ABSTRACT
BACKGROUND
Tobacco treatment is underused in primary care. We designed a Tobacco Care Management system to increase the delivery of treatment and reduce the burden on primary care providers (PCPs). A one-click functionality added to the electronic health record (EHR) allowed PCPs to refer smokers to a centralized tobacco treatment coordinator (TTC) who called smokers, provided brief counseling, connected them to ongoing treatment and gave feedback to PCPs.
OBJECTIVE
To study the system’s feasibility and acceptability among PCPs, and its utilization by smokers.
DESIGN
Using a mixed methods design, we documented system utilization quantitatively from February 1, 2010 to July 31, 2011, and conducted two focus groups with PCPs in June 2011.
PARTICIPANTS
Thirty-six PCPs and 2,894 smokers from two community health centers in Massachusetts.
MAIN MEASURES
Quantitative: One-click referral utilization by PCPs, proportion of smokers referred and connected to treatment. Qualitative: PCPs’ reasons for use, barriers to use, and experiences with feedback.
KEY RESULTS
Twenty-nine PCPs (81 %) used the functionality more than once, generating 466 referrals for 15 % of known smokers seen during the study. The TTC reached 260 (56 %) of the referrals and connected 135 (29 %) to additional treatment. The director of one center sent PCPs monthly feedback about their utilization compared to peers. These PCPs referred a greater proportion of their known smokers (18 % vs. 9 %, p < 0.0001) and reported that monthly feedback motivated referrals. PCPs attending focus groups (n = 24) appreciated the system’s simplicity, access to updated resources, and time-efficient way to address smoking, and wanted more feedback about cessation outcomes. They collectively supported the system’s continuation.
CONCLUSIONS
A novel EHR-based Tobacco Care Management system was adopted by PCPs, especially those receiving performance feedback, and connected one-third of referred smokers to treatment. The model has the potential to improve the delivery and outcomes of evidence-based tobacco treatment in primary care.
KEY WORDS: care management, technology assessment, primary care, smoking cessation
BACKGROUND
Smoking remains the leading preventable cause of death in the United States.1,2 Despite the availability of effective treatments for tobacco dependence, most quit attempts fail, with only one-third of smokers using treatment.3 The healthcare system could help to bridge this treatment gap. Physician-delivered interventions are effective, but not routinely provided.3,4 A physician’s brief advice to quit at an office visit increases smoking cessation rates, but only half of smokers who see a physician each year recall receiving this advice.3 Furthermore, most smokers need more than advice to quit. Brief physician counseling plus referral and follow-up for additional care is more effective, but this is even less often provided.5,6
National clinical guidelines recommend that physicians routinely screen patients for tobacco use, advise smokers to quit, and assist them with treatment.4 Physicians’ compliance with these guidelines is limited by a lack of training, perceived lack of skills, and time constraints due to competing priorities at visits.4,7 A new model for tobacco treatment is needed. Ideally, it should include coordination of care across elements of the healthcare system, linkage to community services, and enhanced patient access.8
We and others have developed models of tobacco treatment that incorporate some of these elements.9–14 We tested a set of enhanced electronic health record (EHR) functionalities to improve tobacco treatment delivery by primary care providers (PCPs). These functionalities increased smokers’ rate of accessing counseling, but PCPs used the tools infrequently.14 Another system facilitated referral of smokers to a tobacco care coordinator based within the healthcare system,9 while other investigators facilitated referral of smokers from a PCP’s office to a community-based telephone quitline, located outside the healthcare system.10–12,15–18 This prior work demonstrates that integrating referrals into the EHR has the potential to improve delivery of tobacco treatment and warrants further study.
Using elements from these models, we designed a new Tobacco Care Management system and implemented it at two community health centers affiliated with our integrated healthcare delivery system. The sites were chosen because they serve low-income patients who have a high smoking prevalence in national surveys.19 We evaluated the feasibility and acceptability of the care management system during the first 18 months of implementation. We assessed smokers’ uptake of connections to treatment resources, and PCPs’ utilization, satisfaction, and experiences with the system.
