Abstract
This investigation examined the effectiveness of a self-help (SH), stepped-care (SC) weight loss program. Based on a failure to achieve pre-assigned weight loss goals, participants were eligible to be stepped-up from a SH program to two levels of treatment intensity (weight loss group [WLG]; individual counseling [IC]) beyond SH. The primary outcome was change in body weight. Fifty-three overweight/obese adults (BMI≥27 kg/m2; mean BMI of 37.3, SD=6.6, 89% Caucasian, and 77% female) participated in an 18-week weight loss intervention. During several phases of the investigation, those stepped-up to more intensive treatment lost comparable weight to those who were not stepped-up. Nevertheless, by the end of treatment, individuals who remained in SH (M = 8.6%) lost a significantly greater percentage of weight than individuals who received SH+IC (M = 4.7%; p<.05) and individuals in SH+IC lost a significantly greater percentage of weight than individuals who received SH+WLG+IC (M = 1.6%; p<.05). While some individuals benefited from being stepped-up to greater intensity treatment, other individuals experienced little benefit. The application of SC principles to the treatment of obesity needs further study.
Keywords: Weight loss treatment, Obesity, Stepped-care, Self-help
1. Introduction
Given the scope of the obesity epidemic, the chronic nature of the condition, and the cost of professional care for obesity-related diseases, cost-effective, time-efficient, and minimally intrusive treatments are greatly needed (Mokdad et al., 2003). Applying a stepped-care (SC) approach to the treatment of obesity represents one effort to efficiently allocate treatment resources. In a SC approach to treatment, patients are transitioned (stepped-up) to more intensive treatment when they are unable to meet treatment goals with less intensive treatment (Haaga, 2000; Sobell & Sobell, 2000). Stepped-care approaches have been developed for a variety of conditions, including weight management (Abrams, 1993; Carels, Young, Coit, Darby, et al., 2008; Carels et al., 2005; Carels et al., 2007; Carels et al., 2009; Expert Panel on Detection, 2001; Latner, 2001; NHLBI, 1997; Sobell & Sobell, 2000; Wadden, Brownell, & Foster, 2002).
In various SC models, self-help (SH) behavioral approaches are a recommended low-intensity treatment for initial weight loss efforts (Abrams, 1993; Carels et al., 2005; Carels et al., 2007; Expert Panel on Detection, 2001; NHLBI, 1997; Sobell & Sobell, 2000; Wadden et al., 2002), because they conserve treatment resources (Latner, 2001). However, between 40 and 60% of SH intervention participants are unable to achieve a clinically significant weight loss (5% body weight) prior to being stepped-up to greater intensity treatment (Carels, Young, Coit, Darby, et al., 2008; Carels et al., 2009). As an explanation for this limited success, a number of prominent experts suggest that the current “obesogenic” environment continues to fuel the obesity epidemic while also contributing to the widespread failure of weight loss attempts and maintenance (e.g., Brownell & Horgen, 2004; Lowe, 2003; Nestle, 2004). Preliminary randomized treatment outcome research has shown that individuals who are unable to lose weight using a SH behavioral approach may benefit from a more intensive weight loss group (WLG) that focuses on environmental modification to counteract the harmful impact of the nation's “obesogenic” environment on food consumption and lifestyle activities (Carels et al., 2009). Similarly, stepping up WLG participants who are struggling to lose weight to concurrent IC has received empirical support (Carels et al., 2005; Carels et al., 2007).
Despite the success that many individuals experience after being stepped-up to a more intensive WLG, some individuals continue to struggle with weight loss even after being stepped-up, and at times, SC approaches result in little or no additional weight loss (Carels, Young, Coit, Darby, et al., 2008; Polley, Wing, & Sims, 2002). Unfortunately, there is insufficient research evidence to predict, prior to treatment, which participants will benefit from only a WLG and which participants will require further treatment. Therefore, it is important to create not only more intensive stepped-up treatments, but also to provide participants with the opportunity to benefit from various treatment modalities during a weight loss attempt. To our knowledge, no weight loss study has initiated SH treatment with the possibility of being stepped-up to a WLG, IC, or if performance necessitates, a WLG with concurrent IC.
Providing the opportunity for participants to be stepped-up twice, should their failure to lose weight necessitate, offers the greatest individual support to those who need it, while conserving resources with those who do not require more intensive treatment. The current preliminary pilot investigation utilized a SC approach to weight loss to examine: 1) whether providing individuals more intensive treatment following the failure to meet weight loss goals resulted in comparable weight loss to individuals receiving less intensive treatment (e.g., SH), and 2) if factors commonly known to be associated with weight loss outcomes, such as self-monitoring frequency, and level of energy intake and expenditure (Carels, Young, Coit, Clayton, et al., 2008), differentiate individuals who are successful at losing weight using SH methods from those eligible for greater intensity treatment.
2. Method
2.1. Participants
Participants were recruited through local newspapers, e-mail, and a listserv at a Midwestern university. Participants were included if they were (a) overweight/obese (BMI≥27 kg/m2) and (b) nonsmokers. Participants were excluded if they reported (a) past or current cardiovascular disease, (b) insulin dependent diabetes, or (c) musculoskeletal problems that would prevent participation in moderate physical activity. Participants received no incentives for participating and instead provided a $100 deposit to reduce attrition among participants, which was refunded following completion of the program. This investigation received full human subjects review board approval, and participants provided documentation of their physician's medical clearance prior to participation.
