Abstract
Objective
Parents who overestimate their child’s physical activity (PA) level may not encourage their children to increase their PA. We assessed parental awareness of child PA, and investigated potential correlates of overestimation.
Method
Child PA (accelerometer) and parent-classified child PA [‘active’ ≥ 60mins/day vs. ‘inactive’ <60mins/day moderate and vigorous PA (MVPA)] were measured over 7 days [n=329, 44% male, 39% Latino; Mean (SD) 9.1 (0.7) yrs] in an obesity prevention study in San Diego (Project MOVE). Agreement between date-matched objective MVPA and parent-classified child PA was assessed; % days parental overestimation was the outcome variable. Associations between parental overestimation and potential correlates were investigated using three-level mixed effects linear regression.
Results
Children met PA guidelines on 43% of days. Parents overestimated their children’s PA on 75% of days when children were inactive. Most parents (80%) overestimated their child’s PA on ≥1 measurement day. Parental support for child PA (transport, encouragement and participation with child) (p<0.01) was positively associated with higher overestimation. Parents of girls showed more overestimation than parents of boys (p=0.01).
Conclusion
Most parents incorrectly classified their child as active when their child was inactive. Strategies addressing parental overestimation may be important in PA promotion.
Keywords: physical activity, parental awareness, children, child behavior, overestimation
Introduction
Insufficient physical activity (PA) is a risk factor for obesity in children (Wareham et al., 2005, Steele et al., 2008). Only 42% of US children aged 6–11 meet PA guidelines which are ≥60 minutes of moderate and vigorous PA (MVPA) every day (Troiano et al., 2008). Literature reviews highlight the limited success of PA interventions in children (Salmon et al., 2007, van Sluijs et al., 2007, Dobbins et al., 2009); however the reasons for this are largely unknown.
One possible explanation for the limited effectiveness of PA interventions is that individuals overestimate their PA level, believing themselves to be more active than they really are. This misperception is common for PA (van Sluijs et al., 2007, Ronda et al., 2001, Lechner et al., 2006, Corder et al., 2010, Corder et al., 2011, Watkinson et al., 2010), due to unclear thresholds between healthy and unhealthy PA levels (Ronda et al., 2001). Someone overestimating their PA level may not be aware that they are not optimally active and may see no need to increase their PA level (Ronda et al., 2001). Improving PA awareness by reducing overestimation of PA levels may be an important component of PA promotion. Few interventions address this as a key strategy (van Sluijs et al., 2007, Ronda et al., 2001) although it has been considered in recent interventions in adults (van Stralen et al., 2010).
Parents strongly influence the PA of their children, and usually have primary responsibility for their participation in PA promotion (Giles-Corti et al., 2009). Investigation of parental awareness of child PA levels is important as parents may need to be aware that their children are insufficiently active in order to facilitate their participation in PA promotion (Corder et al., 2010).
To our knowledge, parental awareness of child PA has not been investigated among US or ethnically diverse children and parents. Previous studies have used one habitual PA awareness question to define overestimation (van Sluijs et al., 2007, Ronda et al., 2001, Lechner et al., 2006, Corder et al., 2010, Corder et al., 2011, Watkinson et al., 2010). This is the first study to derive parental overestimation using daily awareness data, allowing for daily variation in children’s PA.
We investigated parental awareness of child PA levels among parents of 7–10 year-old children, and explored correlates of parental overestimation.
Methods
Study design and setting
Children (5 to 8 years-old) and their primary caregivers (n=541 dyads) living in San Diego County were recruited between November 2006 and May 2008 to participate in Project MOVE, a 2-year obesity prevention study involving recreation centers. Families were contacted through phone calls, fliers and community information booths. Parent-child dyads lived within 1.75 miles from one of 30 participating recreation centers and parents could speak and read English or Spanish. Parents provided written informed consent and children provided oral assent. Ethical approval from San Diego State University Institutional Review Board was obtained. Post-intervention data were used here (children 7–10 years-old) as accelerometer data were available for the majority of participating children.
