Abstract
Background & objectives:
Ascent to high altitude has been reported to cause hippocampal atrophy and cognitive impairment in mountaineers. We assessed the cognitive performance and probable occurrence of mild cognitive impairment (MCI) in acclimatized lowlanders (ALL) staying at altitudes above 4,300 m for duration above 12 months and validated a multi-domain cognitive screening test (MDCST) for future demographic studies on MCI.
Methods:
Following evaluation of sensitivity and correlation of the newly developed MDCST battery with Mini Mental State Examination (MMSE) and Clinical Dementia Rating (CDR) scores on a group of 28 individuals, the MDCST battery was validated on a population of 843 ALL staying at high altitude MSL >4,300 m and 862 subjects staying at MSL <230 m. EEG recordings were performed on 840 ALL staying at altitudes above 4,300 m and 743 control subjects staying at MSL <230 m.
Results:
Percentage prevalence of MCI was 4.18 per cent in the ALL population as assessed by MMSE while that of the LL population was <0.42 per cent. The percentage prevalence of MCI based on calculations from the MDCST scores was 12.4 per cent in the ALL population as compared to 1.19 per cent in the LL population. Decrease in alpha wave amplitude at the T3 and T4 sources in MCI subjects was observed in LL group while there was an increase in amplitude for alpha wave in these regions in the ALL groups. Domain specific MDCST showed decline in immediate recall, procedural memory and mind body co-ordination which was negligible in the LL population.
Interpretation & conclusions:
MDCST exhibited excellent psychometric properties in terms of sensitivity, and test-retest reliability qualifying it to be used as a more effective cognitive measure for assessment of MCI in demographic studies in comparison to traditional measures. Our findings also showed increased prevalence of MCI in ALL population staying for longer durations at high altitude which is neurophysiologically distinct from MCI leading to Alzheimer's disease.
Keywords: Electroencephalogram, high altitude, lowlander, mild cognitive impairment, psychometric assessment
The decrease in partial pressure of oxygen on ascent to high altitude has been reported to adversely affect the cognitive performance in both animals and human subjects. Occurrence of hippocampal atrophy and hypoxia mediated neurodegeneration has been shown following ascent to high altitude. There have been reports on increase in latency of P3 component reflecting sensory discrimination and delay in evaluation process and impairment in short term memory following ascent to high altitude1. Recent studies on a small group of human volunteers residing at high altitude revealed impairment in verbal working memory which could be associated with chronic hypoxia exposure2. However, most of these studies have either been performed in mountaineers or on subjects who have stayed at high altitude for shorter durations. No demographic study has ever been conducted to assess the prevalence of mild cognitive impairment (MCI) in the considerable size of human population that stay at high altitude for prolonged durations owing to professional or livelihood reasons.
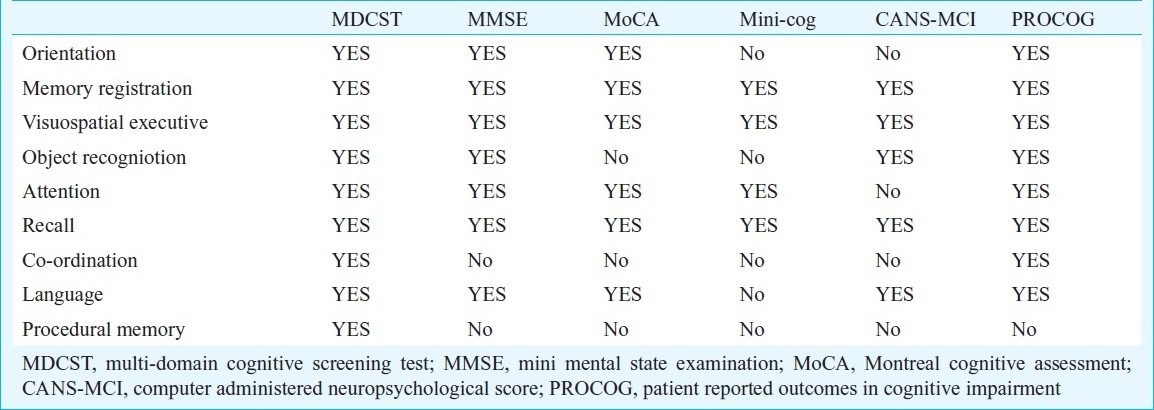
MCI, as the name suggests, is the early stage of cognitive impairment where only a single or a few of the cognitive domains are affected usually to a lesser extent. MCI is characterized by impairment in cognitive domain tests after correction for age and education, but with preserved general cognitive functioning, intact activities of daily living and absence of dementia3. It is however, an excellent indicator for preponderance and progression of an individual towards dementia and cognitive impairment4. The commonly used tests for screening MCI are Mini Mental State Examination (MMSE)5, Montreal cognitive Assessment (MoCA)6, Mini-Cog7, Computer Administered Neuropsychological Score (CANS-MCI)8 and the