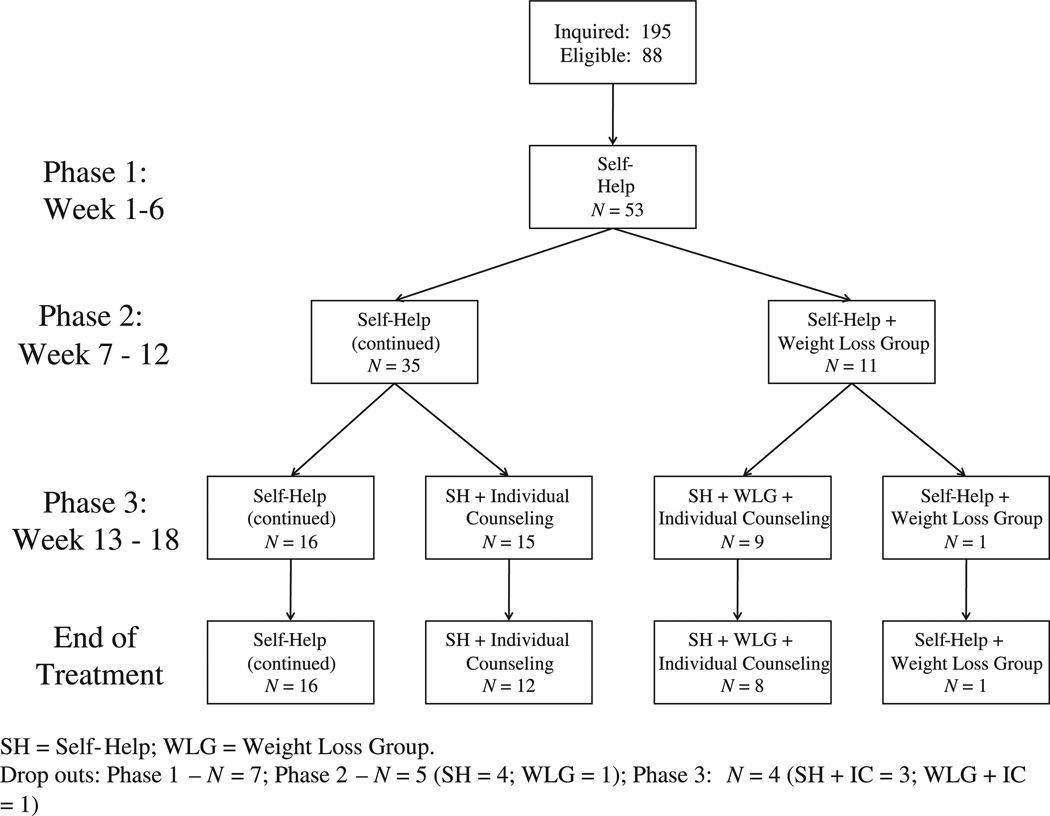
Of the 195 individuals that inquired about the study, 88were eligible, and 53 elected to participate in the study (Fig. 1). Most participants were Caucasian (88.5%; N = 46, not reported=1) and female (77.4%; N = 41) and the mean age of participants was 47.15 (SD = 14.1). Annual income exceeded $30,000 for approximately 70% (N = 35, not reported=2) of the participants and 73% (N = 38, not reported=1) had at least a baccalaureate degree. Mean body mass index (BMI) at baseline was 37.3 (SD = 6.6; range 27.4–61.3). Thirty-seven participants (70%) completed the 18-week intervention.
Fig. 1.
Participant treatment flow diagram.
2.2. Study design
All participants began an 18-week SC program in a SH condition (Phase 1: baseline–week 6; see Fig. 1 for participant attrition and SC eligibility). Participants were informed that their weight would be assessed at week 6, week 12, and post-treatment (week 18). All participants received an initial weight loss goal of 2.5% and 5% of their baseline body weight at the end of the 6th and 12th weeks, respectively. At week 6, participants who were unable to achieve the 2.5% total body weight loss were stepped-up to a 12-week, behavioral WLG and given a new 2.5% weight loss goal for the next six weeks based on their week 6weight (Phase 2:weeks 6–12). Otherwise, participants continued with SH for an additional 6 weeks with a 5% total weight loss goal by week 12.
At week 12, SH participants who had not previously been stepped-up and were able to achieve the 5% total body weight loss continued with SH for an additional 6 weeks with another 2.5% weight loss goal for the final six weeks of the program (Phase 3: weeks 13–18). WLG participants who were able to achieve a 2.5% total body weight loss goal between weeks 6 and 12 continued with the WLG for an additional 6 weeks with another 2.5% weight loss goal for the final six weeks of the program. SH and WLG participants who were unable to achieve their respective weight loss goals from Phase 2 were stepped-up to individual counseling (SH+IC or SH+WLG+IC conditions respectively). Because SH participants who failed to meet Phase 2 weight loss goals had evidenced some success during the prior 12 weeks, we felt that these individuals would best benefit from a more intensive, individualized approach to treatment to assist them in their continued success. Participants in the WLG who were unable to reach their weight loss goal were given concurrent IC to maximize their level of support provided (SH+WLG+IC). For the final six weeks of the program, all participants received a new2.5% weight loss goal based on their week 12 weight (see Fig. 1 for participant attrition and SC eligibility). No further treatment was provided if participants failed to achieve this new goal, which was provided for motivational purposes.
