Abstract
Context
Communication is widely acknowledged as a crucial component of high-quality pediatric medical care, which is provided in situations where parents typically experience strong emotions.
Objectives
To explore emotion using both the LIWC and a self-report questionnaire to better understand the relationship between these two measures of emotion in a pediatric care context.
Methods
Sixty-nine parents of 47 children who were participants in the Decision Making in Pediatric Palliative Care Study at The Children’s Hospital of Philadelphia took part in this study. Parents completed the Positive and Negative Affect Schedule (PANAS) and a semi-structured interview about their children and experience with medical decision making. The transcribed interviews were analyzed with the Linguistic Inquiry and Word Count (LIWC) program, which yields scores for positive and negative emotional expression. The association between LIWC and PANAS scores was evaluated using multivariate linear regression to adjust for potential confounders.
Results
Parents who used more positive words when speaking about their children’s illnesses and the experience of medical decision making were more likely to report lower levels of positive affect on the PANAS: a standard deviation increase in positive emotional expression was associated with an unadjusted 7.6% decrease in self-reported positive affect (P=0.01) and an adjusted 10.0% decrease in self-reported positive affect (P=0.05) after modeling for potential confounders. A standard deviation increase in negative emotional expression was associated with an adjusted 11.3% increase in self-reported negative affect (P=0.04).
Conclusion
The inverse relationship between parents’ positive emotional expression and their self-reported positive affect should remind both researchers and clinicians to be cognizant of the possibilities for emotional miscues, and consequent miscommunication, in the pediatric care setting.
Keywords: Communication, caregivers, chronic disease management, emotion, palliative care
Introduction
Communication between parents and clinicians is widely acknowledged as a crucial component of high-quality care for children with serious pediatric illnesses. Parents rely on this communication in order to understand their child’s medical condition, and can more effectively participate in decision making for their child’s care once they are informed. These interactions occur, however, in a context of high parental stress and often outright distress. In order to improve parent-clinician interactions in these circumstances, clinicians need to understand the strong and seemingly contradictory feelings that parents experience in such situations so that clinicians can help parents participate more actively in shared decision making.1-6
Parents of children with life-threatening illnesses experience heightened positive and negative emotions simultaneously, as they may love and feel proud of their child while at the same time feel sadness and anger about their child’s health prognosis.7,8 Differences among individual parents regarding how they communicate emotions to clinicians (or researchers) are unknown; nevertheless, clinicians on a daily basis make assumptions about parents’ emotional experiences based on a variety of behavioral and interpersonal cues combined with consideration of individual and situational factors. Because these assumptions about parental emotions may not correspond to parents’ subjective emotions, the ensuing quality and effectiveness of communication and palliative care support may suffer.9
Measuring an individual’s emotional state is complex and challenging. Multiple methods have been developed for assessing emotion, including self-report questionnaires, physiological measures, facial measures, and observer ratings. No “gold standard” exists10; each way of measuring emotion likely captures different aspects of a person’s emotional experience and has its associated strengths and weaknesses. Self-report measures are widely used and easy to administer, but these measures assume that respondents have the ability to perceive and name their own emotions, and this ability has been shown to vary substantially among individuals.11,12 Alternatively, recently developed computer-based linguistic word inquiry programs evaluate the verbal and written communication styles of individuals, categorizing words and phrases according to their affective valence as positive or negative and then tallying and compiling individuals’ use of these words and phrases. One such program, the Linguistic Inquiry and Word Count (LIWC), developed by James W. Pennebaker, has been used in studies on emotional expression in adults in treatment for substance abuse,13 women participating in online support groups for breast cancer,14 linguistic styles in children with attention deficit hyperactivity disorder,15 and other psychological research.16-18
When employed along with self-reported affect measures, the LIWC measures of emotional expression may provide additional information regarding how emotions are experienced and communicated by parents of children with serious pediatric illnesses. Whereas prior studies in adult patients with cancer have shown no association between the LIWC measures and self-report of positive and negative emotion,19,20 the LIWC measures were associated with qualitative coders’ ratings.20 Because of this finding, Bantum and colleagues recommend using such measures of emotional expression as a supplement to self-report measures.20 Therefore, in this study, we explore emotion using both the LIWC and a self-report questionnaire to better understand the relationship between these two measures of emotion in a pediatric care context.
