Abstract
Objective
To study risk factors for revision of primary total hip replacement (THR) in a US population-based sample.
Methods
Using Medicare claims, we identified beneficiaries from 29 US states who underwent primary THR between 7/1/1995 and 6/30/1996, and followed them through 12/31/2008. Potential cases had ICD-9 codes indicating revision THR. Each case was matched by state with one control THR recipient who was alive and unrevised when the case had revision THR. We abstracted hospital records to document potential risk factors. We examined associations between preoperative factors and revision risk using multivariate conditional logistic regression.
Results
The analysis data set consisted of 719/836 case-control pairs with complete data for analysis variables. Factors associated with higher revision odds in multivariate models were age ≤75 at primary surgery (OR 1.52, 95% CI 1.20, 1.92), height in highest tertile (OR 1.40, 95% CI 1.06, 1.85), weight in highest tertile (OR 1.66, 95% CI 1.24, 2.22), cemented femoral component (OR 1.44, 95% CI 1.10, 1.87), prior contralateral primary THR (OR 1.36, 95% CI 1.05, 1.76), other prior orthopedic surgery (OR 1.45, 95% CI 1.13, 1.84), and living with others (versus alone; OR 1.26, 95% CI 0.99, 1.61).
Conclusion
This first US population-based case-control study of risk factors for revision of primary THR showed that younger, taller, and heavier patients and those receiving a cemented femoral component had greater likelihood of revision THR over twelve-year follow-up. Effects of age and body size on revision risk should be addressed by clinicians with patients considering primary THR.
Total hip replacement (THR) is a highly effective intervention to improve pain and function in the hip affected by advanced arthritis. More than 280,000 primary THRs are performed every year in the US.1 However, some patients experience symptomatic prosthesis failure due to a range of problems, including loosening, infection, or dislocation. A subset of these patients subsequently undergoes revision surgery. Prior estimates place the revision risk at about 1% per year.2, 3 Due in part to the growing number of primary procedures, revision THR is now performed on over 50,000 people every year in the United States at a direct cost exceeding $1 billion.1
Prior studies identify male sex,4, 5 younger age,4–7 high comorbidity score,4, 6, 8, 9 and uncemented prostheses5 as risk factors for revision of primary THR. Low surgeon THR procedure volume has also been cited as a risk factor, but only in the early period after revision.8, 10 Additional risk factors have been associated with specific indications for revision, such as infection.11–15 Study of revision risk in primary THR is challenging because it is a relatively infrequent outcome that can occur a decade or more after the primary procedure. An additional methodological challenge is the high mortality rate among older patients, who often face a higher risk of death than of revision.2, 16
The objective of this study was to evaluate the risk factors for revision of primary THR in the US Medicare population over twelve years of follow-up. We hypothesized that younger age, male sex, and greater biomechanical load (as represented by height and weight) would be associated with revision risk.
PATIENTS AND METHODS
Study Design
We performed a nested case-control study of risk factors for revision of hip replacement.
Selection of Patients
A sample of 46,877 Medicare beneficiaries in 29 US states who were reported to have undergone primary THR surgery between 7/1/1995 and 6/30/1996 were followed in annual Medicare Provider Analysis and Review (MedPAR) billing records through the end of 2008 to identify hospital admissions for revision THR surgery. The states were chosen to provide a wide geographic range across the US. The surgery procedure code identifying revision surgery was 8153 until September, 2005, when new ICD-9-CM procedure codes of 0070 through 0073 were added for revision THR. We selected all patients with a code for revision hip replacement surgery, which yielded 3,647 putative cases. For each of these potential cases, we randomly selected one control from patients who had primary THR in the same state and were alive and not revised as of the case revision surgery date. All patients were censored at the date of a second total hip replacement (in order to reduce the confusion caused by revisions performed on the contralateral rather than the index hip). Cases were eligible to be controls until two years prior to their revision surgery, since this was considered a conservative estimate for the first appearance of symptoms ultimately leading to revision.