METHODS
Study Setting and Subjects
Two community health centers (Health Centers 1 and 2) in Boston, Massachusetts, with a total of 36 PCPs, including 21 faculty physicians (MDs), three nurse practitioners (NPs), and 12 physician trainees, participated in the study between February 1, 2010 and July 31, 2011. Each health center is affiliated with an academic medical center in the Partners HealthCare System. The study was approved by Partners HealthCare System’s Institutional Review Board.
Both health centers use a locally-developed electronic health record (EHR), which includes progress notes, laboratory results, medication lists, electronic prescribing, and clinical reminders, including a reminder to record smoking status. A screen for documenting smoking status in a coded field can be accessed by all staff. At the start of the study, 57 % of patients with recent visits had a smoking status documented in a coded field and 18 % of those documented (10 % of all patients) were current smokers.
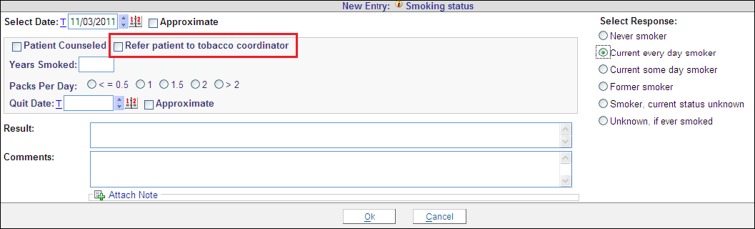
Intervention
We designed the Tobacco Care Management system to function within existing practice infrastructure and workflow. From our previously tested EHR functionalities, we selected the most popular feature, one-click referral to tobacco treatment.14 We streamlined this feature and incorporated elements of a Veteran’s Affairs system, such as the internal tobacco care coordinator (TTC).9 With the new Tobacco Care Management system, when PCPs document patients’ tobacco use, they can refer smokers to a TTC located centrally in the healthcare system with one mouse-click (Fig. 1). Clicking the referral option generated an email to a TTC, who proactively called the patient up to three times. Those patients who did not answer received a voice message identifying the caller from Partners Healthcare System regarding a referral from their doctor, with a call-back number that accepted voice messages. For those who were reached, the TTC conducted an assessment, including screening for medication contraindications, provided brief counseling, and offered to connect the patient to more intensive treatment services. Intensive services included multi-session telephone counseling and two weeks of nicotine patches provided free from the state quitline. In-person counseling was also available through the healthcare system.
Figure 1.
One-click option to refer to a tobacco treatment coordinator.
The TTC recorded the outcome of the referral in an electronic database of referred smokers, entered a note in the EHR and emailed feedback about the smoker to the PCP, including medication recommendations and whether the smoker was connected to the quitline or local resources. The internal TTC model allowed two-way communication with the primary care team about medication management and counseling.
After obtaining practice leaders’ agreement to participate in the study, research staff trained PCPs at one session held at each health center prior to implementing the functionality. The TTC demonstrated how to make the referral and explained what she would do after receiving a referral, what treatment resources she would offer, what would be documented in the EHR and what feedback would be provided to PCPs. We did not specify which types of smokers PCPs should refer in terms of readiness to quit, because we wanted to give PCPs the option to decide who might benefit from the service. During the intervention period, PCPs and practice leaders could also contact study staff or the TTC with questions about the system or specific patients. The TTC sent a performance report of the number of referrals made each month by PCPs in each health center to the respective medical directors. Without prompting by study staff, the medical director at Health Center 1 forwarded the monthly performance report to all PCPs at that health center. The medical director at the Health Center 2 did not distribute the report. There was no further proactive training or detailing beyond the pre-implementation session and the monthly feedback reports sent to medical directors.
Assessment
Quantitative
We used EHR records to measure demographic characteristics and health insurance of patients identified as smokers who were seen at the health centers during the study period, and the proportion of those who were referred using the one-click functionality. Using TTC records, we measured the outcome of the TTC’s efforts to contact referred patients, including the number of call attempts, the number of patients reached by telephone, and the number who accepted referral to further tobacco treatment services.
