Abstract
Background & objectives:
Several studies have reported adverse drug events ranging from 5 to 35 per cent in all age group from outpatient setting. However, adverse drug reactions (ADRs) particularly among a large sample of ambulatory elderly patients in India has not been reported. This study has attempted to identify ADRs and assessed their causality, preventability and severity, and also their risk factors in Indian ambulatory elderly patients.
Methods:
A 2 year long term prospective study included 4005 ambulatory elderly patients (60 yr or above; either sex) at a public teaching hospital. Suspected ADRs were assessed for causality, preventability and severity using Naranjo's probability scale, modified Schumock and Thornton's criteria, and modified Hartwig's criteria, respectively.
Results:
Of the total 4005 prescriptions, 406 were identified with ADRs, giving the occurrence of 10 per cent ADRs in elderly. The total number of ADRs was 422 in 406 prescriptions. Type A ADRs accounted for 46 per cent of the total ADRs. Majority of the ADRs (88.6%) were classified as ‘probable’. The definitely preventable reactions were 22 per cent. The percentage of moderate reaction was 16 per cent. Only 1.6 per cent ADRs was severe in nature. The most common type of ADR was peripheral oedema. The most commonly offending class of drug was cardiovascular drugs (57.6%). Using logistic regression analysis, the risk factors which contributed to ADRs were age above 80 yr (OR=1.7), prescription of multiple drugs (OR=1.8), longer duration of treatment (OR=2.28) and multiple diagnoses (OR=1.8).
Interpretation & conclusions:
In this study, 10 per cent ambulatory elderly patients were found to have ADRs. This indicates that the elderly patients should be closely monitored for ADRs, to avoid clinically significant harmful consequences. The awareness of risk factors of ADRs would help physicians to identify elderly patients with greater risk of ADRs and, therefore, might benefit from ADRs monitoring and reporting programme.
Keywords: ADRs, ambulatory elderly patient, risk factors
Adverse drug reactions (ADRs) are a major cause of morbidity and repeated ADRs related hospitalizations have consistently increased faster than first-time ADRs among elderly patients1. Majority of studies have shown that prevalence of ADRs is higher in the elderly as compared to adult2.
In USA, more than 90 per cent of adults aged 65 yr and older use one medication per week and 10-25 per cent experience an adverse drug reaction. These ADRs are responsible for 3.4 to 7.0 per cent of hospital admissions3. The proportion of outpatients with an ADR ranges from 5 to 35 per cent in all age group of patients4.
Although, the literature review has shown the lack of Indian studies to identify ADRs especially among Indian ambulatory elderly patients, one study conducted among elderly inpatients has reported that one third of hospitalized elderly experienced 419 ADRs5. It has been argued that old age is not a predictor for adverse drug reactions but merely a marker for co-morbidity, altered pharmacokinetics, altered pharmacidynamics and polypharmacy6. Of all the factors that are most consistently associated with adverse drug reactions, polypharmacy is considered to be the most important. In the elderly patients, the multiplicity of disorders requires the use of multiple drugs7. In addition, their altered pharmacokinetics and pharmacodynamics result in an enhanced sensitivity to many drugs. Studies from overseas as well as India have demonstrated that polypharmacy is prevalent and associated with increased potential for adverse drug reactions, inappropriate prescription and drug interactions8,9.
Adverse drug reaction (ADR) monitoring and reporting activity is in its infancy in India. The important reason is lack of awareness and lack of interest of healthcare professionals in ADR reporting and documentation. A study conducted to determine the level of awareness of physicians about ADR and the extent of their involvement in pharmacovigilance activities showed that despite good observation and knowledge of ADR among physicians the rate of ADRs reporting and documentation is very low10. Therefore, this study was aimed to identify ADRs and assess their causality, preventability and severity, and also their risk factors in Indian ambulatory elderly patients.
Material & Methods
A prospective study was carried out in geriatric clinic of Government Medical College and Hospital (GMCH), Chandigarh. The data of 4115 patients were collected from geriatric clinic between July 2009 to February 2011.