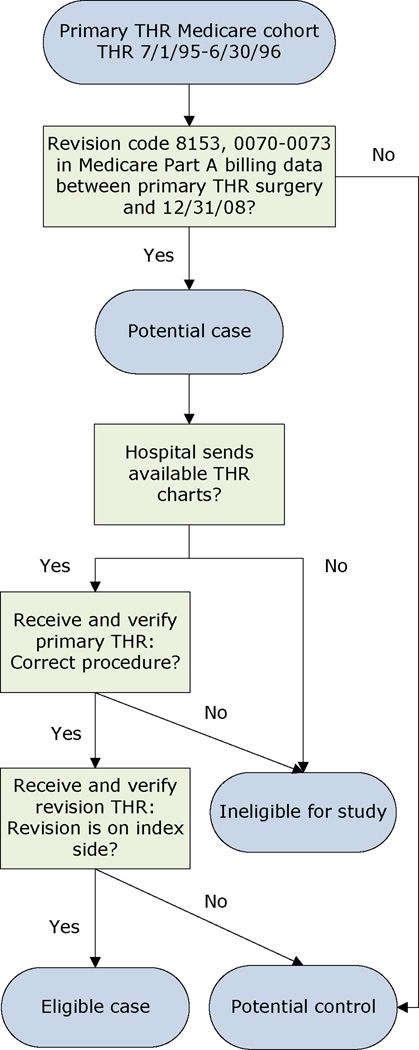
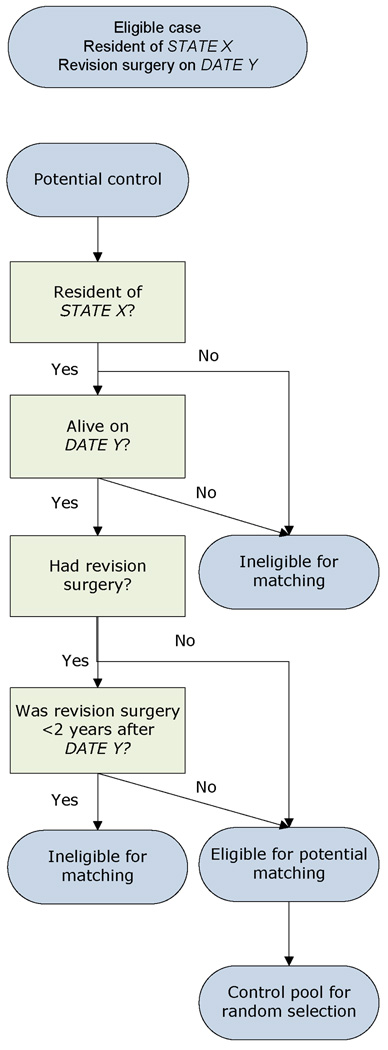
Identification of Cases and Controls
For each of the 3,647 potential cases and 3,647 controls, patient medical records for the dates of the primary THR surgery were requested from the hospitals. For each of the cases, patient medical records for the date of the revision surgery were also requested. Ineligible cases were those whose primary or revision record was inaccessible, whose index surgery was not a primary THR, whose putative revision surgery was shown on the medical record not to be a revision THR, whose primary and revision surgeries were on opposite sides, or whose record showed an ineligible indication for THR (e.g., tumor, acute fracture of hip/pelvis or history of hip infection). Ineligible controls were those whose index surgery was not a primary THR or whose record indicated an ineligible indication for THR. Cases matched to controls whose records were ineligible or unobtainable were then matched to other eligible controls from providers in the same state. Figures 1 and 2 show the steps used to select matched cases and controls.
Figure 1.
Selection of eligible cases and potential controls.
Figure 2.
Random selection of one matched control per case.
Medical Record Review
The medical charts were abstracted by trained medical abstractors at Information Collection Enterprises in York, PA. Data collected included demographic information, surgical data to determine case eligibility, patient history, lifestyle factors, and operative variables.
Data Elements
Demographic data included age at surgery (dichotomized as 65–75 and >75 years), sex, race (categorized as white or non-white), Medicaid buy-in (a variable that identifies subjects with very low income), and zip code at time of surgery (for classification of rural, suburban or urban residence).
Patient history variables, reflecting patient status prior to the primary THR, included prior surgery on index and non-index hip, other major musculoskeletal surgeries, underlying disease leading to THR, height, weight, and comorbidities. The Charlson Comorbidity Score17, 18 was calculated from comorbidities documented in the medical chart at the time of primary THR and was dichotomized as 0–1 or >1 for the analysis. Body mass index (BMI) was calculated from height and weight (kilogram/meter2) at time of THR primary surgery and divided into tertiles (<25 / 25–30 / ≥ 30). Height and weight were divided into by tertiles by sex (males: height in inches ≤68 / 69–71 / ≥72 and weight in pounds ≤177 / 178–203 / ≥204; females: height in inches ≤63 / 64–65 / ≥66 and weight in pounds ≤145 / 146–173 / ≥174).
