Introduction
Almost all persons experience grief when faced with a serious illness.1,2 The grief experienced by seriously ill patients often manifests as physical symptoms (insomnia, loss of appetite, etc.) and emotional, social, spiritual, cognitive, and behavioral changes through which a person attempts to resolve or adjust to the losses imposed by the serious illness. Depression, while common in seriously ill patients, is neither a normal nor a universal phenomenon.3 Depression is underdiagnosed in seriously ill patients, though the prevalence is high. In a recent meta-analysis4 which reviewed 70 studies with 10,071 individuals across 14 countries in oncological, hematological, and palliative care settings, the prevalence of Diagnostic and Statistical Manual of Mental Disorders (DSM)-defined major depression was 14.9% (range: 12/2%–17.7%); for DSM-defined minor depression, 19.2% (9.1%–31.9%); and for all types of depression, 20.7% (12.9%–29.8%). Persistent dysphoria, anhedonia, a sense of hopelessness, helplessness, worthlessness, and an active and persistent desire for an early death could be manifestations of depression2,3 in seriously ill patients. Depression, when present, significantly diminishes the quality of life of these patients and likely complicates the presentation and optimal palliation of other distressing symptoms such as pain and fatigue. Distinguishing between grief and depression in seriously ill patients is vitally important, as the treatments differ.3 Normal grief, an adaptive process, often responds well to counseling and ongoing support. In contrast, depression is a pathological state causing significant distress and needs to be treated with a combination of nonpharmacological and pharmacological modalities. If diagnosed and treated appropriately, depression can be palliated effectively in seriously ill patients.5
Differentiating grief from depression in seriously ill patients
Differentiating between grief and depression2,3 is especially challenging in a seriously ill patient population due to the following reasons: (1) grief and depression share common symptoms and may coexist; (2) many of the somatic symptoms traditionally used to diagnose depression (appetite, weight and libido changes, loss of energy, insomnia) may be present as a part of the serious illness process or due to grief; (3) the affective changes used to identify depression (sadness, crying) are also seen in grief; (4) there is a common misperception that depression is a universal and normal phenomenon in a seriously ill population. Thus clinicians may fail to routinely screen these patients for clinical depression. Therefore there is a great need for a robust instrument that will aid in measuring grief and distinguish it from depression in a seriously ill population.
Existing measurement scales
Many of the existing survey instruments designed to detect depression are unsuitable for seriously ill patients, as questions addressing somatic, affective, and functional criteria often generate false positives. For example, the Hamilton Scale6 for depression identifies decreased social activities and the feeling of sadness, and the Center for Epidemiologic Studies Depression Scale (CES-D)7 screens for poor appetite and sleep disturbances. Two screening instruments that have been studied in a seriously ill population are the Hospital Anxiety and Depression Scale (HADS)8 and the Edinburgh Postnatal Depression Scale (EPDS).9 The HADS,8–10 which has anhedonia as its major construct, consists of anxiety and depression subscales. The HADS, when used to identify depression in a palliative population, had a sensitivity of 68% and specificity of 67% compared to the established, widely accepted, and structured Present State Examination interview9 at a combined (anxiety and depression subscales) cutoff of 19 (the depression subscale was not effective by itself). The EPDS was thought to be a useful screening instrument for palliative care patients,7 but neither the HADS nor the EPDS measure the patient's grief or seek to differentiate it from depression.
Methods
An effective scale tailored to differentiate between grief and depression in a palliative care patient population should
• allow self-rating, without requiring extensive observation of the patient
• be easy to use and should be composed of a small number of items
• be considered relevant by multidisciplinary palliative care clinicians and standardized on the basis of empirical research with palliative care patients over time
Theoretical model underlying the Palliative Grief Depression Scale
The cognitive signs10 helpful in identifying depression include persistent dysphoria, hopelessness, worthlessness, helplessness, anhedonia, and ruminating thoughts of death or suicide. For reasons described earlier, we sought to utilize these to structure the depression items of the PGDS.
