Abstract
Objective: To review the current therapy for granuloma annulare and report a case of refractory generalized granuloma annulare successfully treated with excimer laser. A discussion about the characteristics of excimer laser and the mechanism of its effectiveness is presented. Design: Patient case report and literature review. Setting: Outpatient dermatology practice. Participants: A 73-year-old woman suffering from generalized granuloma annulare for more than 40 years. Measurements: Change in clinical appearance of lesions. Results: Use of excimer laser therapy resulted in prompt and complete resolution in treated areas with no residual skin changes or side effects. Conclusion: Excimer laser therapy is a powerful treatment modality with minimal side effects for patients with granuloma annulare. Further study is necessary to elucidate optimal dosing, long-term efficacy, and safety profile.
Granuloma annulare (GA) is a relatively common disorder with a female predominance that usually presents as 1 to 5cm skin-colored or erythematous annular plaques with peripheral papules. While the localized form most frequently affects the dorsal surfaces of the extremities, GA may also have a generalized distribution characterized by more than 10 sites of involvement, frequently including the trunk, neck, scalp, and occasionally face.
The localized form has the highest incidence in patients under 30 years old and tends to have spontaneous resolution, with approximately one-half of lesions resolving within two years after diagnosis.1,2 Generalized GA has a bimodal distribution, with a peak in children less than 10 years of age and adults older than 40 years of age. Generalized GA exhibits more tenacious behavior and can occasionally be present for more than 10 years without resolution.2 These lesions are typically asymptomatic and patients most commonly seek treatment for cosmetic reasons.3
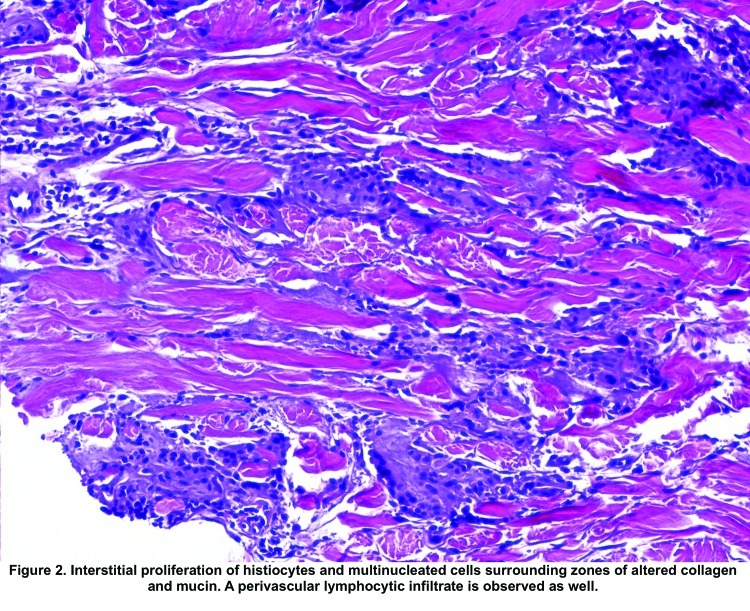
Histologically, GA is characterized by palisading histiocytes and lymphocytes surrounding an amorphous center of degenerating collagen and prominent mucin. This idiopathic reaction is believed to be a type IV hypersensitivity response to an unidentified antigen.2,6,7
Treatment of GA is dictated by lesion distribution. Localized GA has been successfully treated with topical therapy, including steroids under occlusion, intralesional steroid injections, and cryotherapy. Reports of successful treatment with topical tacrolimus as well as a combination of rifampin, ofloxacin, and minocycline have also been observed.4,5
Generalized GA requires aggressive systemic treatment to achieve clinical results. Psoralen + ultraviolet A therapy (PUVA), isotretinoin, dapsone, and cyclosporine have shown effectiveness in resolving generalized GA; however, these therapies are associated with serious side effects, which limit their utility.6
Several case reports and small trials have shown PUVA therapy to have an efficacy rate of 80 to 100 percent in clearing or significantly reducing GA lesions. Treatment duration is dependent on extent of disease and response to treatment.7,8 While effective at clearing GA, PUVA requires both frequent treatments and psoralen ingestion, which can cause gastrointestinal side effects and photosensitization with erythema and pruritus at treatment sites. Long-term use leads to actinic damage localized to treatment areas and an increased risk of cutaneous malignancy.9
Isotretinoin has been used in diffuse GA in patients intolerant or unresponsive to PUVA. Case reports have shown inconsistent efficacy, with either primary treatment failure or recurrence of lesions after discontinuation of therapy; the majority of cases, however, respond to the drug.6 Although effective, isotretinoin therapy is difficult to initiate and maintain. The prescribing physician, patient, and patient’s pharmacist are required to enter the iPledge registry and the patient is subject to mandatory initiation of two methods of birth control with monthly pregnancy tests and office evaluations to prevent isotretinoin’s teratogenicity. These requirements as well as the potential systemic side effects, including hyperlipidemia, hyperglycemia, hepatitis, hematologic dyscrasias, and mental status changes, decrease patient compliance with therapy.