Lifestyle factors ascertained at time of primary THR surgery included smoking habits, both current and past, alcohol use, and living situation (living alone vs. living with others).
Operative variables pertaining to the primary THR included type of anesthesia (general/spinal/epidural), American Society of Anesthesiologists Physical Status Scores (ASA Score), duration of the primary THR surgery (<2.5 hrs vs. ≥2.5 hrs), and acetabular and femoral prosthesis fixations (cemented or cementless).
STATISTICAL METHODS
Comparison of available and unavailable records
We compared characteristics (ascertained from Medicare claims data) of subjects whose records were obtained from hospitals with subjects whose records were not obtained using the chi-square test for categorical variables and the t-test for continuous factors.
Main analysis with matched data
The goal of the analysis was to identify factors associated with revision of a THR. The analysis cohort consisted of those with complete data for the factors being analyzed. Bivariate associations between potential risk factors and revision status were evaluated with McNemar’s chi-square test and conditional logistic regression. Variables associated with revision status with p≤0.05 were advanced to multivariate conditional logistic regression models.
Sensitivity analysis
The predictor variables with the most missing data were height and weight. Subjects with missing data on one or both of these variables were no more likely to have had a revision (i.e., to be a case) than subjects with complete data on these variables (chi-square p=0.61). Weight and height were moderately correlated (r = 0.39 in males and 0.24 in females). These observations support the imputation we performed with the SAS MI and MIANALYZE procedures, which assume that data are missing at random and that the probability of missing values for a given variable is conditioned on the other variables in the analysis.
Unmatched analyses were also performed predicting case status using logistic regression, adjusting for covariates in the final model plus state of hospital for the primary THR surgery. For one of these analyses, a four-category variable was created representing combinations of cemented and uncemented acetabular and femoral components.
All analyses were done using SAS version 9.1 for UNIX (SAS Institute, Cary, NC (2003)).
RESULTS
Description of Study Sample
Record accrual
From the 3,647 potential cases for whom medical records were requested, 836 (23%) eligible cases (pairs of primary and revision records) were obtained. Of the unavailable potential cases, hospitals did not respond to 56% of our requests and hospitals were not able to obtain the medical record in 36%. Another 7% of subjects were ineligible because revision surgery was performed on the non-index hip. Reasons reported by hospitals for not obtaining and/or sending the records for abstraction included destruction of records (47%), need for patient consent (14%), inability to find record (13%), hospital refusal (10%), as well as hospital closure (7%), cost (5%), and IRB issues (4%).
An analysis comparing eligible cases and controls whose records were obtained to potential cases and controls whose records were not obtained suggested that our study sample was similar to the patients whose records were unavailable with respect to age, sex, race, and comorbidity (Appendix Table 1). However, subjects who were included in the analysis were less likely to be operated upon at a high-volume hospital (> 100 THR/year in Medicare population) than subjects whose records were not obtained. This pattern was observed for both cases and controls.
Characteristics of analysis cohort
The sample for the main analysis included the 719 case-control pairs with complete data for the predictors of interest. The average age of these 1,438 patients was 74.0 years (SD±5.8), 39% were male, 34% had BMI ≥ 30, 54% had at least two Charlson comorbidities, 5% had Medicaid coverage, and 5% were non-white.
Characteristics of cases at time of revision THR
Case medical records showed multiple clinical indications for revision of the total hip replacement. The reasons cited, in order of frequency, were: loosening of the prosthesis (51%), repeated dislocations (38%), polyethylene liner wear (14%), osteolysis (11%), periprosthetic fracture of the femur or pelvis (9%) and infection of the THR (5%). When each failure mechanism was stratified by time to revision (≤ 2 years vs. > 2 years), dislocations were associated with earlier revisions (p<0.0001), while loosening, osteolysis, liner wear and periprosthetic fracture were associated with later revisions (p<0.0001, p<0.0001, p<0.0001 and p=0.04, respectively). The data did not suggest that the risk of revision for infection varied over time.
