Abstract
Telemedicine is the practice of healthcare using audio, video, and data communications. The aim of this study was to determine the perceptions of health professionals at hospitals adopting and not adopting telemedicine on its benefits and challenges, and their willingness to use it. The study was conducted at one hospital not adopting telemedicine and three hospitals adopting telemedicine. It was a cross-sectional descriptive study, and the target population was health professionals. Data collection methods included two paper-based questionnaires. Nonparametric statistical analysis and descriptive statistics were used. The study concluded that although telemedicine is promising and the Ministry of Health in Saudi Arabia has allocated a huge budget for e-health, the telemedicine modalities used were very limited. The percentage of adoption of telemedicine by health professionals was low in comparison to the high interest of nonadopters. Nonadopters’ perception of benefits was higher than that of adopters. The most frequently cited benefits among adopters were improving the quality of care, enhancing access to healthcare, and providing patient care and management. However, adopters’ perceptions were low for other benefits such as easy use of the network, the use of store-and-forward telemedicine, and the ability to follow up after face-to-face contacts. The greatest barrier as perceived by health providers was the lack of knowledge about telemedicine. Dissemination of information about telemedicine and proper training of health professionals on its use are recommended.
Keywords: telemedicine, perception, health providers, Saudi Arabia
Introduction
Telemedicine is the use of medical information exchanged from one site to another via electronic communications to improve patients’ health status.1 The World Health Organization (WHO) defines telemedicine as “the delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing health of individuals and their communities.”2 The Institute of Medicine defines telemedicine as “the use of electronic information and communications technologies to provide and support health care when distance separates the participants.”3
Telemedicine applications vary greatly and can be divided into three major categories. The first is patient monitoring or home care that enables medical professionals to monitor patients remotely using various technological devices, such as blood pressure monitors. It is primarily used for managing chronic diseases such as heart disease, diabetes mellitus, and asthma. The second category consists of interactive or real-time applications that use technology for online interaction between participants. These include teleconsultation, videoconferencing, telesurgery, and similar applications. The third category includes store-and-forward applications that use noninteractive technology. This category involves acquiring medical data (such as medical images, biosignals, lab results, etc.) and then transmitting this data to a doctor or medical specialist at a suitable time for assessment, as in teleradiology and telepathology.4, 5, 6
According to the Yale Telemedicine Center in a 1995 report, “Well-developed telemedicine programs have been around [in the United States] since the 1960's, but telemedicine became a hot new concept only very recently when it was evident that health care reform was underway. There were 10 telemedicine programs in 1992, 20 in 1993, and it has been reported that in 1995–96 most US hospitals plan to implement some form of telemedicine program for clinical and/or administrative purposes. In the Yale Telemedicine Center there are a number of current and pending telemedicine projects at the School of Medicine: the Saudi-US Universities Project (SUSUP), the NASA Spacebridge Project, and other projects connecting Yale to other hospitals in Connecticut and nationwide.”7
A website promoting telemedicine in India states that “providing health care services via telemedicine offers many advantages. It can make specialty care more accessible to underserved rural and urban populations. Video consultations from a rural clinic to a specialist can [alleviate] prohibitive travel and associated costs for patients. Video conferencing also opens up new possibilities for continuing education or training for isolated or rural health practitioners, who may not be able to leave a rural practice to take part in professional meetings or educational opportunities.”8 Teleradiology and telepathology allow medical services to be delivered across vast distances and across national and international boundaries.9 In addition, telemedicine improves access to information and services, provides care not previously deliverable, improves quality control in screening programs, and reduces healthcare costs.10
According to one review, “although telemedicine clearly has a wide range of potential benefits, it has also some disadvantages. The main ones that can be envisaged are: a breakdown in the relationship between health professional and patient; a breakdown in the relationship between health professionals; issues concerning the quality of health information; and organizational and bureaucratic difficulties. On balance, the benefits of telemedicine are substantial, assuming that more research will reduce or eliminate the obvious drawbacks.”11
On the other hand, there are several barriers to the practice of telemedicine. These barriers “were grouped in four areas: technological, organizational, human and economic. The main barriers identified were changes in the healthcare model caused by telemedicine, problems with strategic alignment, resistance to change in the (re)definition of roles, responsibilities and new skills, and lack of a business model that incorporates telemedicine in the services portfolio to ensure its sustainability.”12 Other barriers include licensing and costs for technology.13
In a vast country like Saudi Arabia, access to healthcare services in remote and rural areas is of prime importance. Also, the Ministry of Health in Saudi Arabia faces the difficult challenge of providing high-quality care to the entire population and improving access to healthcare services. A national strategic plan therefore stressed the importance of adopting a national telemedicine network.14
The e-Health Center in the King Faisal Specialist Hospital & Research Centre (KFSH&RC) in Riyadh was established in 1993 by a royal decree. The hospital is considered the highest tertiary care institution in the Middle East, and the e-Health Center takes responsibility for helping it accomplish its mission of providing high-quality care for every citizen in Saudi Arabia. The center utilizes fiberoptics and international videoconferencing via Saudi Telecommunication Company (STC) with a view to facilitating access to medical consultations and disseminating healthcare educational activities. Moreover, the National Telemedicine Network has increased from 5 to 22 centers, and 5 more are under study or in the process of implementation.15, 16, 17
Gap in Knowledge
To the researchers’ knowledge, no studies have been conducted in Saudi Arabia assessing the health professionals’ perceptions regarding the benefits and challenges of telemedicine. Also, no studies have been carried out to assess health professionals’ willingness to use telemedicine.
Objectives
The project had the following objectives:
Determine the willingness of healthcare professionals in four facilities (three hospitals adopting telemedicine and one hospital not adopting telemedicine) in the Eastern Province of Saudi Arabia to use telemedicine technologies.
Determine the perceptions of healthcare professionals about the benefits and challenges of telemedicine usage in different healthcare facilities (three hospitals adopting telemedicine and one hospital not adopting telemedicine) in the Eastern Province of Saudi Arabia.
Methods
Study Setting
The study was conducted at the following settings:
King Fahd Hospital of the University (KFHU) in Al-Khobar, Eastern Province, Saudi Arabia, which represented a health facility not adopting telemedicine.
