Abstract
Aims
Young adulthood is a challenging period for patients with Type 1 diabetes as developmental changes complicate Type 1 diabetes management and gaps in care may arise as patients transition from paediatric to adult providers. This period has been associated with worsening diabetes outcomes. One approach to aid young adults during this transition period could entail professionally led support groups to enhance self-motivation and facilitate peer-to-peer interactions. We implemented and evaluated a support group for young adults with Type 1 diabetes as a pilot project.
Methods
Young adults with Type 1 diabetes (18–30 years) participated in monthly, professionally led support groups for 5 months. Questionnaires were completed pre- and post-group and chart review data were collected regarding glycaemic control and visit frequency in the year before and after group participation.
Results
Participation in the group was associated with improvement in HbA1c and decreased self-reported diabetes burden, along with a trend for an increase in diabetes-related self-care behaviours. Frequency of visits did not vary from pre- to post-group. Discussion topics identified by participants included managing diabetes in day-to-day life, experiences and interactions with others who do not have diabetes and emotions related to diabetes. Participants identified that they sought a diabetes care team that offers knowledge, support and a multidisciplinary team.
Conclusions
Professionally led support groups may have utility for increasing social support and optimizing diabetes outcomes in young adults with Type 1 diabetes.
Keywords: support groups, Type 1 diabetes, young adults
Introduction
Young adulthood is a difficult period for patients with Type 1 diabetes. During this period, many developmental changes complicate Type 1 diabetes management, such as navigating college, seeking employment and living away from home for the first time [1,2]. Additionally, many patients with Type 1 diabetes transition their care from paediatric to adult diabetes providers during young adulthood, which has been associated with loss to follow-up care, deteriorating glycaemic control and emergence of diabetes complications [3–5].
Over the past decade, the topic of transitioning to adult care has been a concern for clinicians and researchers from many sub-specialties [6–10]. Several professional organizations recognize the importance of appropriate health care during this period and the need to develop transition guidelines [2,11–13]. Empirical studies are needed in this area.
One approach to helping young adults during this transition period could include professionally led support groups to facilitate peer-to-peer interactions [11]. This may help patients reduce stress and improve problem-solving skills. We implemented a support group for young adults with Type 1 diabetes as a pilot to assess interest for this service, to collect information on the needs/wants of participants regarding diabetes care and to assess the impact of group participation on diabetes management and outcomes.
Patients and methods
Flyers for the support group were posted at the Joslin Diabetes Center and local colleges. Paediatric and adult medical providers at Joslin were made aware of the programme and flyers were sent to age-appropriate individuals (18–30 years) with Type 1 diabetes. Prior to group registration, the group leader spoke to interested patients to answer questions and screen out those with underlying unmanaged major mental illness requiring more intensive individual therapy. Two patients expressed interest and then decided not to participate. All interested patients were enrolled.
Two separate young adult support groups met monthly for five sessions. Participants completed questionnaires at the first and last sessions. Data collected included demographic data, diabetes management information and measures of diabetes-related burden and frequency of self-care behaviours. In addition, retrospective chart review data were collected on HbA1c and visit frequency 1 year prior to and after the first group session.
Measures
Problem Areas in Diabetes survey
The Problem Areas in Diabetes survey (PAID) [14] is a validated, self-report questionnaire designed to measure burden related to having diabetes. Higher score indicates greater burden.
Self-Care Inventory-R
The Self-Care Inventory-R (SCI-R) [15] is a validated, self-report questionnaire designed to measure the frequency of self-care behaviours. Higher score indicates greater frequency of self-care behaviours.
Support group procedures
The group format endorsed the notion that support groups for patients with chronic illness can be helpful in providing peer support and encouragement, improving quality of life and illness management and increasing self-efficacy [16,17]. A clinical psychologist experienced with working with young adults with Type 1 diabetes facilitated all group sessions, which followed a similar, non-manualized format. At the first group session, participants were asked to identify topics for discussion, including barriers to self-care behaviours. After the first session, the facilitator organized the topics into themes for the remaining sessions. One week prior to each subsequent group, the facilitator emailed participants with the topics on the agenda, asking each participant to think about a story or question to share with the group.