Results of Bivariate Analysis
Cases were significantly younger than controls, with 67% of the cases vs. 55% of the controls between 65 and 75 years old, yielding an OR for comparison with those over 75 of 1.7 (95% CI 1.4, 2.1). Cases were significantly more likely than controls to live with others as opposed to alone at the time of primary THR (OR 1.4, 95% CI 1.1, 1.7). Cases were also more likely than controls to have had prior contralateral total hip replacement (OR 1.4, 95% CI 1.1, 1.8), to have had prior major musculoskeletal surgery (OR 1.5, 95% CI 1.2, 1.9), to have had a cemented (as opposed to uncemented) femoral component implanted at the index THR (OR 1.3, 95% CI 1.0, 1.7), to be obese (BMI ≥30) (OR 1.8, 95% CI 1.4, 2.4), and to be in the highest tertile for height (1.6, 95% CI 1.3, 2.1) and weight (2.0, 95% CI 1.6, 2.7) (Table 1). We did not observe clinically or statistically meaningful differences between cases and controls in a range of preoperative and operative features including sex, race, Charlson comorbidity count, Medicaid eligibility, residence population density, smoking status, alcohol intake, hospital and surgeon annual primary THR volume, ASA class at primary surgery, type of anesthesia, fixation of acetabular component, 6/8 prosthesis manufacturers, and surgery duration (for full results of the bivariate analysis, see Appendix Table 2).
Table 1.
Predictors of THR revision in bivariate and multivariate analyses*
| Factor | Cases N (%) |
Controls N (%) |
Crude OR (95% CI) |
Adjusted OR (95% CI) |
|
|---|---|---|---|---|---|
| Age | ≤ 75 | 485 (67) | 392 (55) | 1.73 (1.39, 2.15) | 1.52 (1.20, 1.92) |
| > 75 | 234 (33) | 327 (45) | 1.0 | 1.0 | |
| Sex | Male | 294 (41) | 270 (38) | 1.14 (0.93, 1.40) | ------- |
| Female | 425 (59) | 449 (62) | 1.0 | ------- | |
| Living status | With others | 519 (72) | 469 (65) | 1.39 (1.11, 1.74) | 1.26 (0.99, 1.61) |
| Alone | 200 (28) | 250 (35) | 1.0 | 1.0 | |
| Prior contralateral THR | Yes | 194 (27) | 147 (20) | 1.43 (1.12, 1.83) | 1.36 (1.05, 1.76) |
| No | 525 (73) | 572 (80) | 1.0 | 1.0 | |
| Other orthopedic surgery | Yes | 247 (34) | 188 (26) | 1.49 (1.18, 1.88) | 1.45 (1.13, 1.84) |
| No | 472 (66) | 531 (74) | 1.0 | 1.0 | |
| Height (by sex) | Tertile 3 | 219 (30) | 162 (23) | 1.62 (1.25, 2.10) | 1.40 (1.06, 1.85) |
| Tertile 2 | 233 (32) | 232 (32) | 1.21 (0.96, 1.55) | 1.10 (0.85, 1.43) | |
| Tertile 1 | 267 (37) | 325 (45) | 1.0 | 1.0 | |
| Weight (by sex) | Tertile 3 | 282 (39) | 195 (27) | 2.04 (1.56, 2.67) | 1.66 (1.24, 2.22) |
| Tertile 2 | 231 (32) | 243 (34) | 1.31 (1.01, 1.69) | 1.12 (0.85, 1.48) | |
| Tertile 1 | 206 (29) | 281 (39) | 1.0 | 1.0 | |
| Cemented femur | Yes | 555 (77) | 521 (72) | 1.31 (1.02, 1.68) | 1.44 (1.10, 1.87) |
| No | 164 (23) | 198 (28) | 1.0 | 1.0 | |
Only statistically significant (p≤.05) predictors of revision in bivariate analyses were included in multivariate models. For a full listing of all factors studied, see Appendix Table 2.
