ABSTRACT
BACKGROUND
Uncontrolled hypertension remains a significant problem for many patients. Few interventions to improve patients’ hypertension self-management have had lasting effects. Previous work has focused largely on patients’ beliefs as predictors of behavior, but little is understood about beliefs as they are embedded in patients’ social contexts.
OBJECTIVE
This study aims to explore how patients’ “explanatory models” of hypertension (understandings of the causes, mechanisms or pathophysiology, course of illness, symptoms and effects of treatment) and social context relate to their reported daily hypertension self-management behaviors.
DESIGN
Semi-structured qualitative interviews with a diverse group of patients at two large urban Veterans Administration Medical centers.
PARTICIPANTS (OR PATIENTS OR SUBJECTS)
African-American, white and Latino Veterans Affairs (VA) primary care patients with uncontrolled blood pressure.
APPROACH
We conducted thematic analysis using tools of grounded theory to identify key themes surrounding patients’ explanatory models, social context and hypertension management behaviors.
RESULTS
Patients’ perceptions of the cause and course of hypertension, experiences of hypertension symptoms, and beliefs about the effectiveness of treatment were related to different hypertension self-management behaviors. Moreover, patients’ daily-lived experiences, such as an isolated lifestyle, serious competing health problems, a lack of habits and routines, barriers to exercise and prioritizing lifestyle choices, also interfered with optimal hypertension self-management.
CONCLUSIONS
Designing interventions to improve patients’ hypertension self-management requires consideration of patients’ explanatory models and their daily-lived experience. We propose a new conceptual model — the dynamic model of hypertension self-management behavior — which incorporates these key elements of patients’ experiences.
KEY WORDS: hypertension, medication adherence, qualitative methods, health behavior, self-management
INTRODUCTION
Hypertension continues to be a major US health problem; it is underdiagnosed, undertreated, and even when treated, often poorly controlled; over one-third of patients on antihypertensive medications have uncontrolled disease.1 Poor hypertension control has been attributed to provider factors, such as clinical inertia in prescribing adequate medications2,3 and patient factors, including poor adherence to medications and lifestyle management.4–6 Few interventions to improve hypertension control have had resounding, sustained effects.7. Thus, finding ways to improve hypertension self-management remains a significant challenge.
Prior interventions have included educating patients about hypertension, improving BP self-monitoring at home, and nurse or pharmacist-led care. A recent Cochrane review found that purely educational interventions improved patient knowledge but were largely ineffective in improving hypertension control. Patient self-monitoring and nurse or pharmacist-led interventions held greater promise, although results were heterogeneous.7
One reason for the failure of purely educational interventions may be that they lack a patient-centered focus, thereby failing to address patients’ unique barriers to hypertension self-management. A patient-centered approach would incorporate how patients understand hypertension, attempt to manage hypertension, and prioritize its management in their lives. Many interventions are built upon theories that beliefs or illness perceptions drive patients’ illness self-management.8,9 Kleinman10 reframes beliefs as integrated “explanatory models (EMs)” — patients’ understanding of the causes, pathophysiology, course of illness, symptoms, and effects of treatment. EMs of an illness like hypertension are situated within social contexts; they are formed and persist in the context of the communities in which patients live. Thus, in order to influence health-related self-management behaviors, one must understand both patients’ beliefs about an illness and their social context.
Further understanding hypertension self-management experiences would foster a patient-centered approach to hypertension control. Previous studies have examined patients’ ‘lay’ models of hypertension,11–13 but not how EMs relate to social context, or how they impact various hypertension self-management behaviors. In this qualitative study, we extend prior work by examining patients’ EMs, social contexts, and hypertension self-management behaviors. We explore these aspects of patients’ hypertension experiences and propose a new conceptual model of patients’ illness self-management.
METHODS
Participants and Recruitment
We recruited a purposive sample of African-American, white and Latino patients with uncontrolled hypertension from primary care clinics at two large US Veterans Affairs (VA) Medical Centers serving diverse populations located in the Northeast and Southwest, respectively. In a 1-year period, we sought to recruit 20 patients from each racial/ethnic group to obtain a wide range of responses, with the expectation that we would reach thematic saturation for a diverse population. Each site’s institutional review board approved the study.
Patients were eligible to participate if they had a diagnosis of hypertension and uncontrolled blood pressure (BP) (≥140/90 mmHg) documented at least once in the previous 6 months in the VA’s electronic medical record, and a BP >140/90 mmHg at their primary care visit. A research assistant (RA) called patients prior to their appointment to invite participation. At the visit, the RA administered eligibility screening, collected demographic information, took BP readings and obtained written informed consent. The data were collected between February 2007 and June 2008.