Qualitative
We evaluated PCPs’ experiences and satisfaction with the Tobacco Care Management system by conducting two one-hour focus group discussions, one at each participating health center, in June 2011. Study staff moderated the focus groups using a semi-structured interview guide and audio-recorded them for transcription. Content areas of the guide were PCPs’ reasons for use, patient selection, barriers to use, and experience with programmatic feedback.
Analysis
Quantitative
To quantify utilization of the Tobacco Care Management system, we calculated the average number of referrals per PCP, and adjusted for differences in the number of sessions worked by individual PCPs per full-time equivalent (FTE). We also measured the proportion of known smokers seen during the study period who were referred using the one-click option. We compared smokers who were referred to smokers who were not referred by demographics and insurance status using chi-square and unpaired t-tests. We also report the number of calls made by the TTC, the proportion of patients reached by telephone, and the proportion of patients connected to further treatment.
Qualitative
We performed content analyses of the transcripts and notes from the focus groups using a multi-step process. Two investigators (JKK and GRK) individually reviewed the transcripts before manually structuring the data into major themes. Coding was conducted within each theme. Coding results were compared and any discrepancies were resolved through discussions and review of raw data (JKK, GRK, and ERP).
RESULTS
Primary Care Provider Utilization of the Referral Functionality
Over the 18-month study, 2,894 known smokers made 28,032 visits to the health centers, representing 16 % of all visits. Characteristics of the known smokers differed by health center. Compared to Center 2, Center 1 had a lower proportion of known smokers who were non-white (14 % vs. 65 %, p < 0.0001) and on Medicaid (27 % vs. 42 %, p < 0.0001). A total of 466 referrals to the TTC were made for 422 unique smokers (15 % of all known smokers seen). Forty-two smokers were referred multiple times. Smokers who were referred did not differ by age, gender, race/ethnicity, or insurance from smokers who were not referred (Table 1).
Table 1.
Demographics and Insurance for Documented Smokers Visiting the Health Centers by One-Click Referral, February 1, 2010 Through July 31, 2011
| Smoker characteristics | Health Center 1 | Health Center 2 | ||||
|---|---|---|---|---|---|---|
| One-click referrals (n = 325) | Smokers not referred (n = 1,505) | p* | One-click referrals (n = 97) | Smokers not referred (n = 967) | p* | |
| Mean age [years] (SD) | 48 (13) | 47 (16) | 0.95 | 44 (12) | 43 (15) | 0.64 |
| Female—n (%) | 180 (55) | 845 (56) | 0.80 | 48 (49) | 521 (54) | 0.41 |
| Race—n (%) | ||||||
| White | 276 (85) | 1,301 (86) | 0.91 | 33 (34) | 340 (35) | 0.08 |
| Hispanic | 18 (6) | 83 (6) | -- | 35 (36) | 409 (42) | -- |
| Black | 18 (5) | 76 (5) | -- | 16 (16) | 155 (16) | -- |
| Other † | 12 (4) | 46 (3) | -- | 13 (13) | 63 (7) | -- |
| Insurance—n (%) | ||||||
| Medicaid | 83(26) | 402 (27) | 0.08 | 51 (53) | 400 (41) | 0.16 |
| Medicare | 57 (18) | 259 (17) | -- | 11 (11) | 124 (13) | -- |
| Commercial | 135 (42) | 533 (35) | -- | 23 (24) | 321 (33) | -- |
| Other (Self-pay, uninsured) | 50 (15) | 311 (21) | -- | 12 (12) | 122 (13) | -- |
*P values based on unpaired t-test for age and chi-squared tests for categorical variables, comparing referred smokers to non-referred smokers, within each Health Center
†Other race includes: Asian, American Indian, and unknown/ refused
Of 36 PCPs with access to the one-click referral, 29 (81 %) used it more than once, four PCPs (11 %) used the functionality only once and three PCPs (8 %) never used it. The mean number of referrals among PCPs who used it more than once was 16 referrals over 18 months. The number of referrals varied substantially by health center and PCP. Health Center 1 made 41.6 referrals per FTE, whereas Health Center 2 made 17.9 per FTE. In terms of individual smokers, PCPs at Health Center 1 referred a higher proportion of known smokers (18 %; 325/1,830) than did Health Center 2 PCPs (9 %; 97/1,064) (p < 0.0001). Four frequent users, all from Health Center 1 and who were receiving the monthly performance reports from their medical director, made from 41 to 67 referrals representing 20 to 24 % of the smokers they saw. We had limited access to PCP characteristics that may be associated with utilization; besides characteristics already mentioned, PCPs’ gender did not differ by health center (55 % female at both sites).