Statistical analysis
Quantitative analyses used SAS (version 9.2 for Windows; SAS Institute, Cary, NC, USA). All data are presented as means ± sd or per cent as indicated. Statistics included Pearson correlations, paired t-tests and χ2-test analyses. A P-value of < 0.05 conveyed statistical significance. For qualitative analyses, themes within the data were identified and reported.
Results
Participants were 15 young adults with Type 1 diabetes (93% female, 92% white; see Table 1). Mean age was 26 ± 3.3 years, diabetes duration was 10.6 ± 8.0 years (range 1–22 years) and 40% were currently treated with an insulin pump. Mean self-reported HbA1c was 55 ± 14 mmol/mol (7.2 ± 1.3%), while mean laboratory HbA1c prior to the group start was 59 ± 16 mmol/mol (7.6 ± 1.4%) (r = 0.99, P < 0.0001). Participants were highly educated (> 85% obtained a bachelor's degree or higher), 80% were single and 93% had no children. The majority were seen in an adult diabetes clinic (75%), with the remainder treated by paediatric providers. The majority (86%) had never before participated in any diabetes support group or community-based programme.
Table 1.
Participant characteristics (n = 15)
| Gender | Female | 93% |
| Male | 7% | |
| Race/ethnicity | White | 92% |
| Other | 8% | |
| Age (years) | 26 ± 3.3 | |
| Diabetes duration (years) | 10.6 ± 8.0 | |
| Education* | High school | 7% |
| Associate's degree | 7% | |
| Bachelor's degree | 43% | |
| Master's degree | 36% | |
| PhD | 7% | |
| Unmarried (%) | 80 | |
| No children (%) | 93 | |
| Type of diabetes care | Adult clinic | 73% |
| Paediatric clinic | 27% | |
| Current student (%) | 20 | |
| Diabetes regimen (% pump treated) | 40 | |
| Self-reported HbA1c (mmol/mol) (%) | 54 ± 14 7.2 ± 1.3 |
|
| Laboratory HbA1c prior to group start (mmol/mol) (%) | 59 ± 16 7.6 ± 1.4 |
High school = grade 12; Associate's degree = 2 year college degree; Bachelor's degree = 4 year college degree; Master's degree = Post college degree; PhD = Doctorate degree
Diabetes burden and self-care
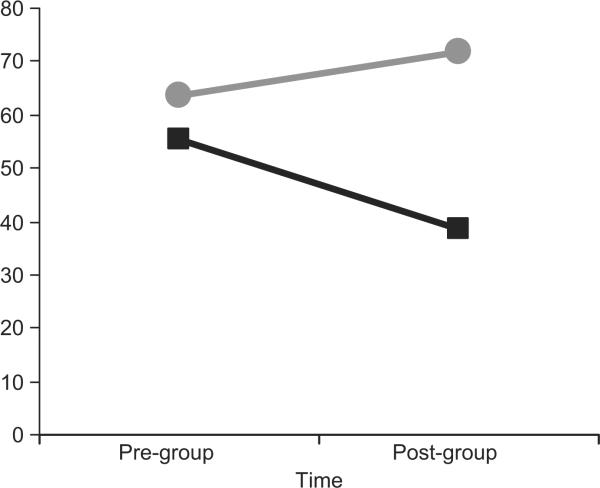
Participants completed the Problem Areas in Diabetes survey and the Self-Care Inventory-R to measure burden related to diabetes and diabetes self-care, prior to the group and at the last group session (Fig. 1). Scores on the Problem Areas in Diabetes survey decreased significantly from pre- to post-group (pre: 55.5 ± 15.6; post: 38.5 ± 19.2; P = 0.02), indicating that participants endorsed less diabetes-related burden after group participation. Scores on the Self-Care Inventory increased from pre- to post-group (pre: 63.6 ± 12.3; post: 72.0 ± 13.7; P = 0.09), indicating that participants increased their self care behaviours, with a trend towards significance.
FIGURE 1.
Problem Areas in Diabetes ( ) and Self-Care Inventory (
) and Self-Care Inventory ( ) results.
) results.
Glycaemic control and utilization of care pre- and post-group
After excluding two participants who did not have documented HbA1c values in the electronic health record in the year prior to the group and one who did not have a value in the year after the first group session, pre- and post-group HbA1c data were available for 12 participants. Mean HbA1c was 63 ± 15 mmol/mol (7.9 ± 1.4%) during the year prior to the group and 60 ± 12 mmol/mol (7.6 ± 1.1%) in the year after the group (P = 0.10), with 2/3 of participants demonstrating improvement.
