Abstract
Background:
Surgical repair is a common method of treatment of acute Achilles rupture in North America because, despite a higher risk of overall complications, it has been believed to offer a reduced risk of rerupture. However, more recent trials, particularly those using functional bracing with early range of motion, have challenged this belief. The aim of this meta-analysis was to compare surgical treatment and conservative treatment with regard to the rerupture rate, the overall rate of other complications, return to work, calf circumference, and functional outcomes, as well as to examine the effects of early range of motion on the rerupture rate.
Methods:
A literature search, data extraction, and quality assessment were conducted by two independent reviewers. Publication bias was assessed with use of the Egger and Begg tests. Heterogeneity was assessed with use of the I2 test, and fixed or random-effect models were used accordingly. Pooled results were expressed as risk ratios, risk differences, and weighted or standardized mean differences, as appropriate. Meta-regression was employed to identify causes of heterogeneity. Subgroup analysis was performed to assess the effect of early range of motion.
Results:
Ten studies met the inclusion criteria. If functional rehabilitation with early range of motion was employed, rerupture rates were equal for surgical and nonsurgical patients (risk difference = 1.7%, p = 0.45). If such early range of motion was not employed, the absolute risk reduction achieved by surgery was 8.8% (p = 0.001 in favor of surgery). Surgery was associated with an absolute risk increase of 15.8% (p = 0.016 in favor of nonoperative management) for complications other than rerupture. Surgical patients returned to work 19.16 days sooner (p = 0.0014). There was no significant difference between the two treatments with regard to calf circumference (p = 0.357), strength (p = 0.806), or functional outcomes (p = 0.226).
Conclusions:
The results of the meta-analysis demonstrate that conservative treatment should be considered at centers using functional rehabilitation. This resulted in rerupture rates similar to those for surgical treatment while offering the advantage of a decrease in other complications. Surgical repair should be preferred at centers that do not employ early-range-of-motion protocols as it decreased the rerupture risk in such patients.
Level of Evidence:
Therapeutic Level I. See Instructions for Authors for a complete description of levels of evidence.
The Achilles tendon is the most commonly ruptured tendon in the body1. Risk factors for primary acute rupture include male sex, use of steroids or fluoroquinolones, and prior rupture on the contralateral side. Diagnosis is made on the basis of a palpable gap and a positive Thompson test. If the physical examination is equivocal, ultrasonography or magnetic resonance imaging can be used to confirm the diagnosis2-4.
Treatment options for acute Achilles tendon rupture include nonsurgical and surgical management. If the treating physician opts for nonsurgical treatment, the patient is treated nonoperatively in a cast, cast-boot, or splint with the foot placed in plantar flexion, with or without early physiotherapy. Surgical options include open, minimally invasive, and percutaneous repair of the tendon5.
Advocates of nonsurgical treatment argue that the tendon apposition achieved by keeping the foot in plantar flexion is sufficient to allow adequate healing of the ruptured tendon. In theory, healing is achieved without the high complication risk associated with surgical treatment. Major complications secondary to surgical treatment of acute Achilles tendon rupture occur in up to 10% of cases and include deep infection, skin necrosis, tendon necrosis, and a draining sinus. The prevalence of minor complications is also substantial, with up to 15% of patients developing skin problems. However, despite these concerns, surgical repair of acute Achilles tendon rupture remains a common treatment in North America2-6.
The majority of surgeons who choose to repair Achilles tendon ruptures do so because nonsurgical treatment has been thought to be associated with an unacceptable rate of rerupture. In fact, according to some studies, the rerupture rate following nonsurgical treatment is as high as 10% to 12%. Surgery, on the other hand, lowers the rate to <3%. The surgical repair of acute Achilles tendon rupture has been further supported by an expected-value decision analysis study7. Thus, the risk of complications associated with surgery has appeared to be an acceptable trade-off for patients and surgeons who pursue surgical treatment2-5.
Traditionally, the affected limb has been immobilized for a minimum of six to eight weeks prior to starting range-of-motion exercises; this is intended to protect the surgical repair (if surgical treatment is chosen) or to maintain tendon apposition (if nonsurgical treatment is chosen). However, more recently, functional bracing and modified postoperative regimens allow patients to perform daily active plantar flexion exercises as soon as ten days following injury. This is thought to stimulate tendon-healing, and it may lower the rerupture rate that is typically associated with nonsurgical treatment8.