Patients and Methods
Sample
All parents were participants in the Decision Making in Pediatric Palliative Care Study at The Children’s Hospital of Philadelphia.7,21 The families of all children receiving both new and existing palliative care consults between October 2006 and July 2008 were screened for eligibility. Parents were eligible to participate if they were English speaking, older than 18 years of age, and if their child was either less than 18 years of age or 18 years of age or older but impaired cognitively and did not make personal medical decisions. Of 88 eligible families screened, 50 families (62.5%) consented to participate and were interviewed. When possible, a second parent was interviewed in addition to the primary parent. All interviews were conducted separately for each parent, and all participants received $25. Enrollment ended when the recruitment goal of 50 families was reached. In total, 73 parents of 50 children participated (i.e., 50 primary parents and 23 additional parents). Although most parents completed the interview and surveys in person, 17 parents (23.3%) participated via telephone and the Internet.
Data Collection
Parents completed several questionnaires and participated in a semi-structured interview about their child and their experiences with medical decision making. All interviews were conducted by the first and third authors. The interview began with the question, “Could you tell me about what has been significant to you about your child’s illness?” and concluded with several open-ended questions about sources of support, religion and spirituality, hope, trust, and feedback on the interview itself. The interviews were audio-recorded and subsequently transcribed. Four parents were missing transcripts because of equipment malfunction during the recording of interviews. Therefore, 69 of 73 parents (95.4%) had transcripts available for analysis. Of these, 62 of 69 (89.9%) parents had complete information regarding self-reported affect.
Main Outcome Measure
Positive and Negative Affect Schedule (PANAS)
The well-validated PANAS22,23 was used to measure parental self-reported affect. The PANAS contains a list of twenty adjectives that correspond to either positive (interested, alert, attentive, excited, enthusiastic, inspired, proud, determined, strong, and active) or negative (distressed, upset, guilty, ashamed, hostile, irritable, nervous, jittery, scared, and afraid) emotions. Parents were asked to rate how much they felt each emotion during the past week using a scale ranging from 1-very slightly to 5-extremely.
Main Predictor Measure
Positive and Negative Emotional Expression
We used LIWC software24 to assess positive and negative emotional expression during the semi-structured interview. The comments of the interviewer were removed from the transcripts prior to analysis. Emotional expression was assessed by the frequency of positive emotion words (e.g., love, nice, sweet; 406 total positive words in the LIWC dictionary) or negative emotion words (e.g., hurt, ugly, nasty; 499 total negative words), divided by the transcript word count.
Parent and Child Demographic and Clinical Characteristics
Parent age was obtained through parental self-report and grouped into the following three categories: 21-34 years, 35-38 years, and 39-66 years. Parent type (Mom, Dad, and other), race (white, black, and other), relationship (married/partnered and other), and education (some high school or high school graduate, some college or college graduate, and some graduate school or graduate school graduate) were also obtained through parental self-report, as was child insurance (private, Medicaid, and low cost/limited/none).
Child age, gender, and diagnosis were obtained from the child’s medical record. The child’s diagnosis was classified according to an established complex chronic conditions coding scheme25,26 into one of the following six categories: neuromuscular, metabolic, malignancy, congenital, respiratory, and gastrointestinal.
The child’s illness trajectory, an established parent-reported measure of the child’s health status,7 was measured as the mean slope of a line plotted connecting the scores over five time points (one year ago, six months ago, one month ago, one week ago, and today) of the parents’ perceptions of the child’s health status (rated on a scale of 1-10); the slope of the resulting line represents the illness trajectory rate.
Statistical Analysis
The analysis aimed, a priori, to evaluate the relationship between positive and negative emotional expression (LIWC) and self-reported affect (PANAS) and to determine whether the observed association was the result of confounding. We report frequencies and percentages for parent and child characteristics. Univariate linear regression was used to determine the association between parent and child characteristics and positive and negative self-reported affect. We examined the effect of LIWC on PANAS measures in two multivariate regression models that account for the clustering of parents within families and provide corrected standard errors. These models also adjusted for observed confounders of the relationship between LIWC and PANAS using the change-in-estimate method described by Greenland.27 This method includes covariates that might be potential confounders into the model in a step-wise fashion and considers variables that change the estimated effect of LIWC on PANAS by 10% (in either direction) to be confounders. The final adjusted model includes LIWC as well as all of the covariates identified as confounders.
To account for scattered missing data for parental age, race, and education, we imputed the missing values using imputation by chained equations using the analysis variables and an indicator variable for each family, to account for clustering of parents within families. To facilitate the interpretation of regression coefficients, positive emotional expression, negative emotional expression, and the illness trajectory measure were centered using z-score transformations. Similarly, self-reported positive and negative affect scores were log transformed so that the β coefficients could be interpreted in the form of percentage change. All analyses were performed in Stata 12.1 (StataCorp LP, College Station, TX).