Data Collection
A trained RA conducted semi-structured 1.5 hour interviews with patients. A $20.00 gift card was given for participation. Patients were asked to describe their family, a typical day, experiences living with hypertension, knowledge about hypertension, what they thought caused hypertension, the severity of their hypertension, their concerns about hypertension, communication with their provider, and medications and strategies they used to manage their hypertension.
Data Analysis
Interviews were audio-recorded, professionally transcribed verbatim, and reviewed for accuracy. We used qualitative analytic techniques informed by grounded theory.14,15 We started by exploring how EMs affected hypertension self-management. Consistent with a grounded theory approach, we sought to identify other aspects of patient experience emergent in the data. Five team members began by open coding five transcripts together, identifying themes grounded in participants’ language, and generating a coding dictionary that was refined with coding of subsequent interviews. We collapsed codes into broader categories, informed by the data and EM categories of “cause,” “course,” “pathophysiology,” “symptoms,” and “treatment,” and by aspects of social context. We identified participants’ hypertension self-management behaviors — reports of what they did to control their hypertension — and developed summary templates describing each participant’s EMs, social context, hypertension self-management behaviors, perceptions of clinical encounters, and primary barrier to hypertension self-management. Investigators paired up to analyze subsequent interviews and complete templates, which were reviewed by the entire team, and cases were contrasted using constant comparison analysis. Throughout the analytic process, we iteratively refined conceptual links between constructs to develop a conceptual model.
RESULTS
We interviewed 48 patients (19 African-American, 20 white, and 9 Hispanic). We failed to recruit the target number of Hispanic patients, due to the relatively low Hispanic prevalence at our sites and greater participation refusal. The average age was 60; 92 % were men; 88 % had at least a high school degree, and yet income was low (see Table 1). The average BP at the clinic visit was 160/93 mmHg. We identified two major domains affecting patients’ hypertension self-management behaviors: 1) four different aspects of EMs, including beliefs regarding the cause of hypertension, hypertension symptoms, the illness course (including whether they thought hypertension was chronic or intermittent), and treatment value and effects; and 2) aspects of patients’ social context, routines, habits, and competing health problems, which we termed “daily-lived experience” (DLE).
Table 1.
Participant Demographics
| Interview participants (N = 48) | |
|---|---|
| Males | 44 |
| Age | Mean – 60 (SD – 10.31) |
| Race | |
| Black | 20 |
| White | 19 |
| Latino | 9 |
| Education | |
| ≤ 8th grade | 3 |
| Some high school | 2 |
| Completed high school | 14 |
| Some college | 8 |
| Completed college | 8 |
| Graduate school | 2 |
| Unknown | 1 |
| Income ($) | |
| <15,000 | 14 |
| 15,000 – 20,000 | 7 |
| 20,000 – 40,000 | 13 |
| 40,000 – 60,000 | 5 |
| >80,000 | 2 |
| Unknown | 7 |
Patients described a wide range of EMs and DLEs that adversely affected their hypertension self-management behaviors and BP control (Tables 2 and 3). We first treat EM and DLE as separate and provide exemplary quotes demonstrating how EMs and DLEs were related to patients’ reported hypertension self-management behaviors. We then show how EMs and DLEs may relate to one another in shaping self-management, and describe the resulting conceptual model. For 47 of the 48 patients we interviewed, we identified at least one EM or DLE that adversely affected their hypertension self-management behavior. We did not identify any unique racial/ethnic differences in EMs or DLE.
Table 2.
Explanatory Models and Corresponding Hypertension Self-Management Behaviors. These Represent the Range of Explanatory Models Described by Patients in Qualitative Interviews as Affecting Hypertension Self-Management Behaviors
| Explanatory Model | Hypertension Self-Management Behavior |
|---|---|
| Cause | |
| Stress as primary cause | Stays calm, avoids stressful situations; takes antidepressant as treatment |
| Exercise causes increased BP | Avoids exercise to keep BP low |
| Pain causes increased BP | Managing pain, taking pain medications will control hypertension |
| Course of Illness | |
| Hypertension comes and goes | Takes medications when BP goes up |
| BP cannot be controlled | Won’t exercise and forgets medications |
| Little concern about hypertension – does not affect my life | Avoids going to the doctor; Forgets medications |
| Own definition of what is considered ‘high’ | Only take medication when BP is >190/100 mmHg |
| Symptoms | |
| I can tell when my BP is high; I get headaches, dizziness when my BP is high | Takes medications only when symptoms occur |
| I have no symptoms of high blood pressure; therefore it is not a problem | Doesn’t take medications |
| Eating bacon doesn’t make me feel bad, so it doesn’t affect my BP. | Eats bacon as desired |
| Treatment | |
| Only exercise can help me control my HBP | Exercises and therefore allows himself to smoke, drink and not take medication. |
| Garlic and vinegar can help me control my HBP. | Focuses on these remedies, while not taking medications or altering diet or sodium intake |
Table 3.