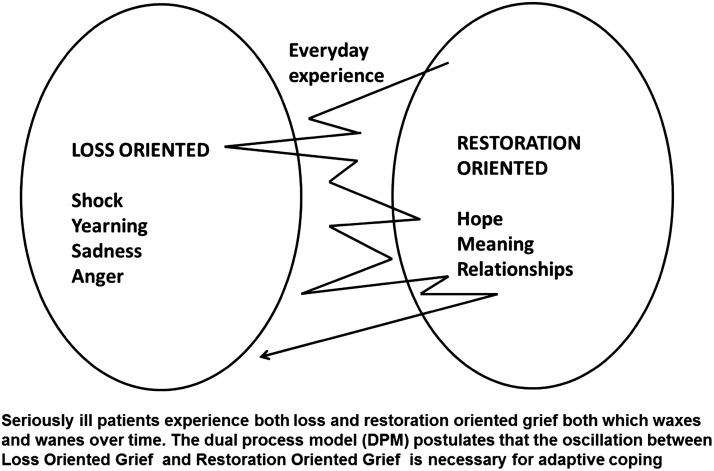
The Grief domain of the PGDS utilized the dual-process model. Seriously ill patients experience both loss and restoration oriented grief both which waxes and wanes over time. The dual process model (DPM) postulates that the oscillation between Loss-Oriented-Grief and Restoration-Oriented-Grief is necessary for adaptive coping.
The dual-process model (DPM)12 postulates that the grieving subject experiences a number of stressors that can be broadly classified into loss-oriented or restoration-oriented stressors. Stroebe12 explains that loss orientation refers to the grieving person's focus on the loss experience per se and restoration orientation refers to the focus on secondary stressors that are consequences of the loss. The DPM conceptualizes grief as a dynamic process with the grieving person alternating between loss-orientation and restoration-orientation. The DPM was identified to be an appropriate framework for the grief manifested by seriously ill patients. Using the DPM, the seriously ill patient's grief can be broadly classified as follows.
Loss-Oriented Grief (LOG) refers to the patient's focus and processing of the experience of loss due to serious illness. When patients recognize that they have a serious and life-limiting illness and that they may die as a result of the illness's progression, they experience a wide array of emotions including numbness, shock, anger, separation anxiety, sadness, and despair as a direct response to the loss. These can be thought of as primary stressors and are directly due to the patient's focus on and processing of some aspects of the perceived losses due to the serious illness.
Restoration-Oriented Grief (ROG) refers to the focus on the secondary stressors that are also consequences of the loss. As seriously ill patients process the implications of their current losses and anticipated future losses, and as they struggle to reconcile with their situation, the focus of their hopes often shifts. A hope for cure may shift to hope for excellent symptom management and quality of life for the rest of their life span. They often try to find meaning in and amidst their illness process. They may reexamine and strengthen existing relationships and/or form new relationships, thereby restructuring their lives to establish a new equilibrium that integrates the serious illness. These processes, intrinsically stressful, may help patients cope functionally with their illness. According to the DPM,12 the grieving person will alternate between LOG and ROG with occasional timeouts when grieving is left alone. The DPM postulates that the oscillation between LOG and ROG is necessary for adaptive coping, as depicted in Figure 1.
FIG. 1.
Dual process model of grief in seriously ill patients.
In our previous work,3 we have described the creation of the Terminally Ill Grief or Depression Scale (TIGDS), a 42 item scale, which was successfully validated in a hospice population. Briefly, an initial 100 item inventory consisting of true/false items was assembled based on extensive literature review, interviews with multi-disciplinary clinicians and seriously ill patients. It was then shortened systematically to create the psychometrically robust 42 item TIGDS. The TIGDS was administered to hospice in-patients along with the Hospital Anxiety Depression Scale (HADS). When compared to the HADS total score, the TIGDS depression subscale showed strong convergent validity and the TIGDS grief subscale showed strong discriminant validity. The TIGDS comprised of 17 Restoration Oriented Grief items, 13 Loss Oriented Grief items and 12 Depression items. While the TIGDS is a psychometrically robust scale (sensitivity of 0.727 and specificity of 0.886), it has not been validated in an out-patient setting with palliative care patients who are upstream in the trajectory of their illness. Also, the TIGDS consisted of 42 items which took about 10 minutes to administer which might be too long for many seriously ill patients. Thus, we aimed to create a shorter 20 item scale, namely the Palliative Grief Depression Scale (PGDS), which could be administered rapidly. Accordingly, we chose the 5 ROG, 5 LOG, and 10 depression subscale items with the highest item-test correlations from the 42-item TIGDS to create the PGDS. The PGDS thus consists of 20 true-false items, the score on each subscale being the number of items that are true (see Table 1. for scores and ranges and the Appendix for the PGDS items):
Table 1.
