Abstract
Background:
The purpose of this study was to systematically examine the impact of insurance status on access to and utilization of elective specialty hand surgical care. We hypothesized that patients with Medicaid insurance or those without insurance would have greater difficulty accessing care both in obtaining local surgical care and in reaching a tertiary center for appointments.
Methods:
This retrospective cohort study included all new patients with orthopaedic hand problems (n = 3988) at a tertiary center in a twelve-month period. Patient insurance status was categorized and clinical complexity was quantified on an ordinal scale. The relationships of insurance status, clinical complexity, and distance traveled to appointments were quantified by means of statistical analysis. An assessment of barriers to accessing care stratified with regard to insurance status was completed through a survey of primary care physicians and an analysis of both patient arrival rates and operative rates at our tertiary center.
Results:
Increasing clinical complexity significantly correlated (p < 0.001) with increasing driving distance to the appointment. Patients with Medicaid insurance were significantly less likely (p < 0.001) to present with problems of simple clinical complexity than patients with Medicare and those with private insurance. Primary care physicians reported that 62% of local surgeons accepted patients with Medicaid insurance and 100% of local surgeons accepted patients with private insurance. Forty-four percent of these primary care physicians reported that, if patients who were underinsured (i.e., patients with Medicaid insurance or no insurance) had been refused by community surgeons, they were unable to drive to our tertiary center because of limited personal resources. Patients with Medicaid insurance (26%) were significantly more likely (p < 0.001) to fail to arrive for appointments than patients with private insurance (11%), with no-show rates increasing with the greater distance required to reach the tertiary center.
Conclusions:
Economically disadvantaged patients face barriers to accessing specialty surgical care. Among patients with Medicaid coverage or no insurance, local surgical care is less likely to be offered and yet personal resources may limit a patient’s ability to reach distant centers for non-emergency care.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
The impact of insurance status on patient access to medical care is a regular subject in the popular press, with predictions of decreased access if Medicare and Medicaid reimbursement is reduced. The associated topic of patient transfers to tertiary care trauma centers has been a recent subject of interest in the medical literature1-4, with reports of inappropriate transfer of patients who were uninsured or enrolled in Medicaid in the absence of an association between transfer and injury severity1,2. These studies have suggested that the reluctance of community hospitals to care for patients who are underinsured (i.e., patients with Medicaid insurance or no insurance) leads to patient transfers and an inappropriate utilization of health-care resources.
Similar concerns with regard to access to specialty care have been raised in one examination of outpatient care at a tertiary orthopaedic center5. Weiner et al.5 examined the impact of insurance status on patients’ need to travel to a tertiary center for orthopaedic spine care. The authors reported that, for patients who were seen from 2003 to 2006, those who had Medicaid insurance traveled fifty-one miles for appointments compared with those who had private insurance and had spine problems, who traveled fourteen miles for appointments5.
The purpose of this study was to systematically examine the impact of insurance status on the provision of specialty hand surgical care. Our first aim was to quantify the impact of insurance status on outpatient evaluations at a tertiary hand center. We hypothesized that patients who were underinsured would account for a disproportionate percentage of patients seen at a tertiary care center with an open scheduling policy and no restrictions based on insurance. Our second aim was to critically assess the impact of insurance status on hand surgical care access. This assessment included quantifying appointment arrival rates and rates of surgical and nonoperative management and investigating the experience of primary care physicians when attempting to obtain hand surgical care for their patients according to patient insurance status. We hypothesized that patients with Medicaid insurance and those without insurance coverage would face greater challenges accessing care than those with private insurance.
Materials and Methods
We obtained institutional review board approval and performed a retrospective cohort study evaluating a convenience sample of all new patient office visits from August 18, 2008, to August 19, 2009, to hand surgeons within the Washington University Department of Orthopaedic Surgery. A total of 3988 patients were identified through a search of the computerized departmental billing database utilizing evaluation-and-management codes representing all levels of new office visits or new consultations.
