ABSTRACT
BACKGROUND
African Americans are significantly more likely than whites to have uncontrolled hypertension, contributing to significant disparities in cardiovascular disease and events.
OBJECTIVE
The goal of this study was to examine whether there were differences in change in blood pressure (BP) for African American and non-Hispanic white patients in response to a medication management and tailored nurse-delivered telephone behavioral program.
PARTICIPANTS
Five hundred and seventy-three patients (284 African American and 289 non-Hispanic white) primary care patients who participated in the Hypertension Intervention Nurse Telemedicine Study (HINTS) clinical trial.
INTERVENTIONS
Study arms included: 1) nurse-administered, physician-directed medication management intervention, utilizing a validated clinical decision support system; 2) nurse-administered, behavioral management intervention; 3) combined behavioral management and medication management intervention; and 4) usual care. All interventions were activated based on poorly controlled home BP values.
MAIN MEASURES
Post-hoc analysis of change in systolic and diastolic blood pressure. General linear models (PROC MIXED in SAS, version 9.2) were used to estimate predicted means at 6-month, 12-month, and 18-month time points, by intervention arm and race subgroups (separate models for systolic and diastolic blood pressure).
KEY RESULTS
Improvement in mean systolic blood pressure post-baseline was greater for African American patients in the combined intervention, compared to African American patients in usual care, at 12 months (6.6 mmHg; 95 % CI: -12.5, -0.7; p = 0.03) and at 18 months (9.7 mmHg; -16.0, -3.4; p = 0.003). At 18 months, mean diastolic BP was 4.8 mmHg lower (95 % CI: -8.5, -1.0; p = 0.01) among African American patients in the combined intervention arm, compared to African American patients in usual care. There were no analogous differences for non-Hispanic white patients.
CONCLUSIONS
The combination of home BP monitoring, remote medication management, and telephone tailored behavioral self-management appears to be particularly effective for improving BP among African Americans. The effect was not seen among non-Hispanic white patients.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-012-2138-x) contains supplementary material, which is available to authorized users.
KEY WORDS: hypertension, telemedicine, self-management, adherence, veterans
Hypertension is the leading single modifiable risk factor for cardiovascular disease, stroke, and related events.1,2 Approximately three in ten adults in the United States have hypertension (blood pressure (BP) ≥ 140/90 mmHg or taking BP medication).3,4 Hypertension is significantly more common among African American adults (prevalence of 41 %) than non-Hispanic whites (prevalence of 28 %).5 The odds of having uncontrolled hypertension are 40 % greater in non-Hispanic African Americans than in non-Hispanic whites.6 Further, psychosocial risk factors for hypertension may have differing impacts among African Americans and whites.7,8 As a result of these disparities and the importance of providing culturally-appropriate disease-management programs, there is a need to analyze data from hypertension disease-management trials with sufficient numbers of African American and non-African American patients to better understand the impact of interventions among different patient populations.
A recently completed clinical trial examined the impact of telemonitoring of blood pressure, nurse-administered telephone medication management, and telephone tailored behavioral management as possible ways to extend care beyond the clinic. We conducted a post-hoc analysis of trial results from that study to determine whether there were differences in how African American and non-Hispanic white patients responded to this patient-centered intervention.
METHODS
Details of the design and primary results of the Hypertension Intervention Nurse Telemedicine Study (HINTS) have been published previously.9–11 The study evaluated three telephone-based interventions through a four-group design: 1) nurse-administered, physician directed medication management intervention, utilizing a validated clinical decision support (CDS) system; 2) nurse-administered, behavioral management intervention; 3) combined behavioral management and medication management intervention; and 4) usual care. Interventions were activated based on home BP measurements collected via telemonitoring.
The trial was approved by the Institutional Review Board of the Durham, NC Veterans Affairs (VA) Medical Center. All subjects provided written informed consent.
Setting and Timing
The intervention was delivered in the primary care clinics of a tertiary care Veterans Affairs Medical Center in Durham, North Carolina. Study recruitment started in May 2006, and the final 18-month follow-up appointment was completed in July 2009.
Patient Eligibility and Randomization
All eligible patients received care through the primary care clinics at the Durham VAMC. To be approached regarding the possibility of participating, patients had to: 1) have a diagnosis of hypertension; 2) be using a BP-lowering medication; and 3) have inadequate BP control (mean of >140/90 mmHg VA clinical blood pressures over the last year). Patients were excluded if they: 1) received dialysis; 2) had a serum creatinine >2.5 or no documentation of renal function; 3) ever had an organ transplant; 4) were hospitalized for stroke, myocardial infarction, or coronary artery revascularization within the previous 3 months; 5) had a diagnosis of metastatic cancer or dementia; 6) did not have a home telephone; 7) resided in a nursing home; 8) received home healthcare; or 9) had severely impaired hearing or speech (due to the need to interact over the phone). As a result of different blood pressure goals,1 patient randomization was stratified by diabetes status.
