Abstract
The pathogenesis and progression of cardiovascular diseases are thought to be exacerbated by stress. Basic research indicates that the Transcendental Meditation® technique produces acute and longitudinal reductions in sympathetic tone and stress reactivity. In adolescents at risk for hypertension, the technique has been found to reduce resting and ambulatory blood pressure, left ventricular mass, cardiovascular reactivity, and to improve school behavior. Research on adults with mild or moderate essential hypertension has reported decreased blood pressure and reduced use of anti-hypertensive medication. The technique has also been reported to decrease symptoms of angina pectoris and carotid atherosclerosis, to reduce cardiovascular risk factors, including alcohol and tobacco use, to markedly reduce medical care utilization for cardiovascular diseases, and to significantly decrease cardiovascular and all-cause morbidity and mortality. These findings have important implications for inclusion of the Transcendental Meditation program in efforts to prevent and treat cardiovascular diseases and their clinical consequences.
®Transcendental Meditation and TM are trademarks registered in the US. Patent and Trademark Office, licensed to Maharishi Vedic Education Development Corporation and are used with permission.
Keywords: Adolescents, meditation, blood pressure, cardiovascular disease, randomized clinical trial, stress reduction, mortality
INTRODUCTION
The burden of cardiovascular (CV) disease (CVD) remains high, with more than 2200 Americans dying of CVD every day, and 813,804 Americans having died of CVD in 2007, making it the leading cause of death in the US. The cost burden is an estimated $286 billion, 17% of national health expenditures [1]. These costs are expected to triple by 2030 [2]. Like most other diseases, CVD is multi-factorial in nature. Well-established preventable CVD risk factors include dyslipidemia [3, 4], high blood pressure (BP) [5], smoking [6], psychological distress/angry temperament [7], metabolic syndrome [8], obesity [9], stress [10] and physical inactivity [11]. Exposure to CVD risk factors during childhood and adolescence has been associated with the development of atherosclerosis later in life [12, 13]. Modifying these risk factors by changes in lifestyle is expected to have beneficial effects on lowering risk of CVD [14].
Environmental and psychosocial stress plays a significant role in the development of essential hypertension (EH) by acting through both acute and long-term BP control mechanisms [15, 16]. Stress is defined as a process in which environmental demands tax or exceed the adaptive capacity of an organism, resulting in physiological changes that, over time, may place the individual at risk for disease development [17]. The biobehavioral model of stress-induced hypertension depicted in Fig. (1) incorporates both the acute phase of the stress response, which results in a rapid BP increase, and the chronic phase of the stress response which acts to maintain elevated BP levels as long as physiologically needed to maintain homeostasis. Stress has been hypothesized as contributing to the development of EH and CVD via a pathway of exaggerated cardiovascular reactivity [15, 16, 18] and to EH also by chronic sympathetic nervous system (SNS) activation [19]. The acute phase of the stress response involves complex neuroendocrine changes characterized by increased sympathetic activation [20]. Animal and human studies have demonstrated that exposure to chronic and acute stress augments SNS and hypothalamic-pituitary-adrenal activity resulting in increased levels of catecholamines, including norepinephrine, and of cortisol [21]. This results in a rapid rise in BP predominantly due to increased vasoconstriction [22], which increases total peripheral resistance [23].
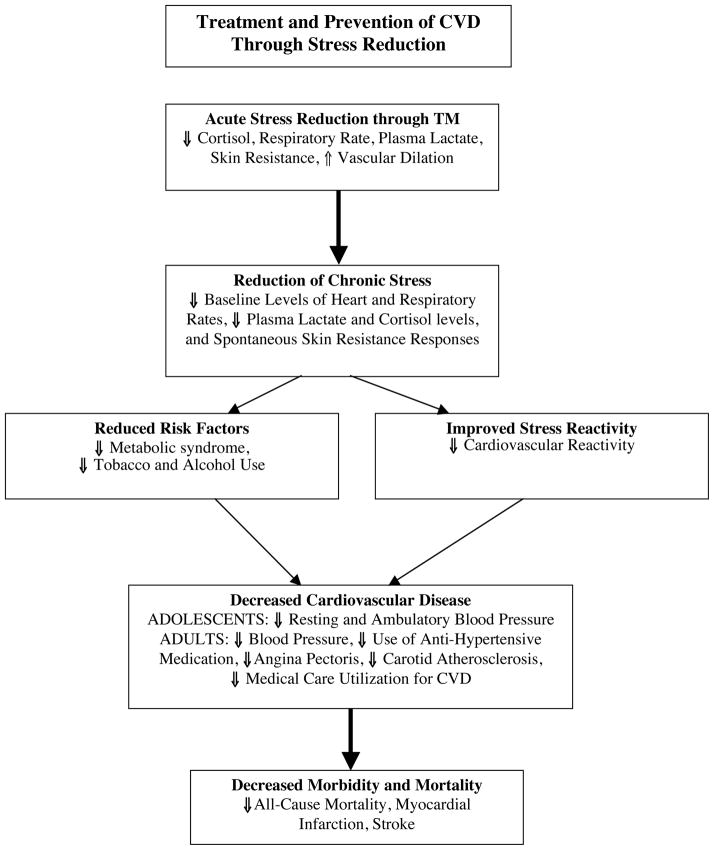
Fig. 1. Treatment and prevention of CVD through stress reduction.
A model of the Transcendental Meditation® (TM) program’s effects on hypertension and CVD as reviewed in this paper is presented. Chronic environmental and psychosocial stresses, and genetic predisposition, contribute to an increase in acute stress-induced SNS arousal, resulting in increased neurohormonal activity and hypothalamic-pituitary-adrenocortical axis dysregulation. Such changes result in greater BP responsivity to the stress, vasoconstriction and increased BP levels. Reduction of acute and chronic stress via TM practice reduces SNS activity resulting in reduced BP reactivity to acute stress. Over time, due to decreased CV reactivity to acute events, there is reduced load upon the heart, resulting in decreased BP levels, thereby helping to prevent EH and CVD.
TREATMENT AND PREVENTION OF CVD THROUGH STRESS REDUCTION
Exposure to stress results in SNS-mediated increases in BP to cope with the immediate need for an increased blood supply to the brain and body. It is well established that SNS activation in turn activates the renin-angiotensin-aldosterone system, which includes release of the potent vasoconstrictive hormone, angiotensin II, which contributes to the acute rise in BP [24]. Increased peripheral vasoconstriction has been implicated in the early development of EH [25] and elevated total peripheral resistance is frequently the underlying hemodynamic mechanism responsible [26–28].
The recurrent and/or sustained exaggerated increases in BP responses to stress are associated with concomitant increases in cardiac and vascular wall tension [29, 30]. It is hypothesized that over time this leads to secondary CV structural adaptation, that is, vascular and ventricular remodeling to help normalize wall tension [20, 29, 31]. An early sign of ventricular remodeling is increased left ventricular mass (LVM), which may lead to left ventricular hypertrophy, the strongest predictor of CV morbidity and mortality, other than advancing age [32–34]. Research findings have shown that BP reactivity in youth predicts left ventricular hypertrophy [35, 36], and although not entirely consistent [37], several prospective studies observed that BP reactivity also predicts EH [38–41].
Exaggerated CV reactivity to stress has been hypothesized [15, 16, 18] to play a particularly significant role in the development of EH due to exposure to both chronic and acute psychosocial and environmental stress (e.g., verbal/physical conflict with law/authority figures or family members, racism, inadequate economic resources, social disorganization, lower education and occupational status) [42–44]. Over the past decade pediatric studies found that exaggerated BP reactivity to laboratory behavioral stressors is an independent predictor of increases in measures of pre-clinical CVD [45].
Chronic environmental stress is not easily altered. However, our model proposes that the effects of stress can be ameliorated via behavioral stress reduction, i.e., changing how the individual responds to stressors to reduce their negative impact on health. An individual’s acute CV responses to stress can be moderated by numerous psychological/lifestyle factors. For example, anger and hostility have been shown to be related to CV reactivity and a wide range of physical health problems including EH and CVD [46–51], Similarly, coping styles (i.e., anger suppression, anger expression), perceived environmental stress (i.e., general stress levels, stressful life events, unfair treatment), environmental noise [52], and coping resources (e.g., family functioning, social support, stress reduction skills) are implicated in the SNS pathway. These variables have been associated with resting BP and/or CV reactivity in adolescents and/or young adults [53–57].
Evidence for the efficacy of certain non-pharmacologic approaches to preventing and controlling EH is compelling [58]. Clinical research, primarily in adults, has shown behavioral interventions to have great promise in reducing BP levels, improving stress-related coping skills, and alleviating psychosocial distress. The benefits of psychosocial-behavioral interventions with respect to hypertension and CHD have been demonstrated in a number of trials in adults [59, 60]. Stress reduction programs include those involving various kinds of meditation, cognitive behavioral skills training, yoga, and muscle relaxation. This review is limited to examining applications of the Transcendental Meditation (TM) program in prevention and treatment of EH and CVD.
There are several significant and unique aspects of the findings contained in this review. First and foremost is the wide range of subject populations involved, including minorities and youth. The research endeavor with TM is among the few extending behavioral stress reduction research to the adolescent population. Studies in youth are important for at least three reasons: (1) Studies have examined the effectiveness of a non-pharmacological therapy on BP reduction prior to the potentially confounding influences of sustained elevated BP that adversely affects the functioning of the organ systems later on in life [61]; (2) CVD etiology begins in childhood; epidemiological studies indicate that BP percentile rankings for age and sex track from late childhood through adolescence into adulthood [62–64]. Consequently, it is important to study individuals at a time when preventive strategies may still be effective prior to the development of pathology; and (3) until recently, the prevention of EH and CVD has not been a high priority in pediatric patients. As a result, little is known about the factors underlying pediatric EH. Therefore, given that the incidence of EH is increasing at an alarming rate, the prevention of EH and its consequences in the pediatric population has become an important area of investigation. Prevention of EH prior to the onset of target organ damage has been shown to be highly cost-effective [65].
The importance of this review lies in the concept that wide implementation of a non-pharmacological BP-reducing intervention could potentially have an enormous impact on public health. Even a small downward shift in the distribution of BP in the youth of a few mm Hg could potentially reduce the incidence of EH and related CVD [66, 67]. The results of this review will provide insight into what has now become a very timely and important issue.
THE TRANSCENDENTAL MEDITATION (TM) TECHNIQUE
The experience during a practice session of TM may be characterized by repeated cycles of movement of attention from the active thinking level to more abstract, subtle levels, attaining a quiescent state at the subtlest thinking level, and typically followed by movement of attention back to the more active levels [68]. During the practice of the TM technique, the ordinary thinking process is said to be “transcended” (or gone beyond) as the awareness gradually settles down and is eventually experienced as free of all mental content, remaining silently awake within itself, and producing a psychophysiological state of “restful alertness” [68]. These periods are said to be characterized by an experience of stillness, rest, stability, order, and by an absence of mental boundaries [69].
The TM technique falls within the category of “automatic self-transcending” because the practice allows the mind to effortlessly settle inward, beyond thought, to experience the source of thought, pure awareness, which is also known as transcendental consciousness [70, 71]. This is said to be the most silent and peaceful level of consciousness, which is associated with significantly increased EEG coherence and deep physiological rest [72], the benefits of which are thought to carry over into ordinary waking, dreaming and sleep [73].
Clinical reports indicate that the TM technique can easily be learned by individuals of any age, level of education, occupation, or cultural background [74, 75]. TM practitioners are instructed to sit in a comfortable position, with eyes closed. The technique is prescribed to be practiced 15 to 20 minutes twice daily, at a convenient time, once in the morning and once in the afternoon [76]. TM does not involve breath control procedures and no specific breathing pattern is prescribed [77].
The TM technique was derived from the Vedic tradition of India and was introduced into the West in the late 1950’s by the late Maharishi Mahesh Yogi [78]. Since then more than five million people worldwide have learned the technique [68]. Because the technique has been taught in a systematic and reliable way since its introduction, researchers have been assured that TM practitioners studied are using the identical procedure taught by instructors who have all had the same rigorous training, a distinct advantage over some other meditation techniques [79]. This unique feature has made widespread research on the TM program feasible [80] and by now more than 600 research studies have been conducted at more than 250 universities and research centers. These studies were published in over 100 journals in the past 40 years, making TM one of the most widely researched types of meditation, with six volumes of collected papers on TM published and a seventh in press [74, 75, 81].