All patients aged ≥60 yr who visited the geriatric clinic during the study period, and were prescribed medication(s), were included in the study. Data on demographic details and prescribed medications were collected using structured format. For each patient, a form was completed with regard to patient age, gender, diagnosis, past medications, currently prescribed drugs, their brand names, daily doses, treatment durations, indications for each drug, laboratory investigation reports. Data of 110 patients with incomplete information were excluded. Therefore, a total of 4005 prescriptions were included for analysis.
International Classification of Disease (ICD-10)11, was used for coding the diagnosis and Anatomical Therapeutic Chemical (ATC)12 classification was used for medications. The adverse drug reactions based on the causes were classified on the basis of Edward & Aronson classification system. According to this, there are six types of ADRs namely Type A (augmented pharmacologic effects), Type B (bizarre effects), Type C (chronic effects), Type D (delayed effects), Type E (end-of-treatment effects) and Type F (failure of therapy)13.
Identification of adverse drug reactions: Suspected ADRs were assessed for causality, preventability and severity using Naranjo's probability scale14, modified Schumock & Thornton's criteria15 and modified Hartwig's criteria16, respectively. The degree of association of an ADR with a drug was done with the help Naranjo's algorithm which involves assigning score to a set of questions. The total score for a particular ADR was calculated and the association was termed into one of these categories– definite (score >9), probable (score 5-8), possible (score 1-4) or doubtful (score 0). Modified Schumock and Thornton's criteria18 have three sections namely definitely preventable, probably preventable and not preventatable, each consists of three questions. Severity was identified using Modified Hartwig's criteria19 which involve seven severity levels. Severity of the identified ADRs was assessed at different levels, ranging between 1 and 7. Levels 1 and 2 indicated mild, 3 and 4 considered as moderate and level 5 and above, as severe ADRs. The potential risk factors assessed were age, sex, number of medications, number of diagnoses and duration of treatment.
The study protocol was approved by the ethics committee of Government Medical College & Hospital, Chandigarh. Each patient gave written informed consent. Each patient was assigned a sequential identification number.
Statistical analysis: The results are represented as mean ± SEM and percentages as applicable; age, diagnosis, number of medications and duration of treatments were variable for determination of risk factors. Odds ratio was calculated to assess the most common risk factors for ADRs. Statistical significance was determined at 95 per cent level of confidence. The data were analyzed using Sigma Stat package (Ver. 3.5).
Results
A total of 2208 male and 1797 females were included in the study (55 vs 45%). The average age of patients was 68.28 ± 0.11 yr. Of the 4005 patients, 2402 patients belonged to the age group 60-69 yr (60% of total) while 30.8 per cent of the patients belonged to the age group 70-79 yr and the remaining (9.2%) were more than 80 yr of age.
It was found that approximately 69 per cent of the patients suffered from two or more diseases. On an average, each patient had 2.01±0.01 diagnoses; 41 per cent of patients were diagnosed as having 2 co-morbidities; 21 per cent had 3 co-morbid conditions and 7.4 per cent had a range of 4 to 6 co-morbidities. The most common pair of diseases was hypertension-diabetes, coronary artery disease-hypertension or diabetes, hypertension-cerebrovascular disease, diabetes-polyneuropathy and coronary artery disease-digestive disorder. It was found that 97 per cent of the patients suffered from diseases of circulatory system followed by digestive system disorders (48%) and endocrine, nutritional, metabolic diseases accounted for 44 per cent. Hypertension (64.8%), diabetes mellitus (36%) and ischaemic heart disease (24.7%) were the most frequently reported disorders.
The average number of medications prescribed was 6.45±0.04. The distribution of medication followed the normal Gaussian distribution. Over half of the patients (57.9%) received more than five medications concurrently. The average duration of prescribed medication was found to be 36.25±0.42 days.