Two previous meta-analyses of randomized and pseudorandomized trials comparing surgical with nonsurgical treatment have already been published, with the latest one including studies up to 20049,10. The authors concluded that although surgical treatment significantly reduced the risk of rerupture of the tendon, it also led to a higher rate of other complications. However, since the latest of the two previously published meta-analyses, several additional randomized controlled clinical trials have sought to clarify the best treatment for acute Achilles tendon rupture11-13. These trials, particularly those using functional bracing, have challenged the conclusions of the previous meta-analyses. Because of the conflicting results in the current body of literature, a reexamination of the evidence is needed to take into consideration the new trials. The aim of the present meta-analysis was to compare surgical with nonsurgical treatment with regard to the rerupture rate, overall rate of other complications, return to work, strength, calf circumference, and functional outcomes, as well as to explore the effects of early range of motion on the rerupture rate.
Materials and Methods
Study Selection
Two reviewers independently searched the most commonly used medical databases (Cochrane Central Register of Controlled Trials, MEDLINE, Web of Science, and Embase) from January 2005 through December 2011, using the search strings “Achilles tendon”[MeSH] OR “achilles”[tw] OR “tendoachilles”[tw] OR “calcaneal”[tw] OR “calcanean”[tw] OR “calcaneus”[tw] AND “rupture”[MeSH] OR “rupture”[tw] OR “ruptures”[tw] OR “ruptured”[tw] OR “lesion”[tw] OR “lesions”[tw] OR “tear”[tw] OR “tears”[tw] and random*. We also scanned the reference lists of the included articles for additional articles that met the inclusion criteria, and we searched proceedings of relevant meetings from 2005 to 2011 to identify unpublished reports.
We included studies of patients with acute Achilles tendon rupture from any cause. All randomized controlled trials comparing surgical intervention with nonsurgical treatment were considered for inclusion. For a study to be considered for inclusion, treatment had to have been initiated within three weeks of the rupture. Surgical treatment included open or minimally invasive techniques. Nonsurgical management included casting or splinting. There were no restrictions on inclusion on the basis of weight-bearing status or use of early range of motion. Trials that included patients with delayed presentation (beyond three weeks) and trials that included patients being treated for rerupture were excluded. Duplicate data were excluded. There were no language restrictions, and foreign-language papers were translated.
The quality of each study selected for inclusion was evaluated by two independent reviewers with use of the bias tool recommended by the Cochrane Handbook for Systematic Reviews of Interventions, version 5.0.214. We attempted to clarify any uncertainties in results or methodology by means of personal correspondence with the authors. Because all of the included studies were randomized controlled trials of similar methodological quality, they were not weighted on the basis of methodology.
Data Extraction and Outcome Measures
Data were extracted independently by two reviewers with use of standardized extraction forms. The primary outcome of interest was the rerupture rate. Secondary outcomes included the rate of other complications, strength, range of motion, time to return to work, calf circumference, and functional outcomes.
Statistical Analysis
If the standard error was not reported, it was imputed with use of the technique described by Ma et al.15. If neither the mean nor the standard error was reported, these were imputed from the median and range with use of the technique described by Hozo et al.16. Publication bias was assessed with use of the Begg and Egger tests. These tests examine funnel plot asymmetry and the adjusted rank correlation to determine the presence of publication bias. Dichotomous variables were expressed as the risk difference or the risk ratio. Continuous data were reported as the weighted mean difference (for outcomes measured with use of a single scale) or as the standardized mean difference (for outcomes measured with use of different scales). Heterogeneity across the combined data was assessed with use of the I2 test. A p value of <0.15 on the I2 test was considered an indicator of significant heterogeneity. Pooled summary statistics were calculated with use of a fixed-effect model if heterogeneity was not significant or with use of a random-effect model if heterogeneity was significant. Differences were considered significant if the p value was <0.05. Meta-regression and subgroup analysis were employed to assess factors responsible for heterogeneity of the primary outcome.
Source of Funding
There was no external funding source.