SAFETY OF THE TM PROGRAM
The practice of TM is considered safe and it can be performed without adopting any specific system of spirituality or belief. No serious adverse events were reported in an efficacy review of 20 randomized controlled trials that included 397 experimentally treated subjects [82] and no safety concerns were raised in a report with 813 studies of meditation practices for health, including the TM technique [83]. The findings supported the safety and potential efficacy of meditative practices for treating certain illnesses, particularly in non-psychotic mood and anxiety disorders. Importantly, the NIH-sponsored clinical trials conducted with TM, as reviewed below, did not observe any adverse effects from TM practice.
NEUROPHYSIOLOGICAL EFFECTS OF TM PRACTICE
The neurological and physiological changes that take place through the practice of the TM technique have been studied since the 1970’s [84]. TM practice produces markedly higher alpha power in the frontal cortex and lower beta and gamma waves in the same frontal areas during practice, and creates greater alpha coherence between the left and right hemispheres and anterior and posterior brain areas [85–89]. Basic research has shown that alpha EEG coherence and synchrony supply the long-range integration of distal brain areas necessary for conscious awareness, attention, semantic processing, memory, learning, and mental health [90–92]. The significance of the findings on alpha EEG coherence and synchrony, observed during the TM technique, are that they appear to facilitate the neural communication and integration underlying its beneficial physiological, behavioral, and clinical effects [71].
Neuroimaging suggests that executive areas of the brain, the medial prefrontal cortex and anterior cingulate cortex, are involved in the generation of alpha activity induced by TM practice [93]. The patterns of cerebral-metabolic rate in a positron emission tomography study showed that compared to eyes-closed rest, TM practice increases frontal and parietal activity, corresponding to enhanced inner awareness and decreased thalamic activity, corresponding to decreased sensory processing as the mind settles inward during meditation [94]. TM practice also appears to increase functional connectivity in the Default Mode Network [95] which is believed to be the brain substrate for one’s sense of self and self-efficacy [96]. A meta-analysis has found that TM practice markedly increases self-actualization, which may be due to the increased connectivity in the Default Mode Network [97].
TM has been classified as a “state enlivening” approach. That is, the effects of practicing the technique are seen outside the practice and appear to accrue from physiological stress reduction and enlivening brain coherence. Many of the changes outside of meditation may even be incompatible with what one does during meditation (e.g., transcending mental activity during meditation results in improved intellectual performance, reaction time, and mindfulness in activity) [98, 99]. The state-enlivening approach of TM is in contradistinction to a “practice-makes-perfect” mechanism of other meditation techniques, such as focused attention, non-judgmental awareness, and compassion, whereby the benefits one wants to gain in activity are practiced during meditation.
PSYCHOLOGICAL AND PHYSIOLOGICAL MECHANISMS OF TM PRACTICE
The stress response involves complex neuroendocrine changes characterized by increased sympathetic activation. Acute physiological changes during the practice of TM are thought to be due to an integrated response [100], resulting in reduced baseline levels of stress hormones. A more adaptive response to stress is facilitated by the unique deep metabolic rest gained during the practice, in which the body’s homeostatic mechanism normalizes malfunctions in the system. A meta-analysis of 32 studies performed during and outside the TM technique found consistent evidence for reductions in SNS activation, as indicated by acute reductions during TM practice in respiratory rate and plasma lactate and increased basal skin resistance compared with control subjects sitting with eyes closed. There were also lower baseline levels of heart rate, respiratory rate, plasma lactate, and spontaneous skin resistance responses outside of meditation [101]. Related studies have found lower 24-hr levels of vanillylmandelic acid, indicating reduced turnover of norepinephrine and epinephrine, which also reflects reduced SNS activity due to TM practice. These factors may contribute to decreased contractility or reactivity of the vascular smooth muscle and to reduced total peripheral resistance, and subsequently reduced BP and CVD risk.
The hypothalamic-pituitary-adrenocortical axis provides mechanisms by which emotions and stress produce hormones that impact the body. For example, elevated baseline levels of plasma cortisol, a major stress hormone in humans, are associated with a greater prevalence of ischemic heart disease [102]. Prospective and randomized studies of the TM technique indicate that it has acute as well as longitudinal effects on reducing baseline cortisol, as well as average cortisol across stress sessions [103]. Other stress-related hormones of the hypothalamic-pituitary-adrenocortical axis, aldosterone and dehydroepiandrosterone sulfate, also change with TM practice. Aldosterone, a hormone that increases the absorption of sodium and water in the kidneys, decreases with TM practice, suggesting another mechanism by which the practice may reduce blood volume and normalize BP [104].
TM practice also increases levels of dehydroepiandrosterone sulfate [103], an androgen hormone produced in the adrenal glands, which at low levels is a significant predictor of CVD and ischemic heart disease, controlling for other risk factors [105]. The impact of TM practice on the sympathetic-adrenal-medulla system was studied examining plasma catecholamine levels at two different times of day. Morning and evening norepinephrine levels and morning epinephrine levels were significantly lower in the TM group compared with control subjects, suggesting a low hormonal response to daily stress caused by sympathetic tone regulation [106]. The implications are that patients will be benefited by reduced levels of stress hormones via TM practice.
A review of eight meta-analyses of a total of 587 studies on a wide variety of variables concluded that the TM technique is more effective than clinically derived methods in reducing several CVD risk factors, i.e., BP, trait anxiety, cigarette use, alcohol use, and drug use [107]. Research evidence reviewed below indicates that practice of the TM technique benefits many of the risk factors that contribute to CVD in both youth (Part 1) and adults (Part 2).
PART 1: PREVENTION: BLOOD PRESSURE REDUCTION STUDIES IN YOUTH
Current treatments to control elevated BP and cholesterol in individuals with unfavorable levels of these CVD risk factors are not typically effective in reducing morbidity and mortality [4]. Therefore, primary prevention of all major risk factors starting early in life is critical. Hypertension is no longer considered an adult disease [67]. BP levels ‘track’ relative to peers from late childhood onward [108], and these levels may predict EH in young adulthood [108, 109]. Children in the highest BP quintile are at greater risk to develop EH in early adulthood [108, 110]. The incidence of EH has risen dramatically in recent years among youth [67], increasing as much as sevenfold among minority populations including African Americans, in which rates are now estimated at 5–12% [111]. These rates in adolescents are expected to increase together with increases in obesity [112].
CVD ranks as the number two cause of death in children under the age of 15 [113]. In 1997, the National Institutes of Health (NIH) announced an initiative for pediatric intervention studies for primary prevention of CVD, which may benefit overall health and well-being, and reduce healthcare costs over the life span [114]. Electrolyte supplementation and diet interventions have met with mixed results in children, with studies finding minimal to no effect upon BP in normotensive youth [109, 115]. However, physical activity has been shown to be beneficial in lowering BP and improving lipid blood profiles in children [116]. The Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC-6) failed to support the use of relaxation therapies for the treatment or prevention of hypertension [117], although a study with the TM program was cited as having lowered BP at 3 months [118]. Furthermore, JNC-7 made no mention of relaxation therapies or meditation as lifestyle modification options to manage hypertension, but rather emphasized weight and sodium reduction, adopting the ‘DASH’ diet, increasing physical activity and moderating alcohol [119]. Those with normal (pre-hypertensive) and optimal BP are encouraged to make lifestyle modifications to further reduce their risk of developing CVD [119]. In view of the recommendation of JNC-7 that health-promoting lifestyle modifications be implemented well before BP reaches the “hypertension” range, this review examining effectiveness of a behavioral technique on BP lowering is highly relevant [119].
IMPACT OF TM ON RESTING BP AND BP REACTIVITY IN ADOLESCENTS
Studies examining the impact of TM practice on BP in youth have been conducted by the Georgia Prevention Institute of the Georgia Health Sciences University. A preliminary 8-week randomized clinical trial (RCT) examined resting BP and BP reactivity in adolescents with high normal BP [120]. Thirty-five adolescents (ages 15–18 years) with resting systolic BP (SBP) between the 85th to 95th percentile for their age, height and gender on 3 consecutive occasions, were assigned to either TM (n=17) or health education control (CTL, n=18) groups. The groups did not differ significantly on anthropomorphic, demographic, or pretest hemodynamic variables. The CTL group received lifestyle education sessions based on NIH guidelines on lowering BP through weight loss, diet and increasing physical activity. The TM group engaged in 15-min meditation sessions twice each day for 2 months including sessions during the school lunch break. Subjects’ CV function (BP, heart rate, and cardiac output) were measured outside of meditation at minutes 10, 12 and 14 of supine rest and in reaction to a behavioral stressor (simulated car driving) and a social stressor (interview about a stressful event) and then every minute during the 10-minute stressor period. Assessors were blinded with respect to treatment status.
After two-months, subjects were re-tested on the same protocol. The TM group exhibited a statistically significant 4.8 mm Hg decrease in resting SBP from pre- to 2 month post-intervention, compared to an increase of 2.6 mm Hg in the CTL group, in accord with the meta-analysis showing TM lowers resting baseline levels of SNS activation in meditators [101]. The TM group also exhibited greater decreases from pre- to post-intervention in SBP, heart rate and cardiac output reactivity to the car driving stressor, and in SBP reactivity to the social stressor interview compared to the CTL group. This was the first randomized study of reduction of resting BP and CV reactivity to acute stress in at-risk youth using the TM program, however, these findings may be viewed with caution due to the small sample size. Lowering BP and reducing exaggerated CV reactivity to chronic stress may beneficially impact on CV structure and function, thereby reducing CVD risk [30, 121].
IMPACT OF TM ON AMBULATORY BP IN YOUTH
A 16-week RCT was conducted with 156 African Americans (mean age=16 yrs) with high normal SBP (pre-hypertensive, 85th to 95th percentile for their age group i.e., 129/75 mm Hg) [122]. Subjects were identified via BP screening conducted in the schools and were assigned to TM or CTL following pre-testing. On school days the TM group meditated for 15 minutes each day at school under the daily supervision of a certified TM instructor. On weekends and after school subjects practiced unsupervised at home. Average self-reported compliance with TM at home was 75.9%. The CTL group participated in 15-minute CV health education sessions daily on school days. Interventions (TM and control) were provided alternately to schools over the study period to counterbalance the effect of school environment. Ambulatory 24-hr BP measures were recorded at pretest, 2- and 4-month posttests, and at follow-up 4-months after posttest. Reproducibility of ambulatory results have been validated in youth [123, 124]. The study found decreased daytime SBP and diastolic BP (DBP) in the TM group compared to controls by approximately 4 mm Hg over the four-month intervention period, with a similar SBP decrease maintained at the follow-up 4 months later [122]. These reductions in BP demonstrate a beneficial impact of TM during daytime when the at-risk youth would most likely be encountering stressful events.
IMPACT OF TM PRACTICE ON LEFT VENTRICULAR MASS IN ADOLESCENTS
The above-mentioned RCT also examined impact in heart structure in a sub-sample of the above-mentioned ambulatory BP study. The impact of TM practice on LVM was studied in 62 (30 TM; 32 health education CTL) pre-hypertensive African American youth. Based on findings that TM beneficially lowers BP, it was hypothesized that TM would decrease LVM. The echocardiographic-derived measure of LVM was measured before and after the 4-month TM intervention and at the 4-month follow-up via 2-D guided M-mode echocardiography. Blinding of the sonographers to subjects’ group classifications decreased likelihood of any systematic bias in the measurements. The TM group exhibited a significantly greater decrease in LVM indexed by height2.7 (LVM/ht2.7) at 4 months follow-up compared to the CTL group. These findings indicate that 4 months of TM resulted in decreases in LVM index and these changes were significant at follow-up compared to CTL [125]. Interestingly, the findings also indicated that the TM group showed greater control of body weight after formal cessation of the intervention, with a significant difference between the two groups at follow up [125]. The subjects were not screened for left ventricular hypertrophy as a basis for study entry but rather were screened for elevated BP.