Daily-Lived Experience and Corresponding Reported Behaviors that Interfere With Hypertension Self-Management. These Represent the Range of DLEs Described by Patients in Qualitative Interviews as Affecting Behaviors that Might Interfere with Hypertension Self-Management
| Daily-Lived Experience | Behaviors Interfering with Hypertension Self-Management |
|---|---|
| Lonely, isolated lifestyle | Eats out at restaurants for social interaction, which limits ability to control salt intake. |
| Serious competing chronic illnesses | Disregards hypertension in favor of managing these illnesses. Unable to engage in exercise. |
| Lack of routines and an unstructured lifestyle | Forgets to take medications; misses doctor appointments. |
| Experiences medication side effects, such as impotence | Decides not to take medications. |
| Frequent alcohol use | Avoids medications while drinking, doubles up on medications when not drinking. |
Explanatory Models (EMs)
One aspect of EMs was notably absent from patients’ interviews: pathophysiology, or a biomedical conceptualization of the condition. Few patients described their understanding of the pathophysiology of hypertension, and when they did, these understandings were not linked to hypertension self-management behaviors. In contrast, perceptions of cause, illness course, symptoms, and treatment were related to self-management in several ways.
Cause
When asked what caused their high BP, patients’ responses corresponded to notions of both the chronic disease of hypertension and to a temporary increase in BP associated with daily activities. Patients did not distinguish these two ‘illnesses,’ and often engaged in behaviors to avoid the latter, rather than behaviors that addressed biomedically attributed causes of hypertension . Patients noted causes including: 1) heredity, 2) general life stress, 3) poor diet (especially salt intake), and 4) lack of exercise. Patients also described causes typically associated with temporary rises in BP: 1) increased situational stress, 2) pain, and 3) exercising. Hypertension self-management behaviors were related to both types of perceived causes. For example, one woman who responded that stress was the cause of her hypertension went on to say:
"I think that my main reason for moving upstate is to find tranquility and maybe calm myself. And I keep saying, if I move upstate, I won’t have hypertension, I probably will not need medication, the lifestyle’s going to be different, it’ll be more relaxed." (#1– Latino woman, age 51)
This woman had described a complex, stressful city life, including work and family stressors. Her EM that stress was the cause of her hypertension, reflected in her statement that if she moved she would no longer have hypertension, led her to consider altering her living situation. This view could perhaps contribute to poorer medication adherence.
Course of Illness
The course of illness refers to patients’ perceptions of the path, controllability and severity of the illness. Some patients viewed hypertension as an intermittent problem that comes and goes. They were not concerned with hypertension as a chronic problem that needed constant management; rather, they focused on it when they knew their BP was high. For example, one woman stated:
"If my blood pressure is anywhere between, let’s say, 190 over 100, then I’m okay. As far as I’m concerned, I feel fine….right now that’s what it’s running about. And I’m still taking my medicine, though I’m not up to the max dose that I was up to before. So in my eyes, I’m fine. … if after a point … it starts creeping up to 220 over 120, then I have to do something at that point. It’s getting too high. I know that. But if it’s in the low 90, 180 range, to me, that’s not considered high for me. Because I feel I’m still feeling fine. I can function." (#2 – African American woman, age 53)
This woman expressed an EM of hypertension as intermittent; moreover, ‘normal BP’ for her is incongruent with the biomedical view of poor hypertension control. Subsequently, she altered her self-management behavior depending on her EM of ‘high’ blood pressure. She hinted that how she feels and functions, rather than an objective measurement, changes her behavior.
Symptoms
Patients discussed symptoms of hypertension in two ways: 1) “There are no symptoms of hypertension,” or 2) “I can feel when my blood pressure is high” (see the previous quote). In the first view, patients stated that since they did not have any symptoms associated with their hypertension, there was no need to adhere to hypertension management recommendations. One man who didn’t have symptoms stated:
"[Hypertension] doesn’t affect me. If it would just hit me, “boom!” and it would like put me to a point where I was … I’m getting dizzy from eating bacon or whatever, then I would change that, I wouldn’t do that. But it hasn’t." (#3 – African American man, age 73)
He expressed an EM in which the presence of symptoms indicated a need for concern, incongruous with the view of hypertension as the silent killer. Subsequently, he continued to eat bacon, despite recommendations to the contrary.
