Abstract
Objective
Proposed DSM-5 severity dimensions reveal ambiguity regarding the extent to which certain features define boundaries between similar diagnoses or represent underlying dimensions within a broader category of bulimic syndromes. The current study utilized a novel mixed modeling approach that can simultaneously model latent dimensions and latent categories to address this ambiguity.
Method
Data from structured clinical interviews in 528 adult participants were analyzed.
Results
A 3-class solution with one severity dimension that was invariant across groups provided the best-fitting model. Both latent classes 1 and 2 included bulimic syndromes but were distinguished by greater purging and weight phobia in latent class 1. Latent class 3 resembled a non-eating disorder class. External validation analyses supported significant differences among empirically derived groups.
Discussion
Weight phobia contributes to categorical distinctiveness among bulimic syndromes whereas other features (purging, binge eating, and weight) may do so only in specific combinations. Uniform severity criteria may be appropriate across bulimic syndromes.
Keywords: bulimia nervosa, eating disorder not otherwise specified, factor mixture analysis, nosology
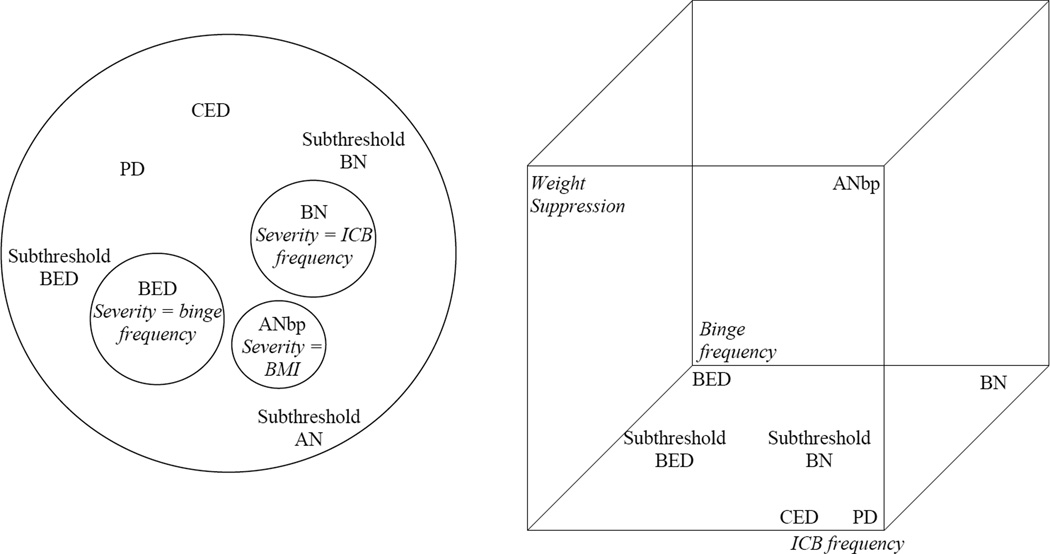
The Diagnostic and Statistical Manual for Mental Disorders Fifth Edition (DSM-5) will include dimensional ratings of severity for eating disorder diagnoses to account for differences in treatment response and course observed within diagnostic categories and to inform clinicians regarding the level of intervention that might be warranted for a given clinical presentation.1 Frequency of inappropriate compensatory behaviors has been proposed for describing severity of bulimia nervosa (BN). Frequency of binge-eating episodes has been proposed for the new diagnosis of binge eating disorder (BED), and body mass index (BMI) has been proposed for anorexia nervosa (AN). However, these same features are used to demarcate one eating disorder from another. For example, BMI would be a key variable that would distinguish between the diagnosis of AN binge-purge subtype and BN, and inappropriate compensatory behaviors would be a key feature for distinguishing between BN and BED. Thus, proposed categories and dimensional ratings for these categories in the DSM-5 appear to view certain eating disorder features as representing both severity dimensions and as demarcating categories. Although this approach fits distinctions that can be made between diagnoses with minimal symptom overlap (e.g., the restricting subtype of AN and BED), it creates ambiguity for understanding whether disorders with significant symptom overlap (e.g., AN binge-purge subtype, BN, and BED) should be thought of as being categorically distinct as proposed for the DSM-5 or as residing on continuums of severity within a broader category of bulimic syndromes (see Figure 1).
Figure 1.
Proposed Model of Bulimic Syndromes in the DSM-5 vs. an Alternative Dimensional Model of Bulimic Syndromes.
Note: ANbp=Anorexia nervosa, binge-purge subtype; BN=Bulimia Nervosa, BED=Binge Eating Disorder, PD=Purging Disorder, CED=nonpurging Compensatory Eating Disorder, BMI=Body Mass Index, ICB=Inappropriate Compensatory Behaviors
One method for addressing this ambiguity is to examine the latent structure of bulimic syndromes from a statistical perspective. Statistical approaches can reveal whether there are naturally occurring cut-points between syndromes, and where these cut-points reside, or whether distinctions between diagnoses appear to be artificially imposed by diagnostic criteria sets. Although a recent review2 found strong support for the predictive validity of distinguishing between AN binge-purge subtype, BN, and BED in terms of treatment response, course and outcome, limited support has emerged for the etiological validity of these distinctions. For example, heritability estimates for bulimic syndromes range from 54% to 83% in female twin samples3–5, with no significant difference in heritability between narrowly (a2=.62) and broadly defined (a2=.61) BN3. In addition, the correlation between additive genetic factors for broadly defined BN and AN has been estimated at ra=.793, supporting the possibility that broad phenotypes may lead to greater understanding of the genetic underpinnings of bulimic syndromes. If statistical analyses indicate that differences in BMI, binge eating, and purging reflect variations in severity rather than type, then future studies might examine whether evidence of predictive validity might also support a dimensional approach, consistent with recommendations for the NIMH Research Domain Criteria (RDoC) initiative.6
Unfortunately, prior latent structure studies of eating disorders have employed methods that assume either latent dimensions (e.g., factor analysis) or latent categories (e.g., latent class analysis) which cannot address this ambiguity. Although taxometric analyses are ideally suited to distinguish categories from continua, they rely on the presence of multiple indicators that discriminate between potential categories – a requirement not met by some bulimic syndrome diagnoses that are typically demarcated from one another by a single feature.7 For example, BN and BED are distinguished by the presence versus absence of inappropriate compensatory behaviors, limiting the utility of taxometric methods for examining whether inappropriate compensatory behaviors represent a severity dimension for bulimic syndromes with BED at one end of the spectrum and BN with high frequency purging at the other or whether presence versus absence of inappropriate compensatory behaviors represents a cut-point between BN and BED as defined within the DSM-5. Recently, factor mixture analyses (FMA) have been developed to allow for the simultaneous modeling of latent categories and latent dimensions8, 9 and seem ideally suited to resolve discrepancies in our understanding of the latent structure of bulimic syndromes. This approach may help resolve questions regarding the relationship between BN and forms of eating disorder not otherwise specified (EDNOS) that may be viewed as separate eating disorders (e.g., BED and purging disorder; PD10) or as variants of BN that differ on the latent dimensions of frequency of inappropriate compensatory behaviors or frequency of binge eating.