2.2.1. Phase 1: baseline–week 6
The 18-week intervention took place between January and May, 2010. At the baseline visit, participants attended an orientation session in small groups (8–15 individuals per group)where they received study materials: an accelerometer to track energy expenditure, a LEARN weight loss program manual (Brownell, 2004), and instructions on how to self-monitor and electronically report diet and physical activity. Participants were instructed to read one chapter of the weight loss manual each week, self-monitor and record diet and physical activity daily, and create a 500 calorie per day deficit through diet and physical activity. Participants were instructed to electronically report energy expenditure daily via the Internet or paper and pencil copies.
Body weight was measured using a digital scale (BF-350e; Tanita, Arlington Heights, IL) to the nearest 0.1 lb and height was measured to the nearest 0.5 in. using a height rod on a standard spring scale. Baseline and post-treatment body fat estimates were obtained using leg-to-leg bioelectrical impedance (BF-350e). All assessments and interventions were conducted by a licensed clinical health psychologist or psychology doctoral students with experience leading weight loss interventions.
2.2.2. Phase 2: weeks 7–12
Participants who were eligible at week 6 were stepped up to a more intense behavioral intervention compared to SH. These participants partook in a 12-week, group-based behavioral weight loss program, Transforming Your Life (Carels et al., 2009; Carels et al., 2011), which was administered in weekly, 90-minute sessions and consisted of a combination of didactic instruction, individual activities, and out-of class assignments. Following an introductory session and two sessions devoted to nutrition basics, the TYL program emphasized: 1) creating and maintaining healthy habits while disrupting unhealthy habits, 2) creating personal food and physical activity environments that minimize exposure to unhealthy eating and sedentary behaviors and increase exposure to healthy eating and physical activity, and 3) increasing participants' weight loss motivation. Additional intervention details have been published elsewhere (Carels et al., 2011).
2.2.3. Phase 3: weeks 13–18
All participants who missed their phase 2 weight loss goal were stepped up to a more intensive behavioral intervention compared to SH and WLG. The counseling sessions utilized motivational enhancement (Miller & Rollnick, 2002) and problem-solving (D'Zurilla, 1999) techniques. Participants eligible for counseling met weekly for the remainder of the program with a licensed clinical health psychologist or clinical psychology doctoral student for 45-minute individual sessions. The overall goals of the individual sessions were to (a) elicit motivation for change, (b) teach problem-solving skills, (c) identify and remediate any problem-solving skill deficits, and (d) apply problem-solving techniques to participants' problems and evaluate the outcomes (Miller & Rollnick, 2002). Participants received a brief problem-solving manual (available upon request) to reinforce problem-solving principles.
2.3. Measures
2.3.1. Self-monitoring
All participants were instructed to self-monitor their dietary intake daily and were provided with demonstrations of common food measurement procedures as well as written instructions for measurement estimation as a reference. Participants were also instructed to use food and beverage calorie guides or Internet dietary analysis programs, such as Calorie King (http://www.calorieking.com) to estimate energy intake from meals, snacks, and beverages. Additionally, participants were instructed to self-monitor energy expenditure (see below) and all purposeful physical activity (type and duration of physical activity not including activity associated with daily living, such as occupational exertion or taking the stairs). Caltrac accelerometers were provided to participants to assess total energy expended (kcal) as well as activity energy expended (kcal) during consecutive 24 hour periods. Although Caltrac accelerometers have been shown to mildly overestimate the absolute energy cost (i.e., measured VO2) of selected activities, they provide a reliable assessment of total energy expenditure (Balogun, Martin, & Clendenin, 1989; Fehling, Smith,Warner, & Dalsky, 1999).
2.4. Data analysis
Chi-square and ANOVA were used to compare drop-outs to treatment completers as well as participants receiving various levels of treatment intensity (SH, SH+IC, SH+WLG+IC) on demographic characteristics, including BMI. Drop outs during a particular phase of treatment were determined by their failure to complete a weight assessment at the end of the phase. No participants declined greater intensity treatment. ANOVA was used to compare participants receiving various levels of treatment intensity on weight loss (lbs; percent body weight). Chi-square and ANOVA were used to examine the impact of self-monitoring and energy intake and expenditure on SC phase eligibility during Phases 1, 2, and 3.