Other patients described hypertension symptoms including headaches, “pressure on your chest,” feeling “queasy or uneasy,” neck aches, backaches, or racing pulse. One man described having a headache and feeling “the blood [rush] to your head.” Many of these patients altered their hypertension self-management behaviors depending on their symptoms. One man stated:
"I can almost tell when it’s a little bit getting higher, I start feeling a little different in my head, you know, it’s like a headache or something, like a little pressure. So I back off on eating (inaudible) and whatnot, or I take an extra pill on that day. I mean, I usually take two, and I would do that and it sort of levels it again. Or I really stop eating everything that has salt and sodium … and that seems to work." (#4 – Latino man, age 63)
The EM that high blood pressure produces symptoms led him to alter his medication and diet depending upon his symptoms. This behavior, in turn, may contribute to poorly controlled BP.
Treatment
Beliefs about treatment effectiveness shaped hypertension self-management, and were linked to patients’ perceptions of causes and symptoms. Some endorsed taking medications, altering diet and engaging in exercise as effective treatment. Others, such as the following man, expressed concerns about taking medications for BP control, and altered treatment accordingly.
"Higher dosages concern me. I felt that my pressure was higher than…. I must have done something and it started getting higher, and I came to your walk-in clinic. And I was given a higher dosage. And I didn’t take it, I just went home and I relaxed. I think I might have taken one actually, or one-half." (#5 – Latino man, age 63)
This man’s EM that high medication doses may be harmful led him to rely more on relaxation than taking medications to control his hypertension. Note this behavior also reflects an EM that relaxation is an effective treatment.
Another man stated that he didn’t like taking medication, liked to drink and smoke, and that only exercising would control his hypertension:
"So, like I run. I run, until I, you know, I’m tired and can’t run any more. I stop. I sit. I collect myself and then I go again. … I smoke, so I work on my lungs as much as I can. And the thing is I’m trying to clear them so I can breathe better and basically have more wind… But now, I’m on—they got me on—blood pressure pills. I’m taking medication for high blood pressure."
INTERVIEWER:"Right. And how many are you on for blood pressure?"
"Just—I take one a day. You know, sometimes I do. Sometimes I miss it, you know. But my doctor, my primary care doctor, she wants me to take these every day. I don’t like medication too much. I like natural things." (#6 – African American man, age 64)
His EM was that taking medication was unnatural, and therefore concerning. Despite his acknowledgement that smoking is bad for him, he expressed an EM that getting exercise can overcome negative effects from smoking. He subsequently relied solely on exercise to control his BP.
Daily-Lived Experience (DLE)
Patients were asked to tell the interviewer about their lives and describe a typical day. The ways patients managed their hypertension were often embedded in descriptions of their daily activities. We identified five aspects of patients’ DLE that were related to hypertension self-management behaviors: 1) isolated lifestyle, 2) serious competing health problems, 3) lack of habits and routines, 4) barriers to exercise, and 5) prioritizing lifestyle choices (Table 3). Below we provide some exemplars, noting also how patients’ EMs intersected with DLE.
Lonely and Isolated Lifestyle
Many patients lived alone, were retired, unemployed, or on disability. Subsequently, they had little regular daily social interaction. One exception was venturing out to a local diner for daily meals, through which they attained the social interaction necessary to sustain their mental health. This practice, however, meant that they had little control over the amount of salt in their food. One man stated:
"I live alone, you know? So I don’t like cooking for one person. So I always go someplace to get lunches or dinners or whatever, or I go out and eat. Even eggs, you know, you can have a pinch of sodium in eggs, they already have it; they have sodium already. So everything that I eat might have sodium, and that little bit could bring it way up". (#7 – Latino man, age 61)
This man’s EM was that sodium was bad for his hypertension. However, his DLE included eating at restaurants for social engagement, interfering with his ability to control his sodium intake.
Serious Competing Health Problems
Most participants had multiple co-occurring illnesses that competed with their hypertension self-management. Some confused hypertension treatment regimens with regimens for other conditions. Problems such as having arthritis or pain interfered with following exercise recommendations. For others, controlling hypertension was not considered important relative to other conditions. For example, when asked about how concerned he was about hypertension, one man who was HIV positive and had diabetes responded:
"I’m not at all concerned about it, because I got the HIV and I got the diabetes. And high blood pressure is just another one."
INTERVIEWER: "How has it affected your overall health, if in any way?"