recently developed Patient Reported Outcomes in Cognitive Impairment (PROCOG)9. With the recent findings on involvement of several brain regions in cognitive functions and low predictive accuracy of several of the tests for MCI that are currently in use, there is a necessity to increase the scope of cognitive assessment to cognitive domains like procedural memory, mind-body co-ordination, attention and learning of complex tasks through improvised and customized psychometric tests. MMSE which is most widely used for demographic screening of MCI, has been shown to have low sensitivity and is highly influenced by age and education10,11. MoCA on the other hand, has better sensitivity than MMSE, takes a short duration of 10 min to be administered and has a wide application in routine clinical practice. However, MoCA covers only 10 cognitive domains and does not include procedural memory, mind-body co-ordination and learning of complex tasks. PROCOG comprises 55 questions, making it too lengthy to be administered routinely and is thus less preferred for demographic studies. It can rather be used as a confirmatory test following preliminary screening. Further, clinical practice of computer assisted tests like Computer Assessment of MCI (CAMCI)10 or CANS-MCI is difficult in remote locations and specifically in the high altitude regions owing to the technological requirements and administration skills.
The present study was, therefore, designed to investigate the percentage prevalence and extent of MCI in a young and healthy ALL population staying at altitudes above 4,300 m in the trans-Himalayan regions for durations longer than 12 months and to validate a newly designed multi-domain cognitive screening test (MDCST) for demographic studies in remote locations at high altitude. The MDCST scores were compared with MMSE and MoCA scores and the specificity and reliability were determined using electrophysiological recordings. Standard Medical Questionnaire for medical history, Everyday ability Scale for India (EDAS-I) and Clinical Dementia Rating (CDR) formed a part of the neuropsychologic battery and functional assessments performed during the investigation. All these parameters were compared with age, sex and education matched control subjects who had never been to high altitude. A sensitive, rapid, easy to administer and customized neuropsychological battery was used for the study.
Material & Methods
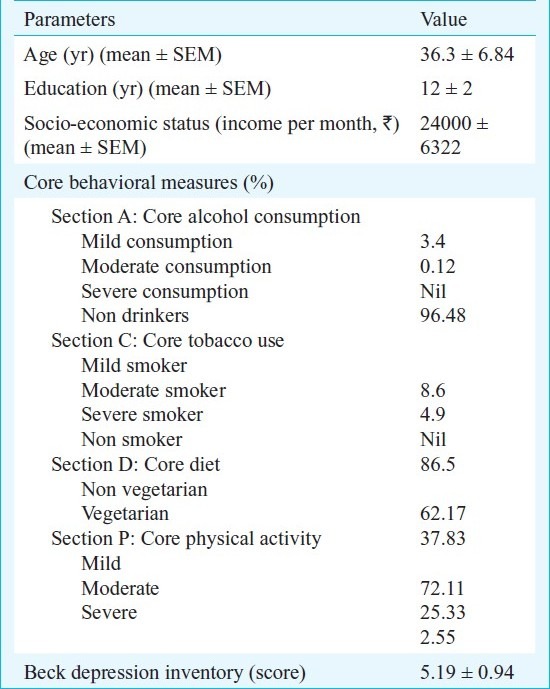
Subjects: The study was conducted in High altitude Physiology division of Defence Institute of High Altitude Research, Leh, India, during August 2009 - January 2011 after obtaining ethical clearance from the institutional ethics committee of Defence Institute of High Altitude Research. A total of 2000 volunteers comprising of male subjects with education of 10-12 yr and between age group of 25-45 yr enrolled voluntarily at different army unit locations after being explained about the study purpose, protocol, and expected outcomes. Amongst the total population, 1000 ALL volunteers staying at altitudes above 4,300 m for duration of more than 12 months were enrolled, of whom 843 qualified the inclusion criteria and participated in the study (Table I). Similarly, 1000 subjects comprising male volunteers of the same age group who resided at a MSL of <230 m in and around the metropolitan area of Delhi and had never been to high altitude were enrolled at Delhi and 862 subjects who met the inclusion criteria participated for the study. Thus, a total of 1705 healthy young male volunteers between the age group of 25-45 yr with no previous history of drug abuse, stroke, epileptic seizures or brain injury, CDR <0.5 and with 10-17 yr of education participated in the demographic study. Following recruitment of subjects, the studies were carried out in make shift set ups in the locations of availability of the subjects that also included remote residential areas in the high altitude region.