At baseline and post-intervention measurement sessions, parents completed a questionnaire, and child and parent anthropometric measures were taken. Parents reported demographics for themselves and their child including: age, gender, Latino ethnicity, family monthly income (<$500–$2000, $2001–$3500, $3501–$5000 and ≥$5001) and parent education (middle school or less through post-graduate). Height (Shorr Measuring Height Board) and weight (SECA 880 and 876) were assessed using standard procedures by trained staff to the nearest 0.1 cm and 0.1 kg, respectively. Body mass index (BMI) z-scores were calculated (Center for Disease Control and Prevention, 2000).
Physical activity
At post-intervention, PA was assessed using Actigraph accelerometers (Ekelund et al., 2003, Ekelund et al., 2001). All children agreeing to wear a monitor (n=370) were fitted with a GT3X or GT1M (recording in 5-second epochs), and asked to wear the monitors for 7 days while awake and to remove them for water-based activities. Accelerometry data were analyzed using a program available at http://www.mrc-epid.cam.ac.uk/Research/Programmes/Programme_5/InDepth/Programme%205_Disclaimer.html to remove: data recorded between 11 pm and 6 am, periods of ≥30 minutes with continuous zero counts and days with <540 minutes of recording (valid day cut-off).
Time (min/d) spent in MVPA was derived using age specific cut-points (Trost et al., 2005). Accelerometer data were used to derive a dichotomous MVPA variable; 60 min/day of MVPA was used to classify children as active or inactive, according to current PA guidelines (US Department of Health and Human Services, 2008). “Classification error” was calculated as daily child MVPA (mins) minus 60 mins (current guidelines). Seven categories of time in MVPA were calculated in 15 minute blocks (from zero to ≥90 minutes) to examine the distribution of PA levels with regard to parental overestimation.
Parental awareness of child PA
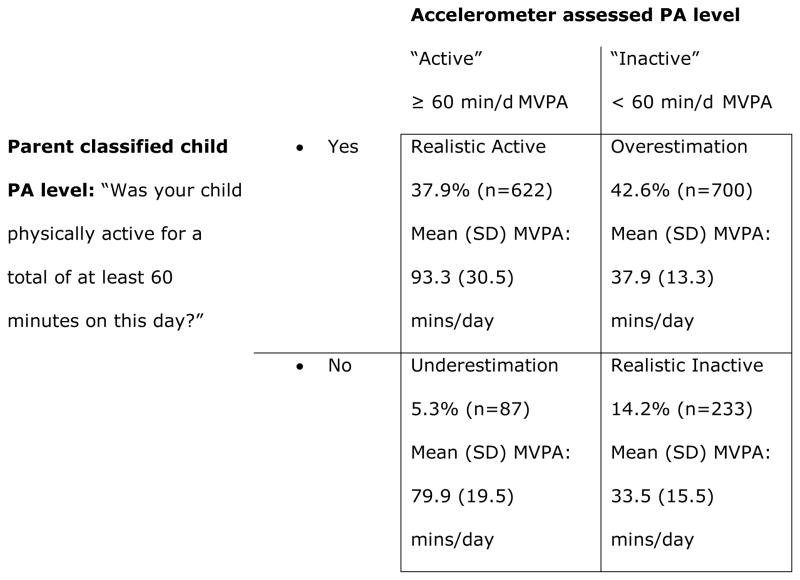
Parental awareness of child PA level was assessed through a daily diary, concurrent with accelerometer measurement, asking the parent: “was your child physically active for a total of at least 60 minutes on this day” with answer categories as “yes” and “no”. For each day with valid PA and awareness data, parent-child dyads were categorized into one of four groups using objective and parent-classified PA (Figure 1). The outcome variable for this analysis was “parental overestimation”, expressed as the percentage of measured days on which parents overestimated their child’s PA level (number of days of parental PA overestimation divided by the number of days with valid matched data). Only one child per parent was enrolled in the study and parents were asked to respond to all surveys for that child only. A sensitivity analysis was done using 45 minutes as the threshold between active and inactive.
Figure 1.
Derivation of parental overestimation (N=1642 measurement days) by comparison of parent rated child PA levels and accelerometer assessed PA levels among 329 children and parents from San Diego County, CA. MVPA; moderate and vigorous PA, min/d; minutes per day.