Results
Studies and Baseline Patient Characteristics
Our search of the databases yielded a total of 614 articles, and one additional study was indentified through scanning of conference proceedings and has since been published. All abstracts were examined, and 596 were considered to not meet the inclusion criteria. A total of nineteen studies were considered for inclusion and the full text was obtained. After consideration of the entire article, ten studies were considered to meet the inclusion criteria (Fig. 1)11-13,17-23.
Fig. 1.
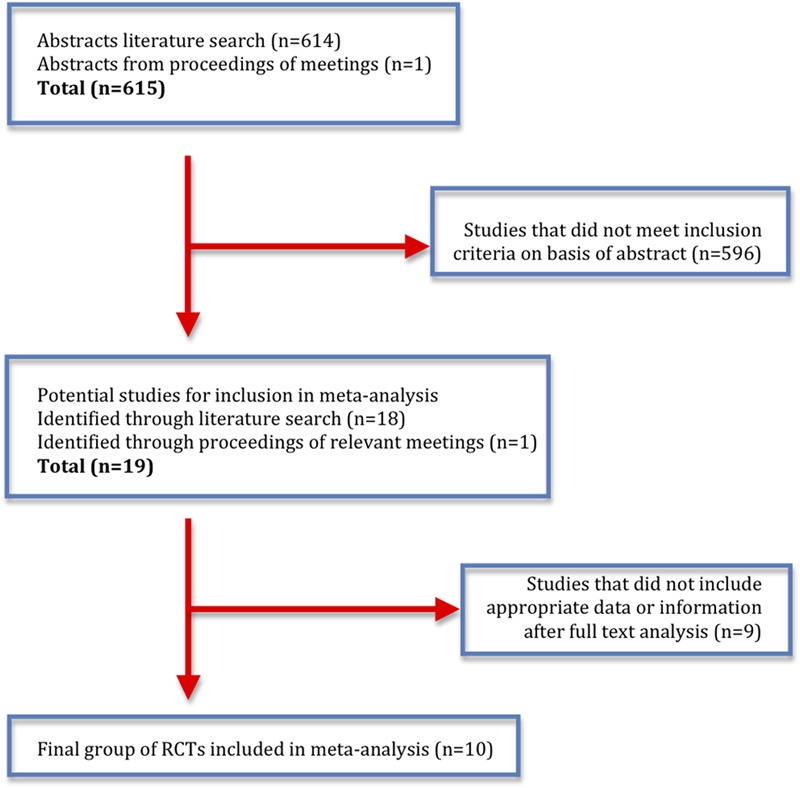
Literature search strategy and results. RCT = randomized controlled trial.
Baseline patient characteristics are presented in the Appendix. The ten selected studies included 418 patients who were treated surgically and 408 patients who underwent nonsurgical treatment. The patients were predominantly male, and the mean age in each patient group was 39.8 years.
Rerupture
All ten of the studies reported the rerupture rate11-13,17-23 (Fig. 2). The pooled results show that the absolute risk difference between the groups was 5.5% in favor of surgery (p = 0.002). This corresponded to a risk ratio of 0.4 in favor of surgery. Of note, there was significant heterogeneity among the studies (p = 0.13 for the I2 test). The number needed to treat (the number of patients who would need to be treated in order to prevent one rerupture) was eighteen patients.
Fig. 2.
