Abstract
BACKGROUND
Assessment and treatment of pain are based largely on patient’s self reports. Patients with limited English proficiency (LEP) may have difficulties communicating their pain symptoms in the presence of language barriers.
OBJECTIVE
To determine whether interpreter use was associated with quality of acute pain treatment among Latina patients with limited English proficiency.
DESIGN
Secondary analysis of two cross-sectional surveys.
PARTICIPANTS
One hundred and eighty-five Latino female patients hospitalized for obstetric and gynecological care who required interpreter services. Patients were classified into two groups according to interpreter availability ('Always' and 'Not Always' available).
MAIN MEASURES
Quality of pain treatment was measured by patient report of 1) overall level of pain control during hospitalization; 2) timeliness of pain treatment; and 3) perceived provider helpfulness to treat pain.
KEY RESULTS
Patients who always received interpreters were more likely to report higher levels of pain control (P = 0.02), timely pain treatment (P = 0.02), and greater perceived provider helpfulness to treat their pain (P = 0.005), compared with patients who not always received interpreters.
CONCLUSION
Use of interpreters by LEP patients was associated with better patient reports on quality of pain treatment, and may also improve clinical interactions related to pain.
KEY WORDS: interpreters, limited English proficiency, Latinos/Latinas, pain, pain treatment
INTRODUCTION
Pain continues to be the most common medical complaint among hospitalized patients, with up to 80 % of medical and surgical patients reporting pain.1,2 Patient reports on the quality of pain treatment are important measures of the overall quality of healthcare. These reports depend not only on the degree of pain relief after treatment, but also on such factors as patients’ expectations3,4 and provider–patient communication.5
Because the assessment and treatment of pain are based largely on patients’ reports about the location, intensity, and quality of pain, effective provider–patient communication is necessary for effective treatment. Patients with limited English proficiency (LEP) may have difficulties communicating their pain symptoms in the presence of language barriers. Suboptimal communication between providers and patients may affect assessment and treatment decisions, and may lead to poor management of pain symptoms. Not surprisingly, previous studies have linked LEP with higher levels of pain and greater barriers to pain management.6,7
Patients in obstetric and gynecologic services can experience significant pain associated with surgical procedures and labor and delivery. Although postoperative pain treatment with opioids is standard of care, management of pain associated with labor and delivery includes a variety of acceptable approaches. Epidural analgesia is most frequently used and recommended by the American College of Obstetricians and Gynecologists.8 The few studies on attitudes of Latinas towards pain during labor and delivery suggest that Latinas have similar pain management expectations as non-minority patients.9,10, Furthermore, in a study among Latinas, exploring factors influencing requests for epidural analgesia, counseling on pain management by the attending obstetrician increased the acceptability of this technique by 10 %.10
Addressing communication barriers between healthcare providers and patients with LEP has assumed ever-increasing importance. Nearly one in five people in the United States (US) speaks a language other than English at home, and 25 million—nearly 9 % of the total US population—are thought to have LEP.11 Spanish is the most common non-English language spoken in the US, and nearly half of native Spanish speakers have LEP.11 The increasing number of LEP patients poses substantial challenges for healthcare providers who manage pain during hospitalizations and in other settings.
One important way to improve communication between providers and LEP patients is to use interpreters.12 Although interpreters do not completely eliminate language barriers, they facilitate communication between providers, patients with LEP, and patients' families. Previous studies have shown that use of interpreters improves communication between healthcare providers and patients with LEP,13–15 and promotes adherence to prescribed treatment regimens and follow-up care for some clinical conditions.16
Considering the importance of provider–patient communication in treating pain, as well as the presence of barriers to pain treatment among LEP patients, we investigated whether the use of interpreters was associated with better pain treatment in hospitalized LEP patients. Our study sample consisted of female Spanish-speaking patients with LEP who were hospitalized for obstetric and gynecological care at two teaching hospitals.