SCHOOL BEHAVIOR
The prevalence of negative school behaviors remains a significant health problem in the U.S. [126]. It has been hypothesized that the high prevalence of negative school behaviors is in part due to greater exposure to chronic psychosocial stress, e.g., inadequate economic resources, family disintegration, information overload, and media violence [127, 128]. School systems are increasingly interested in reducing negative school behaviors, however they have had difficulty identifying programs that are effective and easy to implement on a broad scale [129]. One approach to the growing problem of school-related conduct problems may be to provide skills in stress reduction. Few studies have examined whether stress reduction programs improve school behavior in youth.
The impact of TM practice on school behavior was studied in a sub-sample of the above-mentioned RCT of ambulatory BP study in forty-five African American adolescents (ages 15–18 years). Primary outcome measures were: changes in absenteeism, school rule infractions and suspension days during the 4-month pretest period prior to randomization, compared with the 4-month intervention period. The TM group (n=25) exhibited significantly fewer infractions over the 4 months of intervention compared to a slight increase in the CTL group and there was a reduction of 0.3 suspension days due to behavior-related problems in the TM group compared to an increase of 1.2 suspension days in the CTL group. The TM group exhibited a significant reduction of 6.4 absentee class periods compared to an increase of 4.8 in the CTL group. These findings demonstrate that the TM program conducted in the school setting has a beneficial impact upon absenteeism, rule infractions, and suspension rates in African American adolescents, another indication of stress reduction through the practice of the TM technique [130].
Adolescents should be empowered through education and skill development to assume increasing responsibility for their own health behaviors [131]. School-based interventions including stress reduction can improve the CVD risk profile of children and should be utilized as one means of early primary prevention of CVD [115]. The effective implementation of stress reduction in the school setting depends to a large extent on the training and motivation of the school administration. Nurturing family environments have been shown to be associated with greater benefit in adolescents’ hemodynamic functioning via meditation in programs taught at school and designed to be practiced in the home environment [132]. The findings suggest that with adolescents, a more nurturing and supportive home environment may provide additional social support to increase likelihood of regular practice, thereby fostering greater benefit from meditation practiced in the home setting. At home, parents may provide a supportive role by allowing free time for practice, reminders to foster regular practice and by providing positive reinforcement. Parents may also provide a model for the children and personally benefit by practicing the TM technique themselves. Adolescents without supportive family factors and resources may not benefit as much from interventions requiring practice in the home environment [132]. The support and involvement of parents, school boards, educational professionals, community organizations, industry, and government together is necessary to support the adoption of healthy lifestyles for our society for succeeding generations [133].
Recent epidemiologic studies have documented worrisome trends towards increasing BP and obesity levels in adolescents [134]. Since CVD risk factors have been shown to persist into adulthood, this may translate into a CVD epidemic in the future. Health care providers need to assume greater responsibility for the prevention, detection, and intervention relevant to CVD risk factors in adolescents [135]. The urgent need for both population-based and individual approaches to primary prevention of CVD beginning in childhood cannot be over-emphasized [136]. Larger-scale clinical trials in diverse samples and settings are needed to further clarify the efficacy of this approach [137]. Intervention through stress reduction in youth is suggested as a vital future direction for preventive cardiology.
PART 2: TREATMENT OF CARDIOVASCULAR RISK FACTORS IN ADULTS
Recommendations of BP-lowering by JNC-7 [119] reflects the inescapable epidemiological fact that BP-related disease cannot be minimized only by treating those with clinical EH. Indeed, safe and effective measures to achieve small but significant reductions in BP across entire populations could have a far greater impact in reducing CVD than strategies targeting only higher risk patients. As recommended by JNC-7, the first choice for such measures should be non-pharmacological changes in lifestyle. The TM program’s effects in reducing BP in both hypertensive and pre-hypertensive individuals [118, 120, 122, 138–142], coupled with its additional benefits for health-related behaviors and well-being [141, 143, 144], could be invaluable as part of a population strategy for CVD prevention.
IMPACT OF THE TM PROGRAM ON HYPER- TENSION
Anti-hypertensive drug therapy has been associated with intolerability of adverse side effects [145], impaired quality of life concerns [146], and lack of cost effectiveness [147]. BP control in treated hypertensives is thought to be unsatisfactory due to poor patient compliance (forgetfulness and patient ignorance), insufficient use of combination drug treatment and other difficulties in achieving well-controlled BP [148]. Given the potential role of psychosocial stress in the development of EH, stress reduction with its lack of adverse side effects is a compelling option in the reduction of BP.
Research on the TM technique and hypertension in adults originated at a number of independent universities, starting in the early 1970’s. Collectively, these mostly-uncontrolled studies [149–151] reported a SBP/DBP mean decrease of −12.6/−8.8 mm Hg after a mean of 6 months of TM practice. Moreover, long-term practitioners of the TM technique were found to have significantly lower BP compared with age group-based population norms [152]. Recently, larger and better-controlled RCTs have corroborated early observations that TM practice has a beneficial lowering effect on BP [118, 120, 122, 138–142]. Studies with adults have been extensively reviewed previously and will be summarized below [153–155].
In the first randomized clinical trial (RCT) on the TM technique examining BP, 73 Boston area subjects (mean age 81 years) were studied in homes for the elderly. The subjects were randomly assigned to the TM program, mindfulness training (which involved both a structured word-production task and an unstructured creative mental activity task), a TM-analog (mental relaxation technique), and an untreated control group. SBP in the TM and mindfulness training groups was significantly reduced compared to the other groups [141].
In a subsequent RCT, 127 older African Americans (mean age 67 years) were randomly assigned to TM, Progressive Muscle Relaxation (PMR) or health education (HE) groups [139]. Multiple baseline measurements were taken, and after three months of intervention, the SBP decrease was significant for the TM group, compared to PMR, and HE. In this study, TM practice was found to be more efficacious for those who were not on medication. Subgroup analyses suggested efficacy of TM practice for treating hypertension in patients of both sexes and in the high and low EH risk categories of obesity, alcohol use, psychosocial stress, dietary sodium-to-potassium ratio, physical inactivity, and multiple risks [118]. The TM technique decreased both SBP and DBP significantly more than HE for all six EH risk factors. This was the first RCT to systematically investigate the applicability of stress-reduction techniques to different EH risk factor subgroups among African Americans.
A third RCT assigned 66 normotensive 18–34 year old men to either TM or active control groups modeled after the standard TM course to control for expectancy, instructor attention, and daily time commitment [140]. After four months of treatment, ambulatory DBP decreased only in the high-compliance TM sub-group, suggesting a dose-response effect such that greater benefit is accrued with regular practice.
A fourth RCT on the TM technique and BP [156] involved a collaboration with the Haight-Ashbury Free Medical Clinic, supported by an NIH grant which extended the earlier three-month design [139] to one-year. The study randomly assigned 150 hypertensive African Americans (mean age 49 years) to TM, PMR, or HE groups. Three baseline measurements were taken during each of five sessions spread over one month, and the mean of the 4th and 5th sessions were used as the baseline. This study addressed several design and methodological weaknesses of previous studies and featured: 1) an adequate number of baseline BP measurements to control for habituation and regression to the mean; 2) rigor in designing control treatment, balance of baseline characteristics, randomization, and blind data collection; 3) comparison among two different stress reduction techniques with health education in the same experiment; 4) adequate sample size and one-year follow-up; 5) medication changes controlled and monitored; and 6) selection of stage 1 or 2 hypertensive patients for likelihood of response.
The trial examined an important clinical question, i.e, whether lifestyle modification programs would remain effective in reducing BP over one year in adult African Americans. The study decreased DBP significantly more in the TM group than PMR or HE, and there was a trend for a greater reduction in SBP. Importantly, there was a significant reduction in antihypertensive medication use in the TM group compared to controls [156]. A safeguard against potential researcher bias built into the above RCTs was that BP data were collected by independent personnel at independent institutions.
A fifth RCT examined 298 university students, including 159 subjects at-risk for hypertension, and found significant SBP and DBP decreases at 3 months for the high-risk TM group of 5.0/2.8 mmHg compared with increases of 1.3/1.2 mmHg for high-risk wait-list control subjects. The TM group also showed significant improvements compared with control subjects in total psychological distress, anxiety, depression, anger/hostility, and coping. Moreover, reductions in psychological distress and coping significantly correlated with reductions in SBP and DBP [157].
Two meta-analyses have been published which have summarized many of the above findings [153, 155]. The first examined nine randomized controlled trials and found that the TM program lowered BP an average of 4.7/3.2 mmHg compared with control groups [153]. Subjects ranged in age from adolescent (mean age 16 years) to senior (mean age 81 years), and included normotensive, prehypertensive, and hypertensive individuals. Subgroup analyses of four hypertensive groups and three high-quality studies showed similar BP reductions in all groups.
The second meta-analysis examined effects of a variety of stress reduction programs in hypertensive patients, evaluating studies that used active controls, adequate baseline measurement, and blinded BP assessment. BP decreases associated with biofeedback, relaxation-assisted biofeedback, progressive muscle relaxation, and stress management training were not statistically significant; however, the TM program significantly lowered BP (SBP/DBP) by 5.0/2.8 mmHg [155]. BP reductions of this magnitude are suggested to result in significant decreases in CVD risk [158].
COST EFFECTIVENESS IN TREATING HYPER- TENSION
As reviewed above, randomized studies suggest that TM practice reduces BP in EH as effectively as do drug therapies. Cost-effectiveness of managing hypertension comparing the practice of the TM technique with the five leading anti-hypertensive drugs was analyzed by Herron et al. [159]. This cost-effectiveness comparison in 1996 dollars over a simulated 20-year treatment period reported that TM program had the lowest present value cost. The study suggested that the TM program is a cost-effective treatment for hypertension with many health benefits.
METABOLIC SYNDROME AND INSULIN RESISTANCE
The metabolic syndrome is a cluster of coronary heart disease (CHD) risk factors including hypertension, dyslipidemia, obesity, and insulin resistance [8]. A controlled study showed a 10% decrease in plasma total cholesterol in medication-free, hypercholesterolemic volunteers after 11 months of TM practice, compared with matched controls [160]. A study of executives and managers with normal cholesterol levels reported a significantly lower cholesterol level after 3 months of TM practice, compared with controls [161]. However, a later RCT with the TM technique did not find a significant cholesterol reduction possibly due to significant differences in dietary improvements between the study groups [162, 163]. A 4-month RCT with 103 stable CHD patients was conducted to examine the impact of TM practice on components of the metabolic syndrome and cardiac autonomic nervous system tone. Results indicated statistically significant decreases in adjusted SBP and insulin resistance, and increases in heart rate variability in the TM group compared with HE controls [164]. However, decreases in total cholesterol and lipoproteins in the TM group were not statistically significant, possibly due to a floor effect due to normal levels at baseline in addition to an 83% statin usage. The results suggest that neurohumoral pathways may be mechanistically involved in the metabolic syndrome, and that techniques, such as TM, that target neurohumoral pathways, may be beneficial for CHD reduction. Excessive levels of oxygen free radicals thought to contribute to oxidation of lipids and cholesterol contribute to the mechanisms underlying atherosclerotic CVD [165]. Related to this, 15% lower serum levels of lipid peroxides were found in a study of healthy normotensive TM practitioners compared with matched controls [166].
TREATING POST-TRAUMATIC STRESS DISORDER (PTSD) IN VETERANS
A large number of studies have shown an association between PTSD and CV/metabolic disease biomarkers. They suggest that PTSD may cause autonomic dysregulation and endothelial dysfunction leading to CVD [167]. Drugs and psychotherapeutic interventions are typically used for treating PTSD [168]. Drugs used for PTSD are not without adverse side effects. Psychotherapies used in PTSD treatment require considerable time and effort. In view of the high incidence of PTSD in veterans, TM training has also been recommended as a potential option for improving soldier resilience [169].
A preliminary 3-month RCT conducted at the Denver Vietnam Veterans Outreach Program randomly assigned Vietnam veterans with PTSD to either TM practice (n=10) or psychotherapeutic treatment (n=8). The TM group reported significant reductions in PTSD symptoms and reductions in employment problems, emotional numbness, family problems, depression, anxiety, insomnia, and alcohol problems compared to controls receiving psychotherapy. There was also a trend for reduced stress reactivity, measured as a more rapid physiological recovery from an auditory stressor in the TM group [170].