If certain eating disorder features delineate distinct categories, then adding new diagnostic categories to the DSM-5, such as BED, could reduce reliance on EDNOS without risking loss of information for existing diagnoses.11 In contrast, if certain eating disorder features represent an underlying dimension of severity, then a broad category for bulimic syndromes might subsume related EDNOS (see Figure 1).12 The latter approach also might facilitate identification of underlying dimensions of function related to biological processes, as proposed by the recent Research Domain Criteria (RDoC) initiative.6 Application of FMA to bulimic syndromes appears particularly warranted for examining proposed revisions for the DSM-5.
FMA model latent categories that demonstrate within-class covariation of item probabilities due to illness severity and may be viewed as extensions of latent class analyses (LCA) and factor analyses (FA).8, 9 An advantage over LCA is that FMA model one or more latent dimensions of severity that may contribute to significant covariation among indicators within classes that would lead to the identification of a spurious class in LCA. An advantage over FA is the ability to identify homogeneous latent groups which may be represented as diagnostic categories within nosological systems such as the DSM. Studies that have employed FMA have found that a hybrid model that combines categories and dimensions provides a superior fit for the structure of attention deficit hyperactivity disorder,13 substance use dependence,8 and appearance enhancing drug use.14 To our knowledge, no study has employed FMA to examine the latent structure of bulimic syndromes.
The current study used mixture modeling, specifically a sequence of LCA, FA, and FMA, to examine the latent structure of bulimic syndromes. We focused on bulimic syndromes, including AN binge-purge subtype, BN, BED, PD, and related EDNOS, because these represent disorders in which a single feature may demarcate different diagnoses or may reflect a latent severity dimension within a single broader category (see Figure 1). A central question of this work is whether bulimic syndromes are best represented as distinct diagnostic groups (and, if so, what are the defining features of these groups), a single group with one or more dimensions of severity, or a combination of distinct groups and dimensions. An advance over previous latent structure studies was the inclusion of large numbers of individuals who met DSM-IV criteria for AN binge-purge subtype, BN, both purging and nonpurging subtypes, BED, proposed research criteria for PD,15 and individuals who reported an array of disordered eating features as well as those reporting no disordered eating. This composition ensured that low base rates, often encountered in population-based samples, would not limit statistical power to detect the presence of distinct groups16 while also providing ample variation (from normality to eating disorders) to ensure that analyses did not simply reify groups selected for participation.2 Based on results from FMA studies of other psychiatric illnesses8, 9, 14, we predicted that a model including both latent categories and latent dimensions would provide the best fit to data. Such a model would fall between the DSM-5 based model and fully dimensional model depicted in Figure 1. However, given that this is the first application of FMA to eating disorders, we did not have a priori hypotheses regarding the number or characteristics of latent groups or dimensions.
Methods
Participants
Participants (N=528; 95.3% female) were recruited from the community for studies on bulimic syndromes, some of which have contributed data to other publications.11, 17, 18 Importantly, the largest of these studies11 contributed 192 (36%) participants and allowed for full variation of possible eating disorder symptoms ranging from DSM-IV AN binge-purge subtype to individuals free from eating disorder symptoms to permit evaluation of a dimensional model. Participants were between the ages of 18 and 53 years; mean (SD) age was 26.2 (7.3) years. Racial/ethnic distribution was 77.7% Caucasian, non-Hispanic, 9.7% Asian, 5.9% African American, 5.1% Hispanic, 0.2% American Indian, 0.2% “Other/Mixed,” and 1.3% undisclosed. Reflecting community-based recruitment, most participants (80%; n=422) were not currently in psychological treatment. However, reflecting the range of illness severity in the sample, 13% (n=69) had a history of psychiatric hospitalization.
Procedures and Measures
All participants completed written informed consent prior to participation, and procedures were IRB approved. Individuals were included in analyses if they 1) participated in studies conducted in the first author’s lab between 1998 and 2007, 2) were assessed with the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I)19 modified to omit skip rules in the eating disorders module to ensure conditional independence of indicators, and 3) came from a subsample that did not diverge from other subsamples on demographic features. For example, data were not included from 207 individuals forming a cohort of 40-year olds from the largest study11 because this could have introduced a latent age-group. Despite these efforts, demographic features differed across study sources (Age: F(4, 501) = 32.17, p<.001; Gender: χ2(1)=25.85, p<.001; BMI: F(4, 523) = 25.76, p<.001; and Race: χ2(4)=15.92, p=.003). Consistent with recommendations for an integrative data analysis,20 these demographic variables were entered as covariates into models.
The SCID-I includes modules to assess current and lifetime Eating, Mood, Anxiety, and Substance Use Disorders and an addendum for Impulse Control Disorders. All interviews were audiotaped with participant consent, and 15% were randomly selected and rated by a second interviewer to assess interrater reliability. Interrater reliability, measured using kappa, did not differ significantly across studies (p-values>.10), and, for current and lifetime disorders, respectively, were 0.82 and 0.86 for Eating disorders, 0.86 and 0.92 for Mood disorders, 0.84 and 0.90 for Anxiety disorders, 0.83 and 0.94 for Substance Use disorders, and 0.69 and 0.81 for Impulse Control disorders. Interviews also provided information on demographic variables, suicidality, abuse history, global assessment of functioning, and treatment history.