Results
Our analytic sample consisted of 69 parents from 47 families. Parents participating in the study ranged in age from 21-66 years (mean 37.3 years, standard deviation [SD] 8.1 years). Whereas most parents who participated were mothers (59%), there were 25 (36%) fathers and three (4%) other participants (a stepmother, grandmother, and aunt) (Table 1). Because our results were not impacted by the inclusion of the three “other” parents, we retained them in the analysis. The majority of parents were white (71%), 15% were black, 7% of parents identified themselves as mixed or other, and 7% had an unknown race. Nearly three-quarters (71%) of parents were married, and 68% had at least some college education. Positive and negative self-reported affect did not vary by parent characteristics (Table 1).
Table 1.
Parent Characteristics (n = 69)
| Positive Self-Reported Affect |
Negative Self-Reported Affect |
||||||
|---|---|---|---|---|---|---|---|
| N (%) | Mean | SD | P-value | Mean | SD | P-value | |
| Parent, Age | |||||||
| 21-34y | 23 (33) | 34.6 | 7.4 | Ref | 31.0 | 7.1 | Ref |
| 35-38y | 20 (29) | 36.0 | 8.4 | 0.55 | 27.4 | 12.2 | 0.29 |
| 39-66y | 24 (35) | 34.8 | 7.7 | 0.47 | 25.4 | 9.2 | 0.072 |
| Unknown | 2 (3) | 34.5 | 16.3 | -- | 34.0 | 4.2 | -- |
| Parent, Type | |||||||
| Mom | 41 (59) | 34.9 | 7.6 | Ref | 29.1 | 9.8 | Ref |
| Dad | 25 (36) | 35.8 | 7.9 | 0.73 | 27.8 | 9.5 | 0.87 |
| Othera | 3 (5) | 29.3 | 9.0 | -- | 21.0 | 1.7 | -- |
| Parent, Race | |||||||
| White | 49 (71) | 34.9 | 7.4 | Ref | 27.8 | 9.5 | Ref |
| Black | 10 (15) | 37.9 | 6.7 | 0.25 | 29.6 | 10.5 | 0.62 |
| Other | 5 (7) | 27.2 | 7.5 | -- | 36.7 | 4.5 | -- |
| Unknown | 5 (7) | 37.2 | 10.1 | -- | 24.6 | 9.1 | -- |
| Parent, Relationship | |||||||
| Married/partnered | 49 (71) | 34.3 | 7.5 | 0.39 | 28.6 | 9.3 | 0.50 |
| Other | 20 (29) | 36.5 | 8.4 | 27.2 | 10.1 | ||
| Parent, Education | |||||||
| High School | 13 (19) | 36.6 | 8.4 | Ref | 34.5 | 8.2 | Ref |
| College | 33 (48) | 34.4 | 7.0 | 0.33 | 28.4 | 9.4 | 0.15 |
| Graduate School | 14 (20) | 34.5 | 8.4 | 0.68 | 23.2 | 8.6 | 0.069 |
| Unknown | 9 (13) | 35.3 | 9.6 | -- | 26.6 | 9.1 | 0.30 |
Note: Values were not reported if cell sizes were 5 or less.
Other includes one stepmother, one grandmother, and one aunt.
The majority of children were less than four years of age, with an age range of 0.02 to 24 years (mean 5.4, SD 5.7). Slightly more than half were female (51%), and 49% had Medicaid as their primary insurance. Children had a variety of complex chronic conditions, including neuromuscular (30%), metabolic (26%), malignancies (21%), congenital (15%), respiratory (4%), gastrointestinal (2%), and cardiovascular (2%). Parental positive and negative self-reported affect did not vary by child characteristics except for child age (Table 2). Parents of older children (5-9 years) had a significantly lower mean negative affect score than did parents of children less than one year old (24.3 vs. 31.7, respectively, P= 0.019).
Table 2.