Potential correlates
Potential correlates of overestimation were parentally reported at follow-up (except baseline values for sex, ethnicity, income and parental education). Cronbach’s alpha was computed to determine the internal consistency of items where appropriate.
Two questions asked parents how many days/week their child plays team and non-team sports with eight responses options (0 to 7 days/week): a sum of both questions was used to represent sessions/week that the child does sport.
Parents reported the presence of eight PA-related rules, including “do not go places alone” (ICC=0.42 to 0.74) (Kerr et al., 2008). Responses were “yes”, “no” and “sometimes” with “no” and “sometimes” combined given that if a rule is only ‘sometimes’ present it is unlikely to be enforced.
Parents reported how often they provide encouragement and transport for their child to do PA, and how often they do PA with their child. Response options were “never”, “< once/week”, “1–2 times/week”, “3–4 times/week” and “5–7 times/week” recoded as 0, 1.5, 3.5 and 6 days/week. Parent support for less sedentary time was derived from two questions “to help children think of ways to be less inactive” and “encouraging less inactive time” with responses as above (α=0.79).
Parents reported electronic media items in the child’s bedroom was adapted from a published scale (Rosenberg et al., 2010) (previously reported ICC=0.90). Parents reported the number of types of PA equipment at home (range 0–8) using an adapted scale (original reliability ICC=0.80) (Rosenberg et al., 2010).
Parents selected the frequency of their child’s PA participation at 11 locations (including recreation centers and parks), response categories were never, <once/week, 1–2 times/week, 3–4 times/week and 5–7 times/week (recoded as 0, 1.5, 3.5 and 6 days/week). These have been reported previously (original reliability ICC=0.60 to 0.89) (Kerr et al., 2008). Two composite variables were derived: locations used frequently (sum of locations used ≥1–2 times/week) and total weekly visits to any location (times/week) (Corder et al., 2011).
Statistical Analyses
Characteristics of those included and excluded from the analyses were tested using t-tests or chi-squared tests.
Simple associations between parental overestimation and potential correlates were assessed using three-level mixed effects linear regression with levels as days, children and recreation center recruitment area. Analyses were additionally adjusted for sex, study condition and classification error. Classification error was included as a covariate so results are independent of child MVPA and proximity to the guideline threshold. This also takes into account that overestimation depends on PA levels. Study condition was adjusted for but intervention effects were not assessed. Variables that reached p ≤ 0.10 in the simple models were included in a multiple model and subsequently removed if p ≥ 0.05, variables were removed stepwise, starting with the highest p-value. Stata 12.0 (Statacorp, College Station, TX) was used for analyses.
Results
Of the 541 Project MOVE parent-child dyads, 329 had at least one matched day of objective and parent-classified PA data (mean(SD) 5.0(1.9) days); descriptive data are presented in Table 1. There were no significant differences by sex, parent education, ethnicity, age or BMI z-score between Project MOVE children excluded and included from these analyses (all p>0.05).
Table 1.
Descriptive data for 329 parent-child dyads from San Diego County, CA with data on parental estimation of child PA and results of simple three-level linear regression for associations with parental overestimation (% days parental overestimation).
| Variable | Mean (SD) or % | B | (95% CI) | P value# |
|---|---|---|---|---|
| Sex (% boys) | 44.1 | Reference category | ||
| Sex (% girls) | 55.9 | 6.0 | (0.3, 11.8) | 0.04 |
| Age (years) | 9.1 (0.7) | 3.8 | (−0.1, 7.7) | 0.06 |
| BMI z-score | 0.6 (−2.6, 2.8) | 1.7 | (−1.2, 4.7) | 0.25 |
| * Ethnicity (% non-Latino) | 61.4 | Reference category | ||
| * Ethnicity (% Latino) | 38.6 | −2.7 | (−8.5, 3.2) | 0.38 |
| * Monthly Income (% parents) | ||||
| $0–$2,000 | 22.1 | Reference category | ||
| $2,001–$3,500 | 20.1 | −1.7 | (−10.8, 7.4) | 0.72 |
| $3,501–$5,000 | 22.5 | −3.8 | (−12.6, 5.0) | 0.39 |
| $5,001+ | 35.3 | −0.2 | (−8.1, 7.8) | 0.97 |
| * Parental education (% parents) | ||||
| Middle school or less | 15.5 | Reference category | ||
| High school | 13.7 | −0.1 | (−10.6, 10.6) | 0.99 |
| Some college but not graduated | 26.1 | −0.3 | (−9.4, 8.8) | 0.95 |
| College Graduate | 26.8 | −3.4 | (−12.4, 5.7) | 0.47 |
| Post-graduate work | 17.9 | −4.2 | (−14.1, 5.7) | 0.41 |
| MVPA (mins/day) | 59.4 (25.8) | |||
| Classification error (MVPA mins/day) | −0.6 (25.8) | −0.4 | (−0.4, −0.3) | <0.01 |
Baseline data.