METHODS
Participants
Female Latina patients were surveyed regarding their experiences with care as part of the evaluation for the Hablamos Juntos (HJ) initiative. Sponsored by the Robert Wood Johnson Foundation, HJ was intended to increase linguistic access for Spanish-speaking patients with LEP. Following a competitive application process, ten healthcare organizations located throughout the United States were selected for HJ demonstration projects, including two teaching hospitals. Both hospitals implemented programs to increase the availability of trained interpreters to patients on their obstetric and gynecology units. After institutional review board (IRB) approval at each clinical site, and following the protocol approved by the RAND corporation (Santa Monica, CA), representative samples of patients from these units were asked to complete patient experience surveys after their discharge from the hospital in 2003 (before the start of the demonstration projects), and again in 2006 (near the end of the demonstration projects). Results from both survey waves were included in this study. The surveys were administered in English or Spanish by computer-assisted telephone interviewing. Response rates ranged from 70 % to 76 % across sites and survey waves. Additional details about the surveys and the HJ evaluation have been published elsewhere.17 For the present study, we pooled data from both survey waves after negative testing for interaction between interpreter use and year of the survey.
A total of 368 participants completed the HJ hospital survey across both teaching hospitals and both survey waves. For this study, we limited the sample to LEP participants who indicated that they needed pain medications and interpreter services during their hospital stay (n = 185). Patients who reported a need for interpreter were labeled as LEP.
Study Measures
Quality of Pain Treatment
Participants’ reports on the quality of their pain treatment were elicited by three survey items (Text box). Participants who reported that their pain was not always well controlled were asked whether language barriers were a problem. These items were adapted from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Hospital Survey.18 Similar items have been translated into Spanish and evaluated for equivalence with the English versions.19 The scored responses to these items ranged from 1 (never) to 4 (always) and from 1 (not a problem) to 3 (a big problem). For the three survey items on quality of pain treatment, very few participants responded “never”. We collapsed the never/sometimes category and left the “usually” and “always” categories unchanged.
Text box. Survery items
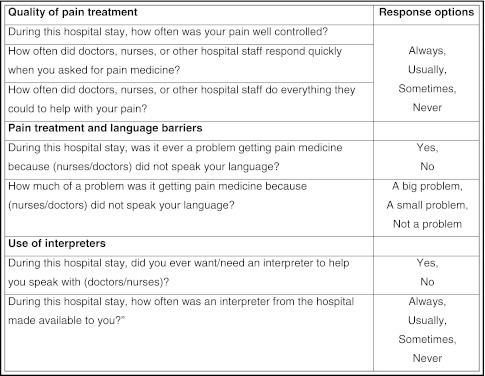
Need and Use of Interpreters
The main predictor variable was constructed from two survey items (Text box). Based on their responses, each participant was placed in one of two mutually exclusive categories: interpreter needed and always available (Always); and interpreter needed and sometimes, usually, or never available (Not Always).
Other Covariates
Our selection of covariates was guided by results from previous studies of patient-reported outcomes.13,20–22 Other covariates included in the analyses were age (18–34, ≥ 35 years), years of education (0–11, ≥ 12), place of birth (US vs. foreign born), insurance status (insured vs. uninsured), and self-reported health status (excellent/very good/good vs. fair/poor). Household income and size were used to categorize households as either 1) below the federal poverty level, or 2) at or exceeding the federal poverty level. The reason for hospitalization (obstetrical childbirth vs. surgery/other), length of hospitalization (1–2 days vs. ≥3 days), and survey year (2003 vs. 2006), were also included in the analyses.
Statistical Analyses
Cross tabulations were used to evaluate unadjusted associations between interpreter use and key demographic characteristics of the participants. To evaluate the associations between interpreter use and pain treatment, we performed unadjusted and adjusted ordered logistic regression analyses, and confirmed that none of these analyses violated the proportional odds assumption. We report the overall adjusted odds ratios for each one of the outcome variables, as well as the covariates included in the adjusted model. In all regression models, Always was the reference category, because it represents the ideal situation for an LEP patient in terms of communication regarding adequate pain treatment. We also present descriptive data on patients’ reports of problems obtaining pain medication, by interpreter availability. P-values less than 0.05 were considered statistically significant. All analyses were conducted using STATA version 11.1 (Stata Corporation, College Station, TX).
Treatment of Missing Values
Rates of missing values were low for all variables (<1 % missing) except for household income, for which 21 % were missing. For household income, we imputed missing values by using a modified regression imputation approach applied in related research.15 We found that participants with and without missing income values were similar with respect to age, gender, place of birth, education, and self-reported health status. In sensitivity analyses, we found no significant differences between the results of regression models in which we included or excluded participants with imputed household income.
RESULTS
Sample Characteristics
Seventy-nine percent of study participants were 18 to 35 years of age; 70 % had less than 12 years of education; 99 % were foreign born; 71 % reported excellent, very good, or good health; 74 % were uninsured; 86 % were hospitalized for childbirth; and 66 % were hospitalized for two days or fewer.