"I think I keep saying, to the best of my knowledge, I don’t feel it anywhere." (#8 – African American man, age 67)
The DLE of having other competing health problems to manage interfered with this man's hypertension self-management. His EM of hypertension as symptomless further rendered it unimportant relative to his other health problems.
Lack of habits and routines
Some patients described highly unstructured lifestyles with few routines, and forgetting to take medications. When asked by the interviewer what made it difficult for him to lower his BP, one man replied:
"Some very simple things. First of all, sometimes I scrap my morning routine. Sometimes I get up in the morning. By the time I realize, ‘Oh, I didn’t take my medicine yet,’ it’s one or two in the afternoon, okay." (#9 – white man, age 54)
This man’s DLE included disrupted routines, which subsequently resulted in not taking his medication as prescribed. This disruption, rather than any EM about his medications, interfered with medication adherence and hypertension control.
Others had unpredictable daily lives. One man described working on a boat at sea, during which time he often forgot to bring enough medication, was unable to obtain refills, and sometimes forgot to take it. He also described difficulty controlling his diet, as the ship’s cook prepared very salty food. Thus, despite having medication and limiting salt as part of his EM for controlling BP, his daily life presented barriers to doing so.
Barriers to Exercise
Many participants expressed an EM that exercise was important to managing their hypertension, but they experienced barriers to exercising. One barrier was other health conditions, such as arthritis, that prevented them from engaging in exercise. Another was an unsafe environment. One man explained:
"I do the exercise. Sometimes I go out and I walk up and down the steps. …‘You do that for 30 minutes,’ I said, ‘It is almost equivalent to walking a mile’ … because in my neighborhood, it is not real safe to be walking around, up and down the street."
INTERVIEWER: "They got loose dogs everywhere, huh?"
"Not only the dogs, gangsters." (#10 – white man, age 64)
This man’s DLE of living in an unsafe neighborhood challenged his ability to get his desired exercise, despite the fact that he endorsed an EM in which exercise helps control BP.
Prioritizing Lifestyle Choices
Patients described lifestyle choices that affected their hypertension self-management. For example, one man stated that he “liked to drink.”
"Sometimes I wouldn’t take [BP medication] for two or three days because I’m drinking. And when I continue, I’ll take two for a couple days, and that’s it. You know, if I feel my pressure is too high so I just double-dose, you get it? Only for a couple days, and then I go back to the regular dose." (#11 – African American man, age 57)
Drinking alcohol was part of his DLE. He understood the potential problems of drinking while taking his medication, so he altered his medication use. He also expressed an EM of the effects of treatment: the total amount of medication taken in a week is important, rather than daily adherence.
EMs and DLE Together
Patients’ narratives about their hypertension reveal the intertwined nature of EMs and DLEs. In some instances, the EM might drive DLE and behavior. For example, in quote #5, the gentleman’s EM is that he doesn’t wish to take medications because they aren’t natural. This subsequently drives his behavior around exercising, which is something that he can do in his daily life.
In other cases, DLE might drive the EM. In quote #1, the woman described a DLE in which stress was prevalent in the inner city context in which she lived. She attributed her high BP to this stressful life context, and in turn, believed that moving to a more peaceful setting would control her BP. If she moved, and her BP did not improve, this could alter her EM about the cause of her hypertension.
Conversely, there are instances where patients’ DLE interfered with their abilities to act on their EM. This is especially salient in the case of sodium intake. Many patients reported that lowering their salt intake was important for controlling their BP, but as noted in quote #7, eating out and eating prepared foods limited patients’ abilities to control their salt intake. This in turn may reinforce an EM that excess salt causes hypertension.
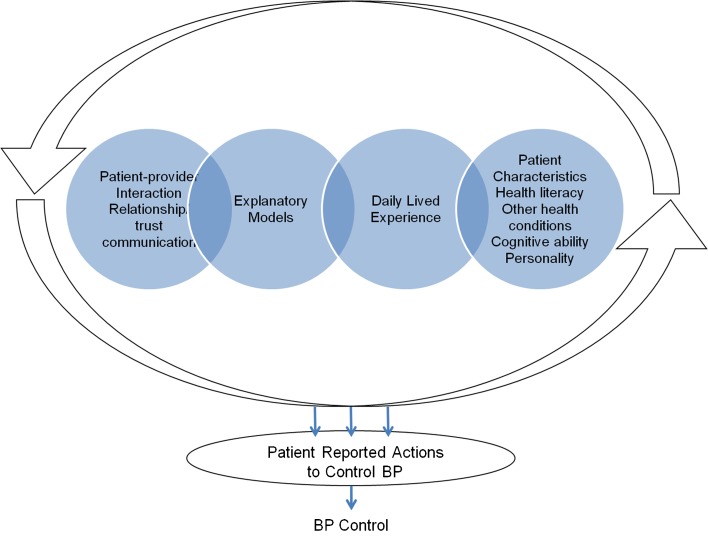
Conceptual links between these constructs resulted in the development of the Dynamic Model of Chronic Disease Self-Management (see Fig. 1). In this model, EMs and DLE continually shape one another in relationship to behavior, and may change over the course of a patient’s illness, as has been noted in our childhood asthma work.16 When discussing EMs and DLEs, patients suggested that communication with providers was also important to their self-management. Research supports the importance of this dimension on patient adherence.17 Thus, we also include patient-provider communication in the model.