Interventions
All patients randomized to one of the three intervention arms were provided a wireless home BP monitor (A&D Medical Digital Blood Pressure, Model UA-767PC) and telemedicine device (Carematix Inc., Model #102), and were advised to take their BP once every other day. Measurements were automatically transmitted to a secure computer server over telephone lines. Both the medication management and behavioral management interventions were initiated in response to an average home BP above pre-specified treatment goals over a 2-week period.
Because home BP measurements average 6–8 SBP/5-6 DBP mmHg lower than values obtained during routine clinic visits,12 intervention trigger alerts were designed based on a 2-week average home BP of ≥135/85 mmHg for non-diabetics.13 Concern over the possibility of treatment goals leading to excessively low diastolic BPs for patients with diabetes resulted in basing the trigger alerts on a 2-week home BP average of ≥135/80 mmHg for diabetic patients.11 A safety alert was activated if two consecutive home BP measurements recorded at least 12 hours apart were greater than 175/105 mmHg. In such an instance, a nurse contacted the patient and initiated an approved safety protocol.
Study Arm 1: Home BP Monitoring with Remote Medication Management
In addition to home BP monitoring, patients randomized to this arm received remote medication management, based on algorithmic medication suggestions that were reviewed by a study physician. Medications suggestions were triggered based on home BP values.
Upon triggering the medication management intervention, a nurse notified a study physician, and provided the physician with a medication change recommendation based upon decision-support software.14 The study physician reviewed the patient’s BP, medication, and adherence (based on patient report and prescription refill data) with the nurse and decided whether to change hypertension medication.15 The nurse communicated recommended changes to the patient, while the study physician electronically prescribed the medication and generated a note in the patient’s medical record that was co-signed by the patient’s primary care provider. The nurse called the patient 3 weeks after the medication change to obtain reports of adverse effects and address patient questions. A patient’s home BP values were reassessed at 6 weeks to determine if a medication change should be triggered again. Patients who maintained adequate BP control did not activate medication management review, but were contacted every 6 months to reinforce their positive behavior.
Study Arm 2: Home BP Monitoring with Behavioral Management Intervention
In addition to home BP monitoring, patients who met the target home BP thresholds described above received a behavioral management intervention, consisting of up to 11 tailored health behavior modules focused on improving hypertension self-management, delivered over the phone by a study nurse. Topics potentially covered included: hypertension knowledge, medication adverse events, memory related to taking medicine, social/medical environment, patient-provider relationship, stress reduction, diet, exercise, weight, smoking, and alcohol. Any difference in the number of encounters delivered was the result of triggering the encounters at different points over the course of the 18-month intervention period when the target home BP thresholds were met. Patients who maintained adequate BP control did not activate the behavioral intervention, but were contacted every 6 months to reinforce their positive behavior.
To ensure that the tailored information was standardized, the nurse used an intervention software application that contained predetermined scripts and patient-specific tailored algorithms for the modules. Each encounter consisted of three or four of the topics listed above, and lasted 10–15 minutes. Individuals in the behavioral only arm did not receive medication management.
Study Arm 3: Combined Intervention
In this arm, patients received the full dose of each intervention [home monitoring + triggered medication management + triggered behavioral intervention]. If triggered based on the home BP measurements, the nurse initially addressed recommended medication adjustments using the established method described above, followed by the tailored behavioral intervention.
Study Arm 4: Usual Care
Patients in all four arms received primary care and management of hypertension according to the discretion of their primary care provider. Usual care patients received no contact with the intervention nurses and did not receive home telemonitoring equipment. There was also no interaction between study staff and primary care providers in relation to usual care patients.
Study Outcome
The present paper examines the intervention group effect upon mean systolic and diastolic BPs at 6, 12 and 18 months of study follow-up. At each measurement point (baseline visit and follow-up visit at 6, 12, and 18 months), a research assistant masked to intervention arms asked patients to rest for 5 minutes before obtaining two BP measures using BpTRU digital BP monitors (Coquitlam, BC, Canada), model BPM-100.16
Analyses
The primary goal was to compare the effects of the intervention arms relative to usual care on systolic and diastolic BP within African American and non-Hispanic white patient subgroups over time. For both systolic and diastolic BPs, general linear models (PROC MIXED in SAS, version 9.2) were used to estimate predicted means at 6-month, 12-month, and 18-month time points, by intervention arm and race subgroups. This modeling approach was used to appropriately handle patients with incomplete follow-up data.17 The outcome variable in these models was the study BP at baseline, 6, 12, and 18 months. The final model parameters included a common intercept for non-Hispanic white patients, a common intercept for African American patients, dummy-coded time, intervention arms interacted with each follow-up time point; each of these terms interacted with race to estimate the differential BP trajectories for African American and non-Hispanic white patients by intervention arm. Estimates and confidence intervals from this model were then used to test for BP differences in the intervention groups relative to usual care at 6, 12, and 18 months within the African American and non-Hispanic white subgroups. An unstructured covariance was included to account for patients’ repeated measurements over time.