Several reports demonstrated that dapsone had clinical merit in resolving generalized GA, but treatment failures resulted from drug ineffectiveness and intolerable side effects ranging from headaches, nausea, and hepatitis to agranulocytosis and aplastic anemia.10,11 Physicians treating with dapsone must be aware of its oxidative potential with resultant hemolytic anemia, and patients should be screened with a glucose-6-phosphate dehydrogenase assay prior to therapy. After treatment is initiated, complete blood counts (CBCs) are drawn weekly for the first month of therapy and then monthly for six months. Baseline liver function should be evaluated and values rechecked every three months of therapy.12 Published reports suggest that successful therapy is clinically evident by 12 weeks of therapy, exposing patients to extensive blood work and monitoring, which adds to treatment inconvenience.
Recently, Inui et al13 reported a patient with GA unresponsive to topical steroids and tacrolimus treated with narrowband ultraviolet B (NBUVB) resulting in resolution in 24 treatments with absence of recurrence. Another retrospective study of NBUVB noted “minimal to mild” improvement of generalized GA, but did not mention treatment regimen, duration, or patient compliance and satisfaction.14
CASE REPORT
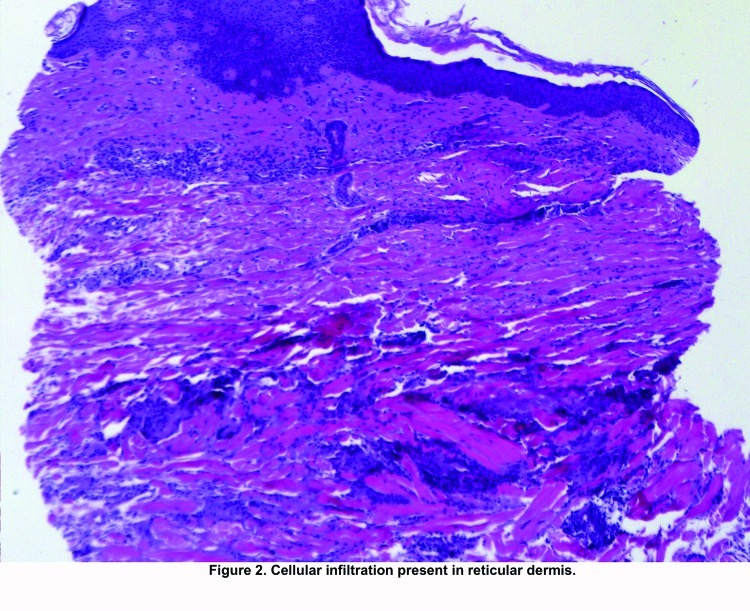
A 73-year-old woman with a long-standing history of GA presented to the dermatology clinic complaining of gradual worsening of her condition. Over the past 40 years, she has had lesions present on her trunk and extremities with gradual involvement of a larger surface area. Previous unsuccessful therapy included PUVA/methotrexate, which was discontinued due to actinic damage; dapsone; isotretinoin; and topical and intralesional steroid injections. Her past medical history was negative for diabetes, hypothyroidism, and diagnosed malignancy, and she denied any family history of autoimmune disease or dermatological conditions. On exam, she had numerous serpiginous plaques and erythematous papules on her chest, abdomen, back, and extremities, sparing the face (Figure 1). A biopsy obtained from an active lesion’s edge showed lymphocytic infiltration of the reticular dermis (Figure 2). At higher magnification, there was an interstitial proliferation of histiocytes and multinucleated cells palisading around zones of altered collagen and mucin, with a perivascular lymphocytic infiltrate, suggesting granuloma annulare (Figure 3).
Figure 1.

Dorsum of patient’s right hand showing serpiginous erythematous plaques consistent with granuloma annulare. The patient had similar lesions on her trunk and extremities, but not her face.
Figure 2.
Cellular infiltration present in reticular dermis
Figure 3.
Interstitial proliferation of histiocytes and multinucleated cells surrounding zones of altered collagen and mucin. A perivascular lymphocytic infiltrate is observed as well.