Our division of hand surgery has no restrictions on appointment scheduling for patients with Medicaid insurance. In the present study, patient insurance status was coded into six categories: 1 was defined as uninsured; 2, as Medicaid; 3, as Medicare; 4, as private coverage; 5, as Workers’ Compensation; and 6, as TRICARE (uniformed service coverage). Private coverage included commercial insurance, managed care organization coverage, and trade union insurance. The distances traveled for individual office visits were determined through use of a web-based calculation from each patient’s home zip code to the office zip code. Of 3988 new patient visits, 3699 encounters were included for final analysis (Fig. 1). By means of a manual chart review, we determined that only eleven patients actually traveled >250 miles from their home address to our clinic. Each of these eleven patients was formally referred from hand surgeons for second or third opinions and traveled a mean distance (and standard deviation) of 361 ± 79 miles. As these eleven patients were not reflective of the patient group that was required to travel long distances to access specialty care, the analysis excluded patients traveling >250 miles.
Fig. 1.
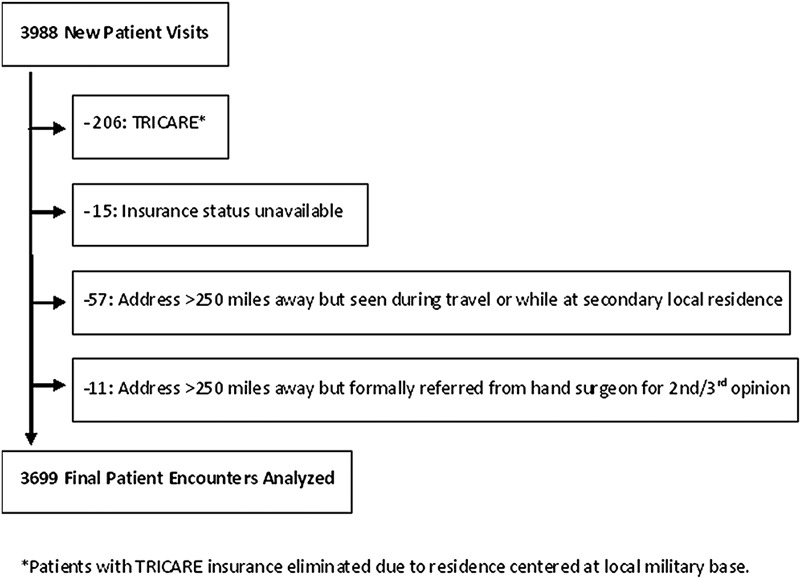
Flow diagram showing patient encounters included in data analysis.
Determining the Impact of Insurance on the Utilization of a Tertiary Center
Two members of the research team (C.M.S. and C.D.C.) independently reviewed the electronic medical records to document the presenting diagnosis at our tertiary center. When appropriate, qualifying statements were also recorded with regard to additional factors related to the patient conditions that could either impact or illuminate the complexity of the patient symptom. An attending surgeon (R.P.C.) reviewed ten charts that had previously been reviewed by each researcher as a quality control. Additionally, following the completion of the record review, one attending surgeon (R.P.C.) reviewed fifty randomly selected charts to ensure accuracy. Manual chart review was performed as it offered more detailed and potentially more accurate data regarding diagnoses and treatment considerations for each patient in comparison with a billing claims database with ICD-9 (International Classification of Diseases, Ninth Revision) or evaluation-and-management codes for the level of visit.
Two attending surgeons (R.P.C. and C.A.G.) mutually agreed on an ordinal rating system for clinical complexity: 1 was defined as simple; 2, as moderate; 3, as complex; and 4, as most complex. Anticipated common diagnoses were categorized according to the expected diagnostic and treatment complexity on the basis of the clinical experience of those surgeons (Table I). To rate clinical complexity, each attending surgeon then independently reviewed an electronic file of diagnoses and qualifying statements that had been derived from the chart reviews and had included all subjects. The qualifying statement review allowed in-depth complexity assessment to increasingly differentiate patients, such as one with a classic presentation of carpal tunnel syndrome compared with one with the same final diagnosis but atypical arm pain and comorbid cervical spine disease. The reviewers (R.P.C. and C.A.G.) were blinded to the patient insurance status and the distance traveled to the appointment. The final complexity rating for each patient was determined by a consensus of the two reviewers (R.P.C. and C.A.G.) in cases of discordant ratings.
TABLE I.