Outcome of Referrals Made
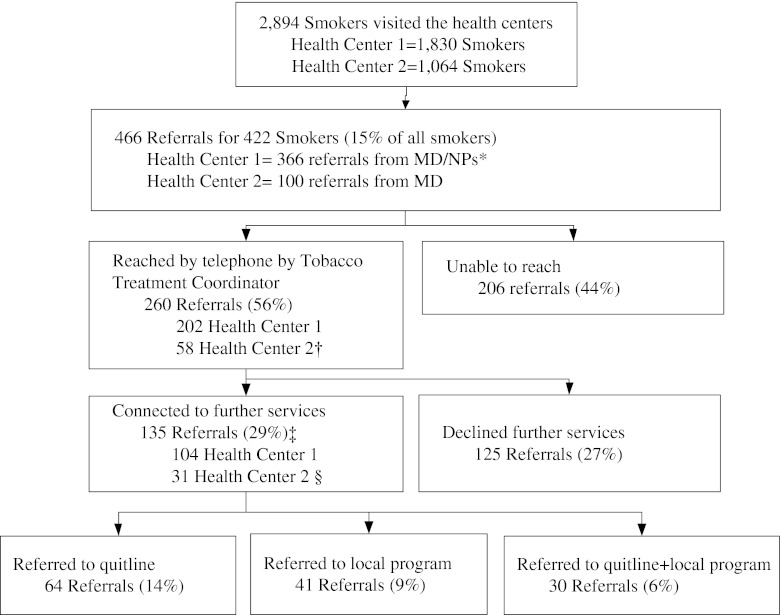
The TTC made 1,064 calls and reached by telephone 9 % of known smokers or 260 (56 %) of the 466 referrals. The proportion reached did not differ by health center (55 % at Center 1 versus 58 % at Center 2, p = 0.65). The median time from receipt of referral to first call attempt by the TTC was 4 days (IQR 5); 84 % of referrals were called within 1 week. Among the 206 referrals not reached, 23 (11 %) had no working number and 183 (89 %) were not reached after three attempts. Of those reached by the TTC, 135 (29 % of referrals) agreed to be connected to additional treatment services (Fig. 2).
Figure 2.
Referrals to the Tobacco Care Management system in two Community Health Centers, February 1, 2010 through July 31, 2011. * Health Center 1 provided primary care providers with monthly performance feedback and made 366 referrals for 325 individual smokers; Health Center 2 did not send monthly feedback and made 100 referrals for 97 individual smokers, chi-squared test for proportion of referred smokers, p < 0.001. † Proportion reached in Health Center 1 vs. Health Center 2, two-tailed Fisher’s exact test, p = 0.65. ‡In terms of individual smokers, 133 (32 %) were connected to further services. § Proportion connected to services in Health Center 1 vs. Health Center 2, two-tailed Fisher’s exact test, p = 0.62.
PCP Focus Groups
Twenty-four (67 %) of 36 PCPs attended and participated in focus group discussions. There were 14 women and ten men, including one trainee.
Reasons for Using the One-Click Referral Functionality
All PCPs felt the one-click option was easy to use, especially compared to other ways of accessing tobacco treatment, and that this option made it easy to keep track of available smoking cessation resources. As one PCP explained, “I find it almost impossible to keep track of what the local resources for smoking are, except for the one-click which is really simple.” Most PCPs used the one-click to offer further treatment to smokers, but not to replace their own efforts. Others used the one-click option when they did not have enough time to discuss smoking cessation themselves.
Types of Smokers Referred
Although PCPs collectively thought the referral option was useful, they differed in the types of smokers that they referred in terms of readiness to quit. Some used it as a way to encourage smokers to think about quitting or commit to a quit date. Others referred only smokers who had a quit date, to follow-up on the quit attempt.