B; beta estimated regression coefficient from three-level mixed effects linear regression and adjusted for study condition, classification error (MVPA mins) and sex with outcome variable as % days of parental overestimation. 95% CI; 95% Confidence Interval, MVPA; moderate and vigorous physical activity, PA; physical activity.
Association with % days of parental overestimation.
Figure 1 shows the grouping of measurement days into four PA awareness categories by objective and parent-classified PA level. In total, 1642 valid measurement days were included. Results primarily focus on overestimation as those children did not meet PA guidelines on some measurement days and their parents may therefore not encourage them to participate in PA promotion.
Parents wrongly classified their child’s PA level on 48% of measured days and overestimated their child’s PA on 43% of all measured days. Children were not meeting PA guidelines (determined using accelerometry) on 57% of valid measurement days and parents overestimated their children’s PA level on 75% of these inactive days. Parents overestimated their child’s PA level on mean (SD) 2.1 (1.8) days/week, with 80% overestimating on ≥1 measurement day. Parents who overestimated their child’s PA level did so by a mean (SD) of 22.0 (13.3) mins/day.
Table 1 shows a summary of the simple associations between individual factors and parental overestimation. Table 2 shows the distribution of parental classification error by categorical objective PA level. Classification error is similar across the four PA categories of <60 mins/day.
Table 2.
Descriptive data for 329 parent-child dyads from San Diego County, CA on percentage days of parental overestimation (n=1642 days) and classification error by category of moderate and vigorous activity.
| Activity category (MVPA mins) | N days | Mean (SD) % overestimation | Mean (SD) classification error* (MVPA mins) |
|---|---|---|---|
| 0 – 14.9 | 73 | 44.3 (42.6) | −44.8 (5.4) |
| 15 – 29.9 | 227 | 50.7 (38.6) | −29.5 (9.2) |
| 30 – 44.9 | 308 | 51.7 (34.4) | −16.1 (11.4) |
| 45 – 59.9 | 325 | 45.6 (32.2) | −5.3 (10.5) |
| 60 – 74.9 | 239 | 0 | 6.1 (9.6) |
| 75 – 89.9 | 181 | 0 | 14.6 (10.9) |
| ≥ 90 | 289 | 0 | 38.7 (22.9) |
PA; physical activity: MVPA; moderate and vigorous activity:
classification error calculated as difference from 60 minute guideline.
Table 3 shows descriptive data on home and family factors and simple associations with parental overestimation. Parent encouragement, transport provision for PA and parents doing PA with their child were positively associated with parental overestimation. The only variable remaining in the final model was parents providing transport for PA (β (95% CI) 2.3 (0.9, 3.7) p<0.01).
Table 3.
Descriptive data for potential home and family correlates and results of simple three-level mixed effects linear regression with potential home and family correlates and % days of parental overestimation of child PA among 329 children and parents from San Diego County, CA.