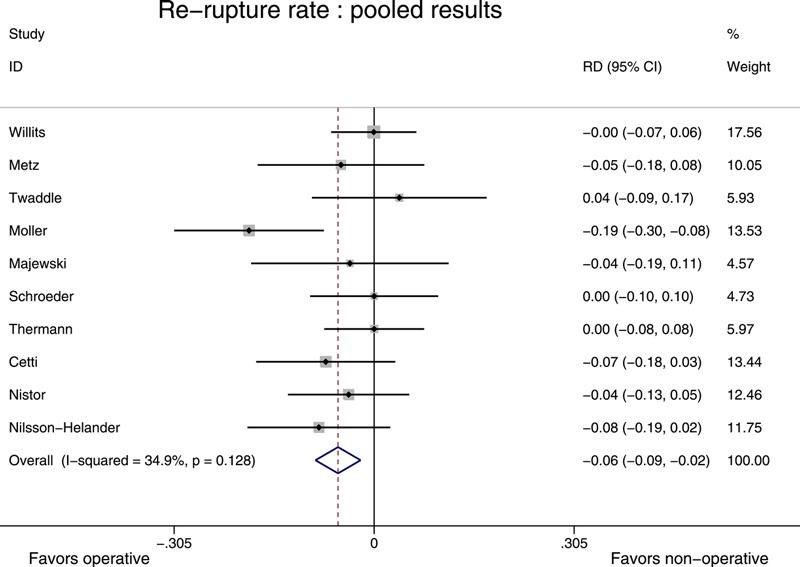
Pooled results for the rerupture rate; results favoring operative intervention are plotted on the left. The risk difference between the two groups was 0.055, or 5.5%, in favor of surgery (p = 0.002). RD = risk difference, and CI = confidence interval.
Since there was significant heterogeneity among the studies, factors that were potentially responsible for the heterogeneity were explored with use of meta-regression. The use of functional rehabilitation was a significant cause of heterogeneity (p < 0.05). The other factors that were considered (study size, duration of follow-up, and year of publication) were not significant. A stratified analysis of rerupture rates according to functional rehabilitation was therefore performed (Fig. 3).
Fig. 3.

Pooled results for the subgroup analysis of the rerupture rate; results favoring operative intervention are plotted on the left. The upper portion of the figure shows a significant difference in the trials that did not use early range of motion, whereas the lower portion shows that there was no significant difference in the trials that used early range of motion. RD = risk difference, and CI = confidence interval.
The results of the stratified analysis showed that if a functional rehabilitation protocol with early range of motion was used, surgical treatment and nonsurgical treatments were equivalent with regard to the rerupture rate (absolute risk difference = 1.7%, p = 0.45), suggesting that no absolute risk reduction was achieved by performing surgery. However, if the treatment protocol used after the rupture included prolonged immobilization, the absolute reduction in the rerupture risk obtained by surgical intervention was 8.8% (p = 0.001). These results suggest that surgical and nonsurgical treatments were equivalent with regard to rerupture if the protocol after the rupture included early range of motion. However, if functional rehabilitation was not employed, surgical repair reduced the absolute rerupture risk by 8.8% and the number needed to treat was therefore twelve patients. Of note, the studies within each subgroup did not show any further evidence of significant heterogeneity (p = 0.61 for the I2 test in the functional rehabilitation group and p = 0.28 in the casting group).
Other Complications
Nine studies reported the total rate of complications other than rerupture12,13,17-23 (Fig. 4). Complications included deep and superficial wound infections, skin and tendon necrosis, fistulas, scar adhesion, sural nerve damage, decreased ankle motion, overlengthening of the tendon, deep venous thrombosis, and pulmonary embolus. The meta-analysis indicated that the risk difference was 15.8% in favor of nonsurgical treatment (p = 0.016). This translated into a risk ratio of 3.897, and one additional complication other than rerupture could be expected for every seven patients treated surgically.
Fig. 4.

Pooled results for the rate of complications other than rerupture; results favoring operative intervention are plotted on the left. The risk difference was 15.8% in favor of nonsurgical treatment. RD = risk difference, and CI = confidence interval.
Time to Return to Work
Four studies reported the time to return to work, expressed as days until work was resumed17,19,22,23 (see Appendix). Fixed-effect analysis showed that, on average, patients whose Achilles tendon rupture was repaired surgically returned to work 19.16 days earlier than patients who underwent nonsurgical treatment (95% confidence interval [CI], 3.9 to 34.0; p = 0.0014).
Range of Motion
Three studies reported the range of ankle motion, expressed as the difference in plantar flexion (in degrees) compared with the contralateral side11,13,19 (Fig. 5). Fixed-effect analysis showed that active plantar flexion relative to the contralateral side was 1.07° less in patients undergoing nonsurgical treatment (95% CI, 0.17° to 1.96°; p = 0.019). However, although these results were statistically significant, they do not represent a clinically important difference.
Fig. 5.