An uncontrolled pilot trial examined the effects of TM practice in veterans of the Iraq and Afghanistan wars [171]. Five veterans were trained in the TM technique and followed for 12 weeks. The subjects ranged in age from 18–65 years of age, and all had a history of moderately severe combat-related PTSD, as diagnosed via clinician-administered and patient-rated measures. The study reported that the subjects’ PTSD symptoms improved with increased quality of life after 8 weeks and that 4/5 were ‘much’ or ‘very much’ improved on the Clinician Global Impression Improvement Scale. The results of both studies should be viewed with caution due to small sample sizes. However, together with previous evidence that TM practice reduces PTSD-related symptoms (e.g., alcohol and drug misuse, anxiety, depression, alcohol problems, autonomic dysfunction) these studies have implications for potential use of the TM technique as a treatment and prevention modality for PTSD in military personnel with an added benefit for prevention of CV problems associated with PTSD.
EFFECTS ON TOBACCO AND ALCOHOL USAGE
Evidence suggests that the restorative rest produced by TM practice normalizes the neurochemical imbalances caused by and motivating substance abuse [172]. As a result, the physiological basis for craving is thought to decline, which is often accompanied by a decline in substance use [173]. A meta-analysis of 198 studies on behavioral techniques for reducing tobacco, alcohol, and drug consumption suggested that TM practice had substantially larger effect sizes in reducing harmful substance consumption than other techniques [174]. The findings also showed that patterns of abstinence were maintained for a longer time. A study with 295 university students showed a significant reduction in drinking rates in males [175]. A prospective study of 324 cigarette smokers found that 51% of those who reported full compliance with the TM practice quit smoking after two years, compared to 21% for both partial TM adherents and non-TM controls. The TM program dispenses no advice to quit smoking [76]. Rather, reduction in smoking behavior subsequent to TM practice is thought to be motivated by reduced need for stimulation and increased sensitivity to the harmful effects of tobacco on the body [176].
IMPACT OF TM PRACTICE ON CORTISOL
Elevated baseline levels of plasma cortisol, a major stress hormone, are associated with a greater prevalence of ischemic heart disease, independent of conventional risk factors [177]. Studies with cortisol have shown acute levels decreasing significantly during meditation [178, 179]. TM practice produces a healthier cortisol profile of lower baseline levels. A 27% decline in blood cortisol concentration during TM practice is consistent with complete inhibition of cortisol excretion from the adrenals [178, 180]. In a four-month longitudinal study of young men, regular twice-daily TM practice decreased basal cortisol levels from pre- to posttest, but cortisol responsiveness to laboratory stress increased in the TM group compared to controls [181]. Longer studies over 6 and 36 month periods have not observed consistent changes in cortisol levels [182, 183]. However, in a study of long-term TM practice examining the cortisol response to a metabolic stressor in women, post-glucose cortisol levels rose faster in the controls and were significantly higher than that in the TM group and urinary excretion of cortisol during this period was 3 times higher in controls than in the TM group. Lower cortisol response to metabolic challenge may reflect improved endocrine regulation relevant to the disease-preventing effects of TM practice in older women [184].
ACUTE EFFECTS OF TM PRACTICE ON CV FUNCTION IN HEALTHY ADULTS
The acute effect of TM practice upon CV function was examined in a preliminary study of 32 healthy middle-aged adults without any history of vascular dysfunction [185]. Long-term TM practitioners (mean twice daily TM practice = 23 years) were compared to a matched normotensive control group on CV function at rest and during 20 minutes of self-relaxation (eyes closed rest for the control group versus TM practice for the TM group). The TM group exhibited significantly greater decreases in SBP and total peripheral resistance compared to self-relaxation in the control group. Vasoconstriction is a result of elevated SNS activity [186], and a wide range of evidence shows TM practice produces acute and enduring reductions in SNS tone [101]. This suggests that decreases in SNS activity and hence vasoconstrictive tone during TM practice may be the hemodynamic mechanism responsible for reduction of high BP over time. The results of this study provide a preliminary contribution to the understanding of the underlying hemodynamic mechanisms responsible for the beneficial influence of TM practice upon CV risk factors.
ANGINA PECTORIS AND CAROTID ATHEROSCLEROSIS IN HEART PATIENTS
A single-blind prospective pilot study of angina pectoris reported that the TM program improved exercise tolerance, increased maximum workload, and delayed appearance of electrocardiographic abnormalities during exercise (delayed onset of ST segment depression) in 12 heart patients after 1 year of TM practice compared to 9 wait listed controls [187]. A RCT of 60 hypertensive African American subjects examined the impact of TM practice on carotid intima-media thickness, a validated surrogate measure for coronary and cerebral atherosclerosis. The findings showed a decrease in carotid artery thickness in the TM group compared with an increase in the control group, suggesting that TM practice may reduce carotid atherosclerosis [188]. Changes of this magnitude predict an 11% reduction in myocardial infarction [189] and an 8–15% reduction in stroke [190].
LEFT VENTRICULAR MASS AND FUNCTIONAL CAPACITY IN ADULTS
Increased LVM is a key indicator of hypertensive heart disease, and a major risk factor for CV mortality. African American subjects with high BP (N = 102, mean age 52.9 years) were randomized to the TM group or a health education control group who learned how to reduce risk of hypertensive heart disease through proper diet and exercise. For patients who learned the TM technique, LVM remained stable from baseline to the 7-month posttest, whereas health education controls showed a significant increase, with a difference in LVM change score of 5.6 g/m2. This suggests that the TM program may be useful in the prevention of left ventricular hypertrophy in African Americans [191]. A preliminary six-month RCT of African American patients (N=23) hospitalized for chronic heart failure found significant improvement on functional capacity on a six-minute walk test in the TM group compared to health education controls. The study also found reduced depression, improvement in health-related quality of life, and a trend towards fewer re-hospitalizations in the TM group [182].
CARDIOVASCULAR MORBIDITY
Cardiovascular disease is the highest cost disease category [192]. A 14-year, pre- and postintervention study in Quebec compared 1418 TM subjects with 1418 controls matched for age, sex, and region on government payments to physicians for medical treatment. For the 8 years before starting TM practice, the yearly rate of increase in payments between groups was not significantly different. For the 6 years after commencing meditation, payments in the TM group decreased 13.8% annually relative to controls [193]. In a follow-up of the patients with the highest 10% of cost from this sample, the TM group’s physician-visit costs decreased 28% relative to controls over a 5-year period of TM practice [194].
More direct evidence for the effects of TM on CV morbidity comes from the results of two large field studies of health-insurance statistics. The first study examined a group of experienced TM participants that increased in size from 694 to 2,119 over the five-year study period [195]. The TM group was compared to the health-insurance norm comprised of approximately 600,000 members and to five other groups (combined N=22,440) selected by the health-insurance company to be of comparable policies, size, and professional membership as the TM group. The TM group’s rate of hospitalization for diseases of the heart and blood vessels was 87% lower than the norm.
The second 4-year study of medical utilization statistics compared inpatient and outpatient utilization rates for the employees of an academic institution in Iowa that practiced the TM technique and other Maharishi Ayurveda natural health care modalities (N = 693) with 12 other small private colleges in Iowa (aggregated group size = 4,148) and with health-insurance norms. The mean hospital admission rates for CVD over the 4-year period were 92% less in the TM group compared to both controls and the normative data [196]. There were also reductions in all medical categories, and the TM group’s overall medical expenditures were 59% lower the norm and 57% lower than controls.
Analysis by age categories in both studies showed the greatest reductions in older people. They both showed approximately a 50% reduction in inpatient and outpatient admission rates for all causes for the younger TM groups. However, the first study found reductions of 68% and 74%, respectively, for TM practitioners over 40 compared to age matched controls [195]. Similarly, the second study found an 88% reduction in hospitalization rates, a 58% reduction in outpatient visits, and an 84% reduction in hospital expenses in TM subjects over 45 compared to age-matched controls. Since CVD incidence increases with age, the findings of this study have profound implications for CVD prevention with TM practice.
CARDIOVASCULAR MORTALITY
Two RCTs found that the TM program decreased mortality rates from CVD, as well as for death by all causes [197, 198]. The first study was a 15-year follow-up of 87 subjects (mean age 81 years) who had been randomly assigned to TM, mindfulness training, mental relaxation or a no-treatment control group. In this study, the survival rate after 3 years for the TM group was 100% compared to 65–87% for other groups [141]. After 15 years, mean survival time for CVD was higher and all-cause mortality was significantly lower for the TM group compared to the other groups combined [197]. In a second study, mortality and cause of death were assessed from vital statistics over 8 years of follow-up on 109 older African American patients with mild hypertension (mean age 67 years) who had participated in a hypertension study [139]. Subjects had been randomly assigned to two active stress reduction approaches—the TM program or PMR—or to a HE control group for three months. The adjusted relative risk for CVD mortality of the TM group compared with HE was significantly reduced by 81%. The adjusted relative risk for all-cause mortality of the TM group compared with PMR showed a trend at 57% reduction in the analysis of the 3-month finishers [198]. When patient data from the above two randomized controlled trials were combined in a post-hoc analysis [199], the TM group showed a 23% reduction in all-cause mortality compared to combined controls, a 30% reduction in the rate of CV mortality and a 49% reduction in the rate of cancer mortality. These findings have been further supported in a larger prospective RCT described below [200], and collectively suggest that the TM technique may offer benefits for reducing all-cause and CVD mortality, consistent with the large decreases in health insurance claims.
CARDIOVASCULAR CLINICAL EVENTS
An RCT supported by the NIH was conducted with 201 African American CHD patients (M age = 59 years). Subjects were assigned to TM or control groups. At the 5-year follow-up the TM group showed a 47% reduction in the primary composite endpoints of all-cause mortality, non-fatal myocardial infarction, and non-fatal stroke. The TM group also had a 5 mm Hg average reduction in SBP associated with a decrease in clinical events, and significant reductions in psychological stress in the high-stress subgroup. Of the 51 primary endpoint events (30 deaths, 5 nonfatal myocardial infarctions, and 6 strokes) during the study, 20 were in the TM group and 31 in the HE group [200]. The findings provide the strongest evidence to date that TM practice is useful in prevention of CHD mortality, myocardial infarction, and stroke [154].
CONCLUSION
In summary, the TM technique is an easily learned, cost-effective means of reducing resting and ambulatory BP and CV reactivity, and lowering LVM in adolescents at risk for hypertension. In adults with mild or moderate EH, TM practice decreases BP, reduces the use of anti-hypertensive medication, and decreases angina pectoris and carotid atherosclerosis. It markedly reduces medical care utilization for CVD, especially in older individuals, and it significantly decreases CVD and all-cause mortality. It decreases resting heart and respiratory rates and cortisol levels, improves CV function, and decreases stress-related risk factors, including alcohol and tobacco use. The mechanism of the effects of TM practice appears to be through acute and longitudinal reductions in sympathetic tone and reactivity to stress.
Considerable compelling evidence for the efficacy of TM practice as an approach to preventing and controlling EH and CVD risk has also been documented in extensive reviews [103, 138, 154, 201, 202]. Evidence presented offers a basis for public health policies and clinical approaches that can greatly affect the incidence and consequences of EH and CVD in the population at large [202]. The effective implementation of stress reduction depends to a large extent on the training and motivation of the health care administration. Large-scale clinical trials are needed to determine if this approach can reduce the incidence of EH and CVD when applied on a widespread basis. The medical, financial, and humanitarian significance of such research can hardly be overestimated. The support and involvement of health professionals, educators, community organizations, industry, and government together is necessary to support the adoption of healthy lifestyles for our society for succeeding generations [133]. Intervention through stress reduction in youth and adults is suggested as a future direction for preventive cardiology [202].
To our knowledge, the trials on the TM technique described here are the first RCTs to demonstrate improvement in CVD risk factors, CV clinical events, and mortality rates through a meditation program. If such improvements are replicated among other at-risk groups and in cohorts of CVD patients, this will have important implications for inclusion of this technique in the efforts to prevent and treat CVD and its clinical consequences.
Acknowledgments
Declared none.