| Potential correlate | Mean (SD) or % | B | (95% CI) | P value# |
|---|---|---|---|---|
| Sports participation (sessions/week) | 3.2 (2.7) | 0.8 | (−0.3, 1.9) | 0.14 |
| Parental encouragement for PA (days/week)1 | 4.6 (2.2) | 1.5 | (0.2, 2.8) | 0.02 |
| Parent transport provision for PA (days/week) | 3.7 (2.3) | 1.9 | (0.7, 3.1) | <0.01 |
| Parental PA with child (days/week) | 2.9 (2.0) | 1.8 | (0.4, 3.3) | 0.01 |
| Parental encouragement for less inactivity (days/week) | 4.3 (2.8) | −0.8 | (−1.8, 0.2) | 0.12 |
| Total PA equipment at home (n available) | 4.2 (2.0) | 1.2 | (−0.3, 2.6) | 0.11 |
| Sedentary equipment in bedroom (n available) | 0.7 (0.4) | 5.5 | (−0.9, 11.9) | 0.09 |
| Child visits to PA locations (visits/week) | 12.1 (6.0) | 0.3 | (−0.1, 0.8) | 0.17 |
| Number of PA locations used ≥ once a week (Mean (SD)) | 4.0 (2.0) | 0.3 | (−1.1, 1.8) | 0.66 |
| Rules for PA | ||||
| Do homework before going out (% have rule) | 70.4 | 2.8 | (−0.5, 9.1) | 0.38 |
| Stay close or within sight of home (% have rule) | 92.7 | 8.2 | (−2.8, 19.2) | 0.14 |
| Do not go into the street (% have rule) | 76.9 | −0.2 | (−6.9, 6.6) | 0.95 |
| Do not go places alone (% have rule) | 92.4 | −3.4 | (−14.1, 7.4) | 0.54 |
| Stay within neighborhood (% have rule) | 93.9 | 4.1 | (−7.9, 16.2) | 0.50 |
| Wear a helmet (when biking etc) (% have rule) | 87.8 | −4.0 | (−12.7, 4.7) | 0.37 |
| Wear protective clothing (e.g. knee pads) (% have rule) | 61.6 | −1.9 | (−7.7, 4.0) | 0.53 |
| Avoid strangers (% have rule) | 92.4 | 0.9 | (−9.7, 11.6) | 0.86 |
B; beta estimated regression coefficient from three-level mixed effects linear regression and adjusted for study condition, classification (MVPA mins) and sex with outcome variable as % days of parental overestimation. 95% CI; 95% Confidence Interval, PA; physical activity.
Association with % days of parental overestimation.
Sensitivity analyses using 45 minutes of MVPA as the guideline threshold showed parents overestimating their child’s PA on 27% versus 43% of all days. Sex was no longer significantly associated with % days overestimation (B (95% CI) p value as 4.3 (−0.3, 0.8) p=0.07) but all other associations were similar.
Discussion
Most parents incorrectly classified their child as meeting PA guidelines on days when children were actually inactive (not meeting the PA guideline). Most parents overestimated their child’s PA level at some point during the measurement period. As this is the first study addressing parental awareness in an ethnically diverse population and using a daily measure, these findings emphasize the relevance of parental overestimation in PA promotion.
The parents in the present study had similar levels of overestimation as a previous British study (Corder et al., 2010). The high prevalence of overestimation identified in both studies supports the potential importance of further research regarding parental awareness. As shown previously, parental overestimation was higher for parents of girls (Corder et al., 2010) and may be partly due to the lower PA level of girls versus boys. The lack of association with BMI contrasts previous results suggesting that parents who overestimate their child’s PA level have children with lower fat mass (Corder et al., 2010).
Parent overestimation of child PA was higher among parents who reported more parent support for child PA. Apart from sex, these parental support variables were the only factors associated with parental overestimation and providing transport was the only variable to remain in the final model. The parental burden of providing support including transport to PA locations may lead parents to assume that their child is sufficiently active even if the child is not meeting guidelines. Although parental PA support is positively associated with child PA (van der Horst et al., 2007), providing more support appears to be associated with higher overestimation. Even if parents support their children to engage in PA, this may still not be sufficient to meet guidelines. A potential strategy might be to encourage parents to consider whether their child’s activities are sufficiently ‘active’ to meet guidelines. This finding also supports promotion of active travel perhaps as an alternative to parents providing motorized transport for children to do PA. Findings may be due to reverse causality as parents who have identified their child as insufficiently active may have started providing support. Higher overestimation was positively associated with parental support which questions our initial hypothesis that parents who wrongly consider their child as active will not encourage their child to do PA. However, it is possible that inactive children still need additional parental support in order to meet guidelines. A trial is necessary to establish whether parental overestimation can be reduced, whether this increases parental encouragement and whether this also increases child PA.