Figure 1.
Dynamic model of hypertension self-management behavior.
DISCUSSION
Patients’ reports of their EMs and DLEs demonstrate that hypertension self-management does not occur primarily in the doctor’s office. Rather, patients self-manage their hypertension in complex social contexts, in which they develop hypertension EMs while engaging in daily activities. Our findings show different ways in which EMs and DLEs can affect patients’ hypertension self-management, including adherence to medications and recommended healthy behaviors.
Previous studies have demonstrated how differences in EMs affect patients’ illness management behaviors13,18 and confirm our finding that patients’ EMs lead patients toward particular hypertension self-management behaviors that may interfere with hypertension control.19 12. Huertin-Roberts12 found that African American women differentiated between “high blood pressure,” thought to be responsive to diet and medication changes, and “high-pertension,” a disease of the nerves caused by stress and factors that elicit emotional upset, and responsive to stress relief rather than antihypertensives. Others have found that medication beliefs contribute to medication adherence.9,20 These studies are consistent with theories of health behavior that account for behavior in terms of patients’ internal cognitive assessments and motivations for engaging in healthy behaviors.21–24
Our findings demonstrate, however, that patients’ self-management is based on more than their EMs or beliefs. Patients’ DLE, including their social context, routines and management of competing health demands, may conflict with their EMs, and interfere with good self-management. Previous work in understanding chronic disease self-management has similarly found an important role of routines in disease self-management.16,25
The intervention challenge is that patients with uncontrolled hypertension have complex constellations of EMs, DLEs, other illnesses and competing priorities that converge to influence self-management behaviors. As shown in the conceptual model, DLEs and EMs are inextricably intertwined to shape behavior. If one were to imagine that an individuals’ hypertension self-management experience were a strand of yarn, each fiber may constitute an EM or DLE; but if one were to pull on one strand, all the others would follow, altering the yarn altogether.
Limitations
Our findings are limited by three factors. Because this study was conducted in the VA, findings may not generalize to non-veteran populations or women, since most participants were men. Additionally, we did not observe the behaviors described; patients’ reported behaviors may differ from actual behavior. Finally, although we reached saturation with our white and African American samples, we were unable to enroll as many Latino patients as intended; therefore, we may have missed some additional novel EMs or DLEs.
Interestingly, participants’ infrequently stated understanding of hypertension pathophysiology was not related to self-management behaviors, suggesting that focusing on explaining how hypertension works in the body may not be an effective approach to improving hypertension control. Hypertension discussion in clinical encounters has often been restricted to adherence assessment (although even this may not occur26), with limited time spent counseling patients about hypertension self-management and lifestyle.27
While prior interventions have been tailored to particular patients’ needs,7,8,28 these interventions remain focused on providing information or education to patients to encourage them to improve their hypertension self-management behaviors, with little focus on patients’ EMs in the daily life context in which they manage their illness. Many participants were able to state what they should do to control hypertension, but persisted in not doing so. Thus, these results suggest that improving patients’ hypertension self-management requires an approach beyond assessment and education.
Encouraging patients to discuss their EMs and DLEs can enhance clinician understanding of patients’ lived experience of hypertension and subsequent self-management behaviors.29 Some participants expressed EMs that are inconsistent with biomedical knowledge leading to poor self-management. In these instances, providers should acknowledge these differences and tailor their intervention to accommodate those beliefs.29,30 For example, a provider may acknowledge that while reducing stress may be helpful for health, hypertension control requires additional lifestyle and medication management. Simply reminding patients to take medications and engage in healthy behavior is unlikely to be effective without addressing aspects of the patients’ context. Techniques such as motivational interviewing may be effective in focusing on these aspects of hypertension management.31 Cooper’s suggestion28 that providers need to ‘get to know the patient as a person,’ would likely lead providers to a better understanding of patients’ DLE. These steps might lead to a decrease in contextual errors in treating hypertension: treatment errors based on a misunderstanding of the patients’ context of disease management.32
Our findings underscore the importance of finding novel approaches in health care delivery systems to address the complex social and behavioral aspects of chronic disease self-management. While providers may address patients’ EMs and DLEs during routine clinical encounters, short clinic visits often preclude such in-depth conversations, although Haidet convincingly argues that such conversations need not necessarily take more time.33 Approaches using team based care,28 including health coaches34 in the context of a patient-centered medical home, may be ideal for addressing these key aspects of patient hypertension self-management.