Condensed Rating System for Clinical Complexity
| 1. Simple |
| Carpal tunnel syndrome |
| Laceration without the tendon, nerve, or artery involved |
| Trigger finger |
| de Quervain tendinitis |
| Sprains |
| Soft-tissue mallet finger |
| Cellulitis |
| 2. Moderate |
| Osteoarthritis in the digit, carpometacarpal joint |
| Extra-articular fracture in the hand or wrist (excluding carpal fractures) |
| Cubital tunnel syndrome |
| Pain: unclear diagnosis, no further referral needed |
| Amputated finger |
| Carpal boss |
| Ganglion cysts |
| Simple digit dislocations |
| Osseous mallet |
| Extensor tendon laceration |
| 3. Complex |
| Intra-articular fractures in the hand or wrist |
| Carpal fracture |
| Pain: no diagnosis but needs further referral to another specialist |
| Complicated presentation of simple problems |
| Congenital deformity |
| Carpal or distal radioulnar joint instability |
| Dupuytren |
| Arthritic degeneration in the wrist, distal radioulnar joint |
| Open fracture in the hand or wrist |
| Tendon rupture |
| Amputations needing revision |
| Flexor tendon laceration outside of zone 2 |
| 4. Most complex |
| Nonunions in the hand or wrist |
| Presenting for revision surgery with primary surgery done elsewhere |
| Flexor tendon laceration zone 2 |
| Carpal fusion or limited fusions for scaphoid nonunion advanced collapse or scapholunate advanced collapse |
We obtained data regarding the Missouri Medicaid enrollment in the county of residence for each of the sixty-five patients who traveled 151 to 250 miles to reach our office6. Pediatric and adult patient Medicaid enrollment data were utilized in combination with age-stratified county populations based on 2008 United States census records7. These county-level data allowed us to assess the percentage of patients with Medicaid coverage who presented from each county relative to the percentage of patients with Medicaid coverage in that county. We only performed this analysis on those patients traveling the greatest distance as this group was expected to maximize discrepant travel by patients with Medicaid coverage who were unable to obtain community hand surgical care. County-level estimates for patients who were uninsured were not available, so similar calculations were not possible for these patients.
This investigation was performed during a year in Missouri when procedural reimbursement percentages of surgeon charges among all insurances was the lowest for Medicaid (15%), with increasing collection rates for Medicare (18%), private insurance (38%), and Workers’ Compensation (50%). The reimbursement for office evaluations followed a similar pattern with regard to collection rates: Medicaid (47%), Medicare (57%), private insurance (77%), and Workers’ Compensation (81%).
Determining the Impact of Insurance Status on Access to Hand Surgical Care
Access to hand surgical care was assessed through the use of three independent measures. One hundred primary care physicians with offices ≥100 miles from our center who were identified as care providers for patients presenting to our offices were queried via e-mail with a web-based electronic survey regarding locally available hand surgical care and the impact of patient insurance status on referrals to community surgeons (see Appendix). Missed appointments were examined at our center over the twelve-month study period to determine patient arrival rates as a function of insurance status. Finally, operative rates for three of the most common presenting diagnoses, including distal radial fracture, carpal tunnel syndrome, and trigger finger, were examined to compare the provision of operative care with the patients reaching the tertiary center according to insurance status.
Statistical Analysis
Descriptive statistics and frequency tables were produced to characterize the study cohort (age, insurance status, distance traveled, and clinical complexity).
The agreement between the two raters of clinical complexity (R.P.C. and C.A.G.) was assessed with use of the weighted Cohen kappa coefficient. The instances in which ratings by the two reviewers (R.P.C. and C.A.G.) differed by >1 point were subsequently confirmed to result from the differential interpretation of diagnostic qualifying statements compared with misclassified data.
The relationship of the patient insurance status and clinical complexity with the distance traveled (as a continuous variable) to appointments was tested with use of analysis of variance (ANOVA) and the Tukey post hoc evaluation of homogenous subsets. The distribution of insurance categories and clinical complexities across distance categories was evaluated with use of chi-square testing. The smallest distance category was fifty miles or less, with subsequent categorization by fifty or 100-mile increments as required to eliminate sparse data cells. The distribution of clinical complexity ratings by insurance status was compared with use of chi-square analysis.
The Fisher exact test of proportions was utilized to statistically evaluate the expected percentage compared with the observed percentage of the Missouri Medicaid referrals, assuming a random referral pattern from the geographical areas that were 151 to 250 miles from our center.
The impact of travel distance on no-show and appointment cancellation rates was determined with use of Student t test and chi-square testing. To ensure comparable travel conditions when assessing arrival rates according to insurance status, we compared appointments from the same home zip code among all patients who had Medicaid coverage and 2384 patients who had private insurance.