Dammam Central Hospital (DCH), a health facility adopting telemedicine, in Dammam, Eastern Province, Saudi Arabia, and connected with KFSH&RC in Riyadh.
Qatif Central Hospital (QCH) in Qatif, which is adopting telemedicine and is connected with KFSH&RC in Riyadh.
Arabian American Oil Company (ARAMCO) hospital in Dhran, which is adopting teleradiology.
Study Design
The study is a cross-sectional descriptive study.
Target Population and Sample Size
Healthcare professionals (physicians, nurses, radiologists, pathologists, technicians, etc.) at different study settings were included in the study. They were classified as adopters and nonadopters as follows:
Nonadopters: This category includes professionals at KFHU in Al-Khobar. Participants totaled 252 for a response rate of 56 percent (the questionnaire was distributed to 450 healthcare professionals).
- Adopters: This category included professionals at three hospitals: DCH, QCH, and ARAMCO. Participants totaled 144 for an overall response rate of 57.6 percent (the questionnaire was distributed to 250 healthcare professionals). Adopters included the following:
- DCH: Participants totaled 70 for a response rate of 70 percent (the questionnaire was distributed to 100 healthcare professionals).
- QCH: Participants totaled 54 for a response rate of 54 percent (the questionnaire was distributed to 100 healthcare professionals).
- ARAMCO: Participants totaled 20 for a response rate of 40 percent (the questionnaire was distributed to 50 healthcare professionals).
Data Collection Technique and Tools
Researchers intended to use two web-based questionnaires. However, great difficulty was encountered in collecting the e-mail addresses of the health professionals. Accordingly, two paper-based questionnaires were designed, distributed to the healthcare professionals, and collected after four weeks (May 2011). The first questionnaire was designed specifically for KFHU (the hospital not adopting telemedicine). The survey collected data regarding demographic and professional characteristics of the healthcare providers, their perceptions on the benefits and challenges of telemedicine, and their willingness to use telemedicine technology. (See Appendix A). The second questionnaire was designed for the hospitals adopting telemedicine (DCH, QCH, and ARAMCO). This survey also collected data regarding demographic and professional characteristics of healthcare providers, their perceptions on the benefits and challenges of telemedicine, and their willingness to adopt telemedicine. (See Appendix B).
A Likert scale was used on both questionnaires to determine the benefits of adopting telemedicine as perceived by health professionals. It ranged from 1 (strongly disagree) to 4 (strongly agree).
Ethical Consideration
An approval from the committee of research ethics of Dammam University was obtained and submitted to all study settings.
Data Analysis
Nonparametric statistical analysis was performed using SPSS version 19. Descriptive statistics were used in the form of frequencies and percentage for categorical variables and mean and standard deviation for continuous variables. The chi-square test was performed to measure the association between some of the variables under study. The Kruskal-Wallis test was conducted to assess any significant statistical differences among the perceptions of more than two groups. Statistical significance between variables of p ≤ .05 was used.
Inclusion Criteria
Healthcare professionals willing to participate in the study and working in the study settings were included in the study. In hospitals adopting telemedicine, only those healthcare providers adopting telemedicine were included.
Exclusion Criteria
In hospitals adopting telemedicine, healthcare providers not adopting telemedicine were excluded from the study.
Results
Table 1 shows that majority of participants at KFHU and at hospitals adopting telemedicine were male (57 percent and 67 percent respectively), with mean age of 37 ± 11 years and 40 ± 9 years respectively, and were of Saudi nationality (52 percent each). Most commonly, they had less than 10 years of experience (49 percent and 42 percent respectively). Regarding the profession of nonadopters, general physicians represented 26 percent. Other professions, including graduates in applied medical sciences, nurses, lab technicians, and medical students/interns, represented 30 percent. For adopters, general physicians accounted for 15 percent, and other professions represented 27 percent.
Table 1.
Profile of Healthcare Providers at Hospitals Adopting and Not Adopting Telemedicine
| Characteristics of Healthcare Providers | Not Adopting Telemedicine (n = 252) | Adopting Telemedicine (n = 144) | ||
|---|---|---|---|---|
| Number | % | Number | % | |
| Gender | ||||
| Male | 143 | 57 | 97 | 67 |
| Female | 109 | 43 | 47 | 33 |
| Age in years | Mean ± SD = 37 ± 11 | Mean ± SD = 40 ± 9 | ||
| <30 | 86 | 34 | 28 | 19 |
| 30–50 | 135 | 54 | 99 | 69 |
| >50 | 31 | 12 | 17 | 12 |
| Nationality | ||||
| Saudi | 132 | 52 | 75 | 52 |
| Non-Saudi | 120 | 48 | 69 | 48 |
| Profession | ||||
| General physician | 65 | 26 | 21 | 15 |
| Specialist | 60 | 24 | 36 | 25 |
| Consultant | 51 | 20 | 48 | 33 |
| Othera | 76 | 30 | 39 | 27 |
| Years of experience | ||||
| <10 | 124 | 49 | 61 | 42 |
| 10–20 | 95 | 38 | 52 | 36 |
| >20 | 33 | 13 | 31 | 22 |
Graduates in applied medical sciences, nurses, lab technicians, and medical students/interns.
Table 2 shows that there was no statistically significant association between the extent of KFHU respondents’ interest in knowing about telemedicine and any of the demographic variables. The majority of respondents (88.5 percent), regardless of demographic characteristics, showed an interest in knowing about telemedicine.
Table 2.
Distribution of Healthcare Providers Not Adopting Telemedicine According to Their Interest in Knowing about Telemedicine
| Characteristics of Healthcare Providers | Interest in Knowing about Telemedicine (n = 252) | |||||
|---|---|---|---|---|---|---|
| Yes (n = 223) | No (n = 29) | Chisquare | p-value | |||
| Number | % | Number | % | |||
| Age in years | ||||||
| <30 | 78 | 91 | 8 | 9 | .626 | .731 |
| 30 to 50 | 118 | 87 | 17 | 13 | ||
| >50 | 27 | 87 | 4 | 13 | ||
| Gender | ||||||
| Male | 130 | 91 | 13 | 9 | 1.897 | .168 |
| Female | 93 | 85 | 16 | 15 | ||
| Nationality | ||||||
| Saudi | 116 | 88 | 16 | 12 | .102 | .749 |
| Non-Saudi | 107 | 89 | 13 | 11 | ||
| Profession | ||||||
| General physician | 60 | 92 | 5 | 8 | 6.156 | .104 |
| Specialist | 48 | 80 | 12 | 20 | ||
| Consultant | 45 | 88 | 6 | 12 | ||
| Othera | 70 | 92 | 6 | 8 | ||
| Years of experience | ||||||
| <10 years | 111 | 90 | 13 | 11 | .258 | .879 |
| 10–20 years | 83 | 87 | 12 | 13 | ||
| >20 years | 29 | 88 | 4 | 12 | ||
Graduates in applied medical sciences, nurses, lab technicians, and medical students/interns.