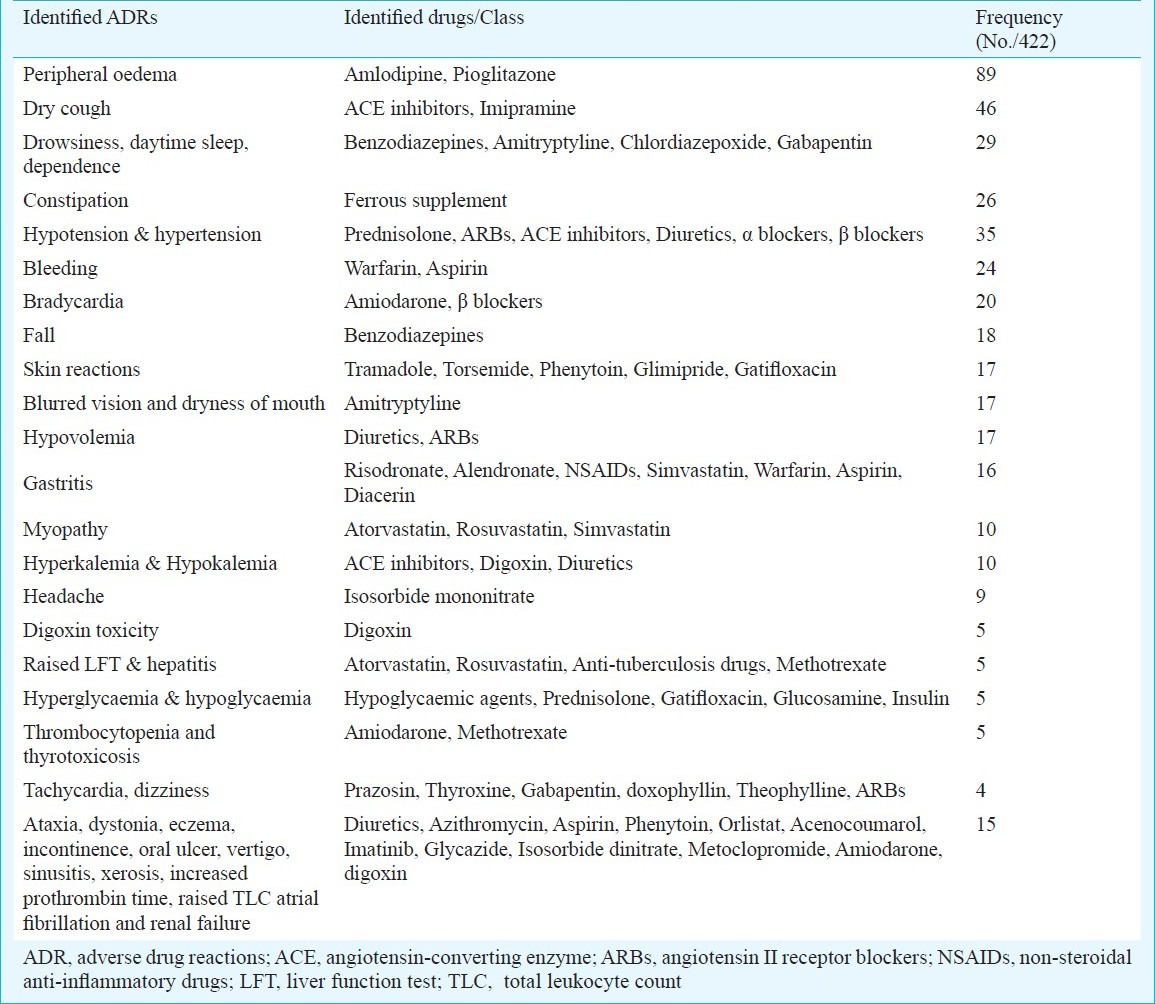
Most prescriptions (90%) did not have any ADRs. The total number of ADRs was 422 in 406 prescriptions. The most commonly identified ADRs were peripheral oedema, dry cough and drowsiness (Table I). The other ADRs were ataxia, dystonia, eczema, incontinence, oral ulcer, vertigo, sinusitis, xerosis, increased prothrombin time, atrial fibrillation and renal failure. The most common offending class of drug according to ATC classification was the cardiovascular drugs, followed by haematinics, antiplatelet agents and heparin and low molecular weight heparin and drugs used to treat neurological disorders (57.5% >12.7% >10%). Type A ADRs accounted for 46 per cent of the total ADRs.