With use of the chi-square test, operative rates for common diagnoses were compared for the group of patients with Medicaid coverage and those with no insurance with the group of patients with Medicare and those with private insurance. The percentages of patients with diagnoses of distal radial fracture, carpal tunnel syndrome, or trigger finger were directly adjusted to allow a similar distribution of these diagnoses between the two patient groups.
Source of Funding
The project described was supported by award number UL1RR024992 from the National Center for Research Resources (<$10,000 in one year). The funds were used for general research support and supplies.
Results
The most common insurance status for this cohort of patients was that of private insurance (69.2%), with patients who had Medicaid coverage or were uninsured accounting for 17.2% of visits. Table II details the descriptive statistics of the study cohort analyzed.
TABLE II.
Descriptive Statistics of the Study Cohort Analyzed
| Statistic | No. of Patients (%) |
| Insurance status | |
| Private | 2561 (69.2) |
| Medicaid | 407 (11.0) |
| Medicare | 357 (9.7) |
| Uninsured | 228 (6.2) |
| Workers’ Compensation | 146 (3.9) |
| Distance traveled | |
| Zero to fifty miles | 3175 (85.8) |
| Fifty-one to 100 miles | 275 (7.4) |
| 101 to 150 miles | 151 (4.1) |
| 151 to 200 miles | 68 (1.8) |
| 201 to 250 miles | 30 (0.8) |
| Age | |
| Less than eighteen years | 488 (13.2) |
| Eighteen years or older | 3211 (86.8) |
| Clinical complexity | |
| Simple | 1023 (27.7) |
| Moderate | 1447 (39.1) |
| Complex | 972 (26.3) |
| Most complex | 257 (6.9) |
The independent ratings of clinical complexity demonstrated substantial agreement between the two raters (R.P.C. and C.A.G.). The weighted kappa value for interrater agreement was 0.82 (95% confidence interval [95% CI], 0.80 to 0.83). Independent scores by the two raters (R.P.C. and C.A.G.) differed by >1 point on only forty-two out of 3699 ratings (1.1%).
Utilization of the Tertiary Center: Distance Traveled
The mean distance traveled by patients varied significantly (p < 0.001) according to patient insurance status. The mean distance (and standard deviation) of miles traveled was greater for patients with Medicaid insurance (39 ± 51 miles) and Workers’ Compensation (43 ± 47 miles) when compared with that for patients with Medicare (22 ± 35 miles), those with private insurance (27 ± 36 miles), and those with no insurance (23 ± 38 miles). As Figure 2 depicts, as the distances of required travel increased, the percentage of patients with Medicaid insurance steadily increased (p < 0.001): less than fifty miles (10%), fifty-one to 150 miles (18%), and 151 to 250 miles (26%).
Fig. 2.
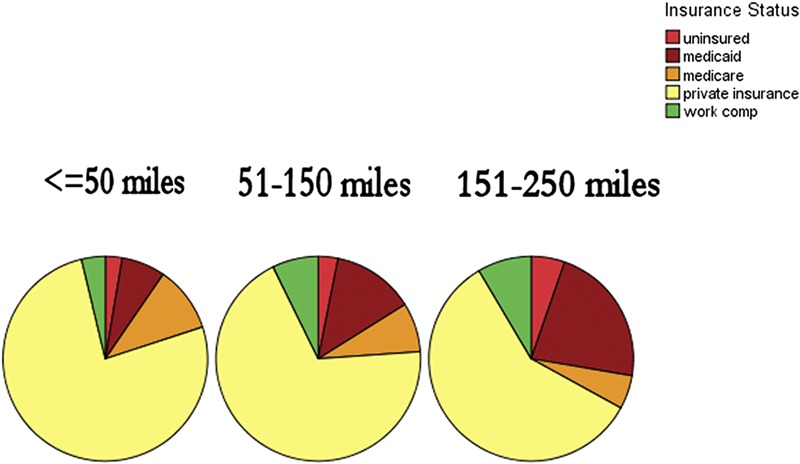
Pie charts showing insurance status among patients from different distance categories.