Child Characteristics (n = 47)
| Positive Self-Reported Affect |
Negative Self-Reported Affect |
||||||
|---|---|---|---|---|---|---|---|
| N (%) | Mean | SD | P-value | Mean | SD | P-value | |
| Child, Age | |||||||
| Less than 1 year | 11 (23) | 33.9 | 8.6 | Ref | 31.7 | 6.4 | Ref |
| 1-4 years | 14 (30) | 34.7 | 7.8 | 0.78 | 29.7 | 10.5 | 0.52 |
| 5-9 years | 11 (23) | 34.3 | 8.1 | 0.76 | 24.3 | 8.5 | 0.019 |
| 10-17 years | 9 (19) | 37.2 | 6.7 | 0.26 | 24.5 | 10.9 | 0.057 |
| 18-24 years | 2 (5) | 40 | 1.4 | -- | 38.5 | 4.9 | -- |
| Child, Gender | |||||||
| Female | 24 (51) | 36.0 | 7.4 | Ref | 29.5 | 10.2 | Ref |
| Male | 23 (49) | 33.8 | 8.1 | 0.28 | 27.0 | 8.8 | 0.33 |
| Child, Insurance | |||||||
| Private | 18 (39) | 34.9 | 7.7 | Ref | 27.4 | 8.4 | Ref |
| Medicaid | 23 (49) | 35.8 | 8.2 | 0.66 | 28.3 | 10.8 | 0.80 |
| Low cost/limited/none | 3 (6) | 33.0 | 2.9 | -- | 32.5 | 8.8 | -- |
| Unknown | 3 (6) | 27.5 | 7.8 | 28.0 | 11.5 | ||
| Child, Complex Chronic | |||||||
| Condition Category | |||||||
| Neuromuscular | 14 (30) | 33.8 | 8.3 | Ref | 29.8 | 8.2 | Ref |
| Metabolic | 12 (26) | 35.6 | 8.3 | 0.58 | 28.9 | 10.5 | 0.80 |
| Malignancy | 10 (21) | 35.2 | 7.5 | 0.59 | 31.0 | 8.8 | 0.72 |
| Congenital | 7 (15) | 36.1 | 6.2 | 0.49 | 24.9 | 9.5 | 0.18 |
| Respiratory | 2 (4) | 38.3 | 6.5 | -- | 15.7 | 2.3 | -- |
| Gastrointestinal | 1 (2) | 20 | 0 | -- | 20 | 0 | -- |
| Cardiovascular | 1 (2) | 36.0 | 0 | -- | -- | ||
Note: Values were not reported if cell sizes were less than 5.
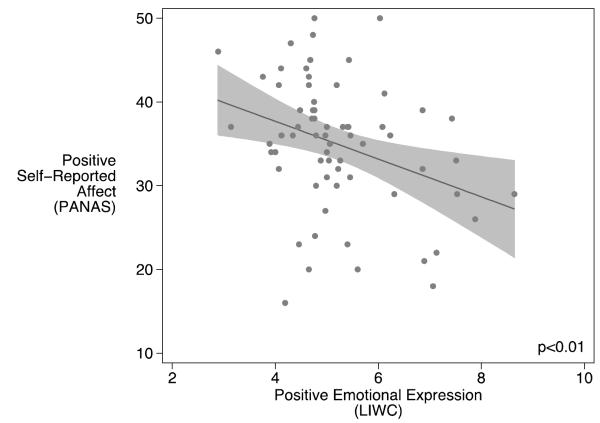
Based on the regression results, parents who demonstrated more positive emotional expression during the semi-structured interview were significantly more likely to report lower levels of positive self-reported affect on the PANAS. A standard deviation increase in positive emotional expression was associated with an unadjusted 7.4% decrease in positive self-reported affect (P=0.015) and an adjusted 7.0% decrease in positive self-reported affect (P=0.057) after modeling for parent age, race, level of education, the child’s insurance, illness trajectory, and whether or not the interview took place over the phone (Table 3).
Table 3.
Relationship Between Positive Emotional Expression and Self-Reported Positive Affect
| N | % Change |
95% CI | P-value | |
|---|---|---|---|---|
| Unadjusted Model | ||||
| Positive Emotional Expression | 69 | −7.4% | −13.0%, −1.8% | 0.02 |
| Adjusted Model | ||||
| Positive Emotional Expression | 69 | −7.0% | −14.6%, −0.5% | 0.057 |
| Parent Age Category, 21-34y | Ref | |||
| Parent Age Category, 35-38y | 8.2% | −11.4%, 27.7% | 0.16 | |
| Parent Age Category, 39-66y | 9.6% | −6.0%, 25.2% | 0.20 | |
| Parent Race, White | Ref | |||
| Parent Race, Black | 2.9% | −15.8%, 21.5% | 0.12 | |
| Parent Race, Other | −18.1 | −46.0%, 9.8% | 0.18 | |
| Parent Education, High School | Ref | |||
| Parent Education, College | −3.5% | −24.9%, 17.9% | 0.30 | |
| Parent Education, Graduate School | −6.6% | −34.4%, 21.2% | 0.20 | |
| Child Insurance, Private | Ref | |||
| Child Insurance, Medicaid | −2.3% | −17.3%, 12.7% | 0.12 | |
| Child Insurance, Low Cost/Limited/None | 5.0% | −16.7%, 26.6% | 0.31 | |
| Illness Trajectory | −2.6% | −11.4%, 6.1% | 0.28 | |
| Phone Interview, In Person | Ref | |||
| Phone Interview, Phone | −2.8% | −17.6%, 12.0% | 0.041 |
Note: Values were not reported if cell sizes were less than 5. Imputed results using N=69 are reported.