Table 3 indicates that there was no statistically significant association between the extent of KFHU respondents’ interest in implementing telemedicine and any of the demographic variables. The majority of respondents (79 percent), regardless of demographic characteristics, showed interest in implementing telemedicine at KFHU.
Table 3.
Distribution of Healthcare Providers Not Adopting Telemedicine According to Their Interest in Implementing Telemedicine
| Characteristics of Healthcare Providers | Interest in Implementing Telemedicine (n = 252) | |||||
|---|---|---|---|---|---|---|
| Yes (n = 199) | No (n = 53) | Chi-square | p-value | |||
| Number | % | Number | % | |||
| Age in years | ||||||
| <30 | 66 | 77 | 20 | 23 | .712 | .701 |
| 30 to 50 | 107 | 79 | 28 | 21 | ||
| >50 | 26 | 84 | 5 | 16 | ||
| Gender | ||||||
| Male | 111 | 78 | 32 | 22 | .361 | .548 |
| Female | 88 | 81 | 21 | 19 | ||
| Nationality | ||||||
| Saudi | 102 | 77 | 30 | 23 | .480 | .489 |
| Non-Saudi | 97 | 81 | 23 | 19 | ||
| Profession | ||||||
| General physician | 50 | 77 | 15 | 23 | 2.076 | .557 |
| Specialist | 46 | 77 | 14 | 23 | ||
| Consultant | 44 | 86 | 7 | 14 | ||
| Othera | 59 | 78 | 17 | 22 | ||
| Years of experience | ||||||
| <10 | 93 | 75 | 31 | 25 | 2.426 | .297 |
| 10–20 | 78 | 82 | 17 | 18 | ||
| >20 | 28 | 85 | 5 | 15 | ||
Graduates in applied medical sciences, nurses, lab technicians, and medical students/interns.
Table 4 demonstrates that 33.3 percent of health professionals at hospitals adopting telemedicine were actually implementing telemedicine and that there were statistically significant associations between actual implementation or usage of telemedicine at these hospitals with profession (p = .000) and years of experience (p = .009). The greatest implementation rates were among consultants (56 percent) and those with more than 20 years of experience (48 percent).
Table 4.
Distribution of Healthcare Providers Regarding Their Actual Implementation of Telemedicine at Hospitals Adopting Telemedicine
| Characteristics of Healthcare Providers | Actual Implementation of Telemedicine at Hospitals Adopting Telemedicine (n = 144) | |||||
|---|---|---|---|---|---|---|
| Yes (n = 48) | No (n = 96 | Chi-square | p-value | |||
| Number | % | Number | % | |||
| Age in years | ||||||
| <30 | 7 | 25 | 21 | 75 | 2.31 | .314 |
| 30 to 50 | 33 | 33 | 66 | 67 | ||
| >50 | 8 | 47 | 9 | 53 | ||
| Gender | ||||||
| Male | 36 | 37 | 61 | 63 | 1.91 | .167 |
| Female | 12 | 26 | 35 | 74 | ||
| Nationality | ||||||
| Saudi | 26 | 35 | 49 | 65 | .125 | .723 |
| Non-Saudi | 22 | 32 | 47 | 68 | ||
| Profession | ||||||
| General physician | 4 | 19 | 17 | 81 | 17.9 | .000 |
| Specialist | 10 | 28 | 26 | 72 | ||
| Consultant | 27 | 56 | 21 | 44 | ||
| Othera | 7 | 18 | 32 | 82 | ||
| Years of experience | ||||||
| <10 | 12 | 20 | 49 | 80 | 9.44 | .009 |
| 10–20 | 21 | 40 | 31 | 60 | ||
| >20 | 15 | 48 | 16 | 52 | ||
Graduates in applied medical sciences, nurses, lab technicians, and medical students/interns.
Table 5 shows statistically significant associations between attendance at teleconferences with facility (p = .000), age (p = .008), profession (p = .010), and years of experience (p = .005). Among participants at hospitals adopting telemedicine, the greatest rates of teleconference attendance were as follows: 85 percent of participants who worked at ARAMCO, 82.4 percent of participants older than age 50, 87.5 percent of participants who were consultants, and 83.9 percent of participants who had more than 20 years of experience attended teleconferences.
Table 5.
Distribution of Healthcare Providers Attending Teleconferences at Hospitals Adopting Telemedicine
| Characteristics of Healthcare Providers | Teleconference Attendance (n = 144) | Chis-quare | p-value | |||
|---|---|---|---|---|---|---|
| Yes (n = 101) | No (n = 43) | |||||
| Number | % | Number | % | |||
| Facility | ||||||
| QCH | 58 | 82.9 | 12 | 17.1 | 19.984 | .000 |
| ARAMCO | 17 | 85.0 | 3 | 15.0 | ||
| DCH | 26 | 48.1 | 28 | 51.9 | ||
| Age in years | ||||||
| <30 | 13 | 46.4 | 15 | 53.6 | 9.730 | .008 |
| 30 to 50 | 74 | 74.7 | 25 | 25.3 | ||
| >50 | 14 | 82.4 | 3 | 17.6 | ||
| Gender | ||||||
| Male | 68 | 70.1 | 29 | 29.9 | 1.003 | .989 |
| Female | 33 | 70.2 | 14 | 29.8 | ||
| Nationality | ||||||
| Saudi | 57 | 76.0 | 18 | 24.0 | 2.567 | .109 |
| Non-Saudi | 44 | 63.8 | 25 | 36.2 | ||
| Profession | ||||||
| General physician | 13 | 61.9 | 8 | 38.1 | 11.304 | .010 |
| Specialist | 24 | 66.7 | 12 | 33.3 | ||
| Consultant | 42 | 87.5 | 6 | 12.5 | ||
| Othera | 22 | 56.4 | 17 | 43.6 | ||
| Years of experience | ||||||
| <10 | 34 | 55.7 | 27 | 44.3 | 10.714 | .005 |
| 10–20 | 41 | 78.8 | 11 | 21.2 | ||
| >20 | 26 | 83.9 | 5 | 16.1 | ||
Graduates in applied medical sciences, nurses, lab technicians, and medical students/interns.