Parental monitoring of child PA in addition to parental education about adequate PA levels for children may target parental overestimation of child PA, but this needs investigation in a trial. Other complementary intervention strategies including goal setting and personalized feedback to parents about their children may improve parental awareness and increase children’s PA (Michie et al., 2009). Self-monitoring step counts using pedometers has potential in PA promotion among children but more research is necessary to establish how self-monitoring can be used most effectively (Lubans et al., 2009) and how best to involve parents.
We are unable to determine causation from this cross-sectional analysis. Results are from post-intervention measurements from an obesity prevention intervention. Analyses were adjusted for study condition and the intervention did not specifically target PA awareness but results could still be influenced by the intervention, possibly due to alterations of parental attitudes towards PA or heightened expectations of children’s PA levels. Accelerometry assessed PA is more accurate than most self-report measures but has limitations including no information about activity type (Corder et al., 2007). We could not assess ‘overestimation’ continuously due to dichotomous parent-classified PA. However, the discrepancy between child PA levels and the guideline was included in analyses, so results are independent of child PA. In future, parents could be asked to classify their child’s PA in multiple categories directly comparable to categorized objective data. However, these results are supported by sensitivity analyses showing similar results when using 45 minutes to define active/inactive. The amount of overestimation was also similar across MVPA categories irrespective of PA level.
Most parents incorrectly classify their child as meeting PA guidelines on days when they are actually inactive. Parent support was associated with greater parental overestimation. Strategies addressing parental awareness of child PA may be important when designing PA promotion interventions for children.
Highlights.
Parents overestimating their child’s PA may not support their children to do more PA.
Most parents incorrectly think that their child is active when they are instead inactive.
Strategies addressing parental overestimation may be important in child PA promotion.
Acknowledgments
Data used for this study were obtained from Project MOVE/me Muevo funded by the National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK072994). Noe C. Crespo was supported by grants T32HL079891 and F31KD079345 and John P. Elder was supported by NIDDK grant R01 DK072994 and partially by PRC grant U48 DP000036.
Abbreviations
- PA
Physical activity
- MVPA
Moderate and vigorous physical activity
Footnotes
Conflict of interest
The authors declare that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Center for Disease Control and Prevention. 2000 http://www.cdc.gov/growthcharts/
- Corder K, Brage S, Ekelund U. Accelerometers-pedometers: methodology and clinical application. Curr Opinion Clin Nutr Metab Care. 2007;10:597–603. doi: 10.1097/MCO.0b013e328285d883. [DOI] [PubMed] [Google Scholar]
- Corder K, Sallis JF, Crespo NC, Elder JP. Active children use more locations for physical activity. Health place. 2011;17:911–9. doi: 10.1016/j.healthplace.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corder K, van Sluijs EM, Goodyer I, Ridgway CL, Steele RM, Bamber D, Dunn V, Griffin SJ, Ekelund U. Physical activity awareness of British adolescents. Arch Ped Adol Med. 2011;165:603–9. [PMC free article] [PubMed] [Google Scholar]
- Corder K, van Sluijs EM, McMinn AM, Ekelund U, Cassidy A, Griffin SJ. Perception versus reality awareness of physical activity levels of British children. Am J Prev Med. 2010;38:1–8. doi: 10.1016/j.amepre.2009.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobbins M, De Corby K, Robeson P, Husson H, Tirilis D. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6–18. Cochrane Database of Systematic Reviews. 2009:Art No: CD007651. doi: 10.1002/14651858.CD007651. [DOI] [PubMed] [Google Scholar]
- Ekelund U, Åman J, Westerterp K. Is the ArteACC index a valid indicator of free-living physical activity in adolescents? Obes Res. 2003;11:793–801. doi: 10.1038/oby.2003.110. [DOI] [PubMed] [Google Scholar]
- Ekelund U, Sjöström M, Yngve A, Poortvliet E, Nilsson A, Froberg K, Wedderkopp N, Westerterp K. Physical activity assessed by activity monitor and doubly labelled water in children. Med Sci Sports Exerc. 2001;33:275–281. doi: 10.1097/00005768-200102000-00017. [DOI] [PubMed] [Google Scholar]
- Giles-Corti B, Kelty SF, Zubrick SR, Villanueva KP. Encouraging walking for transport and physical activity in children and adolescents: how important is the built environment? Sports Med. 2009;39:995–1009. doi: 10.2165/11319620-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Kerr J, Sallis JF, Rosenberg DE, Norman GJ, Saelens BE, Durant N. [Last accessed: September 14th 2010];Active Where? Surveys. 2008 Available at: www.activelivingresearch.org/node/11951.