Utilization of Tertiary Center: Clinical Complexity
With increasing clinical complexity, the mean patient driving distance to the appointment significantly increased (p < 0.001), independent of patient insurance status. As demonstrated in Figure 3, as the distance traveled increased, the percentage of simple conditions decreased and the percentage that had been rated complex to most complex became significantly more prevalent (p < 0.001). For example, with each additional fifty miles traveled, the percentage of patients with simple-level complexity decreased (29%, 21%, 14%, 13%, and 7%) and the percentage of patients with the most complex presentations generally increased (6%, 11%, 17%, 24%, and 20%). The distribution of clinical complexity ratings for patients with no insurance and those with Medicaid insurance were at least as complex as other new patients (Fig. 4). The percentage of patients with Medicaid insurance presenting with simple-level complexity (20% [n = 80]) was significantly less (p < 0.001) than that of patients with Medicare (30% [n = 107]) and those with private insurance (30% [n = 768]). Ten percent of patients with Medicaid insurance (n = 40) were rated as most complex compared with 9% of patients with Medicare insurance (n = 31) and 6% of patients with private insurance (n = 146).
Fig. 3.
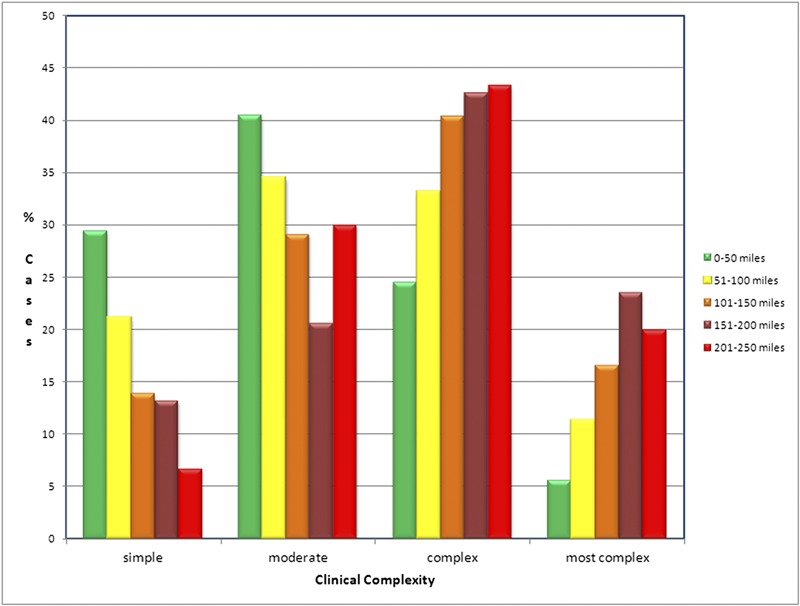
Bar graph showing the percentage of clinical complexity ratings within each distance category.
Fig. 4.
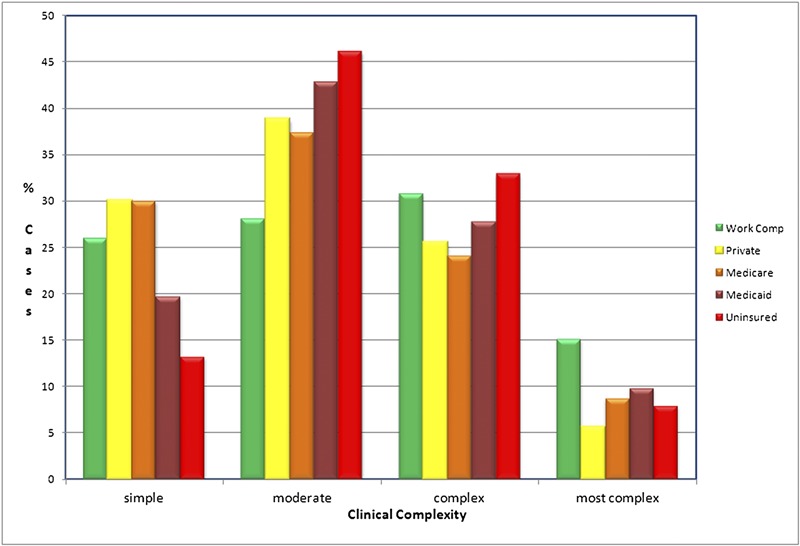
Bar graph showing the distribution of clinical complexity ratings according to insurance status.
Subgroup Analyses
Among the sixty-five Missouri residents driving 151 to 250 miles to the appointment, the expected percentage of Medicaid referrals was 24.4% as a function of Medicaid enrollment in each county. When adjusted for the disparate rates of Medicaid among the pediatric and adult populations of each county, a sample with the age distribution seen by our practice would be expected to have 27.8% Medicaid enrollment. The actual percentage of patients with Medicaid insurance among those presenting from that distance (30.8% [twenty of sixty-five patients]) was not significantly different from the expected rate (p = 0.85).