Table I.
Inclusion criteria of subjects in the study (n=843)
The draft MDCST was first tested on a small group of 28 individuals residing at MSL <230 m of whom 10 individuals between the age group of 35-45 yr had MMSE scores <25, with 8 in the age group of 60-65 yr had MMSE scores <20 and were previously diagnosed with mild Alzheimer's disease using Clinical Dementia Rating (CDR 1.0), and 10 individuals in the age group of 35-45 yr who were considered normal with MMSE scores >29. Following the evaluation of MDCST score on the test group, the score was further validated on the total population of 1705 volunteers and those having scores <35 were considered with MCI while those < 25 were considered moderate cognitively impaired. The correlation of outcome of MDCST with MMSE scores was determined.
Psychometric assessments: A medical questionnaire comprising questions related to occurrence of chronic diseases, physical and physiological ailments, heart problems, stroke, epilepsy, head injury, drug abuse, psychological disorders and general health status was administered to all the volunteers. Core behavioural measures (CBM) like core alcohol consumption (section A), core tobacco use (section C), core diet (section D) and core physical activity (section P) were also applied to all subjects in accordance with WHO guidelines12. Following short listing of the subjects who qualified the inclusion criterion, the EDAS-I13 and Beck Depression Inventory (BDI)14 were applied to assess activities of daily living and to investigate the presence of hitherto undetected depression. The information was verified from a close acquaintance of the subject. Lake Louis Score for acute mountain sickness (AMS) was administered only to the participants enrolled at Leh to negate possible occurrence of AMS symptoms. The neuropsychological assessment for MCI was performed through independent administration of MMSE, MoCA and MDCST batteries. The tests were administered by field investigators under the supervision of a clinical psychiatrist. General, physical and neurologic examination was performed by a clinician and the information was documented in a structured performa. Subjects with underlying heart disease, chest pain, stroke/infarction/cerebral haemorrhage, renal failure, diabetes, viral hepatitis, chronic disease and gastroesophageal reflux disease (GERD) were excluded. Subjects with previous neurologic/psychiatric symptoms, major surgery and familial disorders were also excluded. This ensured inclusion of only healthy subjects in this study.
The MDCST was designed to evaluate the cognitive domains involved in Orientation, Memory registration, Immediate recall, Visuo-spatial executive, Object recognition, Remote memory, Mind-body coordination, Learning, Attention, Problem solving, Language fluency, Delayed recall and Procedural memory (Table II). The score assessed larger number of cognitive domains as compared to MoCA and MMSE (Table III). Accepted methods for creation of a new patient-reported outcomes instrument were followed while designing the MDCST15. Each of the cognitive parameter was assigned equal weightage with respect to the total score and was to be assessed independently. The complete test was to be administered in a single session lasting for 5-10 min depending on individual variations. The procedure for administration of MDCST and the scoring awarded for each parameter was as follows:
Table II.