Results of Multivariate Analysis
We built multivariate conditional logistic regression models predicting revision using variables statistically significantly associated with case status in unadjusted models. With the exception of the prosthesis manufacturer variables, all variables -- including age ≤75 (OR 1.5, 95% CI 1.2, 1.9), living with others (OR 1.3, 95% CI 1.0, 1.6), prior contralateral THR (OR 1.4, 95% CI 1.1, 1.8), prior musculoskeletal surgery (OR 1.4, 95% CI 1.1, 1.8), cemented femoral component (OR 1.4, 95% CI 1.1, 1.9), height in the highest tertile (OR 1.4, 95% CI 1.1, 1.9) and weight in the highest tertile (OR 1.7, 95% CI 1.2, 2.2) -- remained independent significant predictors of revision (Table 1).
Results of Sensitivity Analyses
Alternative models replacing weight in tertiles with BMI in tertiles yielded qualitatively the same results as the main model, with height in the highest tertile as well as BMI in the highest tertile being significantly associated with revision risk (OR 1.7, 95% CI 1.3, 2.2 for height; OR 1.7, 95% CI 1.3, 2.3 for BMI). However, in models replacing height in tertiles with BMI in tertiles, BMI was no longer statistically significantly associated with revision risk. The main analysis was also repeated after excluding the 35 case-control pairs in which infection was listed as an indicator for revision. The results remained unchanged.
We repeated the multivariate modeling on all 836 case-control pairs after multiple imputation of missing values for variables with incomplete data (living status (1% missing), fixation of femoral component (3% missing), weight (7% missing), height (11% missing), and BMI (11% missing)). The set of pooled estimates based on these models was qualitatively the same as the results of the main analysis, with odds ratios for the predictor variables differing between the models by no more than 7%.
The results in an unmatched multivariate analysis were nearly identical to the results of the primary matched analysis, with odds ratios for the predictor variables differing between the two analyses by no more than 5%. In a secondary unmatched analysis, a variable representing combinations of cemented and uncemented femoral and acetabular components was substituted for the cemented femoral component variable. The category for uncemented femoral and cemented acetabular components was excluded since only eight patients received this type of prosthesis. In the analysis, those with cemented femoral and acetabular components had greater risk for revision than subjects with uncemented femoral and acetabular components (OR 1.5, 95% CI 1.0, 2.4) and those with cemented femoral and uncemented acetabular components also had greater risk for revision than those with uncemented femoral and acetabular components (OR 1.5, 95% CI 1.1, 1.9). Finally, we found no evidence of an interaction between age at the time of surgery and cementing of the femoral component on the risk of revision.
DISCUSSION
We used a nested case-control study to examine predictors of revision risk in a cohort of Medicare patients who received primary THR surgery between 7/1/1995 and 6/30/1996. We followed the patients in Medicare files through 12/31/2008 and collected data on potential predictors through medical record review. We found the following risk factors for failure leading to revision THR surgery: younger age (65–75 years old versus > 75), greater height, greater weight, a cemented femoral component, prior contralateral primary THR surgery, other orthopedic surgery, and living with others (as opposed to living alone) at the time of the primary THR. We also found that greater BMI was predictive of revision with similar tertile odds ratios to those of weight. Reasons for revision surgery in our case sample were similar to those reported previously in the literature.19
In contrast to earlier studies of long-term outcomes of total hip replacement utilizing Medicare data, the cases in our study were verified to be revisions of the index primary THR by subsequent medical chart review. This insures a more accurate case determination and eliminates the substantial error inherent in Medicare data, which lacks information on laterality.20
Similar to earlier studies, we found that younger age, in our case 65–75 years old compared to >75, is associated with higher revision risk.4–7 We also found that a prior contralateral primary THR surgery21 or other musculoskeletal surgery is associated with elevated risk of revision. These factors may be surrogates for accessibility to health care, greater willingness to undergo surgery, more favorable expectations of THR surgery, or may reflect orthopedic comorbidity. Similarly, the suggestion in our data that living with others leads to higher risk of revision surgery may be due to the fact that a social support network facilitates transportation and rehabilitation post surgery.