Table I.
List of commonly identified adverse drug reactions (ADRs) and drugs/class
Over 88.6 per cent of the ADRs were probable (n=374) with a score of 5-8. Only 11 were definite (with score equal or over 9) and 37 ADRs were possible type with score range of 1-4. Of the total 422 ADRs, most (73%) belonged to the category of “not preventable”. Definitely preventable ADRs were 22 per cent and probably preventable were only 6 per cent. Based on modified Hartwig severity scale, most of the reactions were categorized as mild (348 of 422), 67 ADRs were moderate type and only seven ADRs were ‘severe’ in nature.
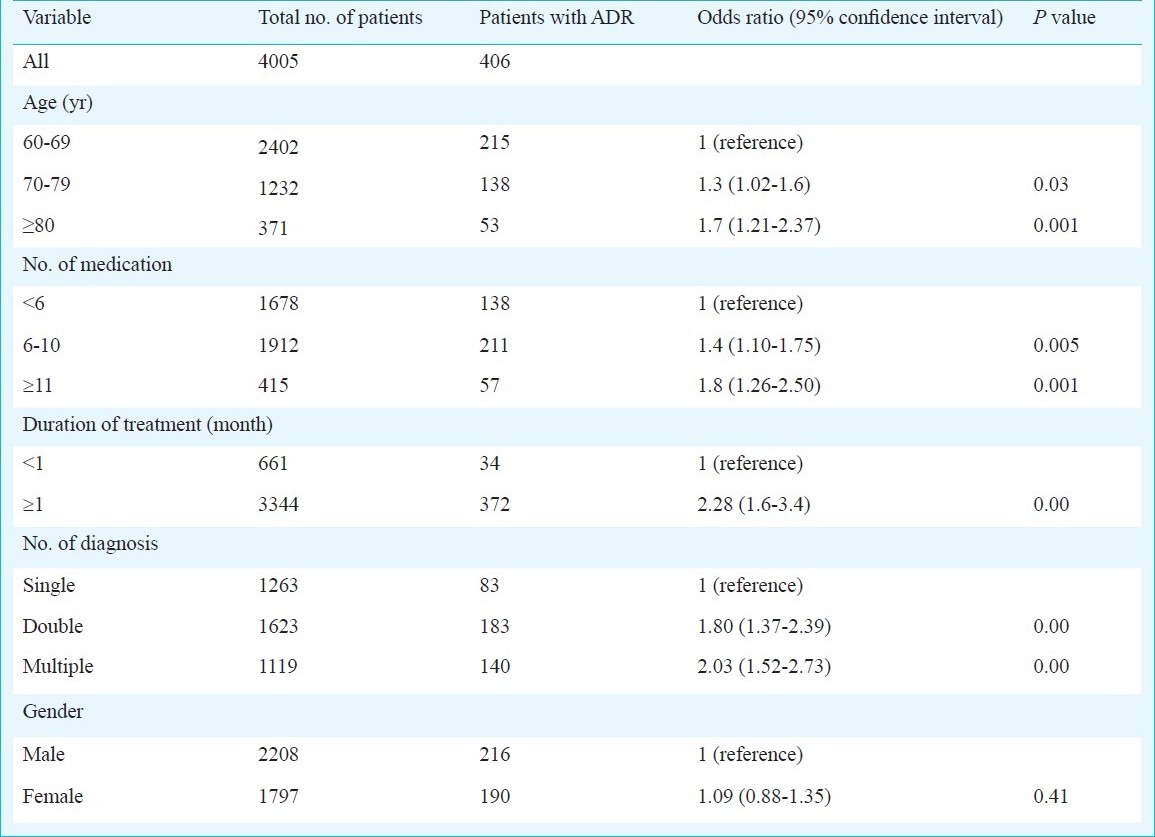
Using logistic regression analysis, it was found that patients of more a`dvanced age (over 80 yr) were at significant risk for ADRs as compared to the patients of age group 60-69 yr. In this study, patients with multiple diseases, multiple medications and longer duration of treatment were more likely to have ADRs. There was no difference in the occurrence of ADRs in female as compared male patients (OR=1.09; CI=0.88-1.35). The effect of variables on the ADRs is depicted in Table II.