Patient Characteristics and Use of Interpreters
Overall, 27 % of the study participants reported always receiving an interpreter (Always), and 73 % sometimes receiving an interpreter (Not Always). Groups were similar with respect to age, health status, income and education levels. (Table 1)
Table 1.
Patient Characteristics by Interpreter Availability
| Patient characteristics | Interpreter availability | |||
|---|---|---|---|---|
| All (n = 185) | Not Always (n = 135) | Always (n = 50) | P-value | |
| Age, years | ||||
| 18-34 | 146 (79 %) | 107 (79 %) | 39 (78 %) | 0.9 |
| ≥35 | 39 (21 %) | 28 (21 %) | 11 (22 %) | |
| Education, years | ||||
| 0-11 | 128 (70 %) | 90 (67 %) | 38 (78 %) | 0.1 |
| ≥12 | 94 (39 %) | 45 (33 %) | 11 (22 %) | |
| Adjusted household income | ||||
| <1.0 poverty level | 106 (57 %) | 76 (56 %) | 30 (60 %) | 0.6 |
| ≥1.0 poverty level | 79 (43 %) | 59 (44 %) | 20 (40 %) | |
| Birthplace | ||||
| United States | 1 (0.5 %) | 1 (0.7 %) | 0 | 0.3 |
| Mexico | 91 (49 %) | 68 (50 %) | 23 (46 %) | |
| Central America | 72 (39 %) | 48 (36 %) | 24 (48 %) | |
| South America/Other | 21 (11 %) | 18 (13 %) | 3 (6 %) | |
| Self-reported health status | ||||
| Excellent/Very Good/Good | 131 (71 %) | 93 (69 %) | 38 (76 %) | 0.3 |
| Fair/Poor | 54 (29 %) | 42 (31 %) | 12 (24 %) | |
| Insured | 48 (26 %) | 35 (26 %) | 13 (26 %) | 0.9 |
| Reason for hospitalization | ||||
| Surgery | 15 (8 %) | 12 (9 %) | 3 (6 %) | 0.7 |
| Childbirth (including cesarean section) | 260 (86 %) | 115 (86 %) | 45 (90 %) | |
| Other medical reason | 10 (5 %) | 8 (6 %) | 2 (4 %) | |
| Wave of interview | ||||
| Wave 1 | 95 (51 %) | 67 (50 %) | 28 (56 %) | 0.4 |
| Wave 2 | 90 (49 %) | 68 (50 %) | 22 (44 %) | |
Comparisons between groups were performed by using chi-square tests or Fisher’s exact test when needed
Patient Reports on Pain Treatment and Use of Interpreters
Table 2 shows adjusted results from the regression analyses estimating the association between patient reports on quality of pain treatment and use of interpreters. Unadjusted results were almost identical to the adjusted ones; therefore, we only present the adjusted analyses. Compared with the Always group, the Not Always group reported significantly lower scores for all three items on quality of pain treatment, including pain control, timely response, and perceived helpfulness from staff. These differences were significant (p < 0.05) in the unadjusted and adjusted models.
Table 2.
Adjusted Odds Ratios Examining the Association of Interpreter Availability and Patient Reports of Quality of Pain Treatment
| Adequate pain control during hospitalization | Timely response to pain | Perceived helpfulness from staff to respond to pain | ||||
|---|---|---|---|---|---|---|
| OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | |
| Interpreter not always available | 0.4 | 0.2-0.8 | 0.4 | 0.2-0.8 | 0.3 | 0.2-0.7 |
| Age ≥ 35y | 0.9 | 0.4-1.9 | 0.9 | 0.4-1.9 | 1.5 | 0.6-3.4 |
| Education ≥ 12y | 0.9 | 0.4-1.7 | 1 | 0.5-1.2 | 0.9 | 0.4-1.8 |
| Income ≥ 1.0 poverty level | 0.7 | 0.3-1.7 | 0.4 | 0.2-1 | 0.7 | 0.4-1.3 |
| Health status Excellent/Very Good/Good | 1.3 | 0.6-2.5 | 1.1 | 0.5-2.2 | 1.4 | 0.7-2.8 |
| Insured | 0.1 | 0.2-0.9 | 0.5 | 0.2-1.2 | 0.8 | 0.4-1.6 |
| Reason for hospitalization childbirth | 1.5 | 0.8-3 | 1.21 | 0.5-3 | 1.3 | 0.7-2.7 |
| Wave 2 | 1.2 | 0.6-2.3 | 1.17 | 0.6-2.2 | 1.1 | 0.6-2.1 |
Calculated using ordered logistic regression; response categories were never/sometimes, usually, always. The reference category for all models was interpreter always available
Patient Reports on Language Barriers
Table 3 presents descriptive data on patient reports of language barriers for obtaining pain treatment from doctors and nurses, by interpreter need and availability. Language barriers were reported by 13 % of patients in the Not Always group, compared to 8 % in the Always group.