The literature regarding the revision risk of cemented and uncemented prostheses is discordant. Since 92% of both patients and controls in our study had uncemented acetabular components, we were unable to study the effect of acetabular fixation. However, we found that use of cemented femoral components was associated with increased revision risk. In an unmatched sensitivity analysis, we found no evidence of an interaction between age at the time of surgery and cementing of the femoral component on the risk of revision. Furthermore, the same increased risk for cemented femoral components was found whether the acetabular component was cemented or not. In contrast, an analysis of revision following cemented and uncemented primary THR in New Zealand for cases from 1999–2006 found similar rates of revision for cemented and uncemented femoral components, except in patients over 75 years of age where revision rates for those with cemented components were significantly lower.22 Also, in a meta-analysis of studies from 1991 to 2004, Morshed et al.23 found that cemented THR had longer implant survival than uncemented in large subsets of study populations, but they indicate that a more recent year of study publication was associated with lower revision risk for uncemented fixation relative to cemented fixation. The relative utilization of cemented and uncemented fixation for THR varies widely throughout the world. For example, the rate of fully cemented THR in Canada in 2006–2007 was only 3% 24, whereas the Swedish rate in 2009 for cemented THR was about 70% and cemented prostheses were the preferred choice for older patients (above mean age 70).25 Geographic differences in fixation preferences and patient populations, combined with the ongoing development of new techniques and materials make this issue difficult to evaluate.
We found a strong association between risk of THR revision surgery and height, weight and BMI. These findings contrast with recent studies reporting no significant association between revision risk and BMI26–29 or body weight.26 Lubbeke et al. reported an increased risk of revision for obese patients compared to non-obese, although the risk was not statistically significant: HR 2.2 (95% CI 0.9–5.3).28 Two studies did report lower post-operative functional outcomes for obese patients, but did not find an elevated risk of revision.27, 29 One possible explanation is that obesity may affect revision risk differently in younger and older age groups. Our study was limited to patients at least 65 years old at the time of the primary THR. It may be that in younger patients, obesity both loads the joint (increasing risk of revision) and also reduces physical activity level (reducing risk), while in older patients, such as those we studied, physical activity may be low irrespective of weight. The lower percentages of obesity observed in European studies, such as those of Lubbeke et al. (24%)28 and Haverkamp et al. (9%),26 as contrasted with our cohort (31% obese and 12% morbidly obese (BMI≥40)), suggest that some earlier studies may have lacked sufficient power to show revision risk from BMI or body weight. We note that height had an effect on revision that was independent of weight or BMI. This suggests that beyond mass or obesity, the size of the individual’s frame affects revision risk. This effect could be due to increased loads and moment arms associated with larger-framed persons.
We note that revision is not a perfect proxy for failure of primary THR. Patients with symptomatic THR failure may not seek care, may seek care but not be offered revision surgery, or may be offered the option and decline. These outcomes could arise from patient comorbidities that make surgery less advisable or from patient preferences for undertaking the procedure upon consideration of its potential risks and benefits. For example, older patients may experience lower rates of prosthesis failure due to lower activity levels, but they may also be less likely to undergo revision for prosthesis failure than younger patients due to concerns about the safety of another major surgery. Similarly, the associations of prior contralateral primary THR, other musculoskeletal surgery, and living alone, as noted above, may relate more to the decision of whether to have revision for a failed THR than to the risk of failure per se. We note as well that other musculoskeletal surgery may be a marker for other orthopedic comorbidity, which in turn may be associated with revision risk.
The results of our study should be viewed in light of several limitations. Since our study focused on persons at least 65 years old at the time of index THR in 1995–1996, we are unable to make any conclusions about revision risk in patients younger than 65, who comprise the fastest-growing group of THR recipients in the U.S.1, 30 Death is an important competing risk in an elderly cohort. Indeed, 50% of our cohort had died by the end of the twelve-year follow-up period. However, since each control had to be alive at the time of the case’s revision, death did not arise as a competing risk in our analysis. Our ability to investigate clinical factors relating to failure leading to revision was limited by the amount of detail and lack of uniformity present in the medical charts collected from many different hospitals, as well as by the unavailability of x-ray analysis. Because we asked hospitals for medical records up to fifteen years old, some hospitals were unable to meet our requests due to factors such as hospital closings or mergers and destruction or loss of records. While our cases were similar to patients whose charts were unavailable in most respects, cases were much more likely to have had their primary and revision surgeries in the same hospital than patients whose charts were unavailable. This reflects the higher likelihood of obtaining both the case primary and case revision records when both surgeries occurred in the same hospital. This could imply a selection of a less mobile population, or of those more satisfied with their primary THR surgery. In addition, the potential for bias due to unmeasured factors and missing data remains an unavoidable limitation of this study. Finally, the advantage of long-term follow-up data such as ours must be weighed against the fact that trends in clinical practice and patient demographics are always changing.