Table II.
Risk factors associated with adverse drug reactions (ADRs)
Discussion
ADRs were found in 10 per cent of elderly patients in this study which was lower as compared to 21 per cent reported by Schneider et al17. A recent study has reported the ADRs related hospitalization rate as 5-12 per cent among elderly and increase in ADR-related hospital admissions in elderly by 143 per cent18.
Adverse drug reactions and non-compliance are important causes of hospital admissions in the elderly patients. Other studies reported high proportion (30.4%) of hospital admissions were ADRs related among elderly patients19. In the present study, 11 patients required hospitalization to manage the condition. The possible reason for these differences may be differences in ADRs reporting and documentation and use of broad definition of ADRs. It is known that frail elderly patients appear to be particularly at risk of ADRs. It is known that elderly patients have reduced renal clearance and literature supports the use of low dose of digoxin. In this study, five patients were prescribed high dose and experienced digoxin toxicity. This can be reduced by increasing the awareness among healthcare professionals regarding drugs.
The most commonly identified ADR was peripheral oedema (89 of 422) due to amlodipine. Calcium channel blocker (CCB) related oedema is caused by preferential arteriolar or pre-capillary dilation without commensurate dilation in the venous or post-capillary circulation. Reported frequency rates for peripheral oedema with CCB therapy are quite varied ranging from 5 per cent to as high as 70 per cent20. Correction of oedema was done by physician with dose reduction or drug withdrawal.
The second most common ADR was ACE inhibitors induced dry cough. Cough may occur within hours of the first dose of medication, or its onset can be delayed for weeks to months after the initiation of therapy. The prevalence of ACE inhibitor-induced cough has been reported to be 5-35 per cent in patients treated with these agents21. Women, individuals with ACE genotype II, and those of black or Asian ethnicity have been reported to be at increased risk of ACE inhibitor-induced cough. Angiotensin II receptor blockers (ARBs) confer many of the same haemodynamic benefits as ACE inhibitors, but these do not directly inhibit ACE activity or inhibit the breakdown of bradykinin. ARBs should be acceptable substitute for ACE inhibitors in patients who have adverse events such as kinin-mediated cough22.
The most commonly offending class of drug was the cardiovascular drugs. The drugs included in this class were CCBs (type C), ACE inhibitors (type C), digoxin (type A) and diuretics (type A). Cardiovascular medications prescribed for cardiovascular disease is challenging because treatment often requires more than one medication, which may be one of unavoidable reasons for multiple drug use and dose variation in the elderly. The finding of this study was consistent with other results where cardiovascular drugs were most often associated with ADR admissions in adults and elderly patients23. Drug classes like antidiabetics, oral anticoagulants and antiplatelets and narrow-therapeutic index drugs accounted for most of the ADRs in present study, as reported earlier also24. Majority of the reactions were type A (46%) which has also been reported by other researchers25. The second most common ADR was type C because elderly patients have chronic disorders. There is no published report showing prevalence of Type C reactions in elderly outpatients.
In this study the causal relation for 88.6 per cent ADRs with drug was probable; corroborating with other results showing majority of reactions as probable26. Only in 11 cases drugs were established with certainty for ADR as causal reason; 73 per cent of the ADRs were not preventable as patients were on chronic medications. Most of the ADRs observed in this study were found to be mild (82.5%).
In this study the suspected ADRs were not identified, but the possible risk factors related to the occurrence of ADRs were determined. The risk factors were more advanced age (>80 yr), multiple diseases, prescription of multiple medications and longer duration of treatment. Advance age was a significant risk factor for ADRs. Possible reasons could be the changes in pharmacokinetics with advancing age.