All patients who provided self-reported race information and randomized to one of the four arms (n = 573) were included in the analyses. All eligible patients that were randomized were included in the analysis, and analyzed according to their treatment assignment. All available data from these patients, including those who subsequently discontinued the study, were also used in the general linear models fit with full-likelihood methods.
RESULTS
Patients
The distribution of self-reported race of the 591 study patients included in the original trial analysis was 48.1 % (n = 284) African American; 49.1 % (n = 289) non-Hispanic white, 1.0 % (n = 6) Hispanic, 1.9 % (n = 11) other race/ethnicity, and 0.2 % (n = 1) refused. In this context, other race/ethnicity is defined as a self-report of a race/ethnic category other than African America or non-Hispanic white. Because of low numbers, the data for the six Hispanic patients, the 11 patients with race/ethnicity other than African American or non-Hispanic white, and the one participant who refused to provide race/ethnicity information, were excluded from the current analyses.
Among the 573 patients contributing data to this study, 91.8 % were male and the mean age was 63.5 years (SD = 10.3). Fifty-nine percent of participants had their study-measured BP under control at baseline. Inadequate baseline BP control was defined as an SBP ≥140 mmHg or a DBP ≥90 mmHg for participants without diabetes, and an SBP ≥130 mmHg or a DBP ≥80 mmHg for participants with diabetes. Mean baseline SBP/DBP was 130.5/80.3 mmHg among African American and 127.8/74.5 mmHg among non-Hispanic white patients. Patient characteristics can be found in Table 1.
Table 1.
Hypertension Intervention Nurse Telemedicine Study (HINTS) Baseline Sample Characteristics, Overall and Stratified by Race
| Baseline Characteristics* | Total (n = 573) | African American (n = 284) | White (n = 289) | p-value |
|---|---|---|---|---|
| Demographics | ||||
| Age (Mean age (SD)) | 63.5 (10.3) | 60.9 (10.5) | 66.1 (9.5) | <0.001 |
| Male | 91.8 % | 90.5 % | 93.1 % | 0.26 |
| Married | 65.4 % | 58.5 % | 72.3 % | <0.001 |
| Completed ≥ high school education | 86.7 % | 87.7 % | 85.8 % | 0.43 |
| Low literacy level (< 9th grade; REALM Score ≤60)† | 38.2 % | 45.8 % | 30.8 % | <0.001 |
| Employed | 35.1 % | 37.0 % | 33.2 % | 0.35 |
| Inadequate income‡ | 18.2 % | 22.9 % | 13.5 % | 0.003 |
| Currently smokes | 20.6 % | 19.0 % | 22.1 % | 0.35 |
| Body mass index (Mean BMI (SD)) | 30.4 (5.3) | 30.7 (5.5) | 30.0 (5.1) | 0.11 |
| Self-reported medication non-adherence § | 45.7 % | 51.4 % | 40.1 % | 0.007 |
| High blood pressure is a serious or very serious problem | 96.3 % | 98.2 % | 94.5 % | 0.04 |
| Medical History | ||||
| >10 year history of high blood pressure (patient reported) | 74.7 % | 78.5 % | 70.9 % | 0.05 |
| Number of hypertension‖ medications (mean (SD) | 2.4 (1.2) | 2.6 (1.2) | 2.2 (1.1) | 0.003 |
| Diabetic | 43.1 % | 45.4 % | 40.8 % | 0.27 |
| Baseline Blood Pressure¶ | ||||
| Systolic (Mean mmHg (SD)) | 129.1 (19.6) | 130.5 (20.3) | 127.8 (18.8) | 0.09 |
| Diastolic (Mean mmHg (SD)) | 77.4 (13.1) | 80.3 (13.2) | 74.5 (12.4) | <0.001 |
| Inadequate blood pressure control# | 41.2 % | 45.4 % | 37.0 % | 0.04 |
* All data except blood pressure , diabetes status, age, body mass index, and number of diabetes medications, were patient-reported based on direct question or patient-completed measure. When missing values existed, they were included in the calculation of percentages
† Literacy was determined using the Rapid Estimate of Adult Literacy (REALM)36
‡ Inadequate income defined as reporting difficulty paying bills no matter what was done or having money to pay the bills only because cut back on things
§ Self-reported non-adherence was assessed using a four-item measure based on Morisky scale.37 Response options ranged from strongly agree (1) to strongly disagree (4). A summary binary variable was created by coding those who responded “strongly agree”, “agree”, “don’t know” or “refused” to any of the four questions as non-adherent; otherwise, patients were coded as adherent
‖ Means are for the n = 501 VA patients whose prescribed hypertension medication fills, as recorded in the national VA database, overlapped with their baseline interview date
¶ When patients had multiple blood pressure readings during their baseline visit, mean systolic and mean diastolic readings were used as the baseline blood pressure values
# Defined as a SBP ≥140 mmHg or a DBP ≥90 mmHg for individuals without diabetes, and SBP ≥130 mmHg or a DBP ≥80 mmHg for individuals with diabetes
No crossover among study groups occurred. No study-related adverse events occurred in any intervention group. Overall, BP measurements were available for 489 (85 %) patients at the 18-month follow-up [248 (87 %) for African American patients; 241 (83 %) for non-Hispanic white patients]. Completion rates of 18-month follow-up were similar across study arms (83 %-90 %).
