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schinke SP, Singer B, Cole K, Contento IR. Reducing cancer risk among Native American adolescents. Preventive Medicine. 1996;25:146–155. doi: 10.1006/pmed.1996.0040. doi:10.1006/pmed.1996.0040, [DOI] [PubMed] [Google Scholar]
- Skinner ML, Haggerty KP, Catalano RF. Parental and peer influences on teen smoking: Are White and Black families different? Nicotine & Tobacco Research. 2009;11:558–563. doi: 10.1093/ntr/ntp034. doi:10.1093/ntr/ntp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun P, Miyano J, Rohrbach LA, Dent CW, Sussman S. Short-term effects of Project EX-4: A classroom-based smoking prevention and cessation intervention program. Addictive Behaviors. 2007;32:342–350. doi: 10.1016/j.addbeh.2006.05.005. doi:10.1016/j.addbeh.2006.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S. Effects of sixty six adolescent tobacco use cessation trials and seventeen prospective studies of self-initiated quitting. Tobacco Induced Diseases. 2002;1:35–81. doi: 10.1186/1617-9625-1-1-35. doi:10.1186/1617-9625-1-1-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, Dent CW, Burton D, Stacy AW, Flay BR. Developing school-based tobacco use prevention and cessation programs. Thousand Oaks, California: Sage Publication; 1995. [Google Scholar]
- Sussman S, Miyano J, Rohrbach LA, Dent CW, Sun P. Six-month and one-year effects of Project EX-4: A classroom-based smoking prevention and cessation intervention program. Addictive Behaviors. 2007;32:3005–3014. doi: 10.1016/j.addbeh.2007.06.016. doi:10.1016/j.addbeh.2007.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, Sun P. Youth tobacco use cessation: 2008 update. Tobacco Induced Diseases. 2009;5(1):3. doi: 10.1186/1617-9625-5-3. doi:10.1186/1617-9625-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger JB, Chou C, Palmer PH, Ritt-Olson A, Gallaher P, Cen S. Project FLAVOR: 1-year outcomes of a multicultural, school-based smoking prevention curriculum for adolescents. American Journal of Public Health. 2004;94:263–265. doi: 10.2105/ajph.94.2.263. doi: 10.2105/AJPH.94.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer WF, Norman GJ, Fava JL, Prochaska JO. Testing 40 predictions from the transtheoretical model. Addictive Behaviors. 1999;24:455–469. doi: 10.1016/s0306-4603(98)00100-2. doi:10.1016/S0306-4603(98)00100-2. [DOI] [PubMed] [Google Scholar]
- Wiehe SE, Garrison MM, Christakis DA, Ebel BE, Rivara FP. A systematic review of school-based smoking prevention trials with long-term follow-up. Journal of Adolescent Health. 2005;36:162–169. doi: 10.1016/j.jadohealth.2004.12.003. doi:10.1016/j.jadohealth.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. New England Journal of Medicine. 2002;347:1585–1592. doi: 10.1056/NEJMsa012979. doi:10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- Zhu S.-H., Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance: A population-based analysis. American Journal of Preventive Medicine. 2000;18:305–311. doi: 10.1016/s0749-3797(00)00124-0. doi:10.1016/s0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]