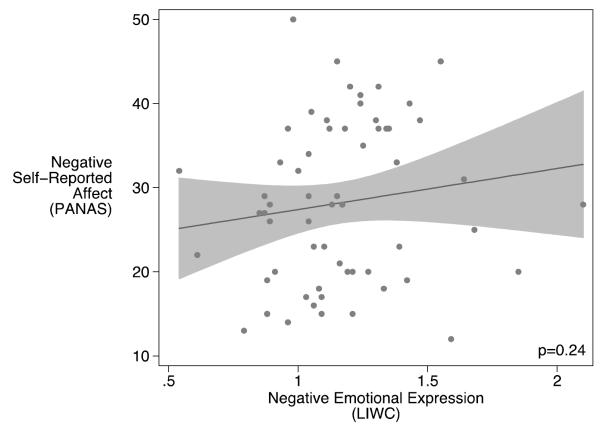
Parents who demonstrated more negative emotional expression during the semi-structured interview were significantly more likely to report higher levels of negative self-reported affect on the PANAS. A standard deviation increase in negative emotional expression was associated with an unadjusted 6.1% increase in negative self-reported affect (P=0.18) and an adjusted 9.4% increase in negative self-reported affect (P=0.036) after adjusting for the same confounders mentioned above (Table 4).
Table 4.
Relationship between Negative Emotional Expression and Self-Reported Negative Affect
| N | % Change |
95% CI | P-value | |
|---|---|---|---|---|
| Unadjusted Model | ||||
| Negative Emotional Expression | 69 | 6.0% | −2.8%, 15.0% | 0.18 |
| Adjusted Model | ||||
| Negative Emotional Expression | 69 | 9.4% | 0.6%, 18.3% | 0.04 |
| Parent Age Category, 21-34y | Ref | |||
| Parent Age Category, 35-38y | −10.6% | −35.6%, 14.4% | 0.24 | |
| Parent Age Category, 39-66y | −14.7% | −35.7%, 6.2% | 0.20 | |
| Parent Race, White | Ref | |||
| Parent Race, Black | −1.8% | −32.7%, 29.0% | 0.90 | |
| Parent Race, Other | 33.9% | −2.8%, 70.5% | 0.42 | |
| Parent Education, High School | Ref | |||
| Parent Education, College | −16.5% | −44.0%, 11.1% | 0.28 | |
| Parent Education, Graduate School | −37.0% | −68.8%, −5.1% | 0.28 | |
| Child Insurance, Private | Ref | |||
| Child Insurance, Medicaid | −5.6% | −27.1%, 16.1% | 0.15 | |
| Child Insurance, Low Cost/Limited/None | 3.2% | −28.0%, 34.3% | 0.28 | |
| Illness Trajectory | 3.6% | −6.0%, 13.1% | 0.12 | |
| Phone Interview, In Person | Ref | |||
| Phone Interview, Phone | −21.8% | −49.6%, 6.1% | 0.21 |
Note: Values were not reported if cell sizes were less than 5.
Imputed results using N=69 are reported.
There were no statistically significant associations observed between positive emotional expression and negative self-reported affect or negative emotional expression and positive self-reported affect. A standard deviation increase in negative emotional expression was associated with an unadjusted 1.7% increase in positive self-reported affect (P=0.51) and an adjusted 2.9% increase in positive self-reported affect (P=0.32) after modeling for parent age, race, level of education, the child’s insurance, illness trajectory, and whether or not the interview took place over the phone. Similarly, a standard deviation increase in positive emotional expression was associated with an unadjusted −0.6% change in negative self-reported affect (P=0.87) and an adjusted 1.5% decrease in negative self-reported affect (P=0.77) after modeling for parent age, race, level of education, the child’s insurance, illness trajectory, and whether or not the interview took place over the phone.