- Lechner L, Bolman C, van Dijke M. Factors related to misperception of physical activity in The Netherlands and implications for health promotion programmes. Health Prom Int. 2006;21:104–112. doi: 10.1093/heapro/dal011. [DOI] [PubMed] [Google Scholar]
- Lubans DR, Morgan PJ, Tudor-Locke C. A systematic review of studies using pedometers to promote physical activity among youth. Prev Med. 2009;48:307–15. doi: 10.1016/j.ypmed.2009.02.014. [DOI] [PubMed] [Google Scholar]
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28:690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- Ronda G, van Assema P, Brug J. Stages of change, psychological factors and awareness of physical activity levels in the Netherlands. Health Prom Int. 2001;16:305–314. doi: 10.1093/heapro/16.4.305. [DOI] [PubMed] [Google Scholar]
- Rosenberg DE, Sallis JF, Kerr J, Maher J, Norman GJ, Durant N, Harris SK, Saelens BE. Brief scales to assess physical activity and sedentary equipment in the home. Int J Behav Nutr Phys Act. 2010;7:10. doi: 10.1186/1479-5868-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon J, Booth ML, Phongsavan P, Murphy N, Timperio A. Promoting physical activity participation among children and adolescents. Epidemiol Rev. 2007;29:144–59. doi: 10.1093/epirev/mxm010. [DOI] [PubMed] [Google Scholar]
- Steele R, Brage S, Corder K, Wareham N, Ekelund U. Physical activity, cardiorespiratory fitness, and the metabolic syndrome in youth. J Appl Physiol. 2008;105:342–351. doi: 10.1152/japplphysiol.00072.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- Trost S, McIver K, Pate R. Conducting Accelerometer-Based Activity Assessments in Field-Based Research. Med Sci Sports Exerc. 2005;37:531–543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- van der Horst K, Chin A, Paw M, Twisk J, van Mechelen W. A Brief Review on Correlates of Physical Activity and Sedentariness in Youth. Med Sci Sports Exerc. 2007;39:1241–1250. doi: 10.1249/mss.0b013e318059bf35. [DOI] [PubMed] [Google Scholar]
- van Sluijs E, Griffin S, van Poppel M. A cross-sectional study of awareness of physical activity: associations with personal, behavioural and psychosocial factors. Int J Behav Nutr Phys Act. 2007;8 doi: 10.1186/1479-5868-4-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Sluijs E, McMinn A, Griffin S. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. Brit Med J. 2007;6:335. doi: 10.1136/bmj.39320.843947.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Stralen MM, de Vries H, Bolman C, Mudde AN, Lechner L. Exploring the efficacy and moderators of two computer-tailored physical activity interventions for older adults: a randomized controlled trial. Ann Behav Med. 2010;39:139–50. doi: 10.1007/s12160-010-9166-8. [DOI] [PubMed] [Google Scholar]
- Wareham N, van Sluijs E, Ekelund U. Physical activity and obesity prevention: a review of the current evidence. Proc Nutr Soc. 2005;64:229–47. doi: 10.1079/pns2005423. [DOI] [PubMed] [Google Scholar]
- Watkinson C, van Sluijs E, Sutton S, Hardeman W, Corder K, Griffin S. Overestimation of physical activity level is associated with lower BMI: a cross-sectional analysis. Int J Behav Nutr Phys Act. 2010;7:68. doi: 10.1186/1479-5868-7-68. [DOI] [PMC free article] [PubMed] [Google Scholar]