Based on SCID-I interviews and DSM-IV criteria, 62 (12%) participants had lifetime diagnoses of DSM-IV AN binge-purge subtype, 165 (31%) had DSM-IV BN (121 with the purging subtype), 155 (29%) had an EDNOS, and 145 participants (27.5%) had no lifetime history of a bulimic syndrome. Among those with EDNOS diagnoses, 44 met DSM-IV proposed criteria for BED, 37 met research criteria for PD,15 19 had a nonpurging compensatory eating disorder (CED; defined by the use of excessive exercise or fasting at least twice per week for three months, the absence of objectively large binge episodes, and presence of undue influence of weight/shape on self-evaluation among individuals of at least minimally normal weight), and 55 had an EDNOS characterized by meeting all criteria for a bulimic syndrome described above with one or more features at subthreshold levels (e.g., all criteria for BN but frequencies of binge-eating and compensatory behaviors less than twice per week for three months). Based on criteria proposed for the DSM-5,1 99 (19%) individuals met lifetime criteria for AN binge-eating/purging type, 171 (32%) had BN, 47 (9%) had BED, and 73 (14%) had an Other Specified Feeding or Eating Disorder. Among these, 35 had PD, 18 had CED, and 20 had subthreshold BN or subthreshold BED. DSM-IV and DSM-5 lifetime diagnoses represent a hierarchy in which a lifetime AN diagnosis ruled out a lifetime BN diagnosis, which ruled out a lifetime BED diagnosis, which ruled out a lifetime EDNOS diagnosis. This hierarchy was used to achieve greater parsimony because the majority of eating disorder cases (>75%) were characterized by a single lifetime diagnosis, and the average n for various lifetime syndrome combinations was small (n<7). For example, despite the heuristic example of an individual meeting criteria for AN, then BN, and then BED over her lifetime, <1% of our sample (n=4) demonstrated this pattern.
Analyses
Indicators
The following lifetime symptoms from the SCID were included in analyses: refusal to maintain a minimally normal weight (coded as absent or present), intense fear of gaining weight or becoming fat (absent or present), undue influence of weight/shape on self-evaluation (absent or present), amenorrhea (absent or present), history of binge eating (absent, subjective binge episode [loss of control but not objectively large amount of food], or objective binge episode [loss of control and objectively large amount of food]), and compensatory behaviors (absent, nonpurging [fasting and excessive exercise], or purging [self-induced vomiting, laxative, or diuretic abuse]). These features were analyzed to determine whether they contributed to the defining boundaries between latent categories or to defining one or more latent dimensions of severity. Additional features of BED (e.g., binge-eating episodes are associated with “eating alone because of being embarrassed by how much one is eating”) were not included because they are conditionally dependent upon the presence of binge eating.
Covariates
Demographic variables (age, sex, and race/ethnicity) and current body mass index (BMI) were included as covariates in analyses. BMI was calculated as weight in kg divided by the square of height in meters. Height and weight were objectively measured in 336 participants (64%), and self-reported in 192 participants (36%). Numerous studies support the test-retest reliability of self-reported height and weight as well as its accuracy when compared with objectively measured height and weight in both clinical and non-clinical samples.21–23
LCA, FA, and FMA were conducted in Mplus Version 5.2124 using maximum likelihood estimation to impute missing values. Data were missing for 0% of participants for cognitive features, 0.4% for history of low weight, 0.6% for binge eating, 4.4% for compensatory behaviors, and 14.4% for amenorrhea (including missing values for men). A series of models were compared, including LCA models ranging from 2–5 classes, 1-factor and 2-factor FA models, and FMA models combining 1–2 factors, 2–4 classes, and the presence/absence of a non-symptomatic (“zero”) class9. The zero-class was parameterized as minimum values on all indicators. FMA models were fit with class-specific variances, as it is possible that classes will differ with respect to the variance of the factor(s) within classes. Models were compared on multiple fit indices including the Akaike Information Criterion (AIC), the Consistent Akaike Information Criterion (cAIC), and the Bayesian Information Criterion (BIC), with the lowest value indicating the best fitting model, and, for categorical models, entropy, with highest values indicating the ability to assign individuals to a latent category with high confidence. Among these indices, BIC has been preferred because it adjusts fit for number of parameters to improve parsimony and because BIC can be compared across non-nested models.25
Validation analyses were conducted to compare groups identified by latent structure analyses on educational and marital status, Axis I disorders, clinical features, and treatment history. Thus, validation analyses focused on variables that differed from the disordered eating features used to form latent groups.26 Across validation analyses, there were 10 independent comparisons conducted, and a Bonferroni-corrected p-value of .005 was used to control for family-wise error rate. When the omnibus test for a variable reached significance at p<.005, post-hoc comparisons among groups were Bonferroni-adjusted for possible pairwise comparisons within each set of analyses.
Results
Latent Structure Analyses
Table 1 presents model fit statistics for LCA, FA, and FMA. Across cAIC, BIC, and entropy, the best-fitting FMA model was superior to the best-fitting LCA and best-fitting FA models, suggesting that bulimic syndromes are best conceptualized as categories that include a dimension of severity. Agreement among various fit indices, including those that emphasize model parsimony (e.g., BIC and cAIC), increases confidence in model selection as do recent simulation analyses suggesting that these indices are robust against various violations of model assumptions.16
Table 1.
Model Fit Statistics for Latent Class Analyses, Factor Analyses, and Factor Mixture Analyses.
| Model | Log L | # Parameters | AIC | cAIC | BIC | Entropy |
|---|---|---|---|---|---|---|
| Latent Class Analyses | ||||||
| 2 c | −1775.292 | 21 | 3592.585 | 3703.235 | 3682.236 | .923 |
| 3 c | −1700.608 | 34 | 3469.217 | 3648.365 | 3614.366 | .793 |
| 4 c | −1658.065 | 47 | 3410.129 | 3657.778 | 3610.777 | .871 |
| 5 c | −1620.221 | 60 | 3360.441 | 3676.588 | 3616.587 | .869 |
| Factor Analyses | ||||||
| 1 f (IRT) | −1794.786 | 18 | 3625.572 | 3720.416 | 3702.415 | - |
| 2 factors | −1735.836 | 28 | 3527.673 | 3675.207 | 3647.207 | - |
| Factor Mixture Analyses | ||||||
| 1 f, zero class | −2097.422 | 10 | 4214.845 | 4267.535 | 4257.536 | - |
| 1 f, 2 c | −1697.534 | 32 | 3459.067 | 3627.679 | 3595.678 | .753 |
| 1 f, 3 c | −1650.035 | 46 | 3392.071 | 3634.448 | 3588.449 | .869 |
| 1 f, 4 c | −1607.121 | 60 | 3334.242 | 3650.388 | 3590.388 | .788 |
| 1 f, 1 c + zero class | −1738.045 | 24 | 3524.090 | 3650.548 | 3626.549 | .963 |
| 1 f, 2 c + zero class | −1669.027 | 38 | 3414.054 | 3614.28 | 3576.279 | .880 |
| 1 f, 3 c + zero class | −1632.352 | 52 | 3368.704 | 3642.697 | 3590.697 | .900 |
| 2 f, zero class | −1882.120 | 20 | 3804.239 | 3909.622 | 3889.621 | - |
| 2 f, 2 c | −1656.854 | 43 | 3399.708 | 3619.010 | 3583.279 | .797 |
| 2 f, 3 c | −1624.163 | 56 | 3360.325 | 3655.395 | 3599.395 | .798 |
Note: Boldface type indicates the best-fitting model within each approach according to BIC. AIC = Akaike Information Criterion; cAIC = consistent AIC; BIC = Bayesian Information Criterion; IRT = Item Response Theory; f = factor; c = class. Neither a 3 factor FA nor 3 factor FMA model could be fit to the data.