Discussion
Whereas negative emotional expression during a semi-structured interview was positively associated with self-reported negative affect in this sample of parents of children receiving palliative care, positive emotional expression was inversely associated with self-reported positive affect. In other words, parents who exhibited more positive emotional expression during a semi-structured interview were likely to have lower self-reported positive affect. This discrepancy between positive emotional expression and self-report of positive affect may generate communication misunderstandings or challenges in parent-clinician interactions.
What causes this discrepancy? And are parents consciously or unconsciously communicating verbal positive affect in excess of their self-reported positive affect? Four possible theoretical explanations may be applicable to both of these questions. First, parents may be trying to influence their own emotions by speaking more positively when they feel less positive. This would be a form of emotional regulation, whereby speaking positively might serve to augment or intensify positive feelings for the parent.28,29 This form of response or behavior also has been referred to as “deep acting,” whereby a person tries to shape their emotional experience by expressing a particular affect.30 (This is also suggested in the song “Put on a Happy Face” by Adams and Strouse from the musical “Bye Bye Birdie”). Of note – and consistent with our findings – although the sharing of positive emotion is thought to improve mood, the sharing of negative emotion has not been found to impact mood.31 Other research had demonstrated an orthogonal relationship between positive and negative affect, in that the two types of affect are thought to be independent of and do not influence each other.23,32,33 These findings may explain, in part, why different relationships are observed between positive emotional expression and self-reported positive affect, and negative emotional expression and self-reported negative affect (and the lack of association between positive emotional expression and self-reported negative affect, and negative emotional expression and self-reported positive affect).
Second, a parent’s expression of affect may be shaped, wittingly or unwittingly, so as to conform with implicit “emotional display rules”34 that parents perceive to be normative in the social situation of a hospital interview. Although the interviewers encouraged parents to speak freely about their experiences, the experience took place in hospital rooms; parents likely communicated differently with the interviewer than they would with family members or others in their private lives. Similar to employees who must manage their emotions on the job through “surface acting,”30 parents may be accustomed to maintaining a certain level of positivity when interacting with hospital staff. In this situation, parents may be trying to be polite or influence the discussion to create a good impression or improve their access to medical personnel and other material support.
Third, parents who are acting out of love for their child also may want to minimize negative emotions and emphasize positive emotions in their communication with others out of a sense of loyalty and protectiveness to the child.35 In other words, because parents have positive feelings for their child, they may speak more positively about their child’s situation than their self-reported affect would suggest. Conceivably, talking negatively about a child’s medical situation is perceived as a betrayal of trust for some parents. Similar patterns of loyalty have been observed in parents of adolescents with problem behaviors 36 and parents of children and young adults with characteristics of borderline personality disorder.37
Fourth, the results, in part, could be the result of potential bias introduced by the two different time frames for the PANAS (which asks respondents to recall over the past week) and the LIWC assessment (which analyzes only what was said during the interview), which could result in discrepancies in either direction (the prior week could have been emotionally more positive or negative than the time of the interview). Given the nature of scheduling interviews, which occurred at the convenience and wishes of the parent, the time of the interview would not have been in or shortly after a moment of medical crisis; conceivably, then, the parents may have recalled less positive affect during a preceding period of time than what they were experiencing at the time of the interview. Such a mechanism would affect not only metrics of this study, but would also potentially cause discrepant communication of affect in routine clinical communication during family meetings or bedside rounds, which also often are timed so as to avoid moments of medical crisis.
This study had several strengths and limitations. A major strength of this study is that interviews with parents were conducted while their children were still living, and, therefore, the effects of retrospective constructive memory and of the grieving process following the child’s death did not influence the findings. Another strength is that we used an innovative, yet scientifically valid, way of expanding our understanding of emotion through use of the LIWC program, while at the same time contrasting this method with the popular PANAS self-report instrument. The major limitation of this study is that it is an analysis of a cohort study on medical decision making in pediatric palliative care and the sample size may not have been large enough to demonstrate the statistical significance of certain associations. For these reasons, our findings should be generalized with caution, and focused instead on provoking further inquiry about the communication of emotional states by parents (as well as other family members, and by patients) and generating testable hypotheses.
The inverse relationship between positive emotional expression and self-reported positive affect in this population should remind both researchers and clinicians to be cognizant of the possibilities for emotional miscues, and consequent miscommunication, in the pediatric care setting. Future research should explore whether the discrepancy between positive emotional expression and positive self-reported affect are evident not only in spoken words but also in facial expressions and body language; whether such discrepancies occur for other emotional states and in other samples of subjects; whether clinicians can detect emotional state discrepancies in routine clinical practice; and the impact of these discrepancies on communication and decision making, and if found to be problematic, how to address these discrepancies.