Barriers to Use
PCPs were discouraged when patients they referred were not reached by the TTC, or declined services once they were reached. Some PCPs wanted more information about whether their referral was helping the patient. They thought information about cessation outcomes for the referral system would motivate their use.
Experiences with Feedback
The monthly performance report that was forwarded by the medical director to Health Center 1 PCPs was identified as a reason for making referrals. As one PCP explained, “We get an excel spreadsheet about who is using it and who is not. I think that is an incentive to use it…peer pressure.”
Comments of Frequent Users
The frequent users noted how the one-click option and email feedback from the TTC fit conveniently into their workflow. Their comments did not differ from lower volume users in the types of smokers referred or their disappointment when patients were not reached.
Although improvements were suggested, PCPs collectively thought the system should be continued.
DISCUSSION
This technology-enhanced Tobacco Care Management System offers a promising solution to the challenge of under-treatment of tobacco dependence in primary care. The system allowed PCPs to enlist another provider in assisting patients to quit smoking, largely by linking them to a telephone quitline, a resource that is available free to smokers nationwide. This was accomplished with little burden or disruption of providers’ workflow during office practice. As evidence of the systems’ acceptability, over 80 % of PCPs used the EHR functionality more than once, and PCPs who received feedback about their performance compared to peers made more referrals. Overall, PCPs referred 15 % of all the known smokers that they saw during the study period. This is within the range of referral rates of smokers to telephone counseling (4 % to 21 %) achieved by care management systems that facilitated referrals directly to community-based quitlines.10–12 Given the impact of smoking cessation on individual patients’ health, increasing smokers’ contacts with effective treatments has large implications for patients.
A distinctive feature of our system, like that implemented in a veteran population, is the location of the TTC within the healthcare system, with full access to medical records.9 This feature allows for coordination between the TTC and the primary care team, and offers two-way communication about referral outcomes and medication. The central location of the TTC also makes the program scalable within a healthcare system to multiple centers with little additional investment. An alternative strategy is to have the PCP refer directly to the community-based quitline.10–13,16–18 While direct referral has advantages in efficiency, existing systems have limited two-way communication with the PCP regarding smokers’ treatment preferences and outcomes. The impact of this could be moderated with enhanced feedback from the quitline.
The TTC reached 56 % of patients referred, a rate comparable to that achieved by the one other system which has used an internal care coordinator (61 %), but our rate of connection to additional treatments was lower (29 % versus 45 %).9 This may, in part, result from differences in types of smokers referred. PCPs referred smokers who were not ready to quit, as well as those preparing to make a quit attempt. It is likely that less motivated smokers had lower rates of contact and acceptance of additional treatment than smokers who were ready to quit. We still succeeded in connecting 3 % of known smokers in our system to the state quitline, which compares favorably to the 1 % of smokers nationally who access quitlines annually.20
The study illustrates the value of performance feedback in quality improvement efforts. Quantitative data demonstrated a large difference between health centers in utilization of the system, and focus groups supported our hypothesis that this could be due to monthly performance feedback provided at the high-use health center. Similar to prior studies, PCPs recognized the performance report as one reason they used the referral system.10 Feedback increased the number of referrals made, and this translated into more smokers connected to treatment.
PCPs were discouraged when smokers were not reached or declined treatment. As mentioned, this may partly be due to referral of some unmotivated smokers. The TTC’s message could easily be tailored to patients’ readiness to quit, and incorporate novel methods to move unmotivated smokers towards quitting, such as a “practice quit attempt.” This might increase the proportion of smokers accepting assistance and ultimately impact quit rates.21 Clarifying that the TTC can help all types of smokers, and reframing the feedback regarding referral outcomes to give context to expectations for rates of successful contact and treatment, may mitigate PCPs’ discouragement.
Efficient use of the one-click referral option requires smoking status to be documented in a coded field in the EHR. At the time of the study, only 57 % of patients had smoking status documented in this way. Promoting structured documentation of tobacco use has been a challenge for our large, diverse system, but it is improving with the inclusion of smoking status documentation among the federal government’s meaningful use standards for EHRs.22 This should improve the reach of our system to all smokers in the healthcare system in the future. Verifying the status of patients without structured documentation is beyond the scope of this analysis, and we do not know how the proportion of known smokers differs from the actual proportion of smokers in the health centers.