Intervention Activation
Over the 18-month intervention period, 197 of the 223 (88 %) African American intervention patients triggered an alert for the nurse to conduct an intervention call as a result of poor BP control. One hundred and eighty-six of the 216 (86 %) white intervention patients triggered an alert. There were a total number of 1039 intervention alerts among African American patients and 888 intervention alerts among non-Hispanic white patients. The number of intervention alerts by race and study arm can be found in online Appendix 1.
Differences in Mean Blood Pressure
The overall race by time by intervention arm effect (9 df test) provided evidence of differential intervention effects over time for African American and non-Hispanic white patients for both systolic BP ( ; p < 0.001) and diastolic BP (
; p < 0.001) and diastolic BP ( ; p < 0.001). Relative to usual care, at 12 months for African American patients, the mean systolic BP was 6.6 mmHg lower (95 % CI: -12.5, -0.7; p = 0.03) in the combined intervention group. However, at 12 months, non-Hispanic white patients in the combined intervention group had BP 1.5 mmHg lower (95 % CI: -7.7, 4.7; p = 0.64), compared to usual care. No other differences in systolic BP were statistically significant between arms at 6 or 12 months (Table 2).
; p < 0.001). Relative to usual care, at 12 months for African American patients, the mean systolic BP was 6.6 mmHg lower (95 % CI: -12.5, -0.7; p = 0.03) in the combined intervention group. However, at 12 months, non-Hispanic white patients in the combined intervention group had BP 1.5 mmHg lower (95 % CI: -7.7, 4.7; p = 0.64), compared to usual care. No other differences in systolic BP were statistically significant between arms at 6 or 12 months (Table 2).
Table 2.
Estimated Differences (95 % CI) in Blood Pressure Between HINTS Intervention and Usual Care Groups at 6, 12 and 18 Months for Race Subgroups, n =573 (284 African American; 289 white)
| Outcome/Subgroup/Time Period | Behavioral Management vs. Usual Care | Medication Management vs. Usual Care | Combined vs. Usual Care |
|---|---|---|---|
| Systolic Blood Pressure* | |||
| African American | |||
| 6 months | -2.8 (95 % CI -8.9, 3.3) | 0.8 (95 % CI -5.2, 6.8) | -1.2 (95 % CI -7.0, 4.6) |
| 12 months | -2.3 (95 % CI -8.3, 3.7) | -2.4 (95 % CI -8.4, 3.6) | -6.6 (95 % CI-12.5, -0.7) |
| 18 months | -0.3 (95 % CI -6.7, 6.0) | -2.5 (95 % CI -8.9, 3.9) | -9.7 (95 % CI-16.0, -3.4) |
| White | |||
| 6 months | 5.0 (95 % CI -0.8, 10.8) | -2.1 (95 % CI -8.0, 3.8) | -0.4 (95 % CI -6.5, 5.7) |