Fig. 1.
The relationship between positive emotional expression and positive self-reported affect, with 95% confidence interval.
Fig. 2.
The relationship between negative emotional expression and negative self-reported affect, with 95% confidence interval.
Acknowledgments
The study was funded by the National Institute of Nursing Research (NR010026). The funding organization had no role in the design of the study beyond the critique offered by the peer-review process; and had no role in the conduct of the study, including the collection, analysis, and preparation of the data or the drafting, editing, review, or approval of the manuscript.
Footnotes
Disclosures The authors declare that no competing financial interests exist.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Klick JC, Hauer J. Pediatric palliative care. Curr Probl Pediatr Adolesc Health Care. 2010;40(6):120–151. doi: 10.1016/j.cppeds.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Feudtner C. Collaborative communication in pediatric palliative care: a foundation for problem-solving and decision-making. Pediatr Clin North Am. 2007;54(5):583–607. doi: 10.1016/j.pcl.2007.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byrne M, Tresgallo M, Saroyan J, et al. Qualitative analysis of consults by a pediatric advanced care team during its first year of service. Am J Hosp Palliat Care. 2011;28(2):109–117. doi: 10.1177/1049909110376626. [DOI] [PubMed] [Google Scholar]
- 4.Gordon C, Barton E, Meert KL, et al. Accounting for medical communication: parents’ perceptions of communicative roles and responsibilities in the pediatric intensive care unit. Commun Med. 2009;6(2):177–188. [PMC free article] [PubMed] [Google Scholar]
- 5.Meert KL, Eggly S, Pollack M, et al. Parents’ perspectives on physician-parent communication near the time of a child’s death in the pediatric intensive care unit. Pediatr Crit Care Med. 2008;9(1):2–7. doi: 10.1097/01.PCC.0000298644.13882.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michelson KN, Emanuel L, Carter A, et al. Pediatric intensive care unit family conferences: one mode of communication for discussing end-of-life care decisions. Pediatr Crit Care Med. 2011;12(6):e336–343. doi: 10.1097/PCC.0b013e3182192a98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feudtner C, Carroll KW, Hexem KR, et al. Parental Hopeful Patterns of Thinking, Emotions, and Pediatric Palliative Care Decision Making. Arch Pediatr Adolesc Med. 2010;164(9):831–839. doi: 10.1001/archpediatrics.2010.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feudtner C. Grief-love: contradictions in the lives of fathers of children with disabilities. Arch Pediatr Adolesc Med. 2002;156(7):643. doi: 10.1001/archpedi.156.7.643. [DOI] [PubMed] [Google Scholar]
- 9.Janvier A, Okah F, Farlow B, Lantos JD. An infant with trisomy 18 and a ventricular septal defect. Pediatrics. 2011;127(4):754–759. doi: 10.1542/peds.2010-1971. [DOI] [PubMed] [Google Scholar]
- 10.Mauss IB, Robinson MD. Measures of emotion: a review. Cogn Emot. 2009;23(2):209–237. doi: 10.1080/02699930802204677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salovey P, Mayer J, Caruso D. The positive psychology of emotional intelligence. In: Synder C, Lopez S, editors. Handbook of positive psychology. Oxford University Press; New York: 2005. pp. 159–171. [Google Scholar]
- 12.Larsen RJ, Fredrickson BL. Measurement issues in emotion research. In: Kahneman D, Diener E, Schwarz N, editors. Well-being: The foundations of hedonic psychology. Russell Sage Foundation; New York: 1999. pp. 40–60. [Google Scholar]
- 13.Liehr P, Marcus MT, Carroll D, et al. Linguistic analysis to assess the effect of a mindfulness intervention on self-change for adults in substance use recovery. Subst Abus. 2010;31(2):79–85. doi: 10.1080/08897071003641271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han JY, Shaw BR, Hawkins RP, et al. Expressing positive emotions within online support groups by women with breast cancer. J Health Psychol. 2008;13(8):1002–1007. doi: 10.1177/1359105308097963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim K. Distinctive linguistic styles in children with ADHD. Psychol Rep. 2009;105(2):365–371. doi: 10.2466/PR0.105.2.365-371. [DOI] [PubMed] [Google Scholar]