3. Results
3.1. Phase 1
3.1.1. Weight loss and stepped-care eligibility
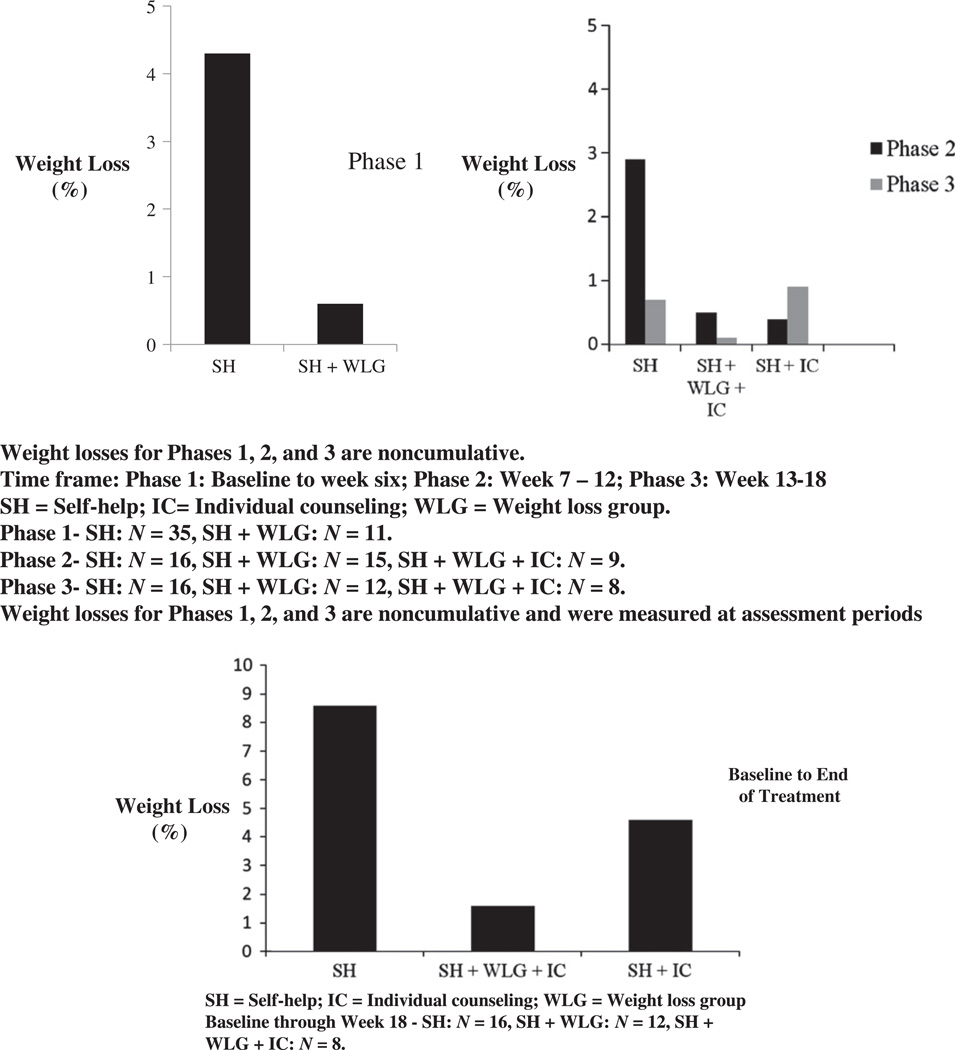
Following the Phase 1 assessment, 35 of 53 participants met or exceeded their 2.5% weight loss goal and remained in SH with an average weight loss of 4.3% total bodyweight (lbs;M = 9.7; SD = 3.1). Eleven participants lost an insignificant amount of weight during Phase 1 (0.6% total body weight; lbs: M = 1.6; SD = 3.9) and were eligible for a WLG. Weight loss (lbs) was significantly greater in individuals who remained in SH compared to individuals stepped-up to a WLG during Phase 1, F (1,45)=51.5, p <0.001, Cohen's d = 2.54 (Table 1; Fig. 2).
Table 1.
Treatment outcomes by level of stepped care.
| Self-help (N=35) |
Self-help+individual counseling (N=15) |
Self-help+weight loss group+individual counseling(N=11) |
||||
|---|---|---|---|---|---|---|
| Proportion including DOs met weight loss goal | Prop. | % | Prop. | % | Prop. | % |
| Week 6 | 35/53 | 66.0 | 11/53 | 20.8 | ||
| Week 12 | 16/35 | 45.7 | 15/35 | 42.9 | 9/11 | 81.8 |
| Week 18 | 5/16 | 31.3 | 3/15 | 20.0 | 1/9 | 11.1 |
| aTotal weight change, % (SD) | 8.6 | (4.7) | 4.7 | (2.2) | 1.6 | (3.0) |
| aTotal weight change, lbs. (SD) | 18.7 | (10.4) | 12.6 | (9.0) | 4.0 | (8.0) |
DO = Drop out.
Baseline through week 18.
Fig. 2.
Weight change during Phase 1, Phase 2, and Phase 3 and total weight loss.
3.1.2. Baseline factors, self-monitoring, energy intake and expenditure, and stepped-care eligibility
Baseline factors (age, gender, income, education, BMI) were unrelated to WLG status with the exception of race. Non-Caucasian participants (N = 6) were more likely to be eligible for WLG than Caucasian participants, χ2(1, N = 52)=7.74, p = 0.02.
Individuals who remained in the SH condition were generally more likely to self-monitor (SH: 93.9%; WLG: 45.5%), χ2(1, N = 44)=11.48, p = 0.001, and self-monitored significantly more days, F (2,44)=24.2, p <0.001, Cohen's d = 1.75, during Phase 1 than individuals stepped-up to the WLG. While individuals in the WLG reported greater caloric expenditure from activity than SH participants, F (1,36)=5.9, p <02, Cohen's d = 1.20, this analysis was based on only 4 WLG participants due to lack of participant reporting (see Table 2).
Table 2.