Our study has several limitations. First, because the study was conducted in two community health centers that are part of an integrated healthcare delivery system, the generalizability of the findings to different populations, clinic types, and healthcare systems is uncertain. However, we believe that the system’s simplicity should facilitate its dissemination. Furthermore, despite a relatively low smoking prevalence (14 %), Massachusetts resembles other states in treatment availability and use.19 Smoking cessation treatments are not universally covered by insurers and the Massachusetts quitline is underused by its population. Second, due to resource limitations, we could not assess the impact of the care management system on abstinence. Fortunately, there is strong evidence for the real-world effectiveness of telephone counseling and quitlines.23,24 Finally, the implementation included minimal training and detailing with a single session per clinic. We did not control other aspects of implementation so that, other than the performance feedback described at focus groups, we are limited in our ability to explain how other elements of implementation contributed to the differences in utilization.
CONCLUSIONS
A technology-enhanced Tobacco Care Management system was feasible and acceptable to PCPs at two community health centers. Our system functioned in a diverse, integrated healthcare system, and PCPs offered it to all types of smokers, including those less motivated to quit. The design, with its simple EHR enhancement and centrally-located tobacco treatment coordinator, is a promising system of integrated care that could be implemented in other healthcare systems that are developing new models for chronic disease management.
Acknowledgements
We are grateful for the participation of the Community Health Centers, and wish to thank Southern Jamaica Plain Health Center, Charlestown Health Center, Michael Lambert, MD, and Mark Eisenberg, MD. We would also like to acknowledge Elizabeth Mort, MD, MPH and Partners HealthCare System’s High Performance Medicine for support of the project.
Partners Healthcare, Inc. funded the Tobacco Care Management program and supported the Tobacco Care coordinator. Dr. Kruse’s effort was supported by grant #T32HP12706-03-00 from the Health Resources and Services Administration for the Harvard General Medicine Fellowship. Dr. Rigotti’s effort was supported by NIH grant #K24-HL08880. The funders of these grants had no role in study design, conduct, data analysis, interpretation, or manuscript preparation, review, or approval.
An earlier version of this information was accepted for presentation as a poster at the Society for Research in Nicotine and Tobacco 18th Annual Meeting, Houston, Texas, March 15, 2012 and the Society for General Internal Medicine 35th Annual Meeting, Orlando, Florida May 12, 2012.
Conflict of Interest
The authors declare that they do not have a conflict of interest. Nancy A. Rigotti reports unpaid consultancy for Pfizer and Alere Wellbeing, research grants to MGH from Nabi Biopharmaceuticals and Pfizer, and royalties from UpToDate.
REFERENCES
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Quitting smoking among adults—United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1513–1519. [PubMed] [Google Scholar]
- 4.Fiore MC, Jaen CR, Baker T, Bailey WC, Benowitz NL, Curry SJ, et al. Clinical Practice Guideline. Rockville: U.S. Department of Health and Human Services. Public Health Service; 2008. Treating Tobacco Use and Dependence: 2008 Update. [Google Scholar]
- 5.Quinn VP, Stevens VJ, Hollis JF, Rigotti NA, Solberg LI, Gordon N, et al. Tobacco-cessation services and patient satisfaction in nine nonprofit HMOs. Am J Prev Med. 2005;29(2):77–84. doi: 10.1016/j.amepre.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 6.Benowitz NL. Chronic disease management approach to treating tobacco addiction: comment on “nicotine therapy sampling to induce quit attempts among smokers unmotivated to quit”. Arch Intern Med. 2011;171(21):1907–1909. doi: 10.1001/archinternmed.2011.545. [DOI] [PubMed] [Google Scholar]
- 7.Schroeder SA. What to do with a patient who smokes. JAMA. 2005;294(4):482–487. doi: 10.1001/jama.294.4.482. [DOI] [PubMed] [Google Scholar]
- 8.American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP), American Osteopathic Association (AOA). Joint principles of the patient-centered medical home. March 2007. www.medicalhomeinfo.org/Joint%20Statement.pdf. Accessed June 29, 2012.