Mean Scores on the PGDS Subscales
| Variable (%) | Mean (%) | SD | Range (%) | |
|---|---|---|---|---|
| PGDS-G, grief subscale scores | ROG | 71.0 | 30.8 | 0–100 |
| LOG | 36.0 | 32.4 | 0–100 | |
| Total grief, ROG+LOG | 107.1 | 43.4 | 0–200 | |
| ROG–LOG | 35.0 | 30.8 | -100–100 | |
| PGDS-D, depression subscale scores | 13.5 | 18.5 | 0–87.5 | |
LOG, Loss-Oriented Grief; PGDS-D, Palliative Grief Depression Scale, Depression; ROG, Restoration-Oriented Grief; SD, standard deviation.
Depression subscale PGDS-D: Ten items (maximum score=10)
Grief subscales PGDS-G: Ten items divided into two parts:
LOG: Five items (maximum score=5)
ROG: Five items (maximum score=5)
Validation of the PGDS
Next, we tested the PGDS in an outpatient palliative care clinic setting in a cohort of 106 seriously ill patients. Note that the grief described in this paper is the seriously ill patient's preparatory grief while processing a limited life span and the implications of the serious illness on his or her life. This type of grief may be somewhat different from the grief of bereavement (the grief experienced by the survivors due to anticipated death or after the death of a loved one), which has been extensively studied and described in the literature.
The new cohort of 106 adult patients with a variety of serious illnesses (both cancer and noncancer diagnoses) were referred to the palliative care clinic over a four-year period from a large tertiary care Veterans Affairs (VA) facility. Patients referred to the clinic were eligible to participate in the study, aside from those with a documented diagnosis of dementia or those deemed by their physician or charge nurse to be unable to participate due to acute distress from situations such as severe pain, dyspnea, or having an altered consciousness.
A trained research assistant approached the patients, obtained informed consent, and then administered the 20-item PGDS and the HADS every time the patient was seen in the palliative care clinic (a maximum of 10 times) or until he or she was discharged from the clinic (typically to home hospice or inpatient hospice). We sought to mimic a real-world setting and thus administered the instruments each time the patient came to clinic instead of at predetermined regular time intervals. The frequency of clinic visits was determined by the palliative care physician based on the patient's needs. Many patients chose to read and respond to the survey by themselves, and a trained research assistant was available to assist patients when they asked for help. Ten of the 106 patients were unable to complete all the survey items even once, due to extreme fatigue, and they were excluded from the dataset. A total of 96 patients completed all items in both scales once, and 32 patients were able to complete both instruments at least three times. The distribution of the number of tests per subject was 1:47, 2:17, 3:15, 4:5, 5:6, 6:1, 8:1, and 10:4 (note that the number of subjects add up to 96). Of the 96 patients, 94 were male and 2 were female; their mean age was 70.6 years, standard deviation (SD)=13.0, range=43–94. A total of 47 patients had cancer diagnoses and the cancer cohort was younger than the noncancer cohort (e.g., end-stage heart disease, lung disease, amyotrophic lateral sclerosis (ALS); mean age 67.0 years, SD=11.5, range=43–94). A total of 49 patients had various noncancer serious illnesses and this cohort was older (mean age=74.0 years, SD 13.5, range=45–94). (See Table 1.)
Results
Test-retest reliability of the PGDS
The Intra-class Correlation Coefficient (ICC) 13,14 was calculated to estimate the test-retest reliability for the 32 patients who had completed the questionnaire three times. The ICCs were calculated for each patient: the LOG score, ROG score, depression score (D), sum of grief scores (ROG+LOG), and difference between grief scores (ROG–LOG). The ICCs were quite high indicating that the PGDS is reliable in our seriously ill outpatient population (see Table 2).
Table 2.