Comparison of self-monitoring and energy intake and expenditure between self-help and stepped-care participants.
| Phase 1 | Phase 2 | Phase 3 | ||||
|---|---|---|---|---|---|---|
| Self-help |
SH+weight loss groupa |
Self-help |
SH+individual counseling |
Self-help |
SH+individual counseling |
|
| Factors | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) |
| Self-monitor frequency (days) | 39.7 (20.9)2 | 7.5 (9.6)2 | 22.1 (14.6) | 13.3 (14.6) | 28.6 (24.3) | 20.0 (23.8) |
| Caloric intake (kcal/daily) | 1610 (510) | 1848 (438) | 1456 (422)1 | 2645 (837)1 | 1448 (423)1 | 2715 (1052)1 |
| Caloric expenditure (kcal/daily) | 2462 (502) | 2643 (783) | 2380 (385) | 2986 (649) | 2262 (447) | 3151 (526) |
| Activity expenditure (kcal/daily) | 543 (235)2 | 879 (437)2 | 530 (215) | 617 (349) | 497 (301) | 672 (399) |
| Caloric Difference | 838 (447) | 774 (777) | 919 (411)1 | 473 (740)1 | 793 (395) | 395 (974) |
| Exercise minutes | 24.3 (14.1) | 14.1 (16.2) | 22.0 (14.6) | 24.8 (19.6) | 21.8 (21.7) | 25.1 (10.7) |
p<.05 (SH versus IC);
p<.05 (SH versus WLG). Note. SH = Self-help; Phase 1: weeks 1–6; Phase 2: weeks 7–12; Phase 3: weeks 13–18; and Total: Baseline to end of treatment.
WLG+IC failed to self-monitor during Steps I and II.
3.2. Phase 2
3.2.1. Weight loss and stepped-care eligibility
During Phase 2, participants lost an average of, 1.4% of total body weight (lbs; M = 3.3; SD = 5.0). SH participants lost an average of 1.6% of total body weight (lbs; M = 3.5; SD = 4.8). WLG participants lost an average of 0.7% of total body weight (lbs; M = 2.5; SD = 5.8). On average, WLG eligible participants attended 9.1 (SD = 2.8) sessions out of 12. SH participants did not lose significantly more weight than WLG participants during Phase 2 (SH: M = 3.5, SD = 4.8; WLG: M = 2.5, SD = 5.8), F (1,40)=0.3, p = ns, Cohen's d = 0.21 (see Table 1; Fig. 2).
Following the Phase 2 assessment, 16 out of 35 SH participants reached their 5% weight loss goal and remained in SH with an average weight loss of 7.9% total body weight (lbs; M = 16.8; SD = 5.8). Fifteen SH participants were eligible for IC (SH+IC) with an average weight loss of 3.8% total body weight (lbs; M = 9.3; SD = 4.1). SH participants who were eligible for IC lost an average of only 0.4 lbs (SD = 2.8) during Phase 2 compared to an average of 6.2 lbs (SD = 4.9) for those participants who remained in SH, F (1,28)=13.3, p <.001, Cohen's d = 1.45.
For WLG participants, one male participant reached his 2.5% weight loss goal for Phase 2 with a weight loss of 4.5% total body weight (14.6 lbs; SH+WLG). Nine participants were eligible for IC concurrent with their WLG (SH+WLG+IC) with an average weight loss of 0.4% total body weight (lbs; M = 1.7; SD = 4.0) during Phase 2 (see Table 1; Fig. 2).
3.2.2. Weight loss: Phase 1 versus Phase 2
Compared to participants who remained in SH, participants who were stepped-up to a WLG in Phase 1 were significantly more likely to be stepped-up to IC in Phase 2, χ2(1, N = 41)=6.2, p <03. Regarding SH participants eligible for SH+IC, their 0.4 lb weight loss during Phase 2 was substantially lower than their 9.3 lb weight loss during Phase 1, t (15)=7.14, p <.01, Cohen's d = 2.14. Regarding WLG participants eligible for IC concurrent with their WLG (SH+WLG+IC), their 1.7 lb (SD = 4.0) weight loss during Phase 2 was comparable to their 1.1 lb weight loss (SD = 4.1) during Phase 1, p = ns. Participants stepped-up to the WLG received little benefit by being stepped-up to a more intense treatment group (see Table 1; Fig. 2).
3.2.3. Baseline factors, self-monitoring, energy intake and expenditure, and stepped-care eligibility
Baseline factors were unrelated to being stepped-up to IC. However, participants who remained in SH following the Phase 2 assessment were significantly more likely to self-monitor than individuals eligible to participate in IC (SH: 61.9%; SH+IC: 38.1%), χ2(1, N = 41)=7.7, p = 0.008. During Phase 2, despite being stepped-up, no WLG participants self-monitored. SH participants consumed significantly fewer daily calories, F (1,19)=7.9, p = 0.02, Cohen's d = 1.47, and created a significantly greater daily caloric deficit, F (1,19)=4.46, p = 0.05, Cohen's d = 1.10, than SH+IC participants (see Table 2).
3.3. Phase 3
3.3.1. Weight loss and stepped-care eligibility
During Phase 3, participants lost an average of 0.8% of total body weight (lbs; M = 2.4; SD = 5.5). Sixteen SH participants lost 0.7% body weight (lbs; M = 2.0; SD = 5.9), 12 SH+IC participants lost 0.9% body weight (lbs; M = 2.9; SD = 5.2), 8 SH+WLG+IC participants lost 0.1% body weight (lbs; M = 1.2; SD = 4.7), and the 1 SH + WLG participant lost 3.8% body weight (lbs; M = 12.4). On average, IC eligible participants attended 3.5 (SD = 1.1) IC sessions out of six. There were no significant differences between groups in weight loss during Phase 3, and no condition was significantly more likely to meet the 2.5% weight loss goal (Table 1; Fig. 2).
3.3.2. Weight loss: Phase 2 versus Phase 3
An important comparison during this phase is whether SH+WLG+IC participants and SH+IC participants, respectively, lost more weight during Phase 3 relative to Phase 2. SH+IC participants lost 2.5 lbs more in Phase 3 relative to Phase 2 (2.9 versus 0.4 lbs; the difference was marginally significant; p <06); however, SH+WLG+IC participants lost 0.6 lbs less in Phase 3 relative to Phase 2 (p = ns). See Table 1 and Fig. 2.