Footnotes
Send Orders of Reprints at reprints@benthamscience.org
DISCLOSURE
This manuscript is an extended and updated version of a previously published manuscript [203].
CONFLICT OF INTEREST
The author(s) confirm that this article content has no conflicts of interest.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 3.Talayero BG, Sacks FM. The role of triglycerides in atherosclerosis. Curr Cardiol Rep. 2011;13:544–552. doi: 10.1007/s11886-011-0220-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daviglus ML, Lloyd-Jones DM, Pirzada A. Preventing cardiovascular disease in the 21st century: therapeutic and preventive implications of current evidence. Am J Cardiovasc Drugs. 2006;6:87–101. doi: 10.2165/00129784-200606020-00003. [DOI] [PubMed] [Google Scholar]
- 5.Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Arch Int Med. 1993;153:598–615. doi: 10.1001/archinte.153.5.598. [DOI] [PubMed] [Google Scholar]
- 6.Keil JE, Sutherland SE, Hames CG, et al. Coronary disease mortality and risk factors in black and white men. Results from the combined Charleston, SC, and Evans County, Georgia, heart studies. Arch Intern Med. 1995;155:1521–1527. [PubMed] [Google Scholar]
- 7.Williams JE, Nieto FJ, Sanford CP, et al. Effects of an angry temperament on coronary heart disease risk: The Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2001;154:230–235. doi: 10.1093/aje/154.3.230. [DOI] [PubMed] [Google Scholar]
- 8.Sorrentino MJ. Implications of the metabolic syndrome: the new epidemic. Am J Cardiol. 2005;96:3E–7E. doi: 10.1016/j.amjcard.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Reaven G, Abbasi F, McLaughlin T. Obesity, insulin resistance, and cardiovascular disease. Recent Prog Horm Res. 2004;59:207–223. doi: 10.1210/rp.59.1.207. [DOI] [PubMed] [Google Scholar]
- 10.Lewis S. Broken heart syndrome: perspectives from East and West. Adv Mind Body Med. 2005;21:3–5. [PubMed] [Google Scholar]
- 11.Eisenmann JC. Physical activity and cardiovascular disease risk factors in children and adolescents: an overview. Can J Cardio. 2004;20:295–301. [PubMed] [Google Scholar]
- 12.Raitakari OT, Juonala M, Kahonen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–2283. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 13.Li S, Chen W, Srinivasan SR, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290:2271–2276. doi: 10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 14.Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004;44:720–732. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Snieder H, Harshfield G, Barbeau P, et al. Dissecting the genetic architecture of the cardiovascular and renal stress response. Biol Psychol. 2002;61:73–95. doi: 10.1016/s0301-0511(02)00053-4. [DOI] [PubMed] [Google Scholar]
- 16.Treiber FA, Davis H, Turner JR. Cardiovascular responsivity to stress and preclinical manifestations of cardiovascular disease in youth. In: Hayman L, McMahon M, Turner JR, editors. Health and Behavior in Childhood and Adolescence: Cross-disciplinary Perspectives. New York: Lawrence Erlbaum Associates, Inc; 2001. [Google Scholar]
- 17.Cohen S, Kessler RC, Underwood Gordon L. Strategies for measuring stress in studies of psychiatric and physical disorders. In: Cohen S, Kessler RC, Underwood Gordon L, editors. Measuring stress. New York: Oxford University Press; 1995. pp. 3–26. [Google Scholar]
- 18.Manuck SB. Cardiovascular reactivity in cardiovascular disease: “Once more unto the breach”. International Journal of Behavioral Medicine. 1994;1:4–31. doi: 10.1207/s15327558ijbm0101_2. [DOI] [PubMed] [Google Scholar]
- 19.Esler M. The sympathetic system and hypertension. Am J Hypertens. 2000;13:99S–105S. doi: 10.1016/s0895-7061(00)00225-9. [DOI] [PubMed] [Google Scholar]
- 20.Julius S, Nesbitt S. Sympathetic overactivity in hypertension. A moving target. Am J Hypertens. 1996;9:113S–120S. doi: 10.1016/0895-7061(96)00287-7. [DOI] [PubMed] [Google Scholar]
- 21.Lovallo WR. Stress and Health: Biological and Psychological Interactions. 2. Thousand Oaks, CA: Sage Publications, Inc; 2005. [Google Scholar]
- 22.Luft FC, Grim CE, Fineberg N, et al. Effects of volume expansion and contraction in normotensive whites, blacks, and subjects of different ages. Circulation. 1979;59:643–650. doi: 10.1161/01.cir.59.4.643. [DOI] [PubMed] [Google Scholar]
- 23.Anderson NB. Ethnic differences in resting and stress-induced cardiovascular and humoral activity. In: Schneiderman N, Weiss SM, Kaufman PG, editors. Handbook of Research Methods in Cardiovascular Behavioral Medicine. New York: Plenum Press; 1989. [Google Scholar]
- 24.Guyton AC, Hall JE. Textbook of Medical Physiology. 11. Philadelphia: W.B. Saunders Company; 2005. [Google Scholar]
- 25.Anderson NB. Racial differences in stress-induced cardiovascular reactivity and hypertension: current status and substantive issues. Psychol Bull. 1989;105:89–105. doi: 10.1037/0033-2909.105.1.89. [DOI] [PubMed] [Google Scholar]
- 26.Saab PG, Llabre MM, Hurwitz BE, et al. Myocardial and peripheral vascular responses to behavioral challenges and their stability in black and white Americans. Psychophysiology. 1992;29:384–397. doi: 10.1111/j.1469-8986.1992.tb01712.x. [DOI] [PubMed] [Google Scholar]
- 27.Treiber FA, Davis H, Musante L, et al. Ethnicity, gender, family history of myocardial infarction, and hemodynamic responses to laboratory stressors in children. Health Psychol. 1993;12:6–15. doi: 10.1037//0278-6133.12.1.6. [DOI] [PubMed] [Google Scholar]
- 28.Treiber FA, McCaffrey F, Musante L, et al. Ethnicity, family history of hypertension and patterns of hemodynamic reactivity in boys. Psychosom Med. 1993;55:70–77. doi: 10.1097/00006842-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Folkow B. The structural factor in hypertension. In: Laragh JH, Brenner SM, editors. Hypertension: Pathophysiology, diagnosis and management. New York: Raven Press; 1990. pp. 5–58. [Google Scholar]
- 30.Folkow B. “Structural factor” in primary and secondary hypertension. Hypertension. 1990;16:89–101. doi: 10.1161/01.hyp.16.1.89. [DOI] [PubMed] [Google Scholar]
- 31.Weber KT, Sun Y, Guarda E. Structural remodeling in hypertensive heart disease and the role of hormones. Hypertension. 1994;23:869–877. doi: 10.1161/01.hyp.23.6.869. [DOI] [PubMed] [Google Scholar]
- 32.Levy D, Garrison RJ, Savage DD, et al. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322:1561–1566. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 33.Koren MJ, Devereux RB, Casale PN, et al. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Int Med. 1991;114:345–352. doi: 10.7326/0003-4819-114-5-345. [DOI] [PubMed] [Google Scholar]
- 34.Casale PN, Devereux RB, Milner M, et al. Value of echocardiographic measurement of left ventricular mass in predicting cardiovascular morbid events in hypertensive men. Ann Intern Med. 1986;105:173–178. doi: 10.7326/0003-4819-105-2-173. [DOI] [PubMed] [Google Scholar]
- 35.Papavassiliou DP, Treiber FA, Strong WB, et al. Anthropometric, demographic, and cardiovascular predictors of left ventricular mass in young children. Am J Cardiol. 1996;78:323–326. doi: 10.1016/0002-9149(96)00286-x. [DOI] [PubMed] [Google Scholar]
- 36.Murdison KA, Treiber FA, Mensah G, et al. Prediction of left ventricular mass in youth with family histories of essential hypertension. Am J Med Sci. 1998;315:118–123. doi: 10.1097/00000441-199802000-00008. [DOI] [PubMed] [Google Scholar]
- 37.Eich RH, Jacobsen EC. Vascular reactivity in medical students followed for 10 yr. J Chron Dis. 1967;20:583–592. doi: 10.1016/0021-9681(67)90035-5. [DOI] [PubMed] [Google Scholar]
- 38.Matthews KA, Woodall KL, Allen MT. Cardiovascular reactivity to stress predicts future blood pressure status. Hypertension. 1993;22:479–485. doi: 10.1161/01.hyp.22.4.479. [DOI] [PubMed] [Google Scholar]
- 39.Menkes MS, Matthews KA, Krantz DS, et al. Cardiovascular reactivity to the cold pressor test as a predictor of hypertension. Hypertension. 1989;14:524–530. doi: 10.1161/01.hyp.14.5.524. [DOI] [PubMed] [Google Scholar]
- 40.Falkner B, Kushner H, Onesti G, et al. Cardiovascular characteristics in adolescents who develop essential hypertension. Hypertension. 1981;3:521–527. doi: 10.1161/01.hyp.3.5.521. [DOI] [PubMed] [Google Scholar]
- 41.Jackson AS, Squires WG, Grimes G, et al. Prediction of future resting hypertension from exercise blood pressure. J Cardiac Rehabil. 1983;3:263–268. [Google Scholar]
- 42.Anderson NB, Armstead CA. Toward understanding the association of socioeconomic status and health: a new challenge for the biopsychosocial approach. Psychosom Med. 1995;57:213–225. doi: 10.1097/00006842-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 43.Clark R, Anderson NB, Clark V, et al. Racism as a stressor for African Americans. A biopsychosocial model. Am Psychol. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 44.Anderson NB, McNeilly M, Myers H. Toward understanding race difference in autonomic reactivity. In: Turner JR, Sherwood A, Light KC, editors. Individual Differences in Cardiovascular Response to Stress. New York: Plenum Press; 1992. pp. 125–145. [Google Scholar]
- 45.Treiber FA, Kamarck T, Schneiderman N, et al. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosom Med. 2003;65:46–62. doi: 10.1097/00006842-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 46.Suls J, Wan CK. The relationship between trait hostility and cardiovascular reactivity: a quantitative review and analysis. Psychophysiology. 1993;30:615–626. doi: 10.1111/j.1469-8986.1993.tb02087.x. [DOI] [PubMed] [Google Scholar]
- 47.Suls J, Wan CK, Costa PTJ. Relationship of trait anger to resting blood pressure: a meta-analysis. Health Psychol. 1995;14:444–456. doi: 10.1037//0278-6133.14.5.444. [DOI] [PubMed] [Google Scholar]
- 48.Rutledge T, Hogan BE. A quantitative review of prospective evidence linking psychological factors with hypertension development. Psychosom Med. 2002;64:758–766. doi: 10.1097/01.psy.0000031578.42041.1c. [DOI] [PubMed] [Google Scholar]
- 49.Anderson NB, Myers HF, Pickering T, et al. Hypertension in blacks: Psychosocial and biological perspectives. J Hypertens. 1989;7:161–172. [PubMed] [Google Scholar]
- 50.Johnson EH, Broman CL. The relationship of anger expression to health problems among black Americans in a national survey. J Behav Med. 1987;10:103–116. doi: 10.1007/BF00846419. [DOI] [PubMed] [Google Scholar]
- 51.Johnson EH. The Deadly Emotions: The Role of Anger, Hostility and Aggression in Health and Emotional Well-Being. New York: praeger Publishing Corp; 1990. [Google Scholar]
- 52.Stansfeld S, Crombie R. Cardiovascular effects of environmental noise: research in the United Kingdom. Noise Health. 2011;13:229–233. doi: 10.4103/1463-1741.80159. [DOI] [PubMed] [Google Scholar]
- 53.Johnson EH, Spielberger CD, Worden TJ, et al. Emotional and familial determinants of elevated blood pressure in black and white adolescent males. J Psychosom Res. 1987;31:287–300. doi: 10.1016/0022-3999(87)90048-1. [DOI] [PubMed] [Google Scholar]
- 54.Johnson EH, Schork NF, Spielberger CD. Emotional and familial determinants of elevated blood pressure in black and white adolescent females. J Psychosom Res. 1987;31:731–741. doi: 10.1016/0022-3999(87)90022-5. [DOI] [PubMed] [Google Scholar]
- 55.Musante L, Turner JR, Treiber FA, et al. Moderators of ethnic differences in vasoconstrictive reactivity in youth. Ethn Dis. 1996;6:224–234. [PubMed] [Google Scholar]
- 56.Wright LB, Treiber FA, Davis H, et al. Relationship between family environment and children’s hemodynamic responses to stress: A longitudinal evaluation. Behav Med. 1993;19:115–121. doi: 10.1080/08964289.1993.9935180. [DOI] [PubMed] [Google Scholar]