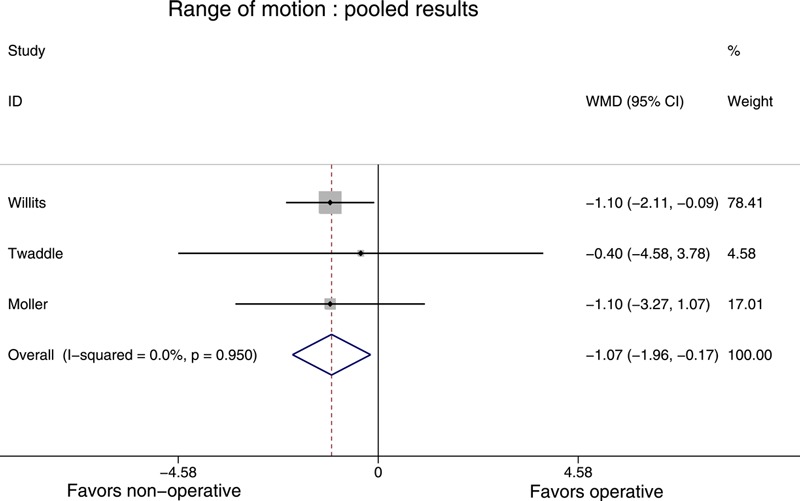
Pooled results for range of motion; results favoring operative intervention are plotted on the right. WMD = weighted mean difference, and CI = confidence interval.
Calf Circumference
Three studies reported the calf circumference, expressed as the difference in circumference (in cm) compared with contralateral side11,13,19 (see Appendix). Fixed-effect analysis showed no significant difference between the two groups (p = 0.357).
Strength
Six studies reported strength, which was expressed with use of different scales in each study12,13,18-20,22 (Fig. 6). Random-effect analysis showed that the standardized mean difference did not differ significantly between the two groups (p = 0.806).
Fig. 6.
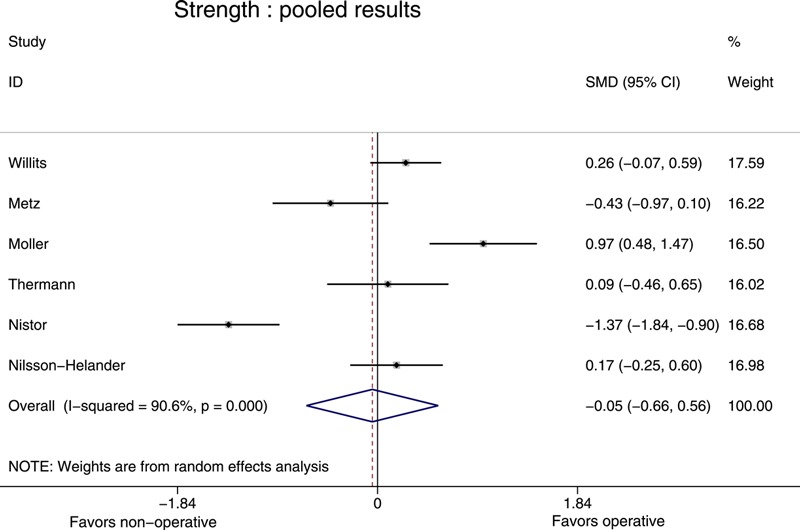
Pooled results for strength; results favoring operative intervention are plotted on the right. SMD = standardized mean difference, and CI = confidence interval.
Functional Outcomes
Four studies reported functional outcomes, expressed with use of different scales (the Musculoskeletal Functional Assessment Instrument [MFAI], Functional Index for the Lower Leg and Ankle [FIL], Leppilahti score, and modified Leppilahti score) in each study11,13,19,22 (see Appendix). Fixed-effect analysis showed that the standardized mean difference did not differ significantly between the two groups (p = 0.226).
Discussion
This study suggests that surgical treatment and nonsurgical treatment of acute Achilles tendon rupture were equivalent with regard to rerupture rate when the nonsurgical treatment protocol included early range of motion. However, if such functional rehabilitation was not employed, surgical repair reduced the rerupture risk by 8.8%, with the number of patients needed to treat to prevent one rerupture being twelve. This should be contrasted against the cumulative burden of complications in these individuals: according to the published data, two of these twelve patients will experience a complication following surgery.