We found a greater percentage of patients with Medicaid insurance among children (25.4% [124 of 488 patients]) compared with adults (8.8% [283 of 3211 patients]). The distance traveled increased with greater clinical complexity for both children and adults (p ≤ 0.001). Similar to adult patients, pediatric patients with Medicaid traveled the greatest mean distances (and standard deviations) to appointments (51.1 ± 63 miles) compared with pediatric patients with other insurance, for example, private insurance (25 ± 33 miles). Pediatric and adult patients with Medicaid insurance from those counties that were 151 to 250 miles from our offices had similar expected and actual percentages (p = 1.0); pediatric patients had 51.4% expected and 56.5% actual percentages and adult patients had 14.6% expected and 17.9% actual percentages.
Access to Hand Surgical Care
Twenty-six primary care physicians (26%) of the 100 physicians e-mailed responded to our survey. Fifty-seven percent of respondents reported that two to four surgeons in their community would see patients with hand problems. Ten percent of respondents reported that their communities had no local access to hand surgical care. Fifty-nine percent of respondents reported that patient insurance status impacted referrals for local hand surgical care. Patient insurance was reported to affect waiting times before appointments, to result in resistance to scheduling, and, in some instances, to prevent appointments entirely. According to primary care provider respondents, community specialists varied in their acceptance of patients (Fig. 5). Forty-six percent of primary care physicians reported that patients with no insurance and those with Medicaid insurance were forced to drive longer distances to access hand surgical care because local surgeons would not accept them. Coupled with this challenge to accessing care, 56% of physicians believed that these patients who were underinsured were more likely to live with their problems compared with patients with private insurance. Forty-four percent of the primary care physicians reported that, if refused by community surgeons, patients who were uninsured would be unable to drive to our tertiary center because of limited personal resources.
Fig. 5.
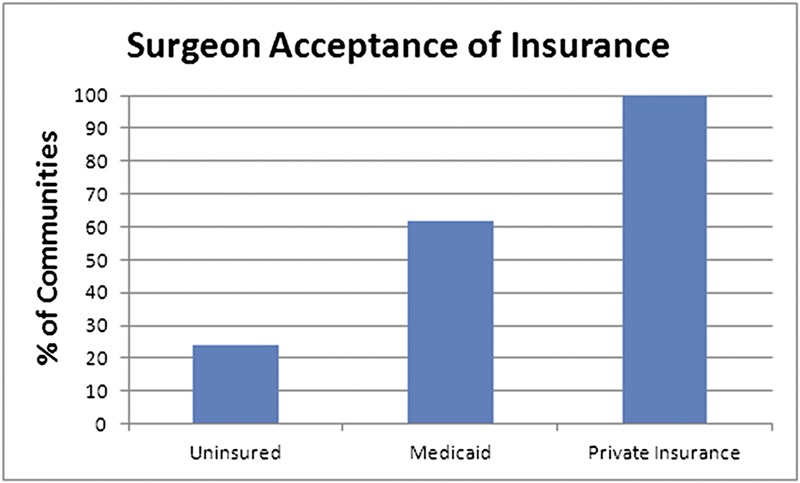
Bar graph showing the percentages of communities with surgeons accepting patients with hand problems according to insurance status according to primary care provider respondents.
Patients with Medicaid insurance who had been referred to our tertiary center more frequently failed to arrive to scheduled appointments than did those with private insurance. The no-show rate was 26% for patients with Medicaid insurance compared with 11% for patients with private insurance (p < 0.001). The no-show to arrival rate was one per 2.8 for patients with Medicaid insurance compared with one per 7.9 for patients with private insurance. The distance required to reach our office was significantly greater (p < 0.001) for patients who failed to arrive for appointments (fifty-eight miles) compared with those who did arrive for appointments (thirty-six miles), and cancellation rates increased from 36% among those traveling less than fifty miles to 61% for those traveling >100 miles (p < 0.001). This impact of travel distance on arrivals was not seen among patients who were well insured (i.e., patients who had Medicare or private insurance) traveling from the same home zip codes as the patients with Medicaid insurance. The mean travel distance for patients who were well insured was similar for those arriving for appointments (fifteen miles) compared with those cancelling appointments (sixteen miles). Cancellation rates for patients who were well insured were statistically similar (p = 0.53) for those who traveled less than fifty miles (27%) and those who traveled >100 miles (31%).