- 57.Wright LB, Treiber F, Davis H, et al. The role of maternal hostility and family environment upon cardiovascular functioning among youth two years later: socioeconomic and ethnic differences. Ethnicity & Disease. 1998;8:367–376. [PubMed] [Google Scholar]
- 58.Labarthe D, Ayala C. Nondrug interventions in hypertension prevention and control. Cardiology Clinics. 2002;20:249–263. doi: 10.1016/s0733-8651(01)00003-0. [DOI] [PubMed] [Google Scholar]
- 59.Linden W, Chambers L. Clinical effectiveness of non-drug treatment for hypertension: A meta-analysis. Ann Behav Med. 1994;16:35–45. [Google Scholar]
- 60.Linden W, Stossel C, Maurice J. Psychological interventions for patients with coronary artery disease. Archives of Internal Medicine. 1996;156:745–752. [PubMed] [Google Scholar]
- 61.Davis PH, Dawson JD, Riley WA, et al. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation. 2001;104:2815–2819. doi: 10.1161/hc4601.099486. [DOI] [PubMed] [Google Scholar]
- 62.Berenson GS, Wattigney WA, Tracy RE. Atherosclerosis of the aorta and coronary arteries and cardiovascular risk factors in persons aged 6 to 30 years and studied at necropsy (The Bogalusa Heart Study) Am J Cardiol. 1992;70:851–858. doi: 10.1016/0002-9149(92)90726-f. [DOI] [PubMed] [Google Scholar]
- 63.Berenson GS, Wattigney WA, Bao W, et al. Epidemiology of early primary hypertension and implications for prevention: the Bogalusa Heart Study. J Hum Hypertens. 1994;8:303–311. [PubMed] [Google Scholar]
- 64.Berenson GS, Srinivasan SR, Bao W. Precursors of cardiovascular risk in young adults from a biracial (black-white) population: the Bogalusa Heart Study. Ann N Y Acad Sci. 1997;817:189–198. doi: 10.1111/j.1749-6632.1997.tb48206.x. [DOI] [PubMed] [Google Scholar]
- 65.Probstfield JL. How cost-effective are new preventive strategies for cardiovascular disease? Am J Cardiol. 2003;91:22G–27G. doi: 10.1016/s0002-9149(03)00229-7. [DOI] [PubMed] [Google Scholar]
- 66.Cook NR, Cohen J, Hebert PR, et al. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–709. [PubMed] [Google Scholar]
- 67.Muntner P, He J, Cutler JA, et al. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–2113. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- 68.Travis FT. Transcendental Meditation technique. In: Craighead WE, Nemeroff CB, editors. The Corsini Encyclopedia of Psychology and Behavioral Science. New York: John Wiley & Sons; 2001. pp. 1705–1706. [Google Scholar]
- 69.Travis F. Autonomic and EEG patterns distinguish transcending from other experiences during Transcendental Meditation practice. Int J Psychophysiol. 2001;42:1–9. doi: 10.1016/s0167-8760(01)00143-x. [DOI] [PubMed] [Google Scholar]
- 70.Alexander CN, Cranson RW, Boyer RW, et al. Transcendental consciousness: A fourth state of consciousness beyond sleep, dreaming and waking. In: Gackenbach J, editor. Sleep and dreams: A Sourcebook. New York: Garland Publishing; 1987. pp. 282–315. [Google Scholar]
- 71.Travis F, Shear J. Focused attention, open monitoring and automatic self-transcending: Categories to organize meditations from Vedic, Buddhist and Chinese traditions. Conscious Cogn. 2010;19:1110–1118. doi: 10.1016/j.concog.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 72.Travis F, Olson T, Egenes T, et al. Physiological patterns during practice of the Transcendental Meditation technique compared with patterns while reading Sanskrit and a modern language. Int J Neurosci. 2001;109:71–80. doi: 10.3109/00207450108986526. [DOI] [PubMed] [Google Scholar]
- 73.Mason LI, Orme-Johnson DW. Transcendental consciousness wakes up in dreaming and deep sleep. Intern J Dream Res. 2010;3:28–32. [Google Scholar]
- 74.Chalmers R, Clements G, Schenkluhn H, et al., editors. Scientific Research on the Transcendental Meditation program: Collected Papers. 2–4. Vlodrop, The Netherlands: MVU Press; 1990. [Google Scholar]
- 75.Orme-Johnson DW, Farrow J, editors. Scientific Research on the Transcendental Meditation program: Collected Papers. Vol. 1. Rheinweiler, West Germany: MERU Press; 1977. [Google Scholar]
- 76.Roth R. Maharishi Mahesh Yogi’s Transcendental Meditation. Washington, DC: Primus; 1994. [Google Scholar]
- 77.Travis F, Wallace RK. Autonomic patterns during respiratory suspensions: Possible markers of Transcendental Consciousness. Psychophysiology. 1997;34:39–46. doi: 10.1111/j.1469-8986.1997.tb02414.x. [DOI] [PubMed] [Google Scholar]
- 78.Alexander CN. Transcendental Meditation. In: Corsini RJ, editor. Encyclopedia of Psychology. 2. New York: Wiley Interscience; 1993. [Google Scholar]
- 79.Wallace KR. The Physiology of Consciousness. Fairfield, IA: Maharishi International University Press; 1993. [Google Scholar]
- 80.Wallace RK, Benson H, Wilson AF. A wakeful hypometabolic physiologic state. American Journal of Physiology. 1971;221:795–799. doi: 10.1152/ajplegacy.1971.221.3.795. [DOI] [PubMed] [Google Scholar]
- 81.Dillbeck M, Barnes VA, Travis F, et al. Scientific Research on Maharishi’s Transcendental Meditation and TM-Sidhi Programme: Collected Papers. Vol. 7. Vlodrop, The Netherlands: Maharishi Vedic University Press; in press. [Google Scholar]
- 82.Arias AJ, Steinberg K, Banga A, et al. Systematic review of the efficacy of meditation techniques as treatments for medical illness. J Altern Complement Med. 2006;12:817–832. doi: 10.1089/acm.2006.12.817. [DOI] [PubMed] [Google Scholar]
- 83.Ospina MB, Bond TK, Karkhaneh M, et al. Meditation practices for health: state of the research. Evid Rep Technol Assess (Full Rep) 2007;155:1–263. [PMC free article] [PubMed] [Google Scholar]
- 84.Wallace RK. The Physiology of Meditation. Scientific American. 1972;226:84–90. [Google Scholar]
- 85.Dillbeck MC, Bronson EC. Short-term longitudinal effects of the transcendental meditation technique on EEG power and coherence. Int J Neurosci. 1981;14:147–151. doi: 10.3109/00207458108985827. [DOI] [PubMed] [Google Scholar]
- 86.Hebert JR, Lehmann D, Tan G, et al. Enhanced EEG alpha time-domain phase synchrony during Transcendental Meditation: implications for cortical integration theory. Signal Processing. 2005;85:2213–2232. [Google Scholar]
- 87.Travis F, Arenander A. Cross-sectional and longitudinal study of effects of transcendental meditation practice on interhemispheric frontal asymmetry and frontal coherence. Int J Neurosci. 2006;116:1519–1538. doi: 10.1080/00207450600575482. [DOI] [PubMed] [Google Scholar]
- 88.Travis F, Haaga DA, Hagelin J, et al. Effects of Transcendental Meditation practice on brain functioning and stress reactivity in college students. Int J Psychophysiol. 2009;71:170–176. doi: 10.1016/j.ijpsycho.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 89.Travis F, Tecce J, Arenander A, et al. Patterns of EEG coherence, power, and contingent negative variation characterize the integration of transcendental and waking states. Biol Psychol. 2002;61:293–319. doi: 10.1016/s0301-0511(02)00048-0. [DOI] [PubMed] [Google Scholar]
- 90.Hummel F, Gerloff C. Interregional long-range and short-range synchrony: a basis for complex sensorimotor processing. Prog Brain Res. 2006;159:223–236. doi: 10.1016/S0079-6123(06)59015-6. [DOI] [PubMed] [Google Scholar]
- 91.Palva S, Palva JM. New vistas for alpha-frequency band oscillations. Trends Neurosci. 2007;30:150–158. doi: 10.1016/j.tins.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 92.Sauseng P, Klimesch W. What does phase information of oscillatory brain activity tell us about cognitive processes? Neurosci Biobehav Rev. 2008;32:1001–1013. doi: 10.1016/j.neubiorev.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 93.Yamamoto S, Kitamura Y, Yamada N, et al. Medial profrontal cortex and anterior cingulate cortex in the generation of alpha activity induced by Transcendental Meditation: A magnetoencephalographic study. Acta Med Okayama. 2006;60:51–58. doi: 10.18926/AMO/30752. [DOI] [PubMed] [Google Scholar]
- 94.Newberg A, Travis F, Wintering N, et al. Neural Imaging: 2006. Miami, Fl: 2006. Cerebral 416 glucose metabolic changes associated with Transcendental Meditation practice. [Google Scholar]
- 95.Travis F, Haaga DA, Hagelin J, et al. A self-referential default brain state: patterns of coherence, power, and eLORETA sources during eyes-closed rest and Transcendental Meditation practice. Cogn Process. 2009;11:21–30. doi: 10.1007/s10339-009-0343-2. [DOI] [PubMed] [Google Scholar]
- 96.Raichle ME, Snyder AZ. A default mode of brain function: a brief history of an evolving idea. Neuroimage. 2007;37:1083–1090. doi: 10.1016/j.neuroimage.2007.02.041. [DOI] [PubMed] [Google Scholar]
- 97.Alexander CN, Rainforth M, Gelderloos P. Transcendental Meditation, self-actualization and psychological health: A conceptual overview and statistical meta-analysis. J Soc Behav Pers. 1991;6:189–247. [Google Scholar]
- 98.Shear J. State-enlivening and practice-makes-perfect approaches to meditation. Biofeedback. 2011;39:51–55. [Google Scholar]
- 99.Tanner MA, Travis F, Gaylord-King C, et al. The effects of the Transcendental Meditation program on mindfulness. J Clin Psychol. 2009;65:574–589. doi: 10.1002/jclp.20544. [DOI] [PubMed] [Google Scholar]
- 100.Jevning R, Wallace RK, Biedebach M. The physiology of meditation: A review. A wakeful hypometabolic integrated response. Neurosci Biobehav Rev. 1992;16:415–424. doi: 10.1016/s0149-7634(05)80210-6. [DOI] [PubMed] [Google Scholar]
- 101.Dillbeck MC, Orme-Johnson DW. Physiological differences between Transcendental Meditation and rest. American Psychologist. 1987;42:879–881. [Google Scholar]
- 102.Pitman RK, Orr SP. Twenty-four-hour urinary cortisol and catecholamine excretion in combat-related posttraumatic stress disorder. Biol Psychiat. 1990;27:245–247. doi: 10.1016/0006-3223(90)90654-k. [DOI] [PubMed] [Google Scholar]
- 103.Walton KG, Schneider RH, Nidich SI, et al. Psychosocial stress and cardiovascular disease Part 2: Effectiveness of the Transcendental Meditation program in treatment and prevention. Behav Med. 2002;28:106–123. doi: 10.1080/08964280209596049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Walton KG, Pugh NDC, Gelderloos P, et al. Stress reduction and preventing hypertension: Preliminary support for a psychoneuroendocrine mechanism. J Altern Compl Med. 1995;1:263–283. doi: 10.1089/acm.1995.1.263. [DOI] [PubMed] [Google Scholar]
- 105.Barrett-Connor E, Khaw KT, Yen SS. A prospective study of dehydroepiandrosterone sulfate, mortality, and cardiovascular disease. N Engl J Med. 1986;315:1519–1524. doi: 10.1056/NEJM198612113152405. [DOI] [PubMed] [Google Scholar]
- 106.Infante JR, Torres-Avisbal M, Pinel PV, JA, et al. Catecholamine levels in practitioners of the transcendental meditation technique. Physiol Behav. 2001;72:141–146. doi: 10.1016/s0031-9384(00)00386-3. [DOI] [PubMed] [Google Scholar]
- 107.Orme-Johnson DW, Walton KG. All approaches of preventing or reversing effects of stress are not the same. Am J Health Promot. 1998;12:297–299. doi: 10.4278/0890-1171-12.5.297. [DOI] [PubMed] [Google Scholar]
- 108.Bao W, Threefoot SA, Srinivasan SR, et al. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. Am J Hypertens. 1995;8:657–665. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- 109.Alpert BS, Murphy JK, Treiber FA. Essential hypertension: Approaches to prevention in children. Medicine and Exercise in Nutrition and Health. 1994;3:296–307. [Google Scholar]
- 110.Lambrechtsen J, Rasmussen F, Hansen HS, et al. Tracking and factors predicting rising in ‘tracking quartile’ in blood pressure from childhood to adulthood: Odense Schoolchild Study. J Hum Hypertens. 1999;13:385–391. doi: 10.1038/sj.jhh.1000836. [DOI] [PubMed] [Google Scholar]
- 111.International Pediatric Hypertension Association. Blood Pressure Facts. 2010 wwwpediatrichypertensionorg.