Higher prescribing rates of medicine among elderly are associated with severity of illness and severe morbidity may influence their susceptibility to ADRs through alterations in pharmacokinetics. The results of this study also found that increased number of medications and co-morbidity increases the risk of occurrence of ADRs, which is consistent with other results27,28.
One report has suggested that pharmacological, immunological and hormonal differences and the fact that women take more medications may explain some gender differences29. However, our study showed no difference in the occurrence of ADRs in male and female patients in concordance with the study by Patel et al30 from England.
In conclusion, the results of our study indicate that the elderly patients should be closely monitored for ADRs, to avoid clinically significant harmful consequences. The awareness of risk factors of ADRs can help physicians to identify elderly patients with greater risk of ADRs.
References
- 1.Zhang M, Holman CDJ, Preen DB, Brameld K. Repeat adverse drug reactions causing hospitalization in older Australians: a population-based longitudinal study 1980-2003. Br J Clin Pharmacol. 2007;63:163–70. doi: 10.1111/j.1365-2125.2006.02839.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies EC, Green CF, Taylor S, Williamson PR, Mottram DR, Pirmohamed M. Adverse drug reactions in hospital in-patients: A prospective analysis of 3695 patient-episodes. PLoS ONE. 2009;4:e4439.4. doi: 10.1371/journal.pone.0004439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamilton HJ, Gallagher PF, O’Mohony D. Inappropriate prescribing and adverse drug events in older people. BMC Geriatrics. 2009;9:5. doi: 10.1186/1471-2318-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ, Annest JL. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006;296:1858–66. doi: 10.1001/jama.296.15.1858. [DOI] [PubMed] [Google Scholar]
- 5.Parthasarathi AG, Ramesh M, Guido S, Basavanagowdappa H. Frequency and nature of adverse drug reactions in elderly in-patients of two Indian medical college hospitals. J Postgrad Med. 2011;57:189–95. doi: 10.4103/0022-3859.85201. [DOI] [PubMed] [Google Scholar]
- 6.Carbonin P, Pahor M, Bernabei R, Sgadari A. Is age an independent risk factor of adverse drug reactions in hospitalized medical patients? J Am Geriatr Soc. 1991;39:1093–9. doi: 10.1111/j.1532-5415.1991.tb02875.x. [DOI] [PubMed] [Google Scholar]
- 7.Honlon JT, Ruby CM, Guay D, Artz M. Geriatrics. In: Dipiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM, editors. Pharmacotherapy: A pathophysiologic approach. 5th ed. New York: McGraw-Hill; 2002. pp. 79–89. [Google Scholar]
- 8.Mandavi , D’Cruz S, Sachdev A, Tiwari P. Prevalence and predictors of inappropriate drug use among older people: results from an Indian public outpatient setting. J Pharmaceutical Health Services Res. 2011;2:29–34. [Google Scholar]
- 9.Tulner LR, Kuper IM, Frankfort SV, van Campen JP, Koks CH, Brandjes DP, et al. Discrepancies in reported drug use in geriatric outpatients: relevance to adverse events and drug-drug interactions. Am J Geriatr Pharmacother. 2009;7:93–104. doi: 10.1016/j.amjopharm.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Amrita P, Singh SP. Status of spontaneous reporting of adverse drug reaction by physicians in Delhi. Indian J Pharm Pract. 2011;4:29–36. [Google Scholar]
- 11.International statistical classification of diseases and related health problems, 10th revision (ICD-10) Geneva: WHO; 2010. World Health Organization. [Google Scholar]
- 12.Anatomical Therapeutic Chemical (ATC) classification index with Defined Daily Dose. Geneva: WHO; 2003. WHO Collaborating Centre for Drug Statistic Methodology. [Google Scholar]
- 13.Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet. 2000;356:1255–9. doi: 10.1016/S0140-6736(00)02799-9. [DOI] [PubMed] [Google Scholar]