Data regarding frequency of visits at Joslin in the year prior to and the year after the first group session included encounters with doctors, nurse practitioners, registered nurses/certified diabetes educators, dieticians, exercise physiologists and mental health providers. Mean and median numbers of visits were approximately the same pre- and post-group (pre: 8.6 ± 7.2 and 7; post: 7.9 ± 5.6 and 8, respectively). The number of visits between participants varied greatly (0–27 pre; 2–27 post; some participants were not Joslin patients). There was no relationship between change in HbA1c and change in visit frequency (pre- to post-group).
Topics important to group participants
Following a request for discussion topics for group sessions, participants identified three unique themes: (1) objective approaches to managing diabetes in day-to-day life; (2) subjective recollections of interactions with peers without diabetes and others regarding diabetes; (3) emotions related to insecurities, concerns about imperfections in care, stress, anxiety and sadness. Attending to diabetes in day-to-day life was a popular topic, which included how to incorporate diabetes management tasks in the workplace and/or at school, explaining challenges related to diabetes to others who are unaware of the disease and its needs, and handling unexpected factors related to diabetes management, such as delayed mealtimes. Next, participants wanted to discuss experiences others have had related to diabetes and were particularly interested in hearing about `how other people aren't perfect'. Third, discussions around emotional issues included stress caused by frequent diabetes management tasks and anxiety related to imperfections in diabetes management, along with fear of complications.
Most participants, on the one hand, noted relative ease with which to take insulin and to comprehend the diabetes management programme, including attention to diet and healthful eating. On the other hand, most participants endorsed challenges with the unremitting demands of constant diabetes management, stresses related to coping with others with regard to diabetes care and general anxiety regarding diabetes during young adulthood.
Preferences for diabetes care
We asked these young adults about their preferences for diabetes care and reasons for changing diabetes treatment teams, if applicable. Participants sought diabetes care providers who were knowledgeable, supportive and responsive, and worked within a multidisciplinary team. Participants reported a need for improved communication with providers, and those who had changed treatment teams reported discomfort with their providers attributable to a number of factors, including inadequate knowledge and insufficient interaction time. Many participants noted that provider communication could be improved, although three participants reported they would not change anything about their care.
Discussion
This pilot project aimed to provide support for young adults, while collecting information related to the needs/wants of this vulnerable group of emerging adults. Young adults with Type 1 diabetes met monthly for 5 months. Eighty per cent of participants attended at least three group sessions, with 53% attending at least four sessions.
We were able to assess the impact of group participation on diabetes-care variables using a pre–post design. Participation in the group was associated with a significant decrease in self-reported diabetes burden. Additionally, reported self-care behaviours increased after group participation. Participation in the group was also associated with a positive impact on HbA1c.
Participants wanted to discuss how others manage diabetes in day-to-day life, experiences and interactions experienced with others who do not have diabetes and emotions related to diabetes. Participants identified understanding their diabetes management plan, taking insulin and healthy eating as aspects of diabetes that were not as hard to cope with, while endorsing challenges with the unremitting demands of constant diabetes management, stresses related to coping with others with regard to diabetes care and general anxiety regarding diabetes. Participants identified that it is important for them to have a diabetes care team that is knowledgeable, supportive and multidisciplinary.
Despite the small number of participants in the current study, group participation was associated with a decrease in perceptions of diabetes-related burden and an increase in self-care behaviours. From these preliminary findings, emerging young adults appear to value the social support generated in group sessions. However, these patients self-selected participation in these groups. Thus, the true efficacy of group social support in young adults with Type 1 diabetes needs to be evaluated in a randomized, prospective manner. In addition, other avenues that provide support, such as social media, could be evaluated. Nonetheless, our preliminary studies are encouraging and support groups may be one way to facilitate optimal diabetes outcomes in this population. Other methods, such as a systems navigator approach, have also been effective in this respect [5]. Future research should focus on developing and testing groups like this to contribute to the effective care of this important population.
Acknowledgements
This work was supported in part by NIH Training Grant no. T32 DK007260, grants from the National Institute of Diabetes and Digestive and Kidney Diseases (DK-46887; 1K12DK094721), the Charles H. Hood Foundation, the Maria Griffin Drury Pediatric Fund and the Katherine Adler Astrove Youth Education Fund.