To address whether different features contribute to severity in each latent class, similar to what has been proposed for the DSM-5, we conducted metric invariance analyses comparing a model in which the mean latent severity dimension was equal across the three latent classes (invariance model) to a model in which these parameters were free to vary (variance model), with class-specific factor variances for both models. Analyses were run without covariates due to problems with model convergence when covariates were included. Compared to fit for the invariance model (Log-likelihood = −1728.401, parameters = 24, AIC = 3504.801, cAIC=3642.697, BIC=3607.260, entropy = .851), the variance model did not provide an improved fit to data (Log-likelihood = −1723.257, parameters = 27, AIC = 3500.513, cAIC=3642.78, BIC=3615.779, entropy = .857). Indeed, BIC was better for the model of metric invariance, supporting factor invariance for the latent severity dimension across the latent classes. This means that the latent severity dimension explains variability within each class in the same way such that the same score would indicate the same severity across classes. Indicator loadings on the latent severity dimension supported that all eating disorder symptoms loaded positively, such that presence of a symptom (vs. its absence) contributed to the severity of bulimic syndromes. Among indicators, those related to body image disturbance demonstrated the highest loadings whereas amenorrhea demonstrated the weakest loading, suggesting that it was least meaningful for contributing to severity of illness.
Using the posterior probabilities from the best-fitting FMA model, 294 (55.7%) participants were assigned to latent class 1 (LC1), 112 (21.2%) to latent class 2 (LC2), and 122 (23.1%) to latent class 3 (LC3). Table 2 presents distributions of symptoms within the latent classes. LC1 was associated with the highest endorsement probabilities across indicators with the exception of nonpurging compensatory behaviors which were more commonly endorsed among members of LC2. LC2 presented a mix of features with the exception of low endorsement of fear of gaining weight or becoming fat (present in 12% of LC2) combined with high endorsement of undue influence of weight and shape on self-evaluation (present in 92% of LC2). LC3 reflected a healthy group that denied most, but not all, eating disorder symptoms. Key features that distinguished LC1 from LC2 included weight phobia and purging, which were more common in LC1 than in LC2, and nonpurging compensatory behaviors, which were more common in LC2 than in LC1. Key features that distinguished between LC2 and LC3 included binge eating and undue influence of weight and shape on self-evaluation, which were more common in LC2 than in LC3.
Table 2.
Distributions of Eating Disorder Symptoms across Latent Classes from Best-Fitting FMA Model.
| Symptom | LC1 N=294 n (%) |
LC2 N=112 n (%) |
LC3 N=122 n (%) |
|---|---|---|---|
| Refusal to maintain expected body weight (EBW) | |||
| None | 204 (69) | 99 (88) | 122 (100) |
| Threshold (Weight < 85% EBW) | 90 (31) | 13 (12) | 0 (0) |
| Fear of Gaining Weight or Becoming Fat | |||
| Absent | 11 (4) | 98 (88) | 122 (100) |
| Threshold | 283 (96) | 14 (12) | 0 (0) |
| Undue Influence of Weight and Shape on Self-Evaluation | |||
| Absent | 4 (1) | 9 (8) | 122 (100) |
| Threshold | 290 (99) | 103 (92) | 0 (0) |
| Amenorrhea | |||
| None (0) | 146 (50) | 102 (91) | 109 (89) |
| Threshold (no menstruation ≥3 consecutive months) | 148 (50) | 10 (9) | 13 (11) |
| Binge eating | |||
| None | 1 (<1) | 43 (38) | 118 (97) |
| Loss of Control/not large amount of food (SBE) | 53 (18) | 13 (12) | 4 (3) |
| Loss of Control/large amount of food (OBE) | 240 (82) | 56 (50) | 0 (0) |
| Compensatory behaviors | |||
| None | 23 (8) | 49 (44) | 122 (100) |
| Nonpurging (e.g., fasting) | 53 (18) | 38 (34) | 0 (0) |
| Purging (e.g., vomiting) | 218 (74) | 25 (22) | 0 (0) |
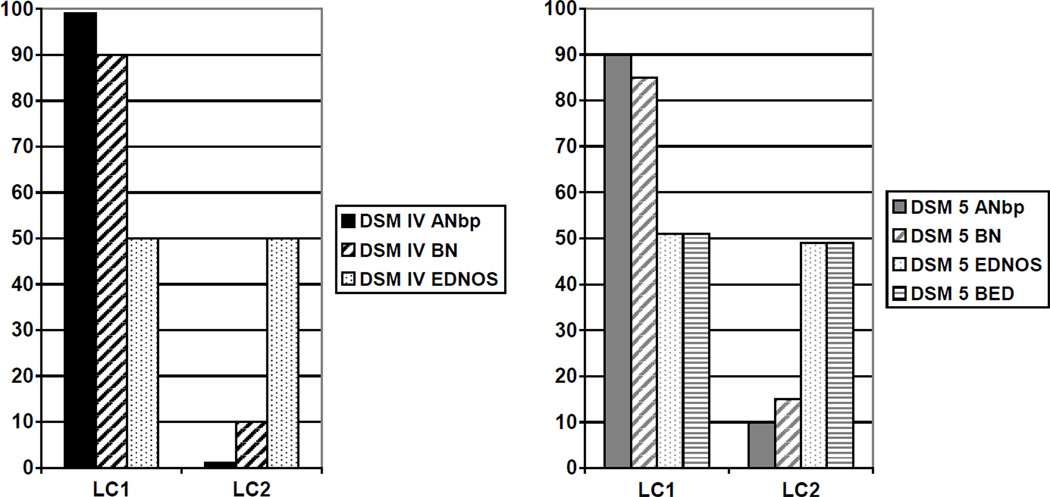
Excluding individuals with no lifetime history of an eating disorder (for which there was excellent agreement between empirically derived latent classes and interview-based diagnoses; kappa=.90), we found significant associations between latent class membership and both DSM-IV diagnostic groups (χ2 (2)=91.21, p<.001) and DSM-5 diagnostic groups (χ2 (3)=58.28, p<.001). Figure 2 presents the distribution of DSM-IV and proposed DSM-5 diagnostic groups across latent classes 1 and 2. Overall, a large majority of individuals with either DSM-IV or DSM-5 diagnoses of AN binge-purge subtype or BN fell within LC1 whereas individuals with DSM-IV and DSM-5 diagnoses of EDNOS were evenly split between LC1 and LC2. Like diagnoses of EDNOS, the proposed DSM-5 group of BED was equally likely to fall within LC1 and LC2 (51% vs. 49%; see Figure 2). Individuals with BED in LC1 were significantly more likely to endorse an intense fear of gaining weight or becoming fat (weight phobia) compared to individuals with BED in LC2 (96% vs. 0%; χ2(1)=43.16, p<.001).