Forty-eight patients who were underinsured and 590 patients who had private insurance presented with a diagnosis of distal radial fracture, carpal tunnel syndrome, or trigger finger. After correcting for the relative rates of each diagnosis, the final operative rate for patients who were underinsured (45.8%) was equivalent (p = 0.92) to that of patients who were insured (45.1%).
Discussion
This study examined the patterns of elective, outpatient health-care utilization at a tertiary center for hand surgery. The investigation was prompted by reports suggesting that patients either with Medicaid insurance or without health insurance have difficulty accessing health care8-11. The majority of investigations into the effects of insurance status on tertiary-level surgical care have examined emergency transfer patterns1-4,12. Emergency patient transfers have occurred under the regulation of the Emergency Medical Treatment and Active Labor Act (EMTALA) since 1986. Thus, these studies have assessed hospital-level compliance with federal regulations. Within this setting, Archdeacon et al. investigated the influence of insurance status on transfers of patients with femoral fractures to a level-1 trauma center from 1999 to 20012. The authors identified a clear tendency for community hospitals to definitively manage patients who were insured and had femoral fractures (67% [thirty-three of forty-nine patients]) and to transfer patients who were not insured (100% [twenty-two patients]).
To our knowledge, no legislative guidance exists with regard to the transfer of care for patients with elective health issues. Physicians of all specialties have an ethical obligation to care for those in need regardless of insurance status but are not legally bound to do so. Therefore, we believe that this investigation into elective outpatient specialty care is unique as an assessment of physicians’ collective willingness to care for patients despite widely disparate reimbursement rates in a setting devoid of legal requirements.
Weiner et al. documented that insurance status played a role in patient referrals for spine surgery and noted that patients who were underinsured traveled thirty-seven miles farther to appointments than patients who were privately insured and bypassed five fellowship-trained spine surgeons en route to the authors’ center5. We similarly identified evidence of difficulty for patients who had Medicaid insurance or were uninsured in accessing hand specialty care. Primary care physicians reported difficulty scheduling these disadvantaged patients with community surgeons for hand evaluations. Although increased travel distance to access medical care is of concern for the entire population, patients who are underinsured are the least capable of absorbing this additional travel burden and travel expense. Additionally, patients who are underinsured may hold less secure employment and may be at higher risk for employment problems secondary to taking time off to travel substantial distances to specialty appointments. From a societal perspective, the distance that the most economically disadvantaged are forced to travel should be minimized.
Our investigation did not demonstrate global misuse of the tertiary hand center as patients presented with similar distributions of clinical complexity regardless of insurance status and increasing clinical complexity was associated with greater distances traveled to appointments. The discrepancy between these data, which suggest appropriate tertiary care resource utilization, and survey data that confirm that the primary care physicians have difficulty getting patients who were underinsured to local surgeons may be explained by the socioeconomic challenges facing patients with Medicaid insurance. If all patients with Medicaid insurance were able to access our tertiary care center at a rate similar to those with private insurance, it is likely that we would have seen a markedly greater percentage of patients with Medicaid insurance. As we found, patients with Medicaid insurance were over twice as likely to fail to show for appointments, and nearly 50% of primary care providers who responded to our survey reported that these patients would be unable to drive to our center because of limited personal resources and would be more likely to live with their problems. This inability to access hand care at a distant tertiary center despite available appointments was also suggested by higher cancellation rates for patients with Medicaid insurance as travel distances increased. Therefore, because patients failed to arrive at our tertiary center, our data regarding tertiary care utilization were biased toward underestimating the number of patients who were underinsured and had been recommended to seek care at the tertiary center. This result may also explain why we found relatively fewer patients with Medicaid insurance presenting with simple diagnoses than those with private insurance and the same population was more likely to be transferred to our emergency department following low-complexity orthopaedic trauma1. The difference between these situations may be that emergency transfers are completed via ambulance and outpatient evaluations require patients to have personal resources to arrive at the tertiary center.