Psychometric behavioral paradigms
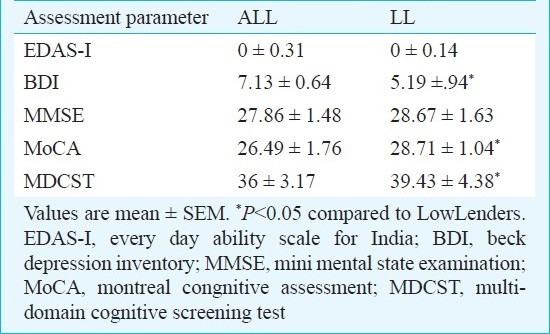
Table III.
Domain specific paradigms in cognitive assessment scores
Orientation: To assess orientation on the MDCST score, the subject had to answer his/her date of birth, present address, day, last festival, and name of head/director/employer. One point was awarded for each correct answer.
Memory registration: The subject was made to remember 5 logically unrelated words. The points awarded were equal to the number of words the subject remembered after repeating the words twice.
Visuospatial executive: The subject was made to match the words to numerical in the order A to 1, B to 2 and so on. The subject was made to replicate the cube and draw a clock with hour and minute hand showing 0800 h. On correct matching of the alphabets with the numbers, cube drawing and correct positioning of either the hour hand or minute hand, fetched the subject one point each. Drawing a clock with numbers written fetched the subject one point.
Object recognition and Remote memory: The subject was made to identify four unrelated objects. The subject was awarded with 1 point for each correct identification. The subject was also made to recall the name of two school teachers and was awarded one point for correct recall.
Mind-body co-ordination and learning: The subject was made to learn a complex task like tying a tie knot in 5 steps. The number of times the subject failed to learn the task was subtracted from 5 to obtain the final score. If the number of attempts were more than 5, the final score for learning the task was 0. If the subject learnt the task in the first attempt but took more than 3 min to complete it in the second and third attempt he was awarded 3 points.
Attention and problem solving: The subject was made to tap a finger depending on number of times ‘A’ appeared on different sites of the computer screen or number of times the administrator uttered the alphabet ‘A’ while reading a jumbled alphabet sequence. The subject was awarded one point on tapping the finger for correct number of times ‘A’ appeared in the jumbled alphabet sequence. The subject was made to read a sequence of numbers forward and then backward. On correct reading of the sequence in both the directions; the subject was awarded one point. For assessment of the problem solving ability, the subject was made to subtract 7 sequentially for four times, starting with 100 and one point was awarded for each correct result.
Language: The subjects were made to read 5 sentences in English or in the local dialect as preferred by the subject. Correct reading of each sentence resulted in awarding of one point.
Delayed recall: Delayed recall was assessed by making the subject recall the words that were presented during memory registration. Each correct recall led to award of one point. If the subject failed to recall 2 words, he was assessed for cued recall by asking to identify the correct words from a list of ten. On correct identification of all the words from the list, the subject was awarded with one point.
Procedural memory: The subject was given a single attempt to perform the complex task that he was made to learn in five steps for assessment of procedural memory. For each correct step the subject was awarded one point.
All the individual parameter scores were then summed to determine the total MDCST score. Subjects scoring >35 were considered to be normal, those scoring <35 were considered to have MCI.
The MDCST was administered to all the volunteers independently by a field investigator and a clinical psychiatrist and the scores were compared to determine the subjective reliability of the scoring. Percentage of volunteers having MCI on the MMSE, MoCA and MDCST test batteries were independently determined. Percentage overlaps of MCI individuals between the scores and those exclusive to each test were also computed. For test-retest reliability, 50 subjects found to have MCI on the MDCST and 50 normal subjects were randomly chosen from amongst the volunteers and the questionnaire was administered three months and six months after the initial test. The subjects were re-examined with the questionnaire for medical health, BDI and CBM prior to determination of test-retest reliability for MDCST.
Electroencephalography: Standard EEG electrode placement (10-20 system) was followed and recordings were acquired from eight electrodes using NeuroTravel-Mini EEG data recorder (ATES MEDICA Device, Italy) at a sampling rate of 500 Hz. Prior to the recordings it was ensured that the subject had a good sleep the previous night and did not take any medication for the last 24 hours. The electrodes were placed at Fp1, Fp2, T3, T4, C3, C4, O1 and O2 positions and the impedance of the electrode-skin interface was maintained below 5Ω. To monitor eye movements, horizontal and vertical electro-oculogram (EOG) was simultaneously recorded. Additional electrodes were placed on the lower jaw to gather electromyogram (EMG) signals resulting due to jaw movements. Data were acquired in eyes closed sitting position for 5 min after an initial latency of 30 sec for stabilization of the EEG waves. The data acquired from each channel were filtered using a 0.5 to 50 Hz filter and corrected for EOG and EMG artifacts, and 30 sec segments of artifact free data were used for power spectrum analysis of alpha, beta, theta and delta frequency bandwidths using AcqKnowledge 4.0.0 software (Biopac Systems, USA). The maximum amplitude of each bandwidth with respect to the source of origin was determined and spectral maps were computed.