Figure 2.
Distribution of DSM-IV and Proposed DSM-5 Eating Disorder Diagnoses across Latent Classes 1 and 2. ANbp – anorexia nervosa binge-purge subtype, BN – bulimia nervosa, BED – binge eating disorder, and EDNOS – eating disorder not otherwise specified.
Given heterogeneity among individuals in the EDNOS category, we further explored whether there were any distinguishable syndromes that were more likely to fall into LC1 versus LC2 among those with EDNOS. Among those with diagnoses of PD, 86% fell within LC1. Among those with diagnoses of CED, 100% fell within LC2. Finally, 64% of those with subthreshold forms of BN or BED fell within LC2. Thus, while FMA provided no basis for distinguishing between purging and nonpurging behaviors among those who binge, results suggested clear distinctions between purging and nonpurging among those who do not binge.
Validation Analyses
Empirically Derived Groups
Latent classes differed significantly on educational status (χ2(6)=26.69, p<.001) and marital status (χ2(6)=26.60, p<.001). Overall, LC1 was less educated than LC2 and LC3. In addition, members of LC1 were half as likely to be married compared to members of LC2 and LC3 and were more than twice as likely to be divorced as members of LC2 and LC3.
Table 3 presents results from validation analyses of empirically derived groups on Axis I disorders, clinical features, and treatment history. Significant differences were found among groups for all Axis I disorders. For lifetime and current mood and anxiety disorders, LC1 endorsed higher prevalence estimates compared to LC2 who reported higher prevalence than LC3. In contrast, for lifetime and current substance use and impulse control disorders, LC1 endorsed higher lifetime prevalence than both LC2 and LC3, which did not differ significantly from one another.
Table 3.
Validation Analyses of Latent Classes (N=528)
| Axis I Disorders | LC1 N=294 |
LC2 N=112 |
LC3 N=122 |
|
|---|---|---|---|---|
| Lifetime | n (%) | n (%) | n (%) | χ2 (2) |
| Mood | 221 (76)a | 58 (53)b | 26 (22)c | 105.87** |
| Anxiety | 131 (45)a | 33 (31)b | 12 (10)c | 47.19** |
| Substance Use | 138 (48)a | 26 (25)b | 17 (14)b | 47.16** |
| Impulse Control | 98 (34)a | 14 (13)b | 5 (4)b | 48.70** |
| Current | n (%) | n (%) | n (%) | χ2 (2) |
| Mood | 75 (26)a | 12 (11)b | 0 (0)c | 43.78** |
| Anxiety | 92 (32)a | 19 (17)b | 7 (6)c | 37.81** |
| Substance Use | 23 (8)a | 1 (1)b | 0 (0)b | 15.92** |
| Impulse Control | 61 (21)a | 9 (8)b | 2 (2)b | 29.62** |
| Clinical Features | n (%) | n (%) | n (%) | χ2 (2) |
| Suicidality in Mood Episode† | 99 (64) | 25 (50) | 10 (38) | 7.58 |
| Physical or Sexual Abuse/Assault | 68 (23)a | 11 (10)b | 10 (8)b | 18.66** |
| GAF Score (Mean (SE)) | 57.5 (0.6)a | 69.1 (1.0)b | 82.2 (0.9)c | F (2,487)=274.69** |
| Treatment History | n (%) | n (%) | n (%) | χ2 (2) |
| Current Treatment | 85 (29)a | 20 (18)a | 2 (2)b | 40.83** |
| Lifetime Treatment | 246 (84)a | 73 (65)b | 31 (25)c | 131.10** |
| Hospitalization | 63 (21)a | 7 (6)b | 0 (0)c | 40.50** |
| Psychotropic Medication Use | 73 (25)a | 9 (8)b | 3 (2)b | 38.59** |
Percentages are taken from among those with a lifetime history of a mood disorder (n=31 in LG1; n=66 in LG2; n=45 in LG3; n=59 in LG4; n=30 in LG5)
p<.001
Superscripts that differ represent significant differences between groups using a Bonferroni corrected p-value.
Significant differences were found for history of physical or sexual abuse/assault and interview-rated Global Assessment of Functioning (GAF) score. LC1 reported significantly higher rates of abuse compared to both LC2 and LC3, which did not differ significantly from one another. GAF scores were significantly worse (reflected by lower scores) in LC1 compared to LC2 and also significantly worse in LC2 compared to LC3.
Significant differences also were found for all treatment history variables. LC3 was associated with significantly lower likelihood of current treatment compared to both LC1 and LC2, which did not differ significantly from each other. Both lifetime treatment and inpatient treatment were significantly more likely in LC1 compared to LC2 and significantly more likely in LC2 than LC3. Finally, members of LC1 were more likely to have received psychotropic medication compared to both LC2 and LC3, which did not differ significantly from one another.
Severity Dimension
Logistic regressions were used to examine the ability of the latent dimension to predict status on the various external validators. Higher scores on the latent severity dimension discriminated significantly between those with the lowest educational level versus those with the highest level (Odds Ratio=2.41, β (SE)=0.880 (.261), p<.001), and those who were single versus those who were married (Odds Ratio=4.69, β (SE)=1.546 (.201), p<.001). Higher scores also discriminated those with a current mood disorder from those with no current mood disorder (Odds Ratio=1.30, β (SE)=0.263 (.071), p<.001).
Although the valence of all associations was in the expected direction (i.e., a higher factor score was associated with greater problems), many did not reach significance using the Bonferroni-corrected p-value (p<.005). Findings that reached traditional thresholds for statistical significance (p<.05) included positive associations between severity and hospitalization (Odds Ratio=1.32, β (SE)=0.274 (.101), p=.006), lifetime impulse control disorder (Odds Ratio=1.21, β (SE)=0.191 (.071), p=.007), current impulse control disorder (Odds Ratio=1.17, β (SE)=0.160 (.067), p=.016), lifetime substance use disorder (Odds Ratio=2.14, β (SE)=0.761 (.365), p=.037), lifetime anxiety disorder (Odds Ratio=4.98, β (SE)=1.605 (.772), p=.038), and suicidality (Odds Ratio=1.14, β (SE)=0.130 (.064), p=.042).