PGDS ICC of 1st, 2nd, and 3rd Test for N=32 Patients Who Completed the PGDS Three Times or More during the Study Period, with 95% Confidence Intervals
| Subscale scores (%) | ICC | Lower bound | Upper bound |
|---|---|---|---|
| ROG | 0.80 | 0.67 | 0.89 |
| LOG | 0.80 | 0.67 | 0.89 |
| PGDS-D | 0.62 | 0.43 | 0.77 |
| ROG+LOG | 0.81 | 0.69 | 0.89 |
| ROG–LOG | 0.79 | 0.66 | 0.88 |
CI, Confidence Intervals; ICC, Intraclass Correlation Coefficient; LOG, Loss-Oriented Grief; PGDS, Palliative Grief Depression Scale; PGDS-D, Palliative Grief Depression Scale, depression; ROG, Restoration-Oriented Grief.
Validity of the PGDS
Comparing the PGDS scores with the HADS scores tested convergent validity. The depression subscale of the PGDS showed a moderate correlation (Spearman correlation, r=0.33; p<.0.0010) with the HADS total score (total HADS score ≥19 was considered to be depression). More importantly, the PGDS total grief score (ROG+LOG) had lower correlation (Spearman correlation, r=0.22; p=0.0317) with the HADS total score, suggesting that the PGDS grief subscales were measuring different constructs.
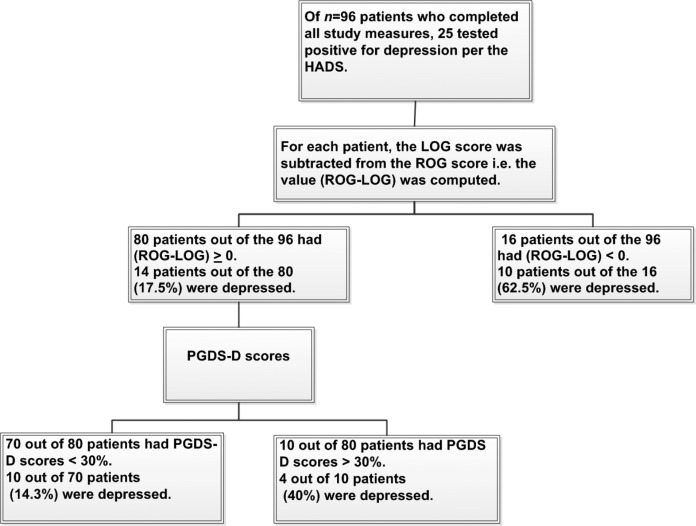
Receiver operating characteristic curve analysis15 to set criteria
The validity of the 20-item PGDS was assessed using a receiver operating characteristic (ROC) curve analysis, comparing the first test for the 96 subjects with the HADS total scores, using a HADS total ≥19 as the gold standard diagnostic of depression, with the predictor variables as listed in Table 1. The ROC procedure examines each of the predictor variables and all possible cutpoints and combinations, and identifies the variable and its cutpoint with the optimal balance between sensitivity and specificity for identifying those particular patients with the specific outcome of interest (namely, clinical depression as indicated by a total HADS≥19). The total group is then divided into two subgroups—those above and below the selected cutpoint on the selected variable—and the process is reiterated until no further discrimination was achieved. The result is a decision tree15 as shown in Figure 2.
FIG. 2.
Receiver Operating Characteristic (ROC) Decision Tree. PGDS, Palliative Grief Depression Scale; ROG, Restoration Oriented Grief; LOG, Loss Oriented Grief; D, Depression. ROG-LOG score for each patient is obtained by subtracting the patient's Loss Oriented Grief score from the Restoration Oriented Grief score.
The first cutpoint identified by the ROC analysis, ROG–LOG at 0%, i.e., when ROG scores were equal to the LOG scores, was the best predictor16 of depression (kappa=0.38; chi square=14.4; p<0.001). Among the 80 patients with ROG+LOG≥0 percent, an additional predictor was PGDS-D at 30% (kappa=0.22; chi square=4.007; p<0.05). Of the 16 patients with ROG–LOG<0, 62.5% were depressed. Of the 10 patients with ROG–LOG≥0 and PGDS-D≥30 % (3 out of 10 items), 4 (40%) were depressed. Of the remaining 70 patients with ROG–LOG≥0% and PGDS-D<30%, only 10 (14%) of the patients were depressed. This indicates that if the PGDS ROG score is equal to or less than the LOG score, or three or more depression items are true out of 10 items in the PGDS-D subscale, the patient should be carefully evaluated for possible depression.