- 14.Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–45. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 15.Schumock GT, Thornton JP. Focusing on the preventability of adverse drug reactions. Hosp Pharm. 1992;27:538. [PubMed] [Google Scholar]
- 16.Hartwig SC, Siegel J, Schneider PJ. Preventability and severity assessment in reporting adverse drug reactions. Am J Hosp Pharm. 1992;49:2229–32. [PubMed] [Google Scholar]
- 17.Schneider JK, Mion LC, Frengley JD. Adverse drug reactions in an elderly outpatient population. Am J Hosp Pharm. 1992;49:90–6. [PubMed] [Google Scholar]
- 18.Hartholt KA, van der Velde N, Looman CW, Panneman MJ, van Beeck EF, Patka P, et al. Adverse drug reactions related hospital admissions in persons aged 60 years and over, The Netherlands, 1981-2007: less rapid increase, different drugs. PLoS ONE. 2010;5:e13977. doi: 10.1371/journal.pone.0013977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan M, Nicklason F, Vial JH. Adverse drug events as a cause of hospital admission in the elderly. Intern Med J. 2001;31:199–205. doi: 10.1046/j.1445-5994.2001.00044.x. [DOI] [PubMed] [Google Scholar]
- 20.Pepine CJ, Cooper-DeHoff RM, Weiss RJ, Koren M, Bittar N, Thadani U, et al. Comparison of effects of nisoldipine-extended release and amlodipine in patients with systemic hypertension and chronic stable angina pectoris. Am J Cardiol. 2003;91:274–9. doi: 10.1016/s0002-9149(02)03154-5. [DOI] [PubMed] [Google Scholar]
- 21.Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough ACCP Evidence-Based Clinical Practice Guidelines. Chest. 2006;129:169S–73S. doi: 10.1378/chest.129.1_suppl.169S. [DOI] [PubMed] [Google Scholar]
- 22.Dykewicz MS. From current opinion in allergy and clinical immunology cough and angioedema from angiotensin-converting enzyme inhibitors: New insights into mechanisms and management. Curr Opin Allergy Clin Immunol. 2004;4:267–70. doi: 10.1097/01.all.0000136759.43571.7f. [DOI] [PubMed] [Google Scholar]
- 23.Brvar M, Fokter N, Bunc M, Mozina M. The frequency of adverse drug reaction related admissions according to method of detection, admission urgency and medical department specialty. BMC Clin Pharmacol. 2009;9:8. doi: 10.1186/1472-6904-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rupawala AH, Kshirsagar NA, Gogtay NJ. A retrospective analysis of adverse events in the elderly in a tertiary referral center in Mumbai (Bombay), India. Indian J Med Sci. 2009;63:167–73. [PubMed] [Google Scholar]
- 25.Jose J, Rao PG. Pattern of adverse drug reactions notified by spontaneous reporting in an Indian tertiary care teaching hospital. Pharmacol Res. 2006;54:226–33. doi: 10.1016/j.phrs.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 26.Suh DC, Woodall BS, Shin SK, Hermes-De-Santis ER. Clinical and economic impact of adverse drug reactions in hospitalized patients. Ann Pharmacother. 2000;34:1373–9. doi: 10.1345/aph.10094. [DOI] [PubMed] [Google Scholar]
- 27.Gandhi TK, Weingart SN, Borus J, Seger AC, Peterson J, Burdick E, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348:1556–64. doi: 10.1056/NEJMsa020703. [DOI] [PubMed] [Google Scholar]
- 28.Zhang M, Holman CDJ, Price SD, Sanfilippo FM, Preen DB, Bulsara MK. Comorbidity and repeat admission to hospital for adverse drug reactions in older adults: retrospective cohort study. BMJ. 2008;337:2752. doi: 10.1136/bmj.a2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rademaker M. Do women have more adverse drug reactions? Am J Clin Dermatol. 2006;2:349–51. doi: 10.2165/00128071-200102060-00001. [DOI] [PubMed] [Google Scholar]
- 30.Patel H, Bell D, Molokhia M, Srishanmuganathan J, Patel M, Car J, et al. Trends in hospital admissions for adverse drug reactions in England: analysis of national hospital episode statistics 1998-2005. BMC Clin Pharmacol. 2007;7:9. doi: 10.1186/1472-6904-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