3.3.3. Self-monitoring, energy intake and expenditure, and stepped-care eligibility
Participants who remained in SH were significantly more likely to self-monitor than individuals eligible to participate in SH+IC (SH: 70.6%; SH+IC: 29.2%), χ2(1, N = 41)=7.0, p <01. Again, no SH+WLG+IC participants self-monitored during Phase 3. The SH group consumed significantly fewer daily calories F (1,18)=6.2, p <03, Cohen's d = 1.32, than the SH+IC group. No other group differences were observed (see Table 2).
3.4. Total intervention effects
By the end of treatment, 16 SH participants lost 8.6% total body weight (lbs; M = 18.7; SD = 10.4; body fat%: M = 5.6; SD = 3.4), 12 SH+IC participants lost 4.7% total body weight (lbs; M = 12.6; SD = 9.0; body fat%: M = 2.6; SD = 2.9), 8 SH+WLG+IC participants lost 1.6% total body weight (lbs; M = 4.0; SD = 8.0; body fat%: M = 2.1; SD = 2.2), and the 1 SH+WLG participant not eligible for concurrent IC lost 10.5% total body weight (34.0 lbs; 8.6% body fat). See Table 1 and Fig. 2.
Across the entire program, SH, SH+IC, and SH+WLG+IC conditions differed significantly in percent weight loss, F (2,36)=9.5, p <001, Cohen's d = 1.01, and actual weight loss (lbs), F (2,36)=5.8, p <008, Cohen's d = 0.79. The SH condition lost a significantly greater percentage of weight than both the SH+IC condition, p <02, (M = −3.5; SE = 1.4) and the SH+WLG+IC condition, p <001, (M = −7.0; SE = 1.6). The SH+IC group lost a significantly greater percentage of weight than the SH+WLG+IC condition (M = −3.5; SE = 1.7). Findings were comparable for total weight loss (lbs).
4. Discussion
This investigation utilized a SC model to examine whether participants could successfully lose weight when provided with a treatment intensity matched to their performance during a weight loss program. If participants did not achieve their weight loss goals at pre-specified 6-week intervals, participants were stepped-up and given more intensive treatment. In reality, nearly all participants initially stepped-up to a WLG in Phase 1 were also eligible for IC at the end of Phase 2, thus obviating the need to examine a subset of participants who only received a WLG. Therefore, in this investigation, participants who remained in SH, participants who were stepped-up to a WLG following Phase 1 and then to IC following Phase 2 (SH+WLG+SH), and participants who were only stepped-up to IC only following Phase 2 (SH+IC) were compared.
At the end of Phase 1 (6th week of the program), approximately 3 out of 4 participants who remained in treatment successfully lost 2.5% of their body weight and remained in SH; approximately 1 in 4 participants who were unsuccessful at losing 2.5% of their weight were stepped-up to a WLG with the intention of providing more intensive treatment to individuals who needed greater support. However, these participants continued to struggle to lose weight throughout treatment. In fact, except for one participant, everyone who failed to lose 2.5% body weight during Phase 1 again failed to lose another 2.5% bodyweight loss during Phase 2 and was stepped-up to receive IC concurrently with the continued WLG. While it is unknown how SH+WLG+IC participants would have performed had they not received SC, there was little evidence that SH+WLG+IC participants benefited from more intensive treatment, either through a WLG alone or in combination with IC. These findings are consistent with research across a number of psychological and behavioral domains, including weight loss, which suggests that an early poor response to treatment is often predictive of poor treatment outcome (Carels, Cacciapaglia, Douglass, Rydin, & O'Brien, 2003; Dubbert & Wilson, 1984; Ilardi & Craighead, 1994; Jeffery,Wing, & Stunkard, 1978).
An examination of the self-monitoring data indicates that one plausible explanation for the poor performance of the SH+WLG+IC participants was their failure to self-monitor, and to a lesser extent, their higher caloric intake relative to SH participants. For example, during the first six weeks of the program, including the orientation week that occurred prior to the intervention, only 46% of SH+WLG+ IC participants reported self-monitoring, and those who reported monitoring only did so on 7.5 days during the entire seven week period. In contrast, 94% of the SH participants self-monitored for an average of 40 days. In fact, despite being stepped-up to a WLG and participating in IC, the SH+WLG+IC participants universally failed to self-monitor during the last 12 weeks of the program. Given the importance of regular self-monitoring to weight loss success (Boutelle, Kirschenbaum, Baker, & Mitchell, 1999; Carels, Young, Coit, Clayton, et al., 2008), it is not surprising that SH+WLG+IC participants struggled to meet their weight loss goals.
Between weeks 6 and 12 (Phase 2) approximately 40% of the remaining participants reached their assigned weight loss goal. However, approximately 60% missed their goal and became eligible for individual counseling (two-thirds of these participants were formerly in SH and one-third were participating in a WLG). It is interesting that during Phase 2, a number of SH participants who had lost considerable weight during Phase 1 failed to reach their 5% weight loss goal. In fact, during Phase 2, SH participants eligible for IC lost only 0.4 lbs in six weeks (SH+IC).