Acknowledgements
This study was supported by the Department of Veterans Affairs, Health Services Research and Development grant #IIR 05-062. Dr. Kressin is supported by a Senior Research Career Scientist award from the Department of Veterans Affairs, Health Services Research & Development Service (RCS 02-066-1). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. A version of this paper was presented as a poster at the Society of General Internal Medicine in May 2009 and the VA Health Services Research and Development annual meeting in February 2009.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Ostchega Y, Yoon SS, Hughes J, Louis T. Hypertension awareness, treatment, and control–continued disparities in adults: United States, 2005–2006. NCHS Data Brief. 2008;3:1–8. [PubMed] [Google Scholar]
- 2.Berlowitz DR, Ash AS, Hickey EC, Friedman RH, Glickman M, Kader B, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339(27):1957–1963. doi: 10.1056/NEJM199812313392701. [DOI] [PubMed] [Google Scholar]
- 3.Rose AJ, Berlowitz DR, Orner MB, Kressin NR. Understanding uncontrolled hypertension: is it the patient or the provider? J Clin Hypertens (Greenwich). 2007;9(12):937–943. doi: 10.1111/j.1524-6175.2007.07332.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bosworth HB, Oddone EZ. A model of psychosocial and cultural antecedents of blood pressure control. J Natl Med Assoc. 2002;94(4):236–248. [PMC free article] [PubMed] [Google Scholar]
- 5.Di Matteo M. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Medical Care. 2004;42(3):200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 6.Stockwell DH, Madhavan S, Cohen H, Gibson G, Alderman MH. The determinants of hypertension awareness, treatment, and control in an insured population. Am J Public Health. 1994;84(11):1768–1774. doi: 10.2105/AJPH.84.11.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glynn L, Murphy A, Smith S, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database of Systematic Reviews. 2010;2010(3):CD005182. [DOI] [PubMed]
- 8.Bosworth HB, Olsen MK, Neary A, Orr M, Grubber J, Svetkey L, et al. Take Control of Your Blood Pressure (TCYB) study: a multifactorial tailored behavioral and educational intervention for achieving blood pressure control. Patient Educ Couns. 2008;70(3):338–347. doi: 10.1016/j.pec.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kressin NR, Wang F, Long J, Bokhour BG, Orner MB, Rothendler J, et al. Hypertensive patients' race, health beliefs, process of care, and medication adherence. J Gen Intern Med. 2007;22(6):768–774. doi: 10.1007/s11606-007-0165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kleinman A, Eisenberg L, Good B. Culture, illness and care: Clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88(2):251–258. doi: 10.7326/0003-4819-88-2-251. [DOI] [PubMed] [Google Scholar]
- 11.Blumhagen D. The meaning of Hyper-tension. In: Chrisman NaM, TW, ed. Clinically applied anthropology: D. Reidel Publishing Company; 1982:297-323.
- 12.Heurtin-Roberts S, Reisen E. The relation of culturally influenced lay models of hypertension to compliance with treatment. American Journal of Hypertension. 1992;5(11):787–792. [DOI] [PubMed]
- 13.Schlomann P, Schmitke J. Lay beliefs about hypertension: an interpretive synthesis of the qualitative research. J Am Acad Nurse Pract. 2007;19(7):358–367. doi: 10.1111/j.1745-7599.2007.00238.x. [DOI] [PubMed] [Google Scholar]
- 14.Strauss AL.Qualitative analysisfor socialscientists. Cambridge [Cambridgeshire]; New York: Cambridge University Press; 1987.