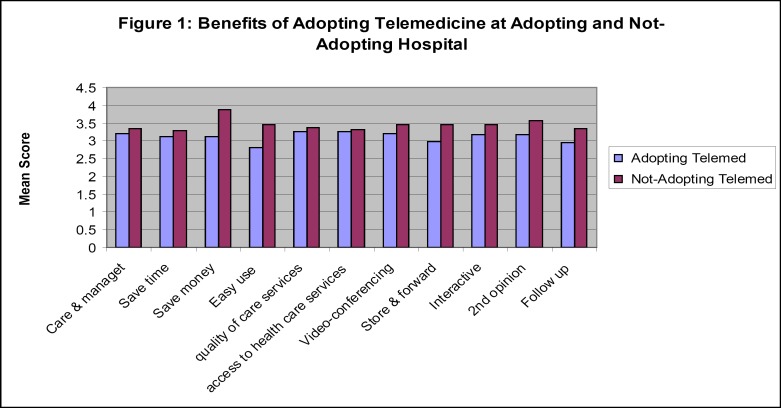
Table 6 shows that healthcare providers at hospitals not adopting telemedicine perceived that adopting telemedicine was beneficial (mean score of 3.30 or higher for all benefits). Table 7 shows that participants at hospitals adopting telemedicine had a mean score of more than 3 for all benefits of telemedicine except easy use of network (2.8), store-and-forward telemedicine (2.97), and follow-up after face-to-face contacts (2.96).
Table 6.
Perceptions of Healthcare Providers Not Adopting Telemedicine on Benefits of Telemedicine (n = 252)
| Benefits of Adopting Telemedicine | Mean | SD |
|---|---|---|
| Provides patient care and management | 3.36 | .711 |
| Saves time | 3.30 | .835 |
| Saves money | 3.88 | .992 |
| Easy use of network | 3.45 | 1.034 |
| Improves quality of care services | 3.37 | .735 |
| Enhances access to health care services | 3.33 | .682 |
| Videoconferencing is very beneficial. | 3.45 | .744 |
| Store-and-forward telemedicine is beneficial. | 3.46 | .926 |
| Interactive telemedicine, i.e., teleconsultation, tele-ICU, teleconferences, etc., is substantial. | 3.45 | .875 |
| Second opinion is important. | 3.58 | .872 |
| Follow-up after face-to-face contact is beneficial. | 3.36 | .847 |
Table 7.
Perception of Healthcare Providers on Benefits of Telemedicine at Hospitals Adopting Telemedicine (n = 144)
| Benefits of Adopting Telemedicine | Mean | SD |
|---|---|---|
| Provides patient care and management | 3.22 | .671 |
| Saves time | 3.13 | .650 |
| Saves money | 3.11 | .616 |
| Easy use of network | 2.80 | .643 |
| Improves quality of care services | 3.26 | .612 |
| Enhances access to healthcare services | 3.26 | .626 |
| Videoconferencing is very beneficial. | 3.22 | .681 |
| Store-and-forward telemedicine is beneficial. | 2.97 | .679 |
| Interactive telemedicine, i.e., teleconsultation, tele-ICU, teleconferences, etc., is substantial. | 3.19 | .679 |
| Second opinion is important. | 3.19 | .672 |
| Follow-up after face-to-face contact is beneficial. | 2.96 | .728 |
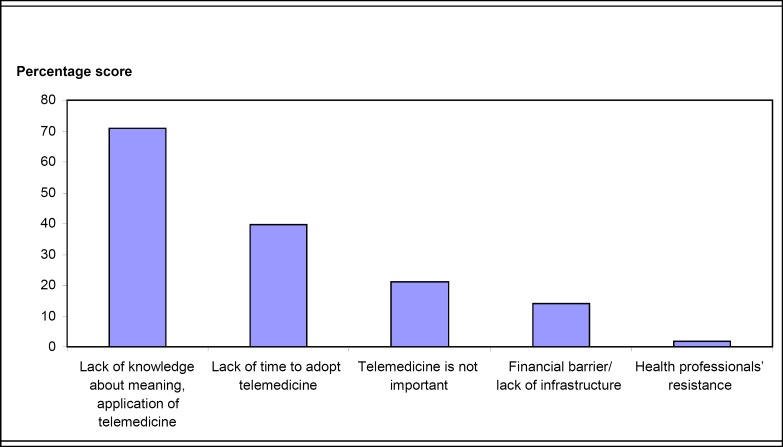
Table 8 shows that the barrier most commonly perceived by healthcare providers at hospitals not adopting telemedicine was lack of knowledge about the meaning of telemedicine and its applications, types, and benefits (71 percent), followed by lack of time to adopt telemedicine (39.7 percent) and then lack of importance of telemedicine (21 percent).
Table 8.
Perceptions of Healthcare Providers at Hospitals Not Adopting Telemedicine on the Barriers/Challenges to the Use of Telemedicine (n = 252)
| Perceived Barriers/Challenges | Numbera | % |
|---|---|---|
| Lack of knowledge about meaning of telemedicine and its applications/types/benefits, etc. | 179 | 71.0 |
| Lack of time to adopt telemedicine | 100 | 39.7 |
| Telemedicine is not important. | 53 | 21.0 |
| Financial barrier/lack of infrastructure | 35 | 13.9 |
| Health professionals’ resistance | 4 | 1.6 |
Some respondents mentioned more than one barrier.