Footnotes
Competing interests Nothing to declare.
References
- 1.Harris MA, Freeman KA, Duke DC. Transitioning from pediatric to adult health care: dropping off the face of the earth. Am J Lifestyle Med. 2011;5:85–91. [Google Scholar]
- 2.Weissberg-Benchell J, Wolpert H, Anderson BJ. Transitioning from pediatric to adult care: a new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care. 2007;30:2441–2446. doi: 10.2337/dc07-1249. [DOI] [PubMed] [Google Scholar]
- 3.Cadario F, Prodam F, Bellone S, Trada M, Binotti M, Trada M, et al. Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: a hospital-based approach. Clin Endocrinol (Oxf) 2009;71:346–350. doi: 10.1111/j.1365-2265.2008.03467.x. [DOI] [PubMed] [Google Scholar]
- 4.Holmes-Walker DJ, Llewellyn AC, Farrell K. A transition care programme which improves diabetes control and reduces hospital admission rates in young adults with Type 1 diabetes aged 15–25 years. Diabet Med. 2007;24:764–769. doi: 10.1111/j.1464-5491.2007.02152.x. [DOI] [PubMed] [Google Scholar]
- 5.Van Walleghem N, Macdonald CA, Dean HJ. Evaluation of a systems navigator model for transition from pediatric to adult care for young adults with type 1 diabetes. Diabetes Care. 2008;31:1529–1530. doi: 10.2337/dc07-2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brumfield K, Lansbury G. Experiences of adolescents with cystic fibrosis during their transition from paediatric to adult health care: a qualitative study of young Australian adults. Disabil Rehabil. 2004;26:223–234. doi: 10.1080/09638280310001644924. [DOI] [PubMed] [Google Scholar]
- 7.McDonagh JE, Southwood TR, Shaw KL. Unmet education and training needs of rheumatology health professionals in adolescent health and transitional care. Rheumatology (Oxford) 2004;43:737–743. doi: 10.1093/rheumatology/keh163. [DOI] [PubMed] [Google Scholar]
- 8.Telfair J, Ehiri JE, Loosier PS, Baskin ML. Transition to adult care for adolescents with sickle cell disease: results of a national survey. Int J Adolesc Med Health. 2004;16:47–64. doi: 10.1515/ijamh.2004.16.1.47. [DOI] [PubMed] [Google Scholar]
- 9.Stabile L, Rosser L, Porterfield KM, McCauley S, Levenson C, Haglund J, et al. Transfer versus transition: success in pediatric transplantation brings the welcome challenge of transition. Prog Transplant. 2005;15:363–370. doi: 10.1177/152692480501500408. [DOI] [PubMed] [Google Scholar]
- 10.Fleming E, Carter B, Gillibrand W. The transition of adolescents with diabetes from the children's health care service into the adult health care service: a review of the literature. J Clin Nurs. 2002;11:560–567. doi: 10.1046/j.1365-2702.2002.00639.x. [DOI] [PubMed] [Google Scholar]
- 11.Court JM, Cameron FJ, Berg-Kelly K, Swift PG. Diabetes in adolescence. Pediatr Diabetes. 2009;10:S185–S194. doi: 10.1111/j.1399-5448.2009.00586.x. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Pediatrics. American Academy of Family Physicians. American College of Physicians-American Society of Internal Medicine Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 13.Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM. Transition to adult health care for adolescents and young adults with chronic conditions: position paper of the Society for Adolescent Medicine. J Adolesc Health. 2003;33:309–311. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- 14.Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 15.Weinger K, Butler HA, Welch GW, La Greca AM. Measuring diabetes self-care: a psychometric analysis of the Self-Care Inventory-Revised with adults. Diabetes Care. 2005;28:1346–1352. doi: 10.2337/diacare.28.6.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olsson CA, Boyce MF, Toumbourou JW, Sawyer SM. The role of peer support in facilitating psychosocial adjustment to chronic illness in adolescence. Clin Child Psychol Psychiatry. 2005;10:78–87. [Google Scholar]
- 17.Coppa K, Boyle M. The role of self-help groups in chronic illness management: a qualitative study. Aust J Prim Health. 2003;9:68–74. [Google Scholar]