- 16.Pennebaker JW, Mayne TJ, Francis ME. Linguistic predictors of adaptive bereavement. J Pers Soc Psychol. 1997;72(4):863–871. doi: 10.1037//0022-3514.72.4.863. [DOI] [PubMed] [Google Scholar]
- 17.Pennebaker JW, King LA. Linguistic styles: language use as an individual difference. J Pers Soc Psychol. 1999;77(6):1296–1312. doi: 10.1037//0022-3514.77.6.1296. [DOI] [PubMed] [Google Scholar]
- 18.Rosenberg HJ, Rosenberg SD, Ernstoff MS, et al. Expressive disclosure and health outcomes in a prostate cancer population. Int J Psychiatry Med. 2002;32(1):37–53. doi: 10.2190/AGPF-VB1G-U82E-AE8C. [DOI] [PubMed] [Google Scholar]
- 19.Owen JE, Giese-Davis J, Cordova M, et al. Self-report and linguistic indicators of emotional expression in narratives as predictors of adjustment to cancer. J Behav Med. 2006;29(4):335–345. doi: 10.1007/s10865-006-9061-8. [DOI] [PubMed] [Google Scholar]
- 20.Bantum EO, Owen JE. Evaluating the validity of computerized content analysis programs for identification of emotional expression in cancer narratives. Psychol Assess. 2009;21(1):79–88. doi: 10.1037/a0014643. [DOI] [PubMed] [Google Scholar]
- 21.Hexem KR, Mollen CJ, Carroll K, Lanctot DA, Feudtner C. How parents of children receiving pediatric palliative care use religion, spirituality, or life philosophy in tough times. J Palliat Med. 2011;14(1):39–44. doi: 10.1089/jpm.2010.0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 23.Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol. 2004;43:245–265. doi: 10.1348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- 24.Linguistic inquiry and word count (LIWC2007) [computer program] LIWC.net; Austin, TX: 2007. [Google Scholar]
- 25.Feudtner C, Feinstein JA, Satchell M, Zhao H, Kang TI. Shifting place of death among children with complex chronic conditions in the United States, 1989-2003. JAMA. 2007;297(24):2725–2732. doi: 10.1001/jama.297.24.2725. [DOI] [PubMed] [Google Scholar]
- 26.Feudtner C, Levin JE, Srivastava R, et al. How well can hospital readmission be predicted in a cohort of hospitalized children? A retrospective, multicenter study. Pediatrics. 2009;123(1):286–293. doi: 10.1542/peds.2007-3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79(3):340–349. doi: 10.2105/ajph.79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gross JJ, Thompson RA. Emotion regulation: conceptual foundations. In: Gross JJ, editor. Handbook of emotion regulation. Guilford Press; New York: 2007. pp. 3–24. [Google Scholar]
- 29.Langston CA. Capitalizing on and coping with daily-life events: expressive responses to positive events. J Pers Soc Psychol. 1994;67(6):1112–1125. [Google Scholar]
- 30.Hochschild AR. The managed heart: commercialization of human feeling. University of California Press; Berkeley and Los Angeles, CA: 2003. [Google Scholar]
- 31.Rimé B. Interpersonal emotion regulation. In: Gross JJ, editor. Handbook of emotion regulation. Guilford Press; New York: 2007. [Google Scholar]
- 32.Tellegen A, Watson D, Clark LA. On the dimensional and hierarchical structure of affect. Psychol Sci. 1999;10(4):297–303. [Google Scholar]
- 33.Diener E, Smith H, Fujita F. The personality structure of affect. J Pers Soc Psychol. 1995;69(1):130–141. [Google Scholar]
- 34.Diefendorff JM, Erickson RJ, Grandey AA, Dahling JJ. Emotional display rules as work unit norms: a multilevel analysis of emotional labor among nurses. J Occup Health Psychol. 2011;16(2):170–186. doi: 10.1037/a0021725. [DOI] [PubMed] [Google Scholar]
- 35.Boszormenyi-Nagi I, Spark GM. Invisible loyalties. Harper & Row; Hagerstown, MD: 1973. [Google Scholar]
- 36.Delsing MJM, van Aken MAG, Oud JHL, De Bruyn EE, Scholte RHJ. Family loyalty and adolescent problem behavior: the validity of the family group effect. J Res Adolesc. 2005;15(2):127–150. [Google Scholar]
- 37.Feldman RB, Guttman HA. Families of borderline patients: literal-minded parents, borderline parents, and parental protectiveness. Am J Psychiatry. 1984;141(11):1392–1396. doi: 10.1176/ajp.141.11.1392. [DOI] [PubMed] [Google Scholar]