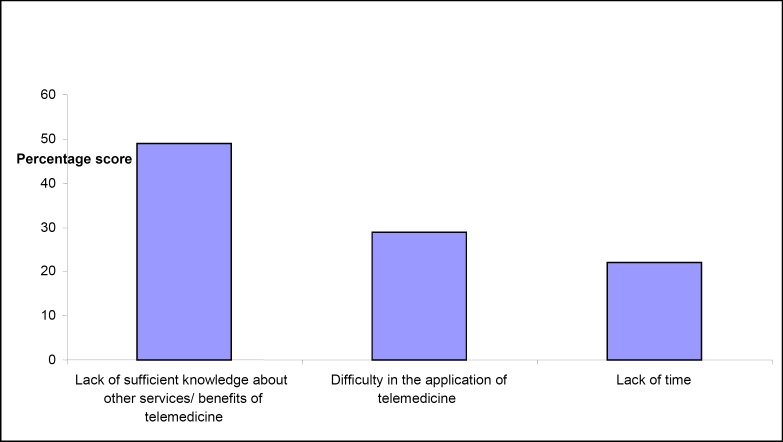
Table 9 demonstrates that barriers experienced by healthcare professionals at hospitals adopting telemedicine were lack of sufficient knowledge about other services/benefits of telemedicine (49 percent), followed by difficulty in the application of telemedicine (29 percent) and then lack of time to adopt telemedicine (22 percent).
Table 9.
Perception of Healthcare Providers at Hospitals Adopting Telemedicine on the Barriers/Challenges to the Use of Telemedicine (n = 144)
| Perceived Barriers/Challenges | Number | % |
|---|---|---|
| Lack of sufficient knowledge about other services/benefits of telemedicine | 71 | 49 |
| Difficulty in the application of telemedicine | 42 | 29 |
| Lack of time to adopt telemedicine | 31 | 22 |
Discussion
Willingness of Healthcare Professionals to Use Telemedicine Technologies
“Telemedicine is the practice of medicine at a distance … where patient and healthcare worker are in different places, and where the interaction may concern diagnosis, treatment/management, or education. Telemedicine deserves consideration because of the real needs of developing countries for healthcare access.”18 Although telemedicine has existed in Saudi Arabia since 1993,19 no studies have been carried out to determine healthcare providers’ perceptions of the benefits and challenges of telemedicine or their willingness to use it. “Feedback from service users [provides] insight into opportunities for improvement so that performance can be optimised.”20
Results of the present study revealed that the majority of healthcare professionals in KFHU were interested in knowing about telemedicine (88.5 percent, Table 2) and in implementing telemedicine technology (79 percent, Table 3) regardless of their demographic parameters. This was consistent with the results of Chismar and Wiley-Patton, which showed the importance of the perception of usefulness by physicians for their adoption and use of information technologies, particularly for clinical tasks.21 The findings were also consistent with the results of another study, conducted in Lagos, Nigeria, in which 78.1 percent of health workers indicated their willingness to adopt telemedicine in healthcare delivery if available and when given appropriate training on its usage.22
In hospitals adopting telemedicine, it was found that only 33.3 percent of health professionals were actually implementing telemedicine (Table 4). In comparison, in Western Australia, 73 percent of survey respondents in healthcare facilities were using telemedicine.23 Men had a higher rate of telemedicine adoption than women (37 percent and 26 percent respectively, Table 4). In Milan, Italy, 80 percent of men were telemedicine adopters,24 and in Hong Kong, “male physicians seemed to exhibit a slightly higher level of intention to use telemedicine technology than their female counterparts.”25
Also, there were significant differences in actual implementation of telemedicine by profession (p = .000) and years of experience (p = .009; see Table 4). Consultants (56 percent) and those with more than 20 years of experience (48 percent) represented the highest frequency of actual implementation of telemedicine (Table 4). This might suggest that the older the healthcare provider, the stronger his or her intention to use telemedicine, perhaps because experience gives providers more insights about the need for new technological tools to improve the quality of care. This result contradicted the results of the survey of doctors in Milan, where physicians with higher seniority considered telemedicine to be of limited interest and were not convinced that it could improve clinical practice.26
With the help of telemedicine, “doctors in rural areas of the world can observe state-of-the-art medical procedures that they would otherwise have had to travel thousands of miles to witness.”27 Results of the present study clarified that there were statistically significant associations between attendance at teleconferences with facility (p = .000), age (p = .008), profession (p = .010), and years of experience (p = .005; see Table 5). Participants from ARAMCO, those older than 50 years, those working as consultants, and those with more than 20 years of experience showed the highest frequency of teleconference attendance (Table 5).
Perception of Healthcare Professionals about the Benefits and Challenges of Telemedicine
One study examining the benefits of telemedicine notes: “Now that worldwide satellite communication is available … telemedicine can be used in many different ways such as improving healthcare access, supporting health workers in isolated settings or addressing the shortage of specialist doctors.”28 In our study, perceptions of participants at the hospital not adopting telemedicine on the benefits of telemedicine were higher for all benefits (mean score 3.30 or higher, Table 6) than the perceptions of participants at hospitals adopting telemedicine (Table 7). This could be attributed to the fact that expectations are high before the actual implementation of telemedicine, while after implementation, in which participants may have experienced difficulties, lack of proper training, or other hurdles, the situation may be different. Participants not adopting telemedicine viewed telemedicine as beneficial in terms of improving quality of care, enhancing access to healthcare services, providing patient care and management, and saving both time and money (Table 6). By comparison, in a new teaching hospital in Lagos, Nigeria, the “majority of respondents believed that [telemedicine] would enhance access to health care services (23.4%), improve quality of care (14.1%), and reduce health care expenditures (6%).”29
Similarly, participants adopting telemedicine perceived the benefits of telemedicine as improving quality of care, enhancing access to healthcare, and saving time and money (Table 7). The study of Milan doctors indicated that the majority of doctors expressed moderate agreement that telemedicine enhanced quality of care,30 while the main benefits noted by the respondents in that survey and a Canadian one were immediate response, easy accessibility, and time and money savings.31, 32
The participants at hospitals adopting telemedicine perceived the least benefits as relating to easy use of the network, store-and-forward telemedicine, and follow-up after face-to-face contact (Table 7). This finding may be related to the fact that the telemedicine network was recently implemented in the Eastern Province, technical issues may be experienced while implementing store-and-forward telemedicine, training of users may not be sufficient, or patients might not show up for telemedicine follow-up as they do with face-to-face contact. The study of Milan doctors found that 9 percent of participants reported a lack of face-to-face contact between doctor and patient.33