This study of a Medicare population emphasizes that age between 65 and 75 years and greater height and weight at the time of THR are potent risks for failure of THR leading to revision surgery. Since both height and weight are independent risk factors in multivariate models, the risk factor for revision may not be obesity per se, but body size, potentially a surrogate for the biomechanical load borne by the implant. This study also identifies prior THR and other orthopedic surgeries as risk factors, possibly highlighting a connection of access to health care or favorable expectations of surgery as motivators for revision surgery. More detailed prospective studies would facilitate interpretation of these findings. We conclude that the effects of age and larger body size on revision risk should be included in discussions between surgeons and patients about the potential risk of failure of primary THR.
Supplementary Material
SIGNIFICANCE AND INNOVATIONS.
-
▪
Over 280,000 primary and 50,000 revision total hip replacements are performed annually in the US.
-
▪
This is the first US population-based study of demographic, clinical and operative risk factors for revision of primary THR.
-
▪
In this nested case-control study with twelve years of follow-up younger age and greater body size (both weight and height) were associated with revision risk, as was use of a cemented femoral component.
Acknowledgments
Grant support: NIH P60 AR 47782, NIH K24 AR 057827
REFERENCES
- 1.HCUP Nationwide Inpatient Sample. United States Department of Health & Human Services; 2009. Agency for Healthcare Research and Quality. [Google Scholar]
- 2.Katz JN, Wright EA, Wright J, Malchau H, Mahomed NN, Stedman M, et al. Twelve-year risk of revision following primary total hip replacement in the US Medicare population. Journal of Bone and Joint Surgery. 2011 doi: 10.2106/JBJS.K.00569. (provisionally accepted for publication). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corbett KL, Losina E, Nti AA, Prokopetz JJ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: a systematic review. PLoS One. 2010;5:e13520. doi: 10.1371/journal.pone.0013520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnsen SP, Sorensen HT, Lucht U, Soballe K, Overgaard S, Pedersen AB. Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms. J Bone Joint Surg [Br] 2006;88-B:1303–1308. doi: 10.1302/0301-620X.88B10.17399. [DOI] [PubMed] [Google Scholar]
- 5.Hailer NP, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthopaed. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res. 2010;468:3070–3076. doi: 10.1007/s11999-010-1399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El Masri F, Kerboull L, Kerboull M, Courpied JP, Hamadouche M. Is the so-called 'French paradox' a reality?: long-term survival and migration of the Charnley-Kerboull stem cemented line-to-line. J Bone Joint Surg Br. 2010;92:342–348. doi: 10.1302/0301-620X.92B3.23151. [DOI] [PubMed] [Google Scholar]
- 8.Paterson JM, Williams JI, Kreder HJ, Mahomed NN, Gunraj N, Wang X, et al. Provider volumes and early outcomes of primary total joint replacement in Ontario. Can J Surg. 2010;53:175–183. [PMC free article] [PubMed] [Google Scholar]
- 9.Soohoo NF, Farng E, Lieberman JR, Chambers L, Zingmond DS. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2363–2371. doi: 10.1007/s11999-010-1354-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fender D, van der Meulen JHP, Gregg PJ. Relationship between outcome and annual surgical experience for the Charnley total hip replacement. J Bone Joint Surg [Br] 2003;85-B:187–190. doi: 10.1302/0301-620x.85b2.12759. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen AB, Svendsson JE, Johnsen SP, Riis A, Overgaard S. Risk factors for revision due to infection after primary total hip arthroplasty. A population-based study of 80,756 primary procedures in the Danish Hip Arthroplasty Registry. Acta Orthop. 2010;81:542–547. doi: 10.3109/17453674.2010.519908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pedersen AB, Mehnert F, Johnsen SP, Sorensen HT. Risk of revision of a total hip replacement in patients with diabetes mellitus: a population-based follow up study. J Bone Joint Surg Br. 2010;92:929–934. doi: 10.1302/0301-620X.92B7.24461. [DOI] [PubMed] [Google Scholar]