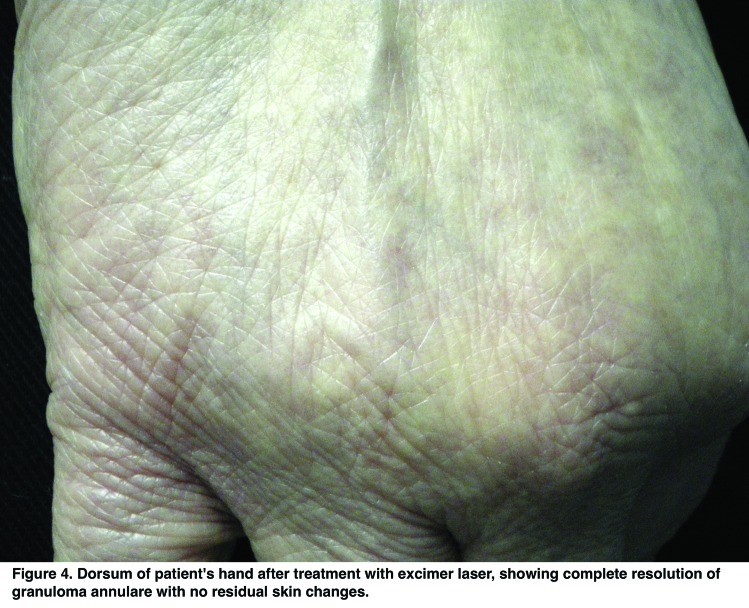
After discussion of her treatment options, the patient consented to a trial of excimer laser therapy on the dorsum of her hands. Treatment was initiated with 300mJ/cm2 with five doses per treatment session. After 15 treatment sessions, there was complete resolution with no residual scarring (Figure 4). The patient tolerated the procedure and reported no side effects. At her six-month follow up, she had no recurrence of GA in treated areas.
Figure 4.
Dorsum of patient’s hand after treatment with excimer laser, showing complete resolution of granuloma annulare with no residual skin changes.
DISCUSSION
The effectiveness of light therapy in the treatment of skin disorders marked by aberrant immune response relates to the antiproliferative effects of UV light on cutaneous lymphocytes via formation of pyrimidine dimers with induction of lymphocyte apoptosis. Additional proposed mechanisms involve altered cytokine expression with decreased cell mediated immunity, replacement of apoptotic T-helper cells with naïve lymphocytes, and decreased antigen presentation by Langerhans cells.15–17 In GA, cooperation between histiocytes and T-helper cells may be blunted by delivery of UVB spectrum light, resulting in decreased immunoreactivity to the unknown antigen implicated in granuloma formation. This mechanism may explain the observed effectiveness of excimer laser therapy in both resolving and suppressing further GA lesions.
The excimer laser system is a source of 308nm wavelength light, which has shown efficacy in treating psoriasis, vitiligo, atopic dermatitis, and other inflammatory dermatoses. It delivers a precise band of light, eliminating the unnecessary treatment of healthy perilesional skin and hyperpigmentation that may occur. This delivery system allows for higher fluence settings and consequent shorter treatment times, with studies reporting a lower cumulative dose necessary to achieve patient satisfaction.18–20 Treatment of GA with the excimer laser has not been previously reported in the literature and represents an exciting avenue of therapy that can lead to shorter time to remission with limited treatment side effects.
CONCLUSION
A case of generalized GA treated with the excimer laser resulted in resolution of lesions that had been refractory to other therapies. The case presented here suggests that further research is necessary to validate these results and determine optimal dosing schedule, safety, and long-term effectiveness.
Footnotes
DISCLOSURE:The authors report no relevant conflicts of interest.