- 112.Guillaume M, Björntorp P. Obesity in children. Horm Metab Res. 1996;28:573–581. doi: 10.1055/s-2007-979856. [DOI] [PubMed] [Google Scholar]
- 113.American Heart Association. Heart Disease and Stroke Statistics — 2005 Update. Dallas, TX: American Heart Association; 2005. [Google Scholar]
- 114.NIH Special Emphasis Panel on Intervention Studies in Children and Adolescents to Prevent Cardiovascular Disease: Minutes of meeting September 8–9, 1997. Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute; 1998. [Google Scholar]
- 115.Resnicow K, Robinson TN. School-based cardiovascular disease prevention studies: review and synthesis. Ann Epidemiol. 1997;7:S14–S31. [Google Scholar]
- 116.Andersen LB, Riddoch C, Kriemler S, et al. Physical activity and cardiovascular risk factors in children. Br J Sports Med. 2011;45:871–876. doi: 10.1136/bjsports-2011-090333. [DOI] [PubMed] [Google Scholar]
- 117.Kaplan NM. The 6th Joint National Committee report (JNC-6): New guidelines for hypertension therapy from the USA. Keio Journal of Medicine. 1998;47:99–105. doi: 10.2302/kjm.47.99. [DOI] [PubMed] [Google Scholar]
- 118.Alexander CN, Schneider RH, Staggers F, et al. Trial of stress reduction for hypertension in older African Americans (part II): sex and risk subgroup analysis. Hypertension. 1996;28:228–237. doi: 10.1161/01.hyp.28.2.228. [DOI] [PubMed] [Google Scholar]
- 119.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC-7 Report. J Am Med Assoc. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 120.Barnes VA, Treiber FA, Davis H. Impact of Transcendental Meditation on cardiovascular function at rest and during acute stress in adolescents with high normal blood pressure. J Psychosom Res. 2001;51:597–605. doi: 10.1016/s0022-3999(01)00261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Pickering TG. Mental stress as a causal factor in the development of hypertension and cardiovascular disease. Curr Hypertens Rep. 2001;3:249–254. doi: 10.1007/s11906-001-0047-1. [DOI] [PubMed] [Google Scholar]
- 122.Barnes VA, Johnson MH, Treiber FA. Impact of Transcendental Meditation on ambulatory blood pressure in African American adolescents. Am J Hypertens. 2004;17:366–369. doi: 10.1016/j.amjhyper.2003.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Barnes VA, Johnson MH, Dekkers JC, et al. Reproducibility of ambulatory blood pressure measures in African American adolescents. Ethn Dis. 2002;12:240–245. [PMC free article] [PubMed] [Google Scholar]
- 124.Barnes VA, Johnson MH, Treiber FA. Temporal stability of twenty-four-hour ambulatory hemodynamic bioimpedance measures in African American adolescents. Blood Press Monit. 2004;9:173–177. doi: 10.1097/00126097-200408000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Barnes VA, Kapuku G, Treiber FA. Impact of Transcendental Meditation on Left Ventricular Mass in African American Adolescents. eCAM. 2012;2012:1–6. doi: 10.1155/2012/923153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Brener ND, Simon TR, Krug EG, et al. Recent trends in violence-related behaviors among high school students in the United States. JAMA. 1999;282:440–446. doi: 10.1001/jama.282.5.440. [DOI] [PubMed] [Google Scholar]
- 127.Guerra NG, Huesmann LR, Tolan PH, et al. Stressful events and individual beliefs as correlates of economic disadvantage and aggression among urban children. J Consult Clin Psychol. 1995;63:518–528. doi: 10.1037//0022-006x.63.4.518. [DOI] [PubMed] [Google Scholar]
- 128.Weist MD, Paskewitz DA, Jackson CY, et al. Self-reported delinquent behavior and psychosocial functioning in inner-city teenagers: a brief report. Child Psychiatry Hum Dev. 1998;28:241–248. doi: 10.1023/a:1022684031414. [DOI] [PubMed] [Google Scholar]
- 129.Everett SA, Kann L, McReynolds L. The Youth Risk Behavior Surveillance System: policy and program applications. J Sch Health. 1997;67:333–335. doi: 10.1111/j.1746-1561.1997.tb03468.x. [DOI] [PubMed] [Google Scholar]
- 130.Barnes V, Bauza LB, Treiber FA. Impact of stress reduction on negative school behavior in adolescents. Health and Quality of Life Outcomes. 2003;1:10. doi: 10.1186/1477-7525-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Washington RL. Interventions to reduce cardiovascular risk factors in children and adolescents. Am Fam Physician. 1999;59:2211–2218. [PubMed] [Google Scholar]
- 132.Barnes VA, Gregoski MJ, Tingen M, et al. Family Environmental Influences of Meditation Efficacy On Hemodynamic Function Among African American Adolescents. J Compl Integrative Med. 2010;7:Article 25. doi: 10.2202/1553-3840.1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lawrence M, Arbeit M, Johnson CC, et al. Prevention of adult heart disease beginning in childhood: intervention programs. Cardiovasc Clin. 1991;21:249–262. [PubMed] [Google Scholar]
- 134.McCrindle BW. Cardiovascular risk factors in adolescents: relevance, detection, and intervention. Adolesc Med. 2001;12:147–162. [PubMed] [Google Scholar]
- 135.Rocchini AP. Raising heart-healthy children. Pediatr Int. 1999;41:597–602. doi: 10.1046/j.1442-200x.1999.01151.x. [DOI] [PubMed] [Google Scholar]
- 136.Harrell JS, Pearce PF, Hayman LL. Fostering prevention in the pediatric population. J Cardiovasc Nurs. 2003;18:144–149. doi: 10.1097/00005082-200304000-00011. [DOI] [PubMed] [Google Scholar]
- 137.Black DS, Milam J, Sussman S. Sitting-Meditation Interventions Among Youth: A Review of Treatment Efficacy. Pediatrics. 2009;124:e532–541. doi: 10.1542/peds.2008-3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Schneider RH, Alexander CN, Salerno J, et al. Stress reduction in the prevention and treatment of cardiovascular disease in African Americans: a review of controlled research on the Transcendental Meditation (TM) program. J Soc Behav Pers. 2005;17:159–180. [Google Scholar]
- 139.Schneider RH, Staggers F, Alexander CN, et al. A randomized controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26:820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 140.Wenneberg SR, Schneider RH, Walton KG, et al. A controlled study on the effects of Transcendental Meditation on cardiovascular reactivity and ambulatory blood pressure. Intern J Neurosci. 1997;89:15–28. doi: 10.3109/00207459708988461. [DOI] [PubMed] [Google Scholar]
- 141.Alexander CN, Langer EJ, Newman RI, et al. Transcendental Meditation, mindfulness, and longevity: An experimental study with the elderly. J Pers Soc Psychol. 1989;57:950–964. doi: 10.1037//0022-3514.57.6.950. [DOI] [PubMed] [Google Scholar]
- 142.Kondwani KA, Schneider RH, Alexander CN, et al. Left ventricular mass regression with the Transcendental Meditation technique and a health education program in hypertensive African Americans. J Soc Behav Pers. 2005;17:181–200. [Google Scholar]
- 143.Alexander CN, Robinson P, Orme-Johnson DW, et al. Effects of Transcendental Meditation compared to other methods of relaxation and meditation in reducing risk factors, morbidity and mortality. Homeostasis. 1994;35:243–264. [Google Scholar]
- 144.Eppley K, Abrams AI, Shear J. Differential effects of relaxation techniques on trait anxiety: A meta-analysis. J Clin Psychol. 1989;45:957–974. doi: 10.1002/1097-4679(198911)45:6<957::aid-jclp2270450622>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 145.Bucca C. Take the side-effects of drugs into account. Lancet. 2004;364:1285. doi: 10.1016/S0140-6736(04)17149-3. [DOI] [PubMed] [Google Scholar]
- 146.Bremner AD. Antihypertensive medication and quality of life--silent treatment of a silent killer? Cardiovasc Drugs Ther. 2002;16:353–364. doi: 10.1023/a:1021790112182. [DOI] [PubMed] [Google Scholar]
- 147.Ambrosioni E. Pharmacoeconomics of hypertension management: the place of combination therapy. Pharmacoeconomics. 2001;19:337–347. doi: 10.2165/00019053-200119040-00002. [DOI] [PubMed] [Google Scholar]
- 148.Grassi G, Seravalle G, Mancia G. Blood Pressure Control and Antihypertensive Treatment. Curr Vasc Pharmacol. 2012 Jan 20; doi: 10.2174/157016112800812719. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 149.Benson H, Wallace RK. Decreased blood pressure in hypertensive subjects who practiced meditation. Circulation. 1972:45–46. 516. doi: 10.1016/0021-9681(74)90083-6. [DOI] [PubMed] [Google Scholar]
- 150.Blackwell B, Hanenson IB, Bloomfield SS, et al. Effects of Transcendental Meditation on blood pressure: A controlled pilot experiment. Psychosomatic Medicine. 1975;37:86 (abstract). [Google Scholar]
- 151.Agarwal BL, Kharbanda A. Effect of transcendental meditation on mild and moderate hypertension. J Assoc Physicians India. 1981;29:591–596. [PubMed] [Google Scholar]
- 152.Wallace RK, Silver J, Mills PJ, et al. Systolic blood pressure and long-term practice of the Transcendental Meditation and TM-Sidhi programs: Effects of TM on systolic blood pressure. Psychosomatic Medicine. 1983;45:41–46. doi: 10.1097/00006842-198303000-00006. [DOI] [PubMed] [Google Scholar]
- 153.Anderson JW, Liu C, Kryscio RJ. Blood Pressure Response to Transcendental Meditation: A Meta-analysis. Am J Hypertens. 2008;21:310–316. doi: 10.1038/ajh.2007.65. [DOI] [PubMed] [Google Scholar]
- 154.Orme-Johnson DW, Barnes VA, Schneider RH. Transcendental Meditation for Primary and Secondary Prevention of Coronary Heart Disease. In: Allan R, Fisher J, editors. Heart & Mind: the Practice of Cardiac Psychology. 2. Washington, DC: American Psychological Association; 2011. pp. 365–379. [Google Scholar]
- 155.Rainforth MV, Schneider RH, Nidich SI, et al. Stress reduction programs in patients with elevated blood pressure: A systematic review and meta-analysis. Curr Hypertens Rep. 2007;9:520–528. doi: 10.1007/s11906-007-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Schneider RH, Alexander CN, Staggers F, et al. A randomized controlled trial of stress reduction in the treatment of hypertension in African Americans over one year. Am J Hypertens. 2005;18:88–98. doi: 10.1016/j.amjhyper.2004.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Nidich SI, Rainforth MV, Haaga DA, et al. A randomized controlled trial on effects of the Transcendental Meditation program on blood pressure, psychological distress, and coping in young adults. Am J Hypertens. 2009;22:1326–1331. doi: 10.1038/ajh.2009.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Staessen JA, Thijisq L, Fagard R, et al. Effects of immediate versus delayed antihypertensive therapy on outcome in the Systolic Hypertension in Europe Trial. J Hypertens. 2004;22:847–845. doi: 10.1097/00004872-200404000-00029. [DOI] [PubMed] [Google Scholar]
- 159.Herron RE, Hillis SL, Mandarino JV, et al. The impact of the Transcendental Meditation program on government payments to physicians in Quebec. American J Health Promot. 1996;10:183–191. doi: 10.4278/0890-1171-10.3.208. [DOI] [PubMed] [Google Scholar]