Table 3.
Patient Report of Language Barriers for Obtaining Pain Medication
| Not Always N = 135 | Always N = 50 | |
|---|---|---|
| Problem getting pain medication from | N (%) | N (%) |
| Nurses | ||
| A big problem | 8(6 %) | 1 (2 %) |
| A small problem | 9 (7 %) | 3 (6 %) |
| Not a problem | 118 (87 %) | 48 (96 %) |
| Doctors | ||
| A big problem | 7 (5 %) | 1 (2 %) |
| A small problem | 10 (7 %) | 1 (2 %) |
| Not a problem | 118 (87 %) | 48 (96 %) |
DISCUSSION
In this study of hospitalized Spanish-speaking women, we found that interpreter use was associated with better patient reports of pain control, timely response to pain needs, and perceived helpfulness of healthcare providers to provide pain treatment. These findings indicate that providing interpreters for hospitalized patients with LEP results in higher-rated patient-reported quality of care for pain control.
When participants were asked how much of a problem it was to obtain pain medicines from doctors and nurses who do not speak Spanish, participants who always had access to an interpreter reported fewer problems than those who did not. These descriptive results suggest that use of interpreters may ease obtaining needed pain medicines, and may contribute to better pain control. Our findings are in agreement with previous research reporting that Spanish-speaking patients in the US experience greater barriers to pain management than English speaking patients, with barriers mostly due to difficulties in communication with providers.7
Our findings are also consistent with previous studies documenting the importance of interpreter services for Latino patients who need to communicate regarding healthcare issues. In a study of uninsured Spanish-speaking Latinos who accessed hospital services, patients who used interpreters reported more satisfaction in their communications with providers, pharmacy, and staff than their counterparts who needed but did not receive interpreters.23 Another study of outpatients similarly found that Latinos who used interpreters were more satisfied with communication about medications.20 We extend this limited body of literature to the potentially positive impact of interpreters on pain treatment among hospitalized Spanish-speaking women.
Our results have clinical implications that support the use of interpreters in managing pain. Unfortunately, interpreters are still grossly underused in clinical settings.24–26 Patients and families with LEP are more likely than others to experience limited communication with healthcare providers, receiving only basic information and poor attention to their questions, concerns, and emotions.27 Further, providers who speak Spanish less than fluently sometimes try to communicate with LEP patients without the benefit of interpreters, especially in routine situations, leading to miscommunication and inadequate assessments of pain.28 Given the complexity of the pain experience, its assessment should not be limited to simple descriptors or ratings. Unfortunately, consideration of the nuances of pain is hindered, if not entirely suppressed, when barriers to communication exist. Effective pain management requires the assessment of pain characteristics, associated symptoms, and potential side effects of analgesic medications. By enhancing communication, interpreters enable pain to be assessed more comprehensively, and may also help providers understand the cultural context of their patients’ medical concerns.28,29
Decisions around pain control during labor and delivery require excellent communication between providers and patients. Patients’ expectations and knowledge about the different alternatives for pain treatment, specifically epidural and spinal analgesia, influence the use of these methods.10 Use of interpreters may be particularly valuable to facilitate communication around pain control with obstetric LEP patients who have lower levels of education, are new to the healthcare system, and have poor knowledge of analgesic alternatives for labor and delivery.
This study also has clear policy implications. In 1999, the Joint Commission on Accreditation of Healthcare Organizations declared that pain assessment was the fifth vital sign, and since that time, healthcare institutions have promoted pain assessment for all patients. Our study suggests that interpreters can help to properly implement this mandate for patients with LEP. In the ideal clinical scenario, language concordance between providers and patients would ensure better outcomes in pain management. Given the multitude of languages spoken in the US and the lack of linguistic diversity in the healthcare workforce, however, this ideal cannot easily be achieved. Meanwhile, promoting a more consistent use of interpreters will improve provider–patient communication and potentially improve clinical assessment and treatment of pain.