REFERENCES
- 1.Smith MD, Downie JB, DiCostanzo D. Granuloma annulare. Int J Dermatol. 1997;36:326–333. doi: 10.1046/j.1365-4362.1997.00257.x. [DOI] [PubMed] [Google Scholar]
- 2.Cyr PR. Diagnosis and management of granuloma annulare. Am Fam Physician. 2006;74:1729–34. [PubMed] [Google Scholar]
- 3.Muhlbauer JE. Granuloma annulare. J Am Acad Dermatol. 1980;3:217. doi: 10.1016/s0190-9622(80)80181-2. [DOI] [PubMed] [Google Scholar]
- 4.Harth W, Linse R. Topical tacrolimus in granuloma annulare and necrobiosis lipoidica. Br J Dermatol. 2004;150:792–794. doi: 10.1111/j.0007-0963.2004.05899.x. [DOI] [PubMed] [Google Scholar]
- 5.Marcus DV, Mahmoud BH, Hamzavi IH. Granuloma annulare treated with rifampin, ofloxacin, and minocycline combination therapy. Arch Dermatol. 2009;145:787–789. doi: 10.1001/archdermatol.2009.55. [DOI] [PubMed] [Google Scholar]
- 6.Looney M, Smith KM. Isotretinoin in the treatment of granuloma annulare. Ann Pharmacother. 2004;38:494–497. doi: 10.1345/aph.1D312. [DOI] [PubMed] [Google Scholar]
- 7.Setterfield JS, Huilgol SC, Black MM. Generalised granuloma annulare successfully treated with PUVA. Clin Exp Dermatol. 1999;24:458–460. doi: 10.1046/j.1365-2230.1999.00532.x. [DOI] [PubMed] [Google Scholar]
- 8.Grundmann-Kollmann M, Ochsendorf FR, Zollner TM, et al. Cream psoralen plus ultraviolet A therapy for granuloma annulare. Br J Dermatol. 2001;144:996–999. doi: 10.1046/j.1365-2133.2001.04188.x. [DOI] [PubMed] [Google Scholar]
- 9.Van Praag MC, Tseng LN, Mommaas AM, et al. Minimising the risks of PUVA treatment. Drug Safety. 1993;8(5):340–349. doi: 10.2165/00002018-199308050-00002. [DOI] [PubMed] [Google Scholar]
- 10.Martín-Sáez E, Fernández-Guarino M, Carrillo-Gijón R, et al. Efficacy of dapsone in disseminated granuloma annulare: a case report and review of the literature. Actas Dermosifiliogr. 2008;99:64–68. [PubMed] [Google Scholar]
- 11.Potter MN, Yates P, Slade R, et al. Agranulocytosis caused by dapsone therapy for granuloma annulare. J Am Acad Dermatol. 1989;20:87–88. doi: 10.1016/s0190-9622(89)70013-x. [DOI] [PubMed] [Google Scholar]
- 12.Wolf R. Dapsone: unapproved uses or indications. Clin Dermatol. 2000;18:37–53. doi: 10.1016/s0738-081x(99)00093-0. [DOI] [PubMed] [Google Scholar]
- 13.Inui S, Nishida Y, Itami S, Katayama I. Disseminated granuloma annulare responsive to narrowband ultraviolet B therapy. J Am Acad Dermatol. 2005;53:533–534. doi: 10.1016/j.jaad.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 14.Yashar SS, Gielczyk R, Scherschun L, et al. Narrow-band ultraviolet B treatment for vitiligo, pruritus, and inflammatory dermatoses. Photodermatol Photoimmunol Photomed. 2003;19:164–168. doi: 10.1034/j.1600-0781.2003.00039.x. [DOI] [PubMed] [Google Scholar]
- 15.Dogra S, De D. Narrowband ultraviolet B in the treatment of psoriasis: the journey so far! Indian J Dermatol Venereol Leprol. 2010;76(6):652–661. doi: 10.4103/0378-6323.72461. [DOI] [PubMed] [Google Scholar]
- 16.Monfrecola G, Baldo A. Retinoids and phototherapy for psoriasis. J Rheumatol. 2009;83([Supplement].):71–72. doi: 10.3899/jrheum.090231. [DOI] [PubMed] [Google Scholar]
- 17.Nicolaidou E, Antoniou C, et al. Narrowband ultraviolet B phototherapy and 308-nm excimer laser in the treatment of vitiligo: a review. J Am Acad Dermatol. 2009;60(3):470–477. doi: 10.1016/j.jaad.2008.07.053. [DOI] [PubMed] [Google Scholar]
- 18.Aubin F, Vigan M, Puzenat E, et al. Evaluation of a novel 308nm monochromatic excimer light delivery system in dermatology: a pilot study in different chronic localized dermatoses. Br J Dermatol. 2005;152:99–103. doi: 10.1111/j.1365-2133.2005.06320.x. [DOI] [PubMed] [Google Scholar]
- 19.Do JE, Shin JY, Kim DY, et al. The effect of 308nm excimer laser on segmental vitiligo: a retrospective study of 80 patients with segmental vitiligo. Photodermatol Photoimmunol Photomed. 2011;27:147–151. doi: 10.1111/j.1600-0781.2011.00587.x. [DOI] [PubMed] [Google Scholar]
- 20.Nisticò SP, Saraceno R, Schipani C, et al. Different applications of monochromatic excimer light in skin diseases. Photomed Laser Surg. 2009;27(4):647–654. doi: 10.1089/pho.2008.2317. [DOI] [PubMed] [Google Scholar]