Discussion
The purpose of this study was to examine whether bulimic syndromes are best conceptualized as multiple categories with unique dimensions of severity, as a single category composed of multiple severity dimensions, or a combination of categories with one or more dimensions of severity. Results support a hybrid model in which there are categorically distinct entities as well as a single latent dimension of severity among those with bulimic syndromes. Thus, findings support neither the proposed DSM-5 model of bulimic syndromes nor a fully dimensional model as depicted in Figure 1. Of note, analyses indicated that the latent severity dimension reflected the same construct across categories, suggesting that severity might be captured by a symptom count across diagnoses rather than separate dimensions for each diagnosis, which has been proposed for the DSM-5.1 This approach would fit heterogeneity present within any diagnostic category. For example, among individuals with DSM-5 AN who do not differ on BMI, presence of explicit weight phobia, binge-eating, and purging behaviors would denote greater severity compared to the absence of any or all of these features. Importantly, analyses did not support a categorical boundary between AN binge-purge and BN purging subtype. Instead, findings suggest that these syndromes reside on a dimension in which low weight accounts for differences in severity. Given recent data supporting that higher weight suppression predicts worse treatment outcome in BN27 and worse 10-year outcome28, one might reconceptualize AN binge-purge subtype as falling at the extreme end of weight suppression within a broader bulimic syndrome category. Further, among those with weight phobia, both binge eating or purging may contribute to severity. Based on these results, one might view AN binge-purge subtype as being the most severe bulimic syndrome, followed by BN purging with high weight suppression, followed by BN purging with low weight suppression, followed by BN nonpurging subtype, PD, and then BED characterized by weight phobia. In contrast, eating disorders not characterized by weight phobia appear to be categorically distinct disorders, characterized by lower severity.
Latent classes represented a collection of full-threshold eating disorders and some EDNOS (LC1), several current forms of EDNOS (LC2), and no eating disorder (LC3). Thus, although the same latent dimension score would represent the same level of severity across classes, the classes themselves differed on severity scores, with LC1 representing the most severe eating disorders, LC2 representing what might be considered subthreshold eating disorders, and LC3 largely free of eating disorders. Key indicators that distinguished LC1 from LC2 included weight phobia and purging. Key indicators that distinguished LC2 from LC3 included binge eating and undue influence of weight and shape on self-evaluation. Yet, neither purging nor binge-eating distinguished among syndromes included in LC1, suggesting that it was the configuration of symptoms that produced categories. Finding also support that indicators could simultaneously contribute to categorical distinctions between latent classes and severity within latent classes. For example, purging distinguished between LC1 and LC2 but also loaded significantly onto the latent severity dimension that captured severity within both classes. Validation analyses indicated that the latent classes differed on educational and marital status, comorbid disorders, abuse history, global assessment of functioning, and treatment history.
Although data were collected with an interview that groups questions about AN separately from questions about BN, analyses did not separate AN binge-purge subtype from BN, consistent with other studies failing to find a point of rarity between these syndromes.29–31 An advantage of the current study is that results cannot be attributed to a low base rate or limited number of indicators. Importantly, statistical approaches address only one form of validity for diagnostic categories,32 and studies of course and treatment outcome support the predictive validity of distinguishing between AN binge-purge subtype and BN.2 However, evidence of predictive validity comes from comparisons of results from separate studies of each group rather than identifying an inflection point along the continuum of BMI or weight suppression for which outcomes differ. Future studies may benefit from examining diagnostically mixed samples in which BMI or weight suppression is included as a covariate along with diagnosis to evaluate evidence of predictive validity, consistent with recommendations from the RDoC initiative.6
Although data came from separate studies of bulimic syndromes, analyses did not segregate participants based on their original study cohort. For example, despite a focus on PD for one of the studies included in analyses,18 a latent PD group did not emerge. Instead, most cases of PD fell within LC1 along with cases of AN binge-purge subtype, BN purging and nonpurging subtypes, and BED that came from several studies contributing to analyses. PD was the only form of EDNOS in which a majority of cases appeared in LC1. In contrast, approximately half of BED fell in LC1 and half fell in LC2, apparently divided by the presence versus absence of weight phobia. Given that additional features proposed for a diagnosis of BED in the DSM-5 (e.g., eating alone because of being embarrassed by the amount of food consumed) have demonstrated poor predictive value for making a diagnosis in previous work,33 it would be beneficial to include features in BED criteria that would add to the validity of the diagnosis. Based on our findings, weight phobia could be included as a cognitive feature of BED, similar to proposals to add body image disturbance to the defining features of BED to capture important variance in this group.34 If weight phobia were included as a diagnostic criterion for BN, PD, and BED (and retained for AN), results suggest that differences among these diagnoses might be best captured by using frequency of binge-eating episodes and purging episodes as dimensional severity ratings within a single broad bulimic syndrome category.
While purging frequency might be used as a dimensional severity rating within a broad bulimic syndrome category, our findings extend previous models by suggesting that presence versus absence of purging may indicate a threshold for categorical distinctiveness.35, 36 Most cases of PD were grouped in LC1 with AN and BN. Conversely, all cases of CED were found in LC2. Results are consistent with recent findings that expanding the definition of PD to include nonpurging inappropriate compensatory behaviors increases the heterogeneity and decreases the clinical significance of PD.37
Previous studies38, 39 have produced latent classes characterized by lower weight phobia similar to LC2 in our study. However, these findings have been interpreted as potentially reflecting spurious classifications due to variation in illness severity within one true category. This is the first latent structure study to suggest weight phobia may distinguish categorically distinct disorders of eating. Findings dovetail with recent meta-analytic results suggesting that AN without weight phobia may be qualitatively distinct from AN with weight phobia.40 Thus, the proposal to alter the weight phobia criterion in the DSM-5 to include “persistent behavior to avoid weight gain” even if an individual does not explicitly endorse weight phobia may substantively change who is diagnosed with AN. Although removing explicit endorsement of weight phobia from the diagnostic criteria for AN would permit diagnoses and treatment in individuals who deny the fears they experience, diagnosing individuals with AN who genuinely lack weight phobia will increase the number of individuals diagnosed with this disorder while decreasing the severity and clinical significance of the diagnosis.