- 160.Cooper MJ, Aygen MM. A relaxation technique in the management of hypercholesterolemia. Journal of Human Stress. 1979;5:24–27. doi: 10.1080/0097840x.1979.10545991. [DOI] [PubMed] [Google Scholar]
- 161.De Armond DL. Effects of the Transcendental Meditation program on psychological, physiological, behavioral and organizational consequences of stress in managers and executives in management. Fairfield: Iowa Maharishi University of Management; 1996. [Google Scholar]
- 162.Calderon R, Schneider RH, Alexander CN, et al. Stress, stress reduction and hypercholesterolemia in African Americans: a review. Ethnicity and Disease. 1999;9:451–462. [PubMed] [Google Scholar]
- 163.Calderon RJ. Effects of nonpharmacological approaches on cholesterol levels in mild hypertensive African Americans: A pilot study of the Transcendental Meditation program and a health education program. Fairfield, IA: Maharishi University of Management; 2000. [Google Scholar]
- 164.Paul-Labrador M, Polk D, Dwyer JH, et al. Effects of a randomized controlled trial of transcendental meditation on components of the metabolic syndrome in subjects with coronary heart disease. Arch Intern Med. 2006;166:1218–1224. doi: 10.1001/archinte.166.11.1218. [DOI] [PubMed] [Google Scholar]
- 165.Berliner J, Navab M, Fogelman A, et al. Atherosclerosis: Basic mechanisms. Oxidation, inflammation and genetics. Circulation. 1995;91:2488–2496. doi: 10.1161/01.cir.91.9.2488. [DOI] [PubMed] [Google Scholar]
- 166.Schneider RH, Nidich SI, Salerno JW, et al. Lower lipid peroxide levels in practitioners of the Transcendental Meditation program. Psychosom Med. 1998;60:38–41. doi: 10.1097/00006842-199801000-00008. [DOI] [PubMed] [Google Scholar]
- 167.Stevens G, Mascarenhas M, Mathers C. Global health risks: progress and challenges. Bull World Health Organ. 2009;87:646. doi: 10.2471/BLT.09.070565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Friedman MJ. Posttraumatic stress disorder among military returnees from Afghanistan and Iraq. Am J Psychiatry. 2006;163:586–593. doi: 10.1176/ajp.2006.163.4.586. [DOI] [PubMed] [Google Scholar]
- 169.Rees B. Overview of outcome data of potential meditation training for soldier resilience. Mil Med. 2011;176:1232–1242. doi: 10.7205/milmed-d-11-00067. [DOI] [PubMed] [Google Scholar]
- 170.Brooks JS, Scarano T. Transcendental Meditation in the treatment of post-Vietnam adjustment. J Couns Devel. 1985;64:212–215. [Google Scholar]
- 171.Rosenthal JZ, Grosswald S, Ross R, et al. Effects of transcendental meditation in veterans of Operation Enduring Freedom and Operation Iraqi Freedom with posttraumatic stress disorder: a pilot study. Military Medicine. 2011;176:626–630. doi: 10.7205/milmed-d-10-00254. [DOI] [PubMed] [Google Scholar]
- 172.Walton KG, Levitsky D. A neuroendocrine mechanism for the reduction of drug use and addictions by Transcendental Meditation. In: O’Connell DF, Alexander CN, editors. Self Recovery—Treating Addictions Using Transcendental Meditation and Maharishi Ayur-Veda. Binghamton, NY: Harrington Park Press; 1994. pp. 89–118. [Google Scholar]
- 173.Hawkins MA. Effectiveness of the Transcendental Meditation program in criminal rehabilitation and substance abuse recovery: A review of the research. J Offender Rehabil. 2002;36:47–65. [Google Scholar]
- 174.Alexander CN, Robinson P, Rainforth M. Treating and preventing alcohol, nicotine and drug abuse through Transcendental Meditation Technique: A review and statistical analysis. In: O’Connell DF, Alexander CN, editors. Self Recovery—Treating Addictions Using Transcendental Meditation and Maharishi Ayur-Veda. Binghamton, NY: Harrington Park Press; 1994. pp. 13–88. [Google Scholar]
- 175.Haaga DA, Grosswald S, Gaylord-King C, et al. Effects of the Transcendental Meditation Program on Substance Use among University Students. Cardiol Res Pract. 2011;2011:1–8. doi: 10.4061/2011/537101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Royer A. The role of the Transcendental Meditation Technique in promoting smoking cessation: A longitudinal study. In: O’Connell DF, Alexander CN, editors. Self Recovery—Treating Addictions Using Transcendental Meditation and Maharishi Ayur-Veda. Binghamton, NY: Harrington Park Press; 1994. pp. 221–242. [Google Scholar]
- 177.Reynolds RM, Labad J, Strachan MW, et al. Elevated fasting plasma cortisol Is associated with ischemic heart disease and Its risk factors in people with Type 2 Diabetes: The Edinburgh Type 2 Diabetes Study. J Clin Endocrinol Metab. 2010;95:1–7. doi: 10.1210/jc.2009-2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Jevning R, Wilson AF, Smith WR. Adrenocortical activity during meditation. Horm Behav. 1978;10:54–60. doi: 10.1016/0018-506x(78)90024-7. [DOI] [PubMed] [Google Scholar]
- 179.Michaels RR, Parra J, McCann DS, et al. Renin, cortisol, and aldosterone during transcendental meditation. Psychosom Med. 1979;41:50–54. doi: 10.1097/00006842-197902000-00006. [DOI] [PubMed] [Google Scholar]
- 180.Jevning R, Wilson AF, Smith WR. The transcendental meditation technique, adrenocortical activity, and implications for stress. Experientia. 1978;34:618–619. doi: 10.1007/BF01936994. [DOI] [PubMed] [Google Scholar]
- 181.MacLean CR, Walton KG, Wenneberg SR, et al. Effects of the Transcendental Meditation program on adaptive mechanisms: changes in hormone levels and responses to stress after 4 months. Psychoneuroendocrinology. 1997;22:277–295. doi: 10.1016/s0306-4530(97)00003-6. [DOI] [PubMed] [Google Scholar]
- 182.Jayadevappa R, Johnson JC, Bloom BS, et al. Effectiveness of transcendental meditation on functional capacity and quality of life of African Americans with congestive heart failure: a randomized control study. Ethn Dis. 2007;17:72–77. [PMC free article] [PubMed] [Google Scholar]
- 183.Werner OR, Wallace RK, Charles B, et al. Long-term endocrinologic changes in subjects practicing the Transcendental Meditation and TM-Sidhi program. Psychosom Med. 1986;48:59–66. doi: 10.1097/00006842-198601000-00004. [DOI] [PubMed] [Google Scholar]
- 184.Walton KG, Fields JZ, Levitsky DK, et al. Lowering cortisol and CVD risk in postmenopausal women: a pilot study using the Transcendental Meditation program. Ann NY Acad Sci. 2004;1032:211–215. doi: 10.1196/annals.1314.023. [DOI] [PubMed] [Google Scholar]
- 185.Barnes VA, Treiber FA, Turner JR, et al. Acute effects of Transcendental Meditation on hemodynamic functioning in middle aged adults. Psychosom Med. 1999;61:525–531. doi: 10.1097/00006842-199907000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Ludmer PL, Selwyn AP, Shook TL, et al. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med. 1986;315:1046–1051. doi: 10.1056/NEJM198610233151702. [DOI] [PubMed] [Google Scholar]
- 187.Zamarra JW, Schneider RH, Besseghini I, et al. Usefulness of the Transcendental Meditation Program in the treatment of patients with coronary artery disease. Am J Cardiol. 1996;77:867–870. doi: 10.1016/S0002-9149(97)89184-9. [DOI] [PubMed] [Google Scholar]
- 188.Castillo-Richmond A, Schneider R, Alexander C, et al. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke. 2000;31:568–573. doi: 10.1161/01.str.31.3.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Salonen JT, Salonen R. Ultrasound B-mode imaging in observational studies of atherosclerotic progression. Circulation. 1993;87:II56–II65. [PubMed] [Google Scholar]
- 190.O’Leary DH, Polak JF, Kronmal RA, et al. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults: Cardiovascular Health Study Collaborative Research Group New England. J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 191.Salerno JW, Schneider RH, Alexander CN, et al. A Controlled Trial of Effects of Stress Reduction on Left Ventricular Mass in Hypertensive African Americans (abstract) Ethn & Dis. 2004;14:S2–54. [Google Scholar]
- 192.American Heart Association. Heart Disease and Stroke Statistics — 2010 Update. Dallas, TX: American Heart Association; 2010. [Google Scholar]
- 193.Herron RE, Hillis SL. The impact of the transcendental meditation program on government payments to physicians in Quebec: an update. Am J Health Promot. 2000;14:284–291. doi: 10.4278/0890-1171-14.5.284. [DOI] [PubMed] [Google Scholar]
- 194.Herron R. Changes in physician costs among high-cost Transcendental Meditation practitioners compared with high-cost nonpractitioners over 5 years. American Journal of Health Promotion. 2011;26:56–60. doi: 10.4278/ajhp.100729-ARB-258. [DOI] [PubMed] [Google Scholar]
- 195.Orme-Johnson DW. Medical care utilization and the Transcendental Meditation program. Psychosomatic Medicine. 1987;49:493–507. doi: 10.1097/00006842-198709000-00006. [DOI] [PubMed] [Google Scholar]
- 196.Orme-Johnson DW, Herron RE. An innovative approach to reducing medical care utilization and expenditures. Am J Man Care. 1997;3:135–144. [PubMed] [Google Scholar]
- 197.Alexander C, Barnes V, Schneider R, et al. Randomized controlled trial of stress reduction on cardiovascular and all-cause mortality in the elderly: Results of 8 year and 15 year follow-ups. Circulation. 1996;93:629. [Google Scholar]
- 198.Barnes VA, Schneider RH, Alexander CN, et al. Impact of Transcendental Meditation on mortality in older African Americans with hypertension—eight year follow-up. Journal of Social Behavior and Personality. 2005;17:201–216. [Google Scholar]
- 199.Schneider RH, Alexander CN, Staggers F, et al. Long-term effects of stress reduction on mortality in persons >/=55 years of age with systemic hypertension. Am J Cardiol. 2005;95:1060–1064. doi: 10.1016/j.amjcard.2004.12.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Schneider R, Nidich S, Kotchen JM, et al. Effects of stress reduction on clinical events in African Americans with coronary heart disease: A randomized clinical trial. Circulation. 2009:120. [Google Scholar]
- 201.Schneider RH, Alexander CN, Wallace RK. In search of an optimal behavioral treatment for hypertension: A review and focus on Transcendental Meditation. In: Johnson EH, Gentry WD, Julius S, editors. Personality, Elevated Blood, and Essential Hypertension. Washington: Hemisphere Publishing Corporation; 1992. pp. 291–318. [Google Scholar]
- 202.Walton KG, Schneider RH, Salerno JW, et al. Psychosocial stress and cardiovascular disease Part 3: Clinical and policy implications of research on the Transcendental Meditation program. Behav Med. 2005;30:173–183. doi: 10.3200/BMED.30.4.173-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Barnes VA, Orme-Johnson DW. Clinical and Pre-clinical Applications of the Transcendental Meditation Program® in the Treatment and Prevention of Essential Hypertension and Cardiovascular Disease in Youth and Adults. Curr Hyperten Rev. 2006;2:207–218. doi: 10.2174/157340206778132545. [DOI] [PMC free article] [PubMed] [Google Scholar]