The risk of other complications for surgically treated patients was 3.9 times that of nonsurgically treated patients, which resulted in an absolute risk increase of 15.8%; one additional complication other than rerupture could be expected for every seven patients treated surgically. It is important to mention that the complications reported in the published randomized controlled trials included both minor and major complications. Another important aspect of clinical decision-making is the prevalence of major skin complications in the surgical treatment group. Unfortunately, the data did not allow us to differentiate between major and minor complications or between skin complications and other types of complications in our analysis.
According to the meta-analysis, patients undergoing surgery returned to work nineteen days sooner, on average, than patients undergoing nonsurgical treatment. However, these results are based on a small number of studies, and those studies did not report which criteria were used to determine when a patient should be allowed to resume work activities. Further studies on this subject should be performed using predetermined criteria that patients in both groups must meet prior to returning to work.
The difference in active plantar flexion between the two groups was not clinically important. There was no significant difference between nonsurgical treatment and surgical treatment with regard to calf circumference, strength, or functional outcomes.
Although two meta-analyses have been published previously, our study includes foreign-language papers, contains a substantial number of new randomized trials that have been published since 2004, and includes a subgroup analysis of the rerupture rate. According to the results of our meta-analysis, nonsurgical treatment represents a reasonable treatment choice at centers that use functional rehabilitation with early range of motion since surgical repair did not decrease the rerupture rate and was associated with a higher rate of other complications. Surgical repair can be considered at centers that do not employ early range of motion, or for patients who are poor candidates for this more time-consuming post-injury protocol; although it was associated with a higher overall rate of other complications, it reduced the rerupture rate. The increased risk of having a complication other than a rerupture in the surgical group (risk difference, 15.8%) appears to be more important that the increased risk of having a rerupture (risk difference, 8.8%) in the nonsurgical group. Nevertheless, given that not all complications are major, some patients and surgeons may consider the increased rate of other complications following surgical treatment to be an acceptable trade-off for the reduced rerupture rate. We believe that this information should be part of the informed consent discussion when surgery is being considered.
This meta-analysis shows that surgical treatment and nonsurgical treatment using functional rehabilitation were equivalent with regard to rerupture rate, range of motion, calf circumference, and functional outcomes. However, further research on Achilles tendon rupture treatment is warranted. For instance, randomized trials are needed to compare percutaneous repair with nonsurgical treatment to determine the difference in complications between the two treatment modalities. Another area for future research is the study of criteria that would allow physicians to select patients who would be appropriate for nonsurgical treatment.
Appendix
A table summarizing patient demographics in the included studies and figures showing the pooled data for return to work, calf circumference, and functional outcomes are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
A table summarizing patient demographics in the included studies and figures showing the pooled data for return to work, calf circumference, and functional outcomes
Footnotes
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Józsa L, Kvist M, Bálint BJ, Reffy A, Järvinen M, Lehto M, Barzo M. The role of recreational sport activity in Achilles tendon rupture. A clinical, pathoanatomical, and sociological study of 292 cases. Am J Sports Med 1989;17:338-43 [DOI] [PubMed] [Google Scholar]
- 2.Nyyssönen T, Lüthje P, Kröger H. The increasing incidence and difference in sex distribution of Achilles tendon rupture in Finland in 1987-1999. Scand J Surg. 2008;97(3):272-5 [DOI] [PubMed] [Google Scholar]