Data analysis: Correlation coefficient for draft MDCST score with MMSE and CDR was determined. Scoring of the field investigators and that of the clinical psychiatrist was compared by paired ‘t’ test. The subjects were divided into four groups viz., Group 1: staying at MSL <230 m and normal, Group 2: staying at MSL <230 m and MCI, Group 3: staying at MSL >4,300 m and normal, Group 4: staying at MSL >4,300 m and MCI. Percentage prevalence of MCI was determined in all the populations based on the MDCST scores. One way analysis of variance (ANOVA) was performed to determine the level of significance between the groups. Newman-Keul statistics was calculated for post-hoc analysis. ‘Z’ test of proportion was performed to test the difference in proportion of population under the median scoring for MDCST, MMSE and MoCA. Correlation of MDCST scores with that of MMSE and MoCA was also determined. Internal consistency reliability was assessed for the cognitive parameters by Cronbach's formula for coefficient α on a scale of 0 to 1. Higher scores were indicative of more reliability and consistency. Test-retest reliability to measure the reliability of the scale and discriminant validity between groups was also determined9. P<0.001 was considered to be significant for all tests. Digital Fast Fourier transform (FFT) based power spectrum analysis was evaluated to calculate mean amplitude in the alpha, beta, theta and delta range. Peak values between the groups were compared independently for different regions of interest using one way ANOVA.
Results
The study population consisted of two cohorts viz. ALL and LL comprising 1000 volunteers each with similar age, education and sex. Among the 1000 volunteers (ALL) staying at MSL >4,300 m for >12 months who were initially enrolled for the study, 96 were chronic alcoholics, 13 had severe brain injury in the past, 31 had history of chronic illness in recent past and 17 were unavailable for the complete test procedures. Thus, 843 healthy ALL of Indian ethnicity participated in the study, Similarly, among the 1000 volunteers (LL) staying at MSL <230 m and who had never been to high altitude, 23 had severe head injury, 29 had history of chronic illness in recent past, 12 did not complete the test procedure, 72 were chronic alcoholics and 2 subjects had an history of epileptic seizures. The population thus comprised of 862 low lander (LL) volunteers of Indian ethnicity.
The draft MDCST score in the test cohort of 28 individuals showed high correlation coefficient (0.96) with MMSE and CDR scores. The MDCST score was then applied to both ALL and LL groups. Comparison of the MDCST scores with MMSE and MoCA showed correlation coefficients of 0.62 and 0.84, respectively.
The mean score for EDAS-I, BDI, MMSE, MoCA and MDCST are summarized in Table II. The average EDAS-I score for the ALL group was 0 ± 0.31 while that for the LL group was 0 ± 0.14. The average Lake Louis Score which is an indicator of AMS was 0 ± 0.43 for the ALL population. The average BDI score for the ALL population was 7.13 ± 0.64 while that for the LL was 5.19 ± .94. Based on the BDI scores, percentage prevalence of depression in the ALL population was calculated to be 8.69 per cent as compared to 1.04 per cent in the LL population. Similarly, the mean MMSE score for the ALL population was 27.86 ± 1.48 and percentage prevalence of MCI was 4.18 per cent while that of the LL population was 28.67 ± 1.63 and percentage prevalence of MCI was 0.42 per cent. The mean MoCA scores for the ALL and LL population was 26.49 ± 1.76 and 28.71 ± 1.04, respectively. The difference between both the populations was more evident in the MDCST in which ALL had a population mean of 36 ± 3.17 as compared to 39.43 ± 4.38 in the LL population. The percentage prevalence of MCI based on calculations from the MDCST scores was 12.4 per cent in the ALL population as compared to 1.19 per cent in the LL population.