Participants at hospitals not adopting telemedicine perceived the lack of knowledge about the meaning of telemedicine and its applications, types, benefits, and so forth (71 percent), the lack of time to adopt telemedicine (39.7 percent), and the lack of importance of telemedicine (21 percent; see Table 8) as barriers to the use of telemedicine. Moreover, the main barrier facing participants at hospitals adopting telemedicine was lack of knowledge about the services and benefits of telemedicine (49 percent; see Table 9). This may be due to the lack of wide dissemination of information about telemedicine through workshops, seminars, symposia, conferences, and so forth. Financial barriers and/or a lack of infrastructure was perceived as a barrier by participants at hospitals not adopting telemedicine (13.9 percent; Table 8). However, the Ministry of Health in Saudi Arabia allocated a total of 4 billion in Saudi riyal toward e-health programs in the period from 2008 to 2011.34 Health professionals’ resistance was also mentioned as a barrier by nonadopters (1.6 percent; Table 8). Literature has shown that the perceived usefulness of technology is the factor that contributes the most to physicians’ intention to use or not to use telemedicine technology in their hospitals.35
Other barriers for adopters were difficulty in the application of telemedicine, followed by lack of time to use or adopt telemedicine (29 percent and 22 percent respectively; Table 9). These findings contradicted those of other studies, which reported that budget and infrastructure were the two main factors inhibiting the adoption of telemedicine.36, 37 However, difficulty in the application of telemedicine goes hand in hand with the findings of Rogrove et al., who found that sophistication of the technology was the main barrier to the use of telemedicine.38
Conclusion and Recommendations
Although telemedicine is a promising technology and the Ministry of Health in Saudi Arabia has allocated a large budget for e-health, telemedicine modalities used in the Eastern Province were very limited. The percentage of adoption of already existing telemedicine technologies by health professionals was low. However, the majority of respondents at KFHU, the hospital in the study that had not adopted telemedicine, were interested in learning about and implementing telemedicine. There were statistically significant associations between actual implementation of telemedicine at hospitals adopting telemedicine with profession and years of experience. The perception of participants not adopting telemedicine on its benefits was higher than that of those who had adopted telemedicine. The most frequently cited benefits among adopters were improving quality of care, enhancing access to healthcare, and providing patient care and management. However, the lowest-ranked benefits as mentioned by adopters were easy use of the network, the use of store-and-forward telemedicine, and follow-up after face-to-face contact. The greatest barrier as perceived by healthcare providers not adopting telemedicine was a lack of knowledge about the meaning of telemedicine and its applications, types, and benefits. For participants adopting telemedicine, the most frequently cited barriers were lack of sufficient knowledge about other services and benefits of telemedicine, followed by difficulty in the application of telemedicine and then lack of time to adopt telemedicine. Accordingly, the following are recommended:
Better dissemination of information about the state of the art of research and development in telemedicine via national programs to educate and train healthcare professionals. Increasing awareness could be achieved through seminars, workshops, symposia, conferences, and so forth.
Proper training of healthcare providers on telemedicine to improve their skills.
A decrease in other nonclinical activities required by health professionals adopting telemedicine to allow them to devote more of their time to adopting the various modalities of telemedicine.
Better utilization of the already existing telemedicine network and an increase in the number of telemedicine centers.
These recommendations will help to ensure that the benefits of existing and future investments in telemedicine technologies are fully realized.
Support
This study was funded by the Deanship of Scientific Research at Dammam University in Saudi Arabia (project code 2011055).
Figure 1.
Perception of Participants on Benefits of Telemedicine at Hospitals Adopting and Not Adopting Telemedicine
Figure 2.
Perceptions of Healthcare Providers Not Adopting Telemedicine on the Challenges/Barriers to the Use of Telemedicine
Figure 3.
Perceptions of Healthcare Providers Adopting Telemedicine on the Challenges/Barriers to the Use of Telemedicine
Acknowledgments
This project's achievements could not have been accomplished without the support of Dr. Ghazi Al-Otaibi, Dean of the College of Applied Medical Sciences, and Dr. Hana Al-Harthi, Chair of the Health Information Management and Technology Department, at Dammam University in Eastern Province, Saudi Arabia.
Appendix A
Telemedicine Survey at Teaching Hospital Not Adopting Telemedicine
This survey will be used to determine opinion of healthcare professionals about telemedicine.
Name........................................................................ (Optional)
1) Hospital Title:
2) Gender: □ Male □Female
3) Age in years.....................
4) Nationality: □ Saudi □ Non Saudi
5) Profession:
□ Consultant □ General Physician
□ Specialist □ Other Specialty (specify)
6) Years of experience:............
7) Are you interested to know about telemedicine?
□ Yes □ No
8) Are you actually interested to implement advanced telemedicine technologies, e.g., telepathology, teleradiology, telemedical education, teleconsultation, videoconferencing, etc.? □ Yes □ No
9) In your opinion what are the barriers/challenges of adopting telemedicine (you can choose more than one option):
□ Lack of time to adopt telemedicine
□ Lack of knowledge about meaning of telemedicine
□ Lack of knowledge about applications/ types of telemedicine
□ Lack of knowledge about benefits of telemedicine
□ I think it's not important
□ Financial barrier
□ Other reason, specify.................................................................
In your opinion what are the benefits of adopting telemedicine:
| Benefits of Adopting Telemedicine | Strongly Agree (4) | Agree (3) | Disagree (2) | Strongly Disagree (1) |
|---|---|---|---|---|
| 10) Using telemedicine is beneficial to my patient care and management. | ||||
| 11) Telemedicine helps save time. | ||||
| 12) Telemedicine helps save money. | ||||
| 13) Easy use of network | ||||
| 14) Telemedicine can improve the quality of care services. | ||||
| 15) Telemedicine can enhance access to healthcare services. | ||||
| 16) Videoconferencing is beneficial. | ||||
| 17) Store-and-forward telemedicine is beneficial. | ||||
| 18) Interactive telemedicine, i.e., teleconsultation, tele-ICU, etc., is substantial. | ||||
| 19) Second opinion is important. | ||||
| 20) Follow-up after face-to-face contact is beneficial. |
Appendix B
Telemedicine Survey at Hospitals Adopting Telemedicine
This survey will be used to determine opinion of healthcare professionals about telemedicine.
Name........................................................................ (Optional)
1) Hospital Title:
2) Gender: □ Male □ Female
3) Age in years.....................