- 13.Dale H, Hallan G, Espehaug B, Havelin LI, Engesaeter LB. Increasing risk of revision due to deep infection after hip arthroplasty. Acta Orthop. 2009;80:639–645. doi: 10.3109/17453670903506658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ong KL, Kurtz SM, Lau E, Bozic KJ, Berry DJ, Parvizi J. Prosthetic joint infection risk after total hip arthroplasty in the Medicare population. J Arthroplasty. 2009;24:105–109. doi: 10.1016/j.arth.2009.04.027. [DOI] [PubMed] [Google Scholar]
- 15.Thillemann TM, Pedersen AB, Mehnert F, Johnsen SP, Soballe K. Use of diuretics and risk of implant failure after primary total hip arthroplasty: a nationwide population-based study. Bone. 2009;45:499–504. doi: 10.1016/j.bone.2009.04.247. [DOI] [PubMed] [Google Scholar]
- 16.Gillam MH, Ryan P, Graves SE, Miller LN, de Steiger RN, Salter A. Competing risks survival analysis applied to data from the Australian Orthopaedic Association National Joint Replacement Registry. Acta Orthop. 2010;81:548–555. doi: 10.3109/17453674.2010.524594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46:1075–1079. doi: 10.1016/0895-4356(93)90103-8. discussion 81–90. [DOI] [PubMed] [Google Scholar]
- 19.Clohisy J, Calvert G, Tull F, McDonald D, Maloney WJ. Reasons for revision hip surgery: a retrospective review. Clin Orthop Relat Res. 2004;429:188–192. doi: 10.1097/01.blo.0000150126.73024.42. [DOI] [PubMed] [Google Scholar]
- 20.Katz JN, Wright EA, Baron JA, Corbett KL, Nti A, Malchau H, et al. Predictive value of Medicare claims data for identifying revision of index hip replacement was modest. J Clin Epid. 2011;64:543–546. doi: 10.1016/j.jclinepi.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lie SA, Engesaeter LB, Havelin LI, Gjessing HK, Vollset SE. Dependency issues in survival analyses of 55,782 primary hip replacements from 47,355 patients. Stat Med. 2004;23:3227–3240. doi: 10.1002/sim.1905. [DOI] [PubMed] [Google Scholar]
- 22.Hooper GJ, Rothwell AG, Stringer M, Frampton C. Revision following cemented and uncemented primary total hip replacement. Journal of Bone and Joint Surgery. 2009;91-B:451–458. doi: 10.1302/0301-620X.91B4.21363. [DOI] [PubMed] [Google Scholar]
- 23.Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM., Jr Comparison of cemented and uncemented fixation in total hip replacement. A meta-analysis. Acta Orthop. 2007;78:315–326. doi: 10.1080/17453670710013861. [DOI] [PubMed] [Google Scholar]
- 24.Hip and knee replacements in Canada -- Canadian Joint Replacement Registry (CJRR) 2008–2009 annual report. Ottawa, Ontario: CIHI; 2009. Information CIfH. [Google Scholar]
- 25.Department of Ortopaedics SUH. 2010. 2009 TSHARAR. ed. [Google Scholar]
- 26.Haverkamp D, de Man FH, de Jong PT, van Stralen RA, Marti RK. Is the long-term outcome of cemented THA jeopardized by patients being overweight? Clin Orthop Relat Res. 2008;466:1162–1168. doi: 10.1007/s11999-008-0129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jackson MP, Sexton SA, Yeung E, Walter WL, Walter WK, Zicat BA. The effect of obesity on the mid-term survival and clinical outcome of cementless total hip replacement. J Bone Joint Surg Br. 2009;91:1296–1300. doi: 10.1302/0301-620X.91B10.22544. [DOI] [PubMed] [Google Scholar]
- 28.Lubbeke A, Stern R, Garavaglia G, Zurcher L, Hoffmeyer P. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum. 2007;57:327–334. doi: 10.1002/art.22542. [DOI] [PubMed] [Google Scholar]
- 29.Yeung E, Jackson M, Sexton S, Walter W, Zicat B. The effect of obesity on the outcome of hip and knee arthroplasty. Int Orthop. 2010;35:929–934. doi: 10.1007/s00264-010-1051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh JA, Vessely MB, Harmsen WS, Schleck CD, Melton LJ, 3rd, Kurland RL, et al. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969–2008. Mayo Clin Proc. 2010;85:898–904. doi: 10.4065/mcp.2010.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.