Discussion
We have developed and validated a short and psychometrically robust tool and refined a new questionnaire, the PGDS, to individually measure and differentiate between grief and depression in a palliative patient population. The PGDS was easy to administer and was acceptable as per our patient reports. Some patients even asked to complete the PGDS after the study period, as they felt that it helped them gain a better insight into their condition. Our data indicate that the PGDS may be a valid and reliable screening tool. Validity was tested by ROC analysis. Convergent validity of the PGDS was further tested against the HADS and found to be acceptable, and there was good discriminant validity between the HADS total scores and the LOG and ROG of the PGDS. This study is also noteworthy for the following reasons: first, to the best of our knowledge, the PGDS is the first scale to attempt to individually measure and distinguish between preparatory grief and depression in seriously ill patients; second, the scale items were originally tested and validated in a hospice population and now further tested in a palliative care clinic population; third, we measured the patients' grief and depression longitudinally over time in a real-world setting. The PGDS ICCs were high, indicating that the individual ROG, LOG, and D scores of each patient did not vary dramatically over time. We expect that the grief and depression scores likely change over longer periods of time depending on patient coping styles as well as the management of grief and depression. We believe that we need to study a large cohort of patients from the early stages of serious illness in a variety of venues before coming to conclusions about the patterns of grief and depression in these patients over time. It is possible that grief responses may be reflective of the patients' underlying coping styles with the serious illness, and this may or may not change over time.
This study is limited by the relatively small sample size and also because it was conducted in a single outpatient palliative care clinic in a VA with a largely male population.
In summary, our study offers valuable data that should be influential in guiding future advances in differentiating between grief and depression in palliative care patients. The PGDS is a valid and reliable screening tool that can be used to make this important clinical distinction. Note that no attempt was made in this study to identify the severity of patients' depression or preparatory grief, as this instrument is designed to distinguish between states of depression and grief. The scale is not time-intensive and can be used either as a self-report measure or can be administered by clinicians. Before general adoption of the PGDS we recommend trials in various clinical settings and on larger samples to test the generalizability of our results. It would also be desirable to track the changes in the patient responses to the grief and depression subscales in longitudinal studies as well as concurrently tracking variables such as quality of life and spiritual distress. Furthermore, it is crucial to ascertain whether discrimination of grief from depression is of any clinical utility. One approach to further study the PGDS might be a randomized clinical trial in which the information from the PGDS is provided to the clinicians caring for them for a randomly selected half of the patients, and used to facilitate clinical decision making, the results to be compared to the other randomly selected half who undergo usual care. Differential treatment responses could be measured by determining the impact of focused interventions on key patient centered outcomes such as depression and quality of life.
Conclusion
The PGDS is a promising tool that may help measure grief and depression in seriously ill adult patients over time, through the trajectory of serious illness. We hope that such differentiation will lead to appropriate management strategies for grief and depression, thereby augmenting the quality of life of seriously ill patients and their families.
Appendix: The Palliative Grief Depression Scale with Scores and Interpretation
The PGDS scale is a brief scale that can be used as a self-report measure or can be administered by the clinician or the patient's family member. It is comprised of 20 true-false items with each true response yielding one point and false response yielding zero points. On completion, the PGDS will yield three raw subscale scores: PGDS-ROG, PGDS-LOG, and PGDS-D. Next, compute the total grief scores (ROG+LOG) and the difference in grief scores (ROG–LOG). Please note that the psychometric properties of the PGDS are preserved and the results are valid only if the items are administered in the order below (i.e., the grief and depression items are all interspersed in the questionnaire).
Scoring and interpretation of PGDS scores:
• LOG is scored positively with one point per true answer and zero points for a false answer and a score range=0 to 5.
• ROG is also scored positively with one point per true answer and zero points for a false answer and a score range=0 to 5.
• Depression is scored positively with one point per true answer and zero points for a false answer and a score range=0 to 10.
PGDS scores and implication on depression:
• If (ROG–LOG)<0, patient is likely depressed.