| 12 months | -1.3 (95 % CI -7.2, 4.6) | -2.8 (95 % CI -8.7, 3.1) | -1.5 (95 % CI -7.7, 4.7) |
| 18 months | 4.6 (95 % CI -1.6, 10.9) | 0.6 (95 % CI -5.8, 6.9) | 3.1 (95 % CI -3.5, 9.7) |
| Diastolic Blood Pressure* | |||
| African American | |||
| 6 months | -0.6 (95 % CI -4.1, 2.9) | 0.7 (95 % CI -2.8, 4.1) | -1.4 (95 % CI -4.7, 2.0) |
| 12 months | 0.0 (95 % CI -3.7, 3.8) | -0.2 (95 % CI -3.9, 3.5) | -1.1 (95 % CI -4.8, 2.5) |
| 18 months | -0.7 (95 % CI -4.5, 3.1) | 0.1 (95 % CI -3.8, 3.9) | -4.8 (95 % CI-8.5, -1.0) |
| White | |||
| 6 months | 1.3 (95 % CI -2.0, 4.7) | -2.9 (95 % CI -6.3, 0.5) | 1.0 (95 % CI -2.6, 4.5) |
| 12 months | -1.1 (95 % CI -4.7, 2.6) | -1.5 (95 % CI -5.1, 2.2) | 1.5 (95 % CI -2.3, 5.4) |
| 18 months | 1.9 (95 % CI -1.8, 5.6) | -0.6 (95 % CI -4.4, 3.2) | 2.4 (95 % CI -1.5, 6.4) |
*Systolic and diastolic blood pressure estimates were based on a longitudinal data model with an unstructured covariance matrix
Negative differences reflect improvement (i.e. decreased blood pressure) compared to usual care, and positive differences reflect worsening (i.e. increased blood pressure) compared to usual care
The model-estimated systolic blood pressure correlation between time points ranged from 0.26 to 0.41. The estimated diastolic blood pressure correlation between time points ranged from 0.41 to 0.53
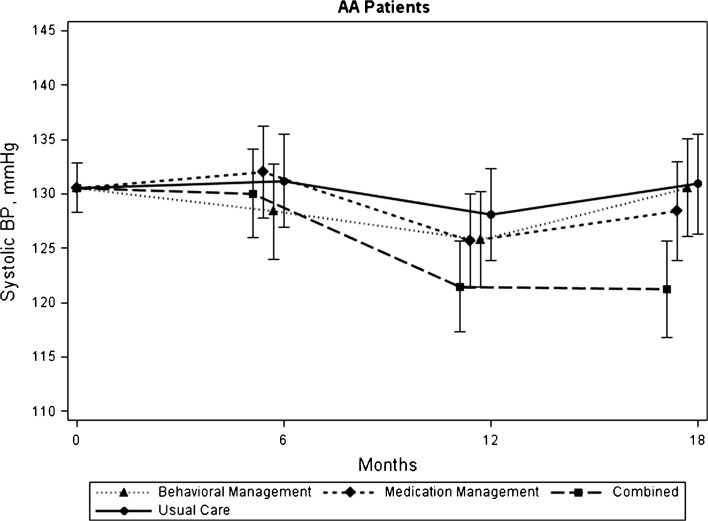
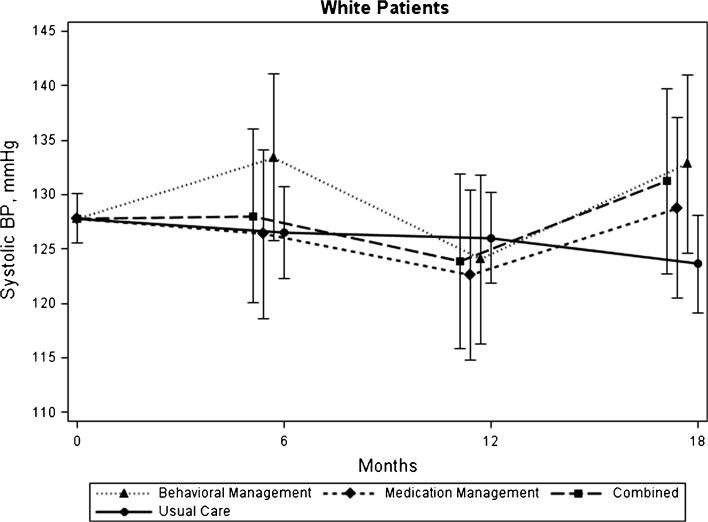
Analogous results are still seen at 18 months. For African American patients at 18 months, the mean systolic BP was -0.3 mmHg lower (95 % CI: -6.7, 6.0; p = 0.91) in the behavioral management group, -2.5 mmHg lower (95 % CI: -8.9, 3.9; p = 0.45) in the medication management group, and -9.7 mmHg lower (95 % CI: -16.0, -3.4 mmHg; p = 0.003) in the combined intervention group, relative to usual care. However, for non-Hispanic white patients at 18 months , the mean systolic BP was 4.6 mmHg higher (95 % CI: -1.6, 10.9 mmHg; p = 0.14) in the behavioral management group, 0.6 mmHg higher (95 % CI: -5.8, 6.9 mmHg; p = 0.86) in the medication management group, and 3.1 mmHg higher (95 % CI: -3.5, 9.7 mmHg; p = 0.36) in the combined intervention group, relative to usual care. Please see Table 2 and Figures 1 and 2.
Figure 1.
Estimated (Bars represent 95 % CIs. BP = blood pressure. Estimates are based on a longitudinal data model with unstructured covariance matrix) systolic blood pressure from baseline to 18 months, by intervention group – among African American patients, n = 284.
Figure 2.