These findings should be interpreted in light of several limitations. First, because the data are observational, causal inferences are impossible. Second, the data set contained only patient-reported outcomes at the time of discharge, so we could not evaluate pain levels at the time of clinical encounters. Specifically, we lack data on the type of analgesic treatment received by patients and on actual pain measurements, such as intensity and duration of pain, which have previously been identified as important indicators of the quality of pain treatment.30,31 Nonetheless, patient-related outcomes, including patient perceptions of treatment, are also important measures of quality. Third, we did not have specific information about patient’s expectations of the health care system, or overall patient satisfaction with health care staff, which may influence responses to the questions asked. Finally, our study population was highly selected, so our findings may not be readily generalized to men, rural populations, community samples, or women hospitalized for reasons other than obstetric or gynecological care.
In conclusion, use of interpreters is associated with better self-reported quality of pain treatment in patients with LEP, and may enhance clinical interactions related to pain. Despite the limitations of our study, these findings illuminate a possible avenue to improve the quality of pain management for LEP patients. Future studies are needed to evaluate the clinical effect of interpreter services on pain treatment for patients in this population.
Acknowledgements
Research Funding
This work was supported by the National Cancer Institute [U01 CA114642 to DB]; the National Institute of Diabetes and Digestive and Kidney Diseases [DK 082325 to NJ, PI: DB]; the National Center for Research Resources [1KL2-RR02-5015 to Mary Disis]; and the Department of Health and Human Services [1T32GM086270-01 to NJ, PI: Debra Schwinn]. Gerardo Moreno and Mei Leng received support from the University of California, Los Angeles, Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA Grant P30-AG021684).
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97:534–40. doi: 10.1213/01.ANE.0000068822.10113.9E. [DOI] [PubMed] [Google Scholar]
- 2.Whelan CT, Jin L, Meltzer D. Pain and satisfaction with pain control in hospitalized medical patients: no such thing as low risk. Arch Intern Med. 2004;164:175–80. doi: 10.1001/archinte.164.2.175. [DOI] [PubMed] [Google Scholar]
- 3.Jamison RN, Taft K, O'Hara JP, Ferrante FM. Psychosocial and pharmacologic predictors of satisfaction with intravenous patient-controlled analgesia. Anesth Analg. 1993;77:121–5. [PubMed] [Google Scholar]
- 4.Jamison RN, Ross MJ, Hoopman P, et al. Assessment of postoperative pain management: patient satisfaction and perceived helpfulness. Clin J Pain. 1997;13:229–36. doi: 10.1097/00002508-199709000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Bovier PA, Charvet A, Cleopas A, Vogt N, Perneger TV. Self-reported management of pain in hospitalized patients: link between process and outcome. Am J Med. 2004;117:569–74. doi: 10.1016/j.amjmed.2004.05.020. [DOI] [PubMed] [Google Scholar]
- 6.Jacob E, McCarthy KS, Sambuco G, Hockenberry M. Intensity, location, and quality of pain in Spanish-speaking children with cancer. J Pediatr Nurs. 2008;34:45–52. [PubMed] [Google Scholar]
- 7.Mosher CE, Duhamel KN, Egert J, Smith MY. Self-efficacy for coping with cancer in a multiethnic sample of breast cancer patients: associations with barriers to pain management and distress. Clin J Pain. 2010;26:227–34. doi: 10.1097/AJP.0b013e3181bed0e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ACOG Committee Opinion No. 295. American College of Obstetricians and Gynecologists. Pain relief during labor. Obstet Gynecol 2004;104:213. [PubMed]
- 9.Lee WW, Burelbach AD, Fosnocht D. Hispanic and non-Hispanic white patient pain management expectations. Am Emerg Med. 2001;19:549–50. doi: 10.1053/ajem.2001.28038. [DOI] [PubMed] [Google Scholar]
- 10.Orejuela F, Garcia T, Green C, et al. Exploring factors influencing patient request for epidural analgesia on admision to labor and delivery in a predominantly Latino population. J Immigr Minor Health. 2012;14(2):287–91. doi: 10.1007/s10903-011-9440-2. [DOI] [PubMed] [Google Scholar]
- 11.Shin HB, Kominsky RA. Language Use in the United States: 2007. American Community Survey Reports, ACS-12. Washington, D.C.: U.S. Census Bureau; 2010.