The current study adopted a novel approach to evaluate the empirical typology of syndromes characterized by various eating disorder features. Additional strengths include our large sample size, diversity of clinical presentations and severity, structured clinical interview assessments with high interrater reliability, and range of external validators. Despite these strengths, the study had certain weaknesses that should be considered when interpreting findings. Although we included a range of different EDNOS presentations that have not been examined in previous studies of bulimic typology, we had smaller numbers of some of the possible subtypes, including CED. Future studies would benefit from employing an approach similar to the current study in which enhanced recruitment of CED is used in conjunction with recruitment of participants presenting with a full range bulimic syndromes to better characterize where these syndromes fall in relation to disorders characterized by binging, purging, or both binging and purging.
Because data come from cross-sectional assessments, only statistical evidence of points of rarity32 and concurrent validity41 could be examined. Syndromes which were grouped together within a single latent class could demonstrate valid distinctions against a different set of external validators.2 Indeed, a recent review found that AN binge-purge subtype, BN, and BED demonstrate predictive validity due to distinctions in course, outcome (including mortality), and treatment response, but demonstrate minimal etiological validity given evidence of shared family transmission and shared neurobiological correlates.2 Diverging evidence of validity might be addressed through the development of different classification schemes, one for clinical settings that emphasizes predictive validity42 and one for research settings that emphasizes etiological validity.6 Current results may facilitate both approaches by identifying how symptoms may perform in statistical models when examined in relation to predictive and etiological validity. Within clinical settings, results suggest that clinicians should remain attuned to the full spectrum of eating disorder symptoms present in their patients regardless of the specific diagnoses that patients receive under the DSM-5. For example, rather than focusing on a single dimension, such as BMI, in patients with AN, results suggest that the cumulative presence of multiple features (low BMI, binge eating, purging) would contribute to illness severity. Although recommended criteria for the DSM-5 eliminate explicit endorsement of weight phobia for AN and place purging in the absence of binge eating among syndromes that are “not elsewhere classified,” attention to the presence of these features is warranted given their grouping with recognized eating disorders in LC1, which was associated with the highest levels of comorbidity, worst psychosocial function, greatest likelihood of trauma histories, and highest treatment needs.
Acknowledgments
This work was supported by grants from the National Institute of Mental Health (R03 MH61320; R01 MH61836; R01 MH63758; PI: Pamela K. Keel).
Footnotes
Financial Disclosure of Interest:
The authors have no financial conflicts of interests to disclose.
References
- 1.American Psychiatric Association. [Accessed December 16, 2011];2010 http://www.dsm5.org/ProposedRevisions/Pages/EatingDisorders.aspx. [Google Scholar]
- 2.Keel PK, Brown TA, Holland LA, Bodell LP. Empirical classification of eating disorders. Annu Rev Clin Psychol. 2012;8:381–404. doi: 10.1146/annurev-clinpsy-032511-143111. 27. [DOI] [PubMed] [Google Scholar]
- 3.Bulik CM, Thornton LM, Root TL, Pisetsky EM, Lichtenstein P, Pedersen NL. Understanding the relation between anorexia nervosa and bulimia nervosa in a Swedish national twin sample. Biol Psychiatry. 2010;67(1):71–77. doi: 10.1016/j.biopsych.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bulik CM, Sullivan PF, Wade TD, Kendler KS. Twin studies of eating disorders: a review. Int J Eat Disord. 2000;27:1–20. doi: 10.1002/(sici)1098-108x(200001)27:1<1::aid-eat1>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 5.Kendler KS, MacLean C, Neale M, Kessler R, Heath A, Eaves L. The genetic epidemiology of bulimia nervosa. Am J Psychiatry. 1991;148:1627–1637. doi: 10.1176/ajp.148.12.1627. [DOI] [PubMed] [Google Scholar]
- 6.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 7.Keel PK, Crosby RD, Holm-Denoma J, et al. Latent structure of bulimic syndromes: An empirical approach utilizing latent profile analyses and taxometric analyses. In: Striegel-Moore RH, Wonderlich SA, Walsh BT, Mitchell JE, editors. Developing an Evidence-Based Classification of Eating Disorders: Scientific Findings for DSM-5. Arlington, VA: American Psychiatric Association; 2011. pp. 145–164. [Google Scholar]
- 8.Muthen B. Should substance use disorders be considered as categorical or dimensional? Addiction. 2006;101(Suppl 1):6–16. doi: 10.1111/j.1360-0443.2006.01583.x. [DOI] [PubMed] [Google Scholar]
- 9.Muthen B, Asparouhov T. Item response mixture modeling: application to tobacco dependence criteria. Addict Behav. 2006;31:1050–1066. doi: 10.1016/j.addbeh.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 10.Keel PK, Wolfe BE, Liddle RA, DeYoung KP, Jimerson DC. Clinical features and physiological response to a test meal in purging disorder and bulimia nervosa. Arch Gen Psychiatry. 2007;64:1058–1066. doi: 10.1001/archpsyc.64.9.1058. [DOI] [PubMed] [Google Scholar]
- 11.Keel PK, Brown TA, Holm-Denoma J, Bodell LP. Comparison of DSM-IV versus proposed DSM-5 diagnostic criteria for eating disorders: reduction of eating disorder not otherwise specified and validity. Int J Eat Disord. 2011;44:553–560. doi: 10.1002/eat.20892. [DOI] [PubMed] [Google Scholar]
- 12.Walsh BT, Sysko R. Broad categories for the diagnosis of eating disorders (BCD-ED): an alternative system for classification. Int J Eat Disord. 2009;42:754–764. doi: 10.1002/eat.20722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lubke GH, Muthen B, Moilanen IK, et al. Subtypes versus severity differences in attention-deficit/hyperactivity disorder in the Northern Finnish Birth Cohort. J Am Acad Child Adolesc Psychiatry. 2007;46:1584–1593. doi: 10.1097/chi.0b013e31815750dd. [DOI] [PubMed] [Google Scholar]