Estimated (Bars represent 95 % CIs. BP = blood pressure. Estimates are based on a longitudinal data model with unstructured covariance matrix) systolic blood pressure from baseline to 18 months, by intervention group – among white patients, n = 289.
The only statistically significant difference in diastolic BP between any intervention group relative to the usual care group was that by 18 months among African American patients, mean diastolic BP was 4.8 mmHg lower (95 % CI: -8.5, -1.0 mmHg; p = 0.01) for patients in the combined intervention arm, compared to usual care (see Table 2).
DISCUSSION
In a post-hoc analysis, we examined differences by race in the effects of medication management, behavioral self-management support, and a combination of the two interventions delivered by telephone and activated by home BP monitoring, among adults with hypertension treated in VA primary care. The combined intervention was effective among African American patients by 12 and 18 months: however, the intervention was not as effective among non-Hispanic white patients.
Differences in the intervention effect observed in the present study are similar to differences seen in a study of home BP monitoring plus behavioral phone calls (without medication management) conducted at two university-affiliated primary care practices in the same city as the present study. In that study, we observed a stronger intervention effect on BP control for non-white (predominantly African American) patients when testing a combination of home BP monitoring and a nurse-delivered telephone behavioral intervention.18 The consistency of the two findings occurred despite key differences in the two study populations (e.g., higher proportion female subjects [66 % in previous study], non-VA setting, and differing patterns of baseline hypertension control).
Related results have also been seen among VA patients in a telephone osteoarthritis self-management program delivered using scripted telephone calls and goal setting over the phone. In that study, nonwhite patients reported that they perceived scripted phone calls and educational materials to be more helpful than white patients.19 These phone calls were delivered in a similar fashion as those in the HINTS study, pointing to a possible difference in the way self-management materials are received by race (not measured for the HINTS study).
The fact that the combination of medication management and tailored behavioral self-management support was effective among African American patients while the individual interventions were not, points to the notion that hypertension, like other illnesses, is a biopsychosocial condition.8,20 While there are clear biologic risk factors for uncontrolled hypertension that can be addressed by medication, there are also behavioral factors such as medication adherence, exercise, and diet.21–23 These behavioral issues may be impacted by a number of social and cultural factors, such as perception of hypertension risk, interaction with the healthcare system, trust in the healthcare system, and social support.8,24–26 All of these may be further impacted by underlying patient characteristics, such as level of stress, health literacy, and self-efficacy in relation to managing hypertension and treatment side effects.8,27
While the exact reason(s) for the differences in intervention impact by race are unclear, there is evidence that African Americans and whites may, as groups, have differences in many of the important biopsychosocial issues described above. For example, there is evidence of different patterns of interaction with the healthcare system,28 and differences in BP responses to reductions in sodium in the diet.29,30 Further, Kressin et al. (2010) found that African Americans have different patterns of beliefs concerning hypertension (e.g. belief that high blood pressure is largely due to an individual’s behavior). Accounting for these differences in regression modeling attenuates associations between race and blood pressure.31 This attenuation indicates that disparities in hypertension may be associated with differences in beliefs about the illness, which can potentially be targeted through disease management interventions. As described in the methods section, the behavioral intervention, which was combined with medication management in the combined arm, covered many of the psychosocial and disease-perception issues that may impact blood pressure control. Further, it has been previously reported, using HINTS data, that patient race was not associated with study physicians’ deciding to intensify medication regimens,15 indicating that results in this paper were not the result of differing medication treatment decisions. The combination of the medication management and addressing psychosocial factors related to hypertension may have impacted different issues among African American and white patients.
Two other possible explanations for the observed differences in intervention impact by race are: improved access to care for under-represented individuals, available in the VA healthcare system; and potential synergistic effect of behavior and medication management.
This study has several potential limitations. Data were limited to only African Americans and non-Hispanic whites seen in primary care clinics at one tertiary care VA Medical Center. Furthermore, our study was not designed to detect treatment differences in patient subgroups; therefore, our ability to provide definitive evidence of a differential treatment response by race was somewhat limited. Finally, the comprehensive nature of the self-management intervention makes it difficult to discern which aspects of our intervention were the most beneficial.
The rate of cardiovascular disease and related events is significantly greater among African Americans than whites, upwards of 30–300 %, depending on the specific condition.4,32–34 While all patients must be treated as individuals, this paper adds to the growing body of literature suggesting that the utilization of patient-centered disease management interventions that address both medical and behavioral aspects of hypertension outside of the traditional healthcare setting may be especially beneficial for African Americans. Such interventions could possibly: be included as components of patient-centered medical homes seeking to improve access to care, enhance chronic illness management, and reduce health disparities.35
Electronic Supplementary Material
(DOCX 16 kb)
Acknowledgements
Sources of Funding
This research is supported by a grant from Veterans Affairs, Health Services Research and Development (VA HSR&D) (IIR 04-426). Dr. Bosworth is supported by a VA HSR&D Research Career Scientist award (RCS 08-027) and an Established Investigator Award from American Heart Association. Dr. Powers is supported by a VA HSR&D Career Development Award (CDA 09-212). ATHENA-HTN development and testing was supported in part by VA HSR&D (CPI 99-275, IMV-04-062).