- 3.Hess GW. Achilles tendon rupture: a review of etiology, population, anatomy, risk factors, and injury prevention. Foot Ankle Spec. 2010 Feb;3(1):29-32 Epub 2009 Dec 15 [DOI] [PubMed] [Google Scholar]
- 4.Cary DV. How to diagnose and manage an acute Achilles tendon rupture. JAAPA. 2009 Aug;22(8):39-43 [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Orthopaedic Surgeons. The diagnosis and treatment of acute Achilles tendon rupture: guideline and evidence report. 2009 Dec 4. http://www.aaos.org/research/guidelines/ATRguideline.pdf. Accessed 2010 Feb. [Google Scholar]
- 6.Molloy A, Wood EV. Complications of the treatment of Achilles tendon ruptures. Foot Ankle Clin. 2009 Dec;14(4):745-59 [DOI] [PubMed] [Google Scholar]
- 7.Kocher MS, Bishop J, Marshall R, Briggs KK, Hawkins RJ. Operative versus nonoperative management of acute Achilles tendon rupture: expected-value decision analysis. Am J Sports Med. 2002 Nov-Dec;30(6):783-90 [DOI] [PubMed] [Google Scholar]
- 8.Wallace RG, Heyes GJ, Michael AL. The non-operative functional management of patients with a rupture of the tendo Achillis leads to low rates of re-rupture. J Bone Joint Surg Br. 2011 Oct;93(10):1362-6 [DOI] [PubMed] [Google Scholar]
- 9.Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute Achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005 Oct;87(10):2202-10 [DOI] [PubMed] [Google Scholar]
- 10.Bhandari M, Guyatt GH, Siddiqui F, Morrow F, Busse J, Leighton RK, Sprague S, Schemitsch EH. Treatment of acute Achilles tendon ruptures: a systematic overview and metaanalysis. Clin Orthop Relat Res. 2002 Jul;(400):190-200 [DOI] [PubMed] [Google Scholar]
- 11.Twaddle BC, Poon P. Early motion for Achilles tendon ruptures: is surgery important? A randomized, prospective study. Am J Sports Med. 2007 Dec;35(12):2033-8 Epub 2007 Sep 20 [DOI] [PubMed] [Google Scholar]
- 12.Nilsson-Helander K, Silbernagel KG, Thomeé R, Faxén E, Olsson N, Eriksson BI, Karlsson J. Acute Achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010 Nov;38(11):2186-93 Epub 2010 Aug 27 [DOI] [PubMed] [Google Scholar]
- 13.Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, Fowler P, Kean CO, Kirkley A. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010 Dec 1;92(17):2767-75 Epub 2010 Oct 29 [DOI] [PubMed] [Google Scholar]
- 14.Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.0.2 [updated September 2009]. Oxford, United Kingdom: The Cochrane Collaboration; 2009. http://www.cochrane-handbook.org [Google Scholar]
- 15.Ma J, Liu W, Hunter A, Zhang W. Performing meta-analysis with incomplete statistical information in clinical trials. BMC Med Res Methodol. 2008 Aug 18;8:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005 Apr 20;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cetti R, Christensen SE, Ejsted R, Jensen NM, Jorgensen U. Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med. 1993 Nov-Dec;21(6):791-9 [DOI] [PubMed] [Google Scholar]
- 18.Thermann H, Zwipp H, Tscherne H. [Functional treatment concept of acute rupture of the Achilles tendon. 2 years results of a prospective randomized study]. Unfallchirurg. 1995 Jan;98(1):21-32 German [PubMed] [Google Scholar]
- 19.Möller M, Movin T, Granhed H, Lind K, Faxén E, Karlsson J. Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Joint Surg Br. 2001 Aug;83(6):843-8 [DOI] [PubMed] [Google Scholar]
- 20.Nistor L. Surgical and non-surgical treatment of Achilles tendon rupture. A prospective randomized study. J Bone Joint Surg Am. 1981 Mar;63(3):394-9 [PubMed] [Google Scholar]
- 21.Schroeder D, Lehmann M, Steinbrueck K. Treatment of acute Achilles tendon ruptures: open vs. percutaneous repair vs. conservative treatment. A prospective randomized study. Orthop Trans. 1997;21:1228 [Google Scholar]
- 22.Metz R, Verleisdonk EJ, van der Heijden GJ, Clevers GJ, Hammacher ER, Verhofstad MH, van der Werken C. Acute Achilles tendon rupture: minimally invasive surgery versus nonoperative treatment with immediate full weightbearing–a randomized controlled trial. Am J Sports Med. 2008 Sep;36(9):1688-94 Epub 2008 Jul 21 [DOI] [PubMed] [Google Scholar]
- 23.Majewski M, Rickert M, Steinbrück K. [Achilles tendon rupture. A prospective study assessing various treatment possibilities]. Orthopade. 2000 Jul;29(7):670-6 German [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
A table summarizing patient demographics in the included studies and figures showing the pooled data for return to work, calf circumference, and functional outcomes