4) Nationality: □ Saudi □ Non Saudi
5) Profession:
□ Consultant □ General Physician
□ Specialist □ Other Specialty (specify)
6) Years of experience:............
7) Do you actually implement advanced telemedicine technologies at your hospital, e.g., telepathology, teleradiology, telemedical education, teleconsultation, videoconferencing, etc.? □ Yes □ No
8) How many times do you attend teleconferences?
9) In your opinion what are the barriers/challenges of adopting telemedicine (you can choose more than one option):
□ Lack of sufficient knowledge about other services/benefits of telemedicine □ Difficulty in the application of telemedicine □ Lack of time
□ Other reason, specify.................................................................
In your opinion what are the benefits of adopting telemedicine:
| Benefits of Adopting Telemedicine | Strongly Agree (4) | Agree (3) | Disagree (2) | Strongly Disagree (1) |
|---|---|---|---|---|
| 10) Using telemedicine is beneficial to my patient care and management. | ||||
| 11) Telemedicine helps save time. | ||||
| 12) Telemedicine helps save money. | ||||
| 13) Easy use of network | ||||
| 14) Telemedicine can improve the quality of care services. | ||||
| 15) Telemedicine can enhance access to healthcare services. | ||||
| 16) Video conferencing is beneficial. | ||||
| 17) Store-and-forward telemedicine is beneficial. | ||||
| 18) Interactive telemedicine, i.e., teleconsultation, tele-ICU, etc., is substantial. | ||||
| 19) Second opinion is important. | ||||
| 20) Follow-up after face-to-face contact is beneficial. |
Contributor Information
Azza Ali El-Mahalli, Azza Ali El-Mahalli, MD, PhD, is an associate professor in the College of Applied Medical Sciences at Dammam University in Dammam, Saudi Arabia and High Institute of Public Health at Alexandria University in Alexandria, Egypt.
Sahar Hafez El-khafif, Sahar Hafez El-khafif, PhD, is an assistant professor of electronic engineering at Menoufia University in Egypt.
Mona Faisal Al-Qahtani, Mona Faisal Al-Qahtani, PhD, is an assistant professor in the Department of Health Information Management and Technology at Dammam University in Dammam, Saudi Arabia.
Notes
- 1.American Telemedicine Association. “Telemedicine Defined.” Available at http://www.americantelemed.org/i4a/pages/index.cfm?pageid=3333
- 2.World Health Organization. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth. World Health Organization, 2010, p. 9. Available at http://www.who.int/goe/publications/ehealth_series_vol2/en/
- 3.Field Marilyn J., editor. Institute of Medicine, Committee on Evaluating Clinical Applications of Telemedicine. Telemedicine: A Guide to Assessing Telecommunications in Health Care. Washington, DC: National Academy Press; 1996. p. 1. [PubMed] [Google Scholar]
- 4.Sachpazidis, Ilias. “Image and Medical Data Communication Protocols for Telemedicine and Teleradiology.” Dissertation, Department of Computer Science, Technical University of Darmstadt, Germany, July 10, 2008.
- 5.Sisira E. Anthony C. S. Heather B. Elizabeth D. Richard W. Pre-registration Nurses: An Investigation of Knowledge, Experience and Comprehension of E-health. Australian Journal of Advanced Nursing. December 2007-February 2008;25(2):78–83. [Google Scholar]
- 6.American Telemedicine Association. Telemedicine/Telehealth Terminology. Available at http://www.americantelemed.org/files/public/standards/glossaryofterms.pdf (accessed February 2012).
- 7.Yale Telemedicine Center. “Telemedicine at Yale.” Available at http://www.yale.edu/omnibus/Dec95/telemedicine.html
- 8.Aarogya.com. “Advantages of Telemedicine.” Available at http://www.aarogya.com/insurance/telemedicine/4509-advantages-of-telemedicine.html
- 9.Ranson D. Telemedicine and the Law. Journal of Law and Medicine. 2007;15(3):356–59. [PubMed] [Google Scholar]
- 10.Hjelm N. M. Benefits and Drawbacks of Telemedicine. Journal of Telemedicine and Telecare. 2005;11(2):60–70. doi: 10.1258/1357633053499886. [DOI] [PubMed] [Google Scholar]
- 11.Ibid., quote from abstract available at http://www.ncbi.nlm.nih.gov/pubmed/15829049
- 12.Roig F.Saigí F.Barreras para la normalización de la telemedicina en un sistema de salud basado en la concertación de servicios” [Barriers to the normalization of telemedicine in a healthcare system model based on purchasing of healthcare services using providers’ contracts Gaceta Sanitaria 2552011397–402. Quote from abstract in English available at http://www.ncbi.nlm.nih.gov/pubmed/21719160 [DOI] [PubMed] [Google Scholar]
- 13.Rogrove Herbert J. McArthur David. Demaerschalk Bart M. Vespa Paul M. Barriers to Telemedicine: Survey of Current Users in Acute Care Units. Telemedicine and e-Health. 2012;18(1):48–53. doi: 10.1089/tmj.2011.0071. [DOI] [PubMed] [Google Scholar]
- 14.Bin Mulla M. J. The Minister of Communications & Information Technology Report on: “The National Communications and Information Technology Plan: The Vision towards the Information Society”, Kingdom of Saudi Arabia. Available at http://www.mcit.gov.sa/NR/rdonlyres/E8C255A7-E423-4F36-B9B3-C5CAAB6AE87A/0/2NICTPEng.pdf
- 15.World Health Organization. Report on the Intercountry Meeting on Telemedicine (WHO-EM/HTL/006/E/L). 1999. Available at http://whqlibdoc.who.int/hq/1999/WHO-EM_HLT_006_E_L.pdf