Conflict of Interest
The authors declare that they do not have a conflict of interest. All authors are employees of the Department of Veterans Affairs. No author received compensation for preparation of this manuscript, apart from his or her employment.
Disclaimer
The views expressed in this article are those of the authors, and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the United States government, or Duke University.
Footnotes
Clinical Trial Registration
Trial Registration: ClinicalTrials.gov
Clinical TrialsRegistration #: NCT00237692
Registry URL: http://www.clinicaltrials.gov
REFERENCES
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The jnc 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, Creager MA, Culebras A, Eckel RH, Hart RG, Hinchey JA, Howard VJ, Jauch EC, Levine SR, Meschia JF, Moore WS, Nixon JV, Pearson TA. Guidelines for the primary prevention of stroke: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 3.Egan BM, Zhao Y, Axon RN. Us trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O'Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y. Heart disease and stroke statistics–2009 update: A report from the american heart association statistics committee and stroke statistics subcommittee. Circulation. 2009;119:480–486. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- 5.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 6.Ostchega Y, Hughes JP, Wright JD, McDowell MA, Louis T. Are demographic characteristics, health care access and utilization, and comorbid conditions associated with hypertension among us adults? Am J Hypertens. 2008;21:159–165. doi: 10.1038/ajh.2007.32. [DOI] [PubMed] [Google Scholar]
- 7.James SA. John henryism and the health of african-americans. Cult Med Psychiatry. 1994;18:163–182. doi: 10.1007/BF01379448. [DOI] [PubMed] [Google Scholar]
- 8.Bosworth HB, Oddone EZ. A model of psychosocial and cultural antecedents of blood pressure control. J Natl Med Assoc. 2002;94:236–248. [PMC free article] [PubMed] [Google Scholar]
- 9.Bosworth HB, Olsen MK, McCant F, Harrelson M, Gentry P, Rose C, Goldstein MK, Hoffman BB, Powers B, Oddone EZ. Hypertension intervention nurse telemedicine study (hints): Testing a multifactorial tailored behavioral/educational and a medication management intervention for blood pressure control. Am Heart J. 2007;153:918–924. doi: 10.1016/j.ahj.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 10.McCant F, McKoy G, Grubber J, Olsen MK, Oddone E, Powers B, Bosworth HB. Feasibility of blood pressure telemonitoring in patients with poor blood pressure control. J. Telemed. Telecare. 2009;15:281–285. doi: 10.1258/jtt.2009.090202. [DOI] [PubMed] [Google Scholar]
- 11.Bosworth HB, Powers BJ, Olsen MK, McCant F, Grubber J, Smith V, Gentry PW, Rose C, Van Houtven C, Wang V, Goldstein MK, Oddone EZ. Home blood pressure management and improved blood pressure control: Results from a randomized controlled trial. Arch Intern Med. 2011;171:1173–1180. doi: 10.1001/archinternmed.2011.276. [DOI] [PubMed] [Google Scholar]
- 12.Weisser B, Mengden T, Dusing R, Vetter H, Vetter W. Normal values of blood pressure self-measurement in view of the 1999 world health organization-international society of hypertension guidelines. Am J Hypertens. 2000;13:940–943. doi: 10.1016/S0895-7061(00)00259-4. [DOI] [PubMed] [Google Scholar]
- 13.Staessen JA, Thijs L. Development of diagnostic thresholds for automated self-measurement of blood pressure in adults. First international consensus conference on blood pressure self-measurement. Blood Press Monit. 2000;5:101–109. doi: 10.1097/00126097-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Goldstein MK, Coleman RW, Tu SW, Shankar RD, O'Connor MJ, Musen MA, Martins SB, Lavori PW, Shlipak MG, Oddone E, Advani AA, Gholami P, Hoffman BB. Translating research into practice: Organizational issues in implementing automated decision support for hypertension in three medical centers. J Am Med Inform Assoc. 2004;11:368–376. doi: 10.1197/jamia.M1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crowley MJ, Smith VA, Olsen MK, Danus S, Oddone EZ, Bosworth HB, Powers BJ. Treatment intensification in a hypertension telemanagement trial: Clinical inertia or good clinical judgment? Hypertension. 2011;58:552–558. doi: 10.1161/HYPERTENSIONAHA.111.174367. [DOI] [PubMed] [Google Scholar]
- 16.Wright BM, Dore CF. A random-zero sphygmomanometer. Lancet. 1970;1:337–338. doi: 10.1016/s0140-6736(70)90709-9. [DOI] [PubMed] [Google Scholar]