- 15.Charmaz K. Constructing groundedtheory. Thousand Oaks: Sage; 2006. [Google Scholar]
- 16.Yinusa-Nyahkoon LS, Cohn ES, Cortes DE, Bokhour BG. Ecological barriers and social forces in childhood asthma management: examining routines of African American families living in the inner city. J Asthma. 2010;47(7):701–710. doi: 10.3109/02770903.2010.485662. [DOI] [PubMed] [Google Scholar]
- 17.Rao JK, Anderson LA, Inui TS, Frankel RM. Communication interventions make a difference in conversations between physicians and patients - A systematic review of the evidence. Medical Care. 2007;45(4):340–349. doi: 10.1097/01.mlr.0000254516.04961.d5. [DOI] [PubMed] [Google Scholar]
- 18.Bokhour BG, Cohn ES, Cortes DE, Yinusa-Nyahkoon LS, Hook JM, Smith LA, et al. Patterns of concordance and non-concordance with clinician recommendations and parents' explanatory models in children with asthma. Patient Educ Couns. 2008;70(3):376–385. doi: 10.1016/j.pec.2007.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schlomann P, Schmitke J. Lay beliefs about hypertension: An interpretive synthesis of the qualitative research. J. Am. Acad. Nurse Pract. 2007;2007(19):358–367. doi: 10.1111/j.1745-7599.2007.00238.x. [DOI] [PubMed] [Google Scholar]
- 20.Horne R, Clatworthy J, Polmear A, Weinman J. Do hypertensive patients' beliefs about their illness and treatment influence medication adherence and quality of life? J. Hum. Hypertens. 2001;15(Suppl 1):S65–S68. doi: 10.1038/sj.jhh.1001081. [DOI] [PubMed] [Google Scholar]
- 21.Harrison JA, Mullen PD, Green LW. A Meta analysis of studies of the health belief model with adults. Heal Educ Res. 1992;7(1):107–116. doi: 10.1093/her/7.1.107. [DOI] [PubMed] [Google Scholar]
- 22.Figueiras M, Marcelino DS, Claudino A, Cortes MA, Maroco J, Weinman J. Patients' illness schemata of hypertension: The role of beliefs for the choice of treatment. Psychol Heal. 2010;25(4):507–517. doi: 10.1080/08870440802578961. [DOI] [PubMed] [Google Scholar]
- 23.Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health, and behavior: A perceptual-cognitive approach. Psychol Heal. 1998;13(4):717–733. doi: 10.1080/08870449808407425. [DOI] [Google Scholar]
- 24.Rosenstock IM. Why people use health services. Milbank Memorial Fund Quarterly-Health and Society. 1966;44(3):94–127. doi: 10.2307/3348967. [DOI] [PubMed] [Google Scholar]
- 25.Fiese BH, Wamboldt FS, Anbar RD. Family asthma management routines: connections to medical adherence and quality of life. J Pediatr. 2005;146(2):171–176. doi: 10.1016/j.jpeds.2004.08.083. [DOI] [PubMed] [Google Scholar]
- 26.Bokhour BG, Berlowitz DR, Long JA, Kressin NR. How do providers assess antihypertensive medication adherence in medical encounters? J Gen Intern Med. 2006;21(6):577–583. doi: 10.1111/j.1525-1497.2006.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bell RA, Kravitz RL. Physician counseling for hypertension: what do doctors really do? Patient Educ Couns. 2008;72(1):115–121. doi: 10.1016/j.pec.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 28.Cooper LA. A 41-year-old African American man with poorly controlled hypertension: review of patient and physician factors related to hypertension treatment adherence. JAMA. 2009;301(12):1260–1272. doi: 10.1001/jama.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Street RL, Jr, Haidet P. How well do doctors know their patients? Factors affecting physician understanding of patients' health beliefs. J Gen Intern Med. 2011;26(1):21–27. doi: 10.1007/s11606-010-1453-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Frosch DL, Elwyn G. I believe, therefore I do. J Gen Intern Med. 2011;26(1):2–4. doi: 10.1007/s11606-010-1560-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Knight KM, McGowan L, Dickens C, Bundy C. A systematic review of motivational interviewing in physical health care settings. Br J Heal Psychol. 2006;11:319–332. doi: 10.1348/135910705X52516. [DOI] [PubMed] [Google Scholar]
- 32.Weiner SJ, Schwartz A, Weaver F, Goldberg J, Yudkowsky R, Sharma G, et al. Contextual errors and failures in individualizing patient care: a multicenter study. Ann Intern Med. 2010;153(2):69–75. doi: 10.7326/0003-4819-153-2-201007200-00002. [DOI] [PubMed] [Google Scholar]
- 33.Haidet P, Paterniti DA. "Building" a history rather than "taking" one: a perspective on information sharing during the medical interview. Arch Intern Med. 2003;163(10):1134–1140. doi: 10.1001/archinte.163.10.1134. [DOI] [PubMed] [Google Scholar]
- 34.Bodenheimer T, Laing BY. The teamlet model of primary care. Ann. Fam. Med. 2007;5(5):457–461. doi: 10.1370/afm.731. [DOI] [PMC free article] [PubMed] [Google Scholar]