Again, self-monitoring and caloric intake likely contributed to the observed differences between the SH and SH+IC participants. During Phase 2, those who remained in SH were more likely to self-monitor and did so nearly twice as many days as those eligible for SH+IC. Also, of those who self-monitored, participants eligible for SH+IC reported creating a smaller daily caloric deficit (a deficit of 440 calories per day less than SH participants) and consuming 1100 calories more per day than SH participants. In addition to self-monitoring, caloric intake is important for successful weight loss, and this indicator strongly favored SH participants.
Interestingly, between weeks 12 and 18, SH+IC participants lost nearly 3 lbs, while participants in the SH condition and SH+WLG+IC conditions lost 2.0 and 1.2 lbs, respectively. Despite self-monitoring and daily caloric intake differences relative to SH participants, participants stepped up to IC appeared to have benefited from it, based on their significant weight loss during that period. SH+IC participants with the addition of individual counseling lost 2.8 lbs during weeks 13–18 relative to 0.4 lbs during weeks 7–12 with no IC. The greater social support or perceived accountability of a weekly face-to-face meeting may have contributed to the positive weight loss outcomes.
In this investigation, there were indications that matching treatment intensity to achievement of pre-assigned weight loss goals using a SC model was effective in helping some people to lose weight. Specifically, SC benefited most individuals who initially showed some success. As noted above, SH participants eligible for IC lost 0.4 lb during Phase 2; however, upon receiving IC, they evidenced a significant 2.8 pound weight loss during Phase 3. However, weight loss during Phase 3 was not significantly different between SH+WLG+IC, SH, and SH+IC participants. It could be argued that providing people with different intensity treatments contributed to more equitable weight losses among participants during the various time periods. At the same time, it is equally plausible that the commonly observed slowing down of weight loss among successful weight loss program participants accounted for the findings.
Despite some promising findings, several limitations of the study should be acknowledged. The modest sample size in this investigation had limited power to detect group differences that did not evidence a large effect size. Additionally, the small number of individuals who participated in SC and the predominately Caucasian and female sample suggest that replication with a larger, more diverse sample is warranted. To reduce potential confounds, individuals who smoked, had past or current cardiovascular disease, insulin dependent diabetes, or musculoskeletal problems that would prevent participation in moderate physical activity were excluded from the study. Additional potential differences in participants' medical, behavioral, or psychological conditions (e.g., menopausal status, weight loss history, motivation)were not assessed in this investigation and may have adversely influenced treatment outcomes in various groups (Wadden et al., 2002). Future research may benefit from a thorough examination of baseline factors, such as motivation, and their relationship to treatment outcome, stepped-care status, and attrition. The observed changes in dietary intake in this study are based on self-report data, which are susceptible to considerable underreporting (Trabulsi & Schoeller, 2001). It is also unclear whether the observed benefits in those who received IC were due to the specific counseling techniques utilized (motivational enhancement; problem-solving) or simply a function of some other factor, such as additional therapeutic contact. Finally, the duration of the intervention was relatively brief (i.e., 18 weeks), follow-up data is unavailable, and although comparable to similar weight loss treatment outcome research (Honas, Early, Frederickson, & O'Brien, 2003), attrition was somewhat high, thus limiting conclusions of the potential long-term efficacy of the intervention.
Some individuals can be successful at losing weight with a minimally intensive SH intervention. However, other individuals who are experiencing complications that interfere with treatment might benefit from a more intensive intervention. Similarly, individuals who lose insignificant weight early in a program may require SC treatment modalities that utilize non-behavioral forms of treatment, such as pharmacotherapy. Nevertheless, utilizing a SC approach allows those who successfully lose weight in a SH program to do so in the least intrusive way, while allowing for the targeted intervention of participants who require more intensive treatment. Future research would benefit from determining the optimal timing of introducing more intensive treatment and, resources permitting, randomizing individuals to a standard treatment group for comparison (e.g., behavioral weight loss group).
Cost-effective treatments are needed to effectively manage the rising rates of obesity. A SC approach offers a potentially cost-effective approach to treating individuals exhibiting a poor response to the early stages of low intensity treatment. The results from the current investigation suggest that the application of SC principles to the treatment of obesity has promise. However, further research is needed to identify the best manner in which to provide stepped care in weight loss treatment.
Footnotes
Role of funding sources
There was no external funding for this study.
Contributors
All authors designed and implemented the study. Robert Carels conducted literature searches and wrote the introduction. Marissa Wagner Oehlhof and Nova Hinman wrote the methods section. Amanda Gumble and Afton Koball conducted the statistical analysis and wrote the Results section. Kathleen Young wrote the Discussion section. Lynn Darby edited all parts of the manuscript.
Conflict of interest
All authors declare that they have no conflicts of interest.