- 17.Fitzmaurice G, Laird NM, Ware JH. Applied longitudinalanalysis. New York: Wiley Series in Probability and Statistics; 2004. [Google Scholar]
- 18.Bosworth HB, Olsen MK, Grubber JM, Powers BJ, Oddone EZ. Racial differences in two self-management hypertension interventions. Am J Med. 2011;124:468. doi: 10.1016/j.amjmed.2010.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sperber NR, Bosworth HB, Coffman CJ, Juntilla KA, Lindquist JH, Oddone EZ, Walker TA, Weinberger M, Allen KD. Participant evaluation of a telephone-based osteoarthritis self-management program, 2006-2009. Preventing chronic disease. 2012;9:E73. [PMC free article] [PubMed] [Google Scholar]
- 20.Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 21.Chobanian AV. Shattuck lecture. The hypertension paradox–more uncontrolled disease despite improved therapy. N Engl J Med. 2009;361:878–887. doi: 10.1056/NEJMsa0903829. [DOI] [PubMed] [Google Scholar]
- 22.Elmer PJ, Obarzanek E, Vollmer WM, Simons-Morton D, Stevens VJ, Young DR, Lin PH, Champagne C, Harsha DW, Svetkey LP, Ard J, Brantley PJ, Proschan MA, Erlinger TP, Appel LJ. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485–495. doi: 10.7326/0003-4819-144-7-200604040-00007. [DOI] [PubMed] [Google Scholar]
- 23.Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302:401–411. doi: 10.1001/jama.2009.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borzecki AM, Oliveria SA, Berlowitz DR. Barriers to hypertension control. Am Heart J. 2005;149:785–794. doi: 10.1016/j.ahj.2005.01.047. [DOI] [PubMed] [Google Scholar]
- 25.Powers BJ, Oddone EZ, Grubber JM, Olsen MK, Bosworth HB. Perceived and actual stroke risk among men with hypertension. J Clin Hypertens (Greenwich). 2008;10:287–294. doi: 10.1111/j.1751-7176.2008.07797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naik AD, Kallen MA, Walder A, Street RL., Jr Improving hypertension control in diabetes mellitus: The effects of collaborative and proactive health communication. Circulation. 2008;117:1361–1368. doi: 10.1161/CIRCULATIONAHA.107.724005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 28.National healthcaredisparities report,2008. Rockville, MD: Agency for Health Research and Quality; 2009 March
- 29.Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG, Conlin PR, Svetkey LP, Erlinger TP, Moore TJ, Karanja N. Effects of diet and sodium intake on blood pressure: Subgroup analysis of the dash-sodium trial. Ann Intern Med. 2001;135:1019–1028. doi: 10.7326/0003-4819-135-12-200112180-00005. [DOI] [PubMed] [Google Scholar]
- 30.Svetkey LP, Simons-Morton D, Vollmer WM, Appel LJ, Conlin PR, Ryan DH, Ard J, Kennedy BM. Effects of dietary patterns on blood pressure: Subgroup analysis of the dietary approaches to stop hypertension (dash) randomized clinical trial. Arch Intern Med. 1999;159:285–293. doi: 10.1001/archinte.159.3.285. [DOI] [PubMed] [Google Scholar]
- 31.Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3:173–180. doi: 10.1161/CIRCOUTCOMES.109.860841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hozawa A, Folsom AR, Sharrett AR, Chambless LE. Absolute and attributable risks of cardiovascular disease incidence in relation to optimal and borderline risk factors: Comparison of african american with white subjects–atherosclerosis risk in communities study. Arch Intern Med. 2007;167:573–579. doi: 10.1001/archinte.167.6.573. [DOI] [PubMed] [Google Scholar]
- 33.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, Copper LS, Shahar E. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the atherosclerosis risk in communities (aric) cohort. Stroke. 1999;30:736–743. doi: 10.1161/01.STR.30.4.736. [DOI] [PubMed] [Google Scholar]
- 34.Smith SR, Svetkey LP, Dennis VW. Racial differences in the incidence and progression of renal diseases. Kidney Int. 1991;40:815–822. doi: 10.1038/ki.1991.281. [DOI] [PubMed] [Google Scholar]
- 35.Vest JR, Bolin JN, Miller TR, Gamm LD, Siegrist TE, Martinez LE. Medical homes: "Where you stand on definitions depends on where you sit". Med Care Res Rev. 2010;67:393–411. doi: 10.1177/1077558710367794. [DOI] [PubMed] [Google Scholar]
- 36.Davis TC, Crouch MA, Long SW, Jackson RH, Bates P, George RB, Bairnsfather LE. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23:433–435. [PubMed] [Google Scholar]
- 37.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 16 kb)