- 16.The E-health Center. King Faisal Specialist Hospital & Research Center. Jeddah, Saudi Arabia. Available at http://bportal.kfshrc.edu.sa/wps/portal/bportal/!ut/p/c1/04_SB8K8xLLM9MSSzPy8xBz9CP0os3g3M393Y3dHYwMLSwsLA6MQ1zDP0FAnIwMLY6B8JJK8gb-lG1A-0MLZ0ijYyMDRjIDucJB9-PWD5A1wAEcDfT-P_NxU_YLcCFMsE0dFAL12te4!/dl2/d1/L0lDUmlTUSEhL3dHa0FKRnNBL\1lCUlp3QSEhL2Vu/
- 17.United Nations Economic and Social Commission for Western Asia (ESCWA). National Profile for the Information Society in Saudi Arabia. 2009. Available at http://www.escwa.un.org/wsis/reports/docs/SaudiArabia_2005
- 18.Wooton R. Bonnardot L. In What Circumstances Is Telemedicine Appropriate in the Developing World? Journal of the Royal Society of Medicine Short Reports. 2010;1(37):1–10. doi: 10.1258/shorts.2010.010045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.“eHealth Centre.” Available at http://www.kfshrco.com/?p52
- 20.Breen P. Murphy K. Browne G. Molloy F. Reid V. Doherty C., et al. Formative Evaluation of a Telemedicine Model for Delivering Clinical Neurophysiology Services Part II: The Referring Clinician and Patient Perspective. BMC Medical Informatics and Decision Making. 2010;10(49) doi: 10.1186/1472-6947-10-49. Available at http://www.biomedcentral.com/1472-6947/10/49; quote from abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chismar, W. G., and S. Wiley-Patton. “Does the Extended Technology Acceptance Model Apply to Physicians.” Proceedings of the 36th Hawaii International Conference on System Sciences, 2003. Available at http://origin-www.computer.org/plugins/dl/pdf/proceedings/hicss/2003/1874/06/187460160a.pdf?template=1&loginState=1&userData=anonymous-IP%253A%253AAddress%253A%2B96.17.109.62%252C%2B%255B140.98.196.191%252C%2B212.138.110.5%252C%2B96.17.109.62%252C%2B127.0.0.1%255D
- 22.Shittu L. A. Joseph. Olamide Adesanya A. Mathew Izegbu C. Oluwole Oyewopo A. Arigbabuwo Ade. Oladapo Ashiru A. Knowledge and Perception of Health Workers Towards Tele-medicine Application in a New Teaching Hospital in Lagos. Scientific Research and Essays. 2007;2(1):16–19. Available at http://www.academicjournals.org/sre/PDF/PDF%202007/Jan/Shittu%20et%20al2.pdf. [Google Scholar]
- 23.Bahaadinbeigy K. Yogesan K. Wootton R. A Survey of the State of Telemedicine in Western Australia. Journal of Telemedicine and Telecare. 2010;16(4):176–80. doi: 10.1258/jtt.2010.004003. Abstract available at http://www.ncbi.nlm.nih.gov/pubmed/20511567. [DOI] [PubMed] [Google Scholar]
- 24.Gaggioli A. di Carlo S. Mantovani F. Castelnuovo G. Riva G. A Telemedicine Survey among Milan Doctors. Journal of Telemedicine and Telecare. 2005;11(1):29–34. doi: 10.1177/1357633X0501100107. [DOI] [PubMed] [Google Scholar]
- 25.Hu, P. J.-H., Olivia R. Liu Sheng, Patrick Y. Chau, Kar-Yan Tam, and Heidi Fung. “Investigating Physician Acceptance of Telemedicine Technology: A Survey Study in Hong Kong.” Proceedings of the 32nd Hawaii International Conference on System Sciences. IEEE, 1999, p. 6. Available at http://csdl2.computer.org/comp/proceedings/hicss/1999/0001/04/00014027.pdf
- 26.Gaggioli, A., S. di Carlo, F. Mantovani, G. Castelnuovo, and G. Riva. “A Telemedicine Survey among Milan Doctors.” [DOI] [PubMed]
- 27.Abodunrin O. L. Akande T. M. Knowledge and Perception of e-Health and Telemedicine among Health Professionals in LAUTECH Teaching Hospital, Osogbo, Nigeria. International Journal of Health Research. 2009;2(1):51–58. (e2114p123-130). Available at http://www.ijhr.org/vol2_no1/ijhr_2009_2_1_6_Lanre.pdf. [Google Scholar]
- 28.Wooton, R., and L. Bonnardot. “In What Circumstances Is Telemedicine Appropriate in the Developing World?” [DOI] [PMC free article] [PubMed]
- 29.Shittu, L. A. Joseph, A. Olamide Adesanya, C. Mathew Izegbu, A. Oluwole Oyewopo, Ade Arigbabuwo, A. Oladapo Ashiru. “Knowledge and Perception of Health Workers Towards Tele-medicine Application in a New Teaching Hospital in Lagos,” p. 17.
- 30.Gaggioli, A., S. di Carlo, F. Mantovani, G. Castelnuovo, and G. Riva. “A Telemedicine Survey among Milan Doctors.” [DOI] [PubMed]
- 31.Ibid.
- 32.Praxia Information Intelligence and Gartner, Inc. Telehealth Benefits and Adoption: Connecting People and Providers Across Canada. Study commissioned by Canada Health Infoway, May 30, 2011. Available at www.infoway-inforoute.ca/index.php/resources/reports/doc_download/447-telehealth-benefits-and-adoption-connecting-people-and-providers-full
- 33.Gaggioli, A., S. di Carlo, F. Mantovani, G. Castelnuovo, and G. Riva. “A Telemedicine Survey among Milan Doctors.” [DOI] [PubMed]
- 34.Qurban, M., and R. Austria. “Public Perception on E-health Services: Implications of Preliminary Findings of KFMMC for Military Hospitals in KSA.” Proceedings of the European and Mediterranean Conference on Information Systems (EMCIS), Dubai, May 25-26, 2008.
- 35.Chismar, W. G., and S. Wiley-Patton. “Does the Extended Technology Acceptance Model Apply to Physicians.”
- 36.Abodunrin, O. L., and T. M. Akande. “Knowledge and Perception of e-Health and Telemedicine among Health Professionals in LAUTECH Teaching Hospital, Osogbo, Nigeria.”
- 37.Whitten, P. Telemedicine in Michigan: A Policy Report Addressing Legal and Regulatory Barriers. Michigan State University. Available at http://www.ippsr.msu.edu/Publications/ARTelemedicine.pdf (accessed December 17, 2011).
- 38.Rogrove, Herbert J., David McArthur, Bart M. Demaerschalk, and Paul M. Vespa. “Barriers to Telemedicine: Survey of Current Users in Acute Care Units.” [DOI] [PubMed]