References
- Abrams DB. Treatment issues in tobacco dependence: Towards a stepped-care model. Tobacco Control. 1993;2:s17–s37. [Google Scholar]
- Balogun J, Martin D, Clendenin M. Calorimetric validation of the Caltrac accelerometer during level walking. Physical Therapy. 1989;89:501–509. doi: 10.1093/ptj/69.6.501. [DOI] [PubMed] [Google Scholar]
- Boutelle KN, Kirschenbaum DS, Baker RC, Mitchell ME. How can obese weight controllers minimize weight gain during the high risk holiday season? By self-monitoring very consistently. Health Psychology. 1999;18:364–368. doi: 10.1037//0278-6133.18.4.364. [DOI] [PubMed] [Google Scholar]
- Brownell KD. The LEARN program for weight management. 10th Edition. Dallas, TX: American Health Publishing Company; 2004. [Google Scholar]
- Brownell KD, Horgen KB. Food fight: The inside story of the food industry, America's obesity crisis, and what we can do about it. Chicago, IL: Contemporary Books; 2004. [Google Scholar]
- Carels RA, Cacciapaglia HM, Douglass OM, Rydin S, O'Brien WH. The early identification of poor treatment outcome in a women's weight loss program. Eating Behaviors. 2003;4:265–282. doi: 10.1016/S1471-0153(03)00029-1. [DOI] [PubMed] [Google Scholar]
- Carels RA, Darby LA, Cacciapaglia HM, Douglass OM, Harper J, Kaplar M, et al. Applying a stepped care approach to the treatment of obesity. Journal of Psychosomatic Research. 2005;59:375–383. doi: 10.1016/j.jpsychores.2005.06.060. [DOI] [PubMed] [Google Scholar]
- Carels RA, Darby LA, Cacciapaglia HM, Konrad KK, Coit C, Harper J, et al. Using motivational interviewing as a supplement to obesity treatment: A stepped-care approach. Health Psychology. 2007;26:369–374. doi: 10.1037/0278-6133.26.3.369. [DOI] [PubMed] [Google Scholar]
- Carels RA, Wott CB, Young KM, Gumble A, Darby LA, Oehlhof MW, et al. Successful weight loss with self-help: A stepped-care approach. Journal of Behavioral Medicine. 2009;32:503–509. doi: 10.1007/s10865-009-9221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carels RA, Young KM, Coit C, Clayton AM, Spencer A, Hobbs M. Can following the caloric restriction recommendations from the dietary guidelines for Americans help individuals lose weight? Eating Behaviors. 2008;9:328–335. doi: 10.1016/j.eatbeh.2007.12.003. [DOI] [PubMed] [Google Scholar]
- Carels RA, Young KM, Coit C, Darby LA, Clayton AM, Spencer A, et al. The failure of therapist assistance and stepped-care to improveweight loss outcomes. Obesity. 2008;16:1460–1462. doi: 10.1038/oby.2008.49. [DOI] [PubMed] [Google Scholar]
- Carels RA, Young KM, Koball A, Gumble A, Darby LA, Oehlhof MW, et al. Transforming your life: An environmental modification approach to weight loss. Journal of Health Psychology. 2011;16:430–438. doi: 10.1177/1359105310380986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubbert P, Wilson G. Goal-setting and spouse involvement in the treatment of obesity. Behavioral Research and Therapy. 1984;22:227–242. doi: 10.1016/0005-7967(84)90003-2. [DOI] [PubMed] [Google Scholar]
- D'Zurilla TJ. Problem-solving therapy: A social competence approach to clinical intervention. New York, NY: Springer; 1999. [Google Scholar]
- Expert Panel on Detection. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood pressure in adults. JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- Fehling P, Smith D, Warner S, Dalsky G. Comparison of accelerometers with oxygen consumption in older adults during exercise. Medicine & Science in Sports & Exercise. 1999;31:171–175. doi: 10.1097/00005768-199901000-00026. [DOI] [PubMed] [Google Scholar]
- Haaga DA. Introduction to the special section on stepped care models in psychotherapy. Journal of Consulting and Clinical Psychology. 2000;68:547–548. [PubMed] [Google Scholar]
- Honas JJ, Early JL, Frederickson DD, O'Brien MS. Predictors of attrition in a large clinic-based weight loss program. Obesity. 2003;11:888–894. doi: 10.1038/oby.2003.122. [DOI] [PubMed] [Google Scholar]
- Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology: Science and Practice. 1994;1:138–156. [Google Scholar]
- Jeffery RW, Wing RR, Stunkard A. Behavioral treatment of obesity: The state of the art 1976. Behavior Therapy. 1978;9:189–199. [Google Scholar]
- Latner JD. Self-help in the long-term treatment of obesity. Obesity Reviews. 2001;2:87–97. doi: 10.1046/j.1467-789x.2001.00028.x. [DOI] [PubMed] [Google Scholar]
- Lowe MR. Self-regulation of energy intake in the prevention and treatment of obesity: Is it feasible? Obesity Research. 2003;11:44s–59s. doi: 10.1038/oby.2003.223. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York, NY: The Guilford Press; 2002. [Google Scholar]
- Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA : The Journal of the American Medical Association. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute. The sixth report of the joint national committee on prevention, detection, and evaluation, and treatment of high blood pressure. (Rep. No. no. 98–4080) Washington, DC: NIH; 1997. [PubMed] [Google Scholar]
- Nestle M. Food politics. Berkeley, CA: University of California Press; 2004. [Google Scholar]
- Polley B, Wing RR, Sims CJ. Randomized controlled trial to prevent excessive weight gain in pregnant women. International Journal of Obesity. 2002;26:1494–1502. doi: 10.1038/sj.ijo.0802130. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC. Stepped care as a heuristic approach to the treatment of alcohol problems. Journal of Consulting and Clinical Psychology. 2000;68:573–579. [PubMed] [Google Scholar]
- Trabulsi J, Schoeller DA. Evaluation of dietary assessment instruments against doubly labeled water, a biomarker of habitual energy intake. American Journal of Endocrinology Metabolism. 2001;281:E891–E899. doi: 10.1152/ajpendo.2001.281.5.E891. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Brownell KD, Foster G. Obesity:Managing the global epidemic. Journal of Consulting and Clinical Psychology. 2002;70:510–525. doi: 10.1037//0022-006x.70.3.510. [DOI] [PubMed] [Google Scholar]