- 12.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42:727–54. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morales LS, Elliott M, Weech-Maldonado R, Hays RD. The impact of interpreters on parents' experiences with ambulatory care for their children. Med Care Res Rev. 2006;63:110–28. doi: 10.1177/1077558705283125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zayas LH, Cabassa LJ, Perez MC, Cavazos-Rehg PA. Using interpreters in diagnostic research and practice: pilot results and recommendations. J Clin Psychiatry. 2007;68:924–8. doi: 10.4088/JCP.v68n0615. [DOI] [PubMed] [Google Scholar]
- 15.Morales LS, Leng M, Escarce JJ. Risk of cardiovascular disease in first and second generation Mexican–Americans. J Immigr Minor Health. 2011;13:61–8. doi: 10.1007/s10903-009-9262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tocher TM, Larson E. Quality of diabetes care for non-English-speaking patients. A comparative study. West J Med. 1998;168:504–11. [PMC free article] [PubMed] [Google Scholar]
- 17.Wu S, Ridgely MS, Escarce JJ, Morales LS. Language access services for Latinos with limited English proficiency: lessons learned from Hablamos Juntos. J Gen Intern Med. 2007;22(Suppl 2):350–5. doi: 10.1007/s11606-007-0323-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. Department of Health and Human Services. 2008 H-CAHPS Chartbook (publication number 08-0066-EF). Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- 19.Hurtado MP, Angeles J, Blahut SA, Hays RD. Assessment of the equivalence of the Spanish and English versions of the CAHPS hospital survey on the quality of inpatient care. Health Serv Res. 2005;40:2140–61. doi: 10.1111/j.1475-6773.2005.00469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moreno G, Tarn DM, Morales LS. Impact of interpreters on the receipt of new prescription medication information among Spanish-speaking Latinos. Med Care. 2009;47:1201–8. doi: 10.1097/MLR.0b013e3181adcc1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moreno G, Morales LS. Hablamos Juntos (together we speak): interpreters, provider communication, and satisfaction with care. J Gen Intern Med. 2010;25:1282–8. doi: 10.1007/s11606-010-1467-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mosen DM, Carlson MJ, Morales LS, Hanes PP. Satisfaction with provider communication among Spanish-speaking Medicaid enrollees. Ambul Pediatr. 2004;4:500–4. doi: 10.1367/A04-019R1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andrulis D, Goodman N, Pryor C. What a difference an interpreter can make: health care experiences of uninsured with limited English proficiency. Boston, MA: The Access Project; 2002. [Google Scholar]
- 24.Diamond LC, Schenker Y, Curry L, Bradley EH, Fernandez A. Getting by: underuse of interpreters by resident physicians. J Gen Intern Med. 2009;24:256–62. doi: 10.1007/s11606-008-0875-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuo DZ, O'Connor KG, Flores G, Minkovitz CS. Pediatricians' use of language services for families with limited English proficiency. Pediatrics. 2007;119:e920–7. doi: 10.1542/peds.2006-1508. [DOI] [PubMed] [Google Scholar]
- 26.Lee KC, Winickoff JP, Kim MK, et al. Resident physicians' use of professional and nonprofessional interpreters: a national survey. JAMA. 2006;296:1050–3. doi: 10.1001/jama.296.9.1050. [DOI] [PubMed] [Google Scholar]
- 27.Davies B, Contro N, Larson J, Widger K. Culturally-sensitive information-sharing in pediatric palliative care. Pediatrics. 2010;125:e859–65. doi: 10.1542/peds.2009-0722. [DOI] [PubMed] [Google Scholar]
- 28.Diamond LC, Reuland DS. Describing physician language fluency: deconstructing medical Spanish. JAMA. 2009;301:426–8. doi: 10.1001/jama.2009.6. [DOI] [PubMed] [Google Scholar]
- 29.Schenker Y, Lo B, Ettinger KM, Fernandez A. Navigating language barriers under difficult circumstances. Ann Intern Med. 2008;149:264–9. doi: 10.7326/0003-4819-149-4-200808190-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dahl JL, Gordon D, Ward S, Skemp M, Wochos S, Schurr M. Institutionalizing pain management: the Post-Operative Pain Management Quality Improvement Project. J Pain. 2003;4:361–71. doi: 10.1016/S1526-5900(03)00640-0. [DOI] [PubMed] [Google Scholar]
- 31.Gordon DB, Polomano RC, Pellino TA, et al. Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: preliminary psychometric evaluation. J Pain. 2010;11:1172–86. doi: 10.1016/j.jpain.2010.02.012. [DOI] [PubMed] [Google Scholar]