- 9.Sherman SE, Takahashi N, Kalra P, Gifford E, Finney JW, Canfield J, et al. Care coordination to increase referrals to smoking cessation telephone counseling: a demonstration project. Am J Manag Care. 2008;14(3):141–148. [PubMed] [Google Scholar]
- 10.Bentz CJ, Bayley KB, Bonin KE, Fleming L, Hollis JF, Hunt JS, et al. Provider feedback to improve 5A’s tobacco cessation in primary care: a cluster randomized clinical trial. Nicotine Tob Res. 2007;9(3):341–349. doi: 10.1080/14622200701188828. [DOI] [PubMed] [Google Scholar]
- 11.An LC, Bluhm JH, Foldes SS, Alesci NL, Klatt CM, Center BA, et al. A randomized trial of a pay-for-performance program targeting clinician referral to a state tobacco quitline. Arch Intern Med. 2008;168(18):1993–1999. doi: 10.1001/archinte.168.18.1993. [DOI] [PubMed] [Google Scholar]
- 12.Rothemich SF, Woolf SH, Johnson RE, Devers KJ, Flores SK, Villars P, et al. Promoting primary care smoking-cessation support with quitlines: the QuitLink Randomized Controlled Trial. Am J Prev Med. 2010;38(4):367–374. doi: 10.1016/j.amepre.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Borland R, Balmford J, Bishop N, Segan C, Piterman L, McKay-Brown L, et al. In-practice management versus quitline referral for enhancing smoking cessation in general practice: a cluster randomized trial. Fam Pract. 2008;25(5):382–389. doi: 10.1093/fampra/cmn046. [DOI] [PubMed] [Google Scholar]
- 14.Linder JA, Rigotti NA, Schneider LI, Kelley JH, Brawarsky P, Haas JS. An electronic health record-based intervention to improve tobacco treatment in primary care: a cluster-randomized controlled trial. Arch Intern Med. 2009;169(8):781–787. doi: 10.1001/archinternmed.2009.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Willett JG, Hood NE, Burns EK, Swetlick JL, Wilson SM, Lang DA, et al. Clinical faxed referrals to a tobacco quitline: reach, enrollment, and participant characteristics. Am J Prev Med. 2009;36(4):337–340. doi: 10.1016/j.amepre.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Sheffer MA, Baker TB, Fraser DL, Adsit RT, McAfee TA, Fiore MC. Fax referrals, academic detailing, and tobacco quitline use a randomized trial. Am J Prev Med. 2012;42(1):21–28. doi: 10.1016/j.amepre.2011.08.028. [DOI] [PubMed] [Google Scholar]
- 17.Cantrell J, Shelley D. Implementing a fax referral program for quitline smoking cessation services in urban health centers: a qualitative study. BMC Fam Pract. 2009;10:81. doi: 10.1186/1471-2296-10-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernstein SL, Jearld S, Prasad D, Bax P, Bauer U. Rapid implementation of a smokers’ quitline fax referral service in an urban area. J Health Care Poor Underserved. 2009;20(1):55–63. doi: 10.1353/hpu.0.0112. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention Vital signs: current cigarette smoking among adults aged ≥18 years—United States, 2005–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1207–1212. [PubMed] [Google Scholar]
- 20.Barry M, Saul J, Bailey L. U.S. quitlines at a crossroads: Utilization, budget, and service trends 2005–2010. Phoenix, Arizona: 2010 Contract No.: SR-01.
- 21.Carpenter MJ, Hughes JR, Gray KM, Wahlquist AE, Saladin ME, Alberg AJ. Nicotine therapy sampling to induce quit attempts among smokers unmotivated to quit: a randomized clinical trial. Arch Intern Med. 2011;171(21):1901–1907. doi: 10.1001/archinternmed.2011.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 23.Zhu SH, Anderson CM, Tedeschi GJ, Rosbrook B, Johnson CE, Byrd M, et al. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med. 2002;347(14):1087–1093. doi: 10.1056/NEJMsa020660. [DOI] [PubMed] [Google Scholar]
- 24.Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2006;3:CD002850. doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]