Table III shows a comparative evaluation of the cognitive domains assessed by MDCST and other tests. The average time of a session for administration of MDCST was determined to be 8.34 ± 0.24 min. Subjective reliability of administration of MDCST by field investigator showed 97.8 per cent accuracy with P<0.001 when compared to that by the clinical psychiatrist. As shown in Table IV, six cognitive domains viz. Visuo-spatial executive, Attention, Mind-body co-ordination, Immediate recall, Delayed Recall and Procedural memory contributed more towards the MCI in the ALL population while MCI in the LL population was primarily due to impairment in Visuo-spatial executive, Attention and Delayed recall. While 28 per cent of the total MCI subjects of the ALL group showed amnestic MCI, 63 per cent showed multi-domain MCI and 9 per cent had single non-memory domain MCI. On the contrary, 42 per cent of the total MCI subjects of the LL group had amnestic MCI and 31 per cent showed multi-domain MCI, and the remaining 27 per cent had single non memory domain MCI. No statistically significant difference was observed between the scores of MDCST during the test and retest. Discriminant validity test for MDCST showed significant difference between the scores of normal and MCI individuals. All the 79 subjects found positive for MCI on the basis of MMSE scores also had positive scores on MoCA and MDCST. However, 40 subjects were found to be normal on both MMSE and MoCA but had MCI positive scores on MDCST. The average population mean for the MDCST score of normal subjects was 39.43 while that of the MCI individuals was 29.31 (Fig. 1).
Table IV.
Domain specific scoring on administration of MDCST
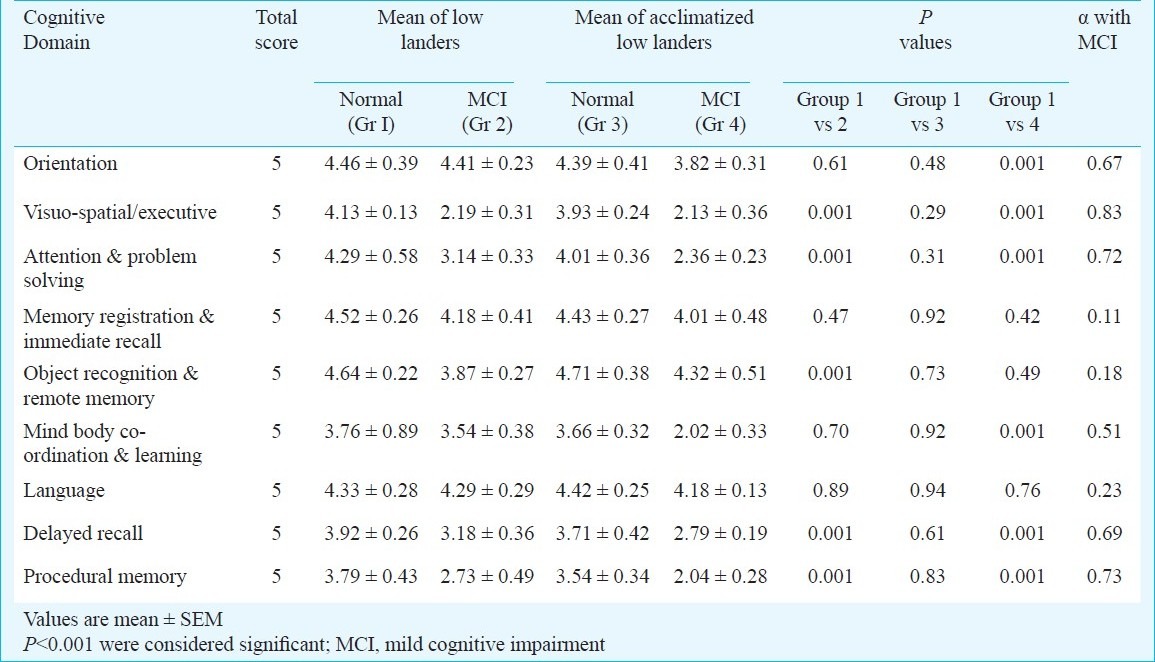
Fig. 1.