• If (ROG – LOG)≥0, and D score<3, patient is likely not depressed.
• If (ROG – LOG)>0 and D score>= 3, patient may be depressed.
PGDS total grief scores and implication on grief:
If ROG+LOG is low, the total grief currently experienced by the patient is low. Please note that grief varies with time and so it would be important to continue to track the patient's grief as he or she progresses through the illness. If ROG+LOG is high, this indicates increased grief and the patient needs to be supported appropriately.
Appendix PGDS Used to Measure the Seriously Ill Patient's Loss-Oriented Grief, Restoration-Oriented Grief, Total Grief, and Depression Scores
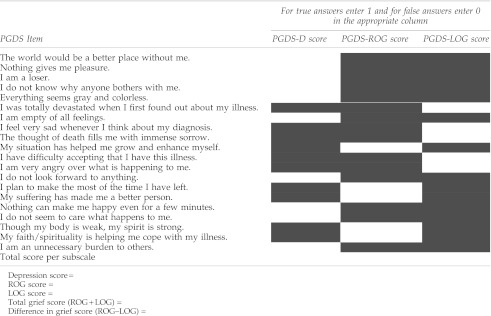 |
Acknowledgments
This work is supported in part by grants RCA 115562A and IR25 MD006857-01 from the National Institutes of Health to Dr. Periyakoil, the Sierra Pacific MIRECC, VA Palo Alto Health Care System and the Department of Veterans Affairs.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Kubler-Ross E. On Death and Dying. New York: Simon & Schuster; 1997. [Google Scholar]
- 2.Periyakoil VS. Hallenbeck J. Identifying and managing preparatory grief and depression at the end of life. Am Fam Physician. 2002;65(5):883–890. [PubMed] [Google Scholar]
- 3.Periyakoil VS. Kraemer HC. Noda A, et al. The development and initial validation of the Terminally Ill Grief or Depression Scale (TIGDS) Int J Methods Psychiatr Res. 2005;14(4):202–212. doi: 10.1002/mpr.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell AJ. Chan M. Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 5.Rayner L. Price A. Evans A, et al. Antidepressants for the treatment of depression in palliative care: Systematic review and meta-analysis. Palliat Med. 2011;25(1):36–51. doi: 10.1177/0269216310380764. [DOI] [PubMed] [Google Scholar]
- 6.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 8.Lloyd-Williams M. An analysis of the validity of the Hospital Anxiety and Depression Scale as a screening tool in patients with advanced metastatic cancer. J Pain Symptom Manage. 2001;22(6):990–996. doi: 10.1016/s0885-3924(01)00358-x. [DOI] [PubMed] [Google Scholar]
- 9.Lloyd-Williams M. Criterion validation of the Edinburgh Postnatal Depression Scale as a screening tool for depression in patients with advanced metastatic cancer. J Pain Symptom Manage. 2000;20(4):259–265. doi: 10.1016/s0885-3924(00)00182-2. [DOI] [PubMed] [Google Scholar]
- 10.Zigmond AS. Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 11.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Arlington, VA: APA; 2000. Text Revision (DSM-IV-TR) [Google Scholar]
- 12.Stroebe MS. Schut H. Models of coping, bereavement: A review. In: Stroebe MS, editor; Hansson RO, editor; Stroebe W, editor; Schut H, editor. Handbook of Bereavement Research. Washington, DC: American Psychological Association; 2001. [Google Scholar]
- 13.Bartko JJ. The intraclass correlation coefficient as a measure of reliability. Psychol Reports. 1996;19:3–11. doi: 10.2466/pr0.1966.19.1.3. [DOI] [PubMed] [Google Scholar]
- 14.McGraw KO. Wong SP. Forming inferences about some intraclass correlations. Psychol Methods. 1996;1:30–46. [Google Scholar]
- 15.Kraemer HC. Evaluating Medical Tests: Objective and Quantitative Guidelines. Newbury Park, GA: Sage; 1992. pp. 76–85. [Google Scholar]
- 16.Kraemer HC. Periyakoil VS. Noda A. Kappa coefficients in medical research. Stat Med. 2002;30(14):2109–2129. doi: 10.1002/sim.1180. [DOI] [PubMed] [Google Scholar]