- 14.Hildebrandt T, Langenbucher JW, Carr SJ, Sanjuan P. Modeling population heterogeneity in appearance- and performance-enhancing drug (APED) use: applications of mixture modeling in 400 regular APED users. J Abnorm Psychol. 2007;116:717–733. doi: 10.1037/0021-843X.116.4.717. [DOI] [PubMed] [Google Scholar]
- 15.Keel PK, Striegel-Moore RH. The validity and clinical utility of purging disorder. Int J Eat Disord. 2009;42:706–719. doi: 10.1002/eat.20718. [DOI] [PubMed] [Google Scholar]
- 16.Swanson SA, Lindenberg K, Bauer S, Crosby RD. A Monte Carlo investigation of factors influencing latent class analysis: An application to eating disorder research. Int J Eat Disord. Aug 31; doi: 10.1002/eat.20958. in press. [DOI] [PubMed] [Google Scholar]
- 17.Keel PK, Holm-Denoma JM, Crosby RD. Clinical significance and distinctiveness of purging disorder and binge eating disorder. Int J Eat Disord. 2011;44:311–316. doi: 10.1002/eat.20821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown TA, Haedt-Matt AA, Keel PK. Personality pathology in purging disorder and bulimia nervosa. Int J Eat Disord. 2011;44:735–740. doi: 10.1002/eat.20904. [DOI] [PubMed] [Google Scholar]
- 19.First M, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders--Patient Edition (SCID/P) Biometrics Research Department: New York State Psychiatric Institute; 1995. [Google Scholar]
- 20.Curran PJ, Hussong AM. Integrative data analysis: the simultaneous analysis of multiple data sets. Psychol Methods. 2009;14:81–100. doi: 10.1037/a0015914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keel PK, Mitchell JE, Miller KB, Davis TL, Crow SJ. Long-term outcome of bulimia nervosa. Arch Gen Psychiatry. 1999;56:63–69. doi: 10.1001/archpsyc.56.1.63. [DOI] [PubMed] [Google Scholar]
- 22.Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr. 2002;5:561–565. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]
- 23.Stunkard AJ, Albaum JM. The accuracy of self-reported weights. Am J Clin Nutrition. 1981;34:1593–1599. doi: 10.1093/ajcn/34.8.1593. [DOI] [PubMed] [Google Scholar]
- 24.Mplus (Version 5) [Computer software] Los Angeles, CA: Muthen & Muthen; 2007. [computer program] [Google Scholar]
- 25.Markon KE, Krueger RF. Categorical and continuous models of liability to externalizing disorders: a direct comparison in NESARC. Arch Gen Psychiatry. 2005 Dec;62:1352–1359. doi: 10.1001/archpsyc.62.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wonderlich SA, Crosby RD, Mitchell JE, Engel SG. Testing the validity of eating disorder diagnoses. Int J Eat Disord. 2007;40(Suppl):S40–S45. doi: 10.1002/eat.20437. [DOI] [PubMed] [Google Scholar]
- 27.Butryn ML, Lowe MR, Safer DL, Agras WS. Weight suppression is a robust predictor of outcome in the cognitive-behavioral treatment of bulimia nervosa. J Abnorm Psychol. 2006;115:62–67. doi: 10.1037/0021-843X.115.1.62. [DOI] [PubMed] [Google Scholar]
- 28.Keel PK, Heatherton TF. Weight suppression predicts maintenance and onset of bulimic syndromes at 10-year follow-up. J Abnorm Psychol. 2010;119:268–275. doi: 10.1037/a0019190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wade TD, Crosby R, Martin NG. Use of latent profile analysis to identify eating disorder phenotypes in an adult Australian twin cohort. Arch Gen Psychiatry. 2006;63:1377–1384. doi: 10.1001/archpsyc.63.12.1377. [DOI] [PubMed] [Google Scholar]
- 30.Duncan AE, Bucholz KK, Neuman RJ, Agrawal A, Madden PA, Heath AC. Clustering of eating disorder symptoms in a general population female twin sample: a latent class analysis. Psychol Med. 2007;37:1097–1107. doi: 10.1017/S0033291707000505. [DOI] [PubMed] [Google Scholar]
- 31.Williamson DA, Womble LG, Smeets MA, et al. Latent structure of eating disorder symptoms: a factor analytic and taxometric investigation. Am J Psychiatry. 2002;159:412–418. doi: 10.1176/appi.ajp.159.3.412. [DOI] [PubMed] [Google Scholar]
- 32.Kendell RE. Clinical validity. Psychol Med. 1989;19:45–55. doi: 10.1017/s0033291700011016. [DOI] [PubMed] [Google Scholar]
- 33.Spitzer RL, Yanovski S, Wadden T, et al. Binge eating disorder: its further validation in a multisite study. Int J Eat Disord. 1993;13:137–153. [PubMed] [Google Scholar]
- 34.Grilo CM, Hrabosky JI, White MA, Allison KC, Stunkard AJ, Masheb RM. Overvaluation of shape and weight in binge eating disorder and overweight controls: refinement of a diagnostic construct. J Abnorm Psychol. 2008;117:414–419. doi: 10.1037/0021-843X.117.2.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williamson DA, Gleaves DH, Stewart TM. Categorical versus dimensional models of eating disorders: an examination of the evidence. Int J Eat Disord. 2005;37:1–10. doi: 10.1002/eat.20074. [DOI] [PubMed] [Google Scholar]
- 36.Wonderlich SA, Joiner TE, Jr, Keel PK, Williamson DA, Crosby RD. Eating disorder diagnoses: empirical approaches to classification. Am Psychol. 2007 Apr;62(3):167–180. doi: 10.1037/0003-066X.62.3.167. [DOI] [PubMed] [Google Scholar]
- 37.Haedt AA, Keel PK. Comparing definitions of purging disorder on point prevalence and associations with external validators. Int J Eat Disord. 2009 Jun 17; doi: 10.1002/eat.20712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Keel PK, Fichter M, Quadflieg N, et al. Application of a latent class analysis to empirically define eating disorder phenotypes. Arch Gen Psychiatry. 2004;61:192–200. doi: 10.1001/archpsyc.61.2.192. [DOI] [PubMed] [Google Scholar]
- 39.Eddy KT, Crosby RD, Keel PK, et al. Application of latent profile analysis to empirically identify eating disorder phenotypes in a clinical sample. J Nerv Ment Dis. 2009;197:41–49. doi: 10.1097/NMD.0b013e3181927389. [DOI] [PubMed] [Google Scholar]
- 40.Thomas JJ, Vartanian LR, Brownell KD. The relationship between eating disorder not otherwise specified (EDNOS) and officially recognized eating disorders: meta-analysis and implications for DSM. Psychol Bull. 2009;135:407–433. doi: 10.1037/a0015326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kendler KS. The nosologic validity of paranoia (simple delusional disorder). A review. Arch Gen Psychiatry. 1980;37:699–706. doi: 10.1001/archpsyc.1980.01780190097012. [DOI] [PubMed] [Google Scholar]
- 42.Walsh BT. DSM-V from the perspective of the DSM-IV experience. Int J Eat Disord. 2007 Nov;(40 Suppl):S3–S7. doi: 10.1002/eat.20397. [DOI] [PubMed] [Google Scholar]