Our study had several limitations. First, the data reflected the experience of a single tertiary center. Our findings may not be generalized to other institutions or practices in other locations. However, we believe that this study accurately reflects our practice as we examined all new patient visits to the orthopaedic hand surgery division over a twelve-month period. Unlike trauma referral studies, there is no Injury Severity Score equivalent or gold-standard method to rate common hand conditions according to their complexity. Therefore, any investigation assessing clinical severity must rely on surgeons to reasonably rate the diagnoses encountered. We developed the ad hoc scoring system utilized in this study by consensus with two attending surgeons (R.P.C. and C.A.G.) and then independently reviewed all diagnoses with qualifiers while blinded to the distance traveled and the insurance status to minimize bias in this assessment. Notably, prior investigations have utilized clinical severity scores (rated by attending physicians), and the complexity ratings in the present study resulted in scoring with high interrater reliability1,12. In this study, we chose to examine patients with Medicaid insurance as a group most likely to be refused by community surgeons. This decision was based on current reimbursement rates in our state. Medicaid reimbursement rates fluctuate over time and vary by state. However, the difficulties in obtaining specialty care for those patients with the insurance coverage least likely to reimburse physicians are probably universal. Finally, our physician survey was limited by a low response rate despite multiple attempts to contact eligible providers.
Patient insurance status appears to impact access to hand surgical care as economically disadvantaged patients face the greatest challenges in accessing outpatient specialty care. These patients both are less likely to be accepted by local surgical offices and, when accepted for care at a tertiary center, are more likely to fail to present for scheduled visits. Improving access to specialty surgical care for economically disadvantaged people will require addressing both health-care resource availability and socioeconomic barriers to traveling to tertiary care centers.
Appendix
A table showing a list of questions provided to primary care physicians is available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Goldfarb CA, Borrelli J, Jr, Lu M, Ricci WM. A prospective evaluation of patients with isolated orthopedic injuries transferred to a level I trauma center. J Orthop Trauma. 2006 Oct;20(9):613-7 [DOI] [PubMed] [Google Scholar]
- 2.Archdeacon MT, Simon PM, Wyrick JD. The influence of insurance status on the transfer of femoral fracture patients to a level-I trauma center. J Bone Joint Surg Am. 2007 Dec;89(12):2625-31 [DOI] [PubMed] [Google Scholar]
- 3.Nathens AB, Maier RV, Copass MK, Jurkovich GJ. Payer status: the unspoken triage criterion. J Trauma. 2001 May;50(5):776-83 [DOI] [PubMed] [Google Scholar]
- 4.Parks J, Gentilello LM, Shafi S. Financial triage in transfer of trauma patients: a myth or a reality? Am J Surg. 2009 Sep;198(3):e35-8 Epub 2009 May 9 [DOI] [PubMed] [Google Scholar]
- 5.Weiner BK, Black KP, Gish J. Access to spine care for the poor and near poor. Spine J. 2009 Mar;9(3):221-4 Epub 2008 May 12 [DOI] [PubMed] [Google Scholar]
- 6.Division of Health and Social Services. www.dhss.mo.gov/ASPsMedicaid/Main.php?cnty=xxx. Accessed 2010 Nov.
- 7.Missouri Census Data Center. Population estimates by age. http://mcdc.missouri.edu/websas/estimates_by_age.shtml. Accessed 2012 Aug 7.
- 8.Freeman HE, Corey CR. Insurance status and access to health services among poor persons. Health Serv Res. 1993 Dec;28(5):531-41 [PMC free article] [PubMed] [Google Scholar]
- 9.Yelin E, Bernhard G, Pflugrad D. Access to medical care among persons with musculoskeletal conditions. A study using a random sample of households in San Mateo County, California. Arthritis Rheum. 1995 Aug;38(8):1128-33 [DOI] [PubMed] [Google Scholar]
- 10.Yong PF, Milner PC, Payne JN, Lewis PA, Jennison C. Inequalities in access to knee joint replacements for people in need. Ann Rheum Dis. 2004 Nov;63(11):1483-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Milner PC, Payne JN, Stanfield RC, Lewis PA, Jennison C, Saul C. Inequalities in accessing hip joint replacement for people in need. Eur J Public Health. 2004 Mar;14(1):58-62 [DOI] [PubMed] [Google Scholar]
- 12.Crichlow RJ, Zeni A, Reveal G, Kuhl M, Heisler J, Kaehr D, Vijay P, Musapatika DL. Appropriateness of patient transfer with associated orthopaedic injuries to a Level I trauma center. J Orthop Trauma. 2010 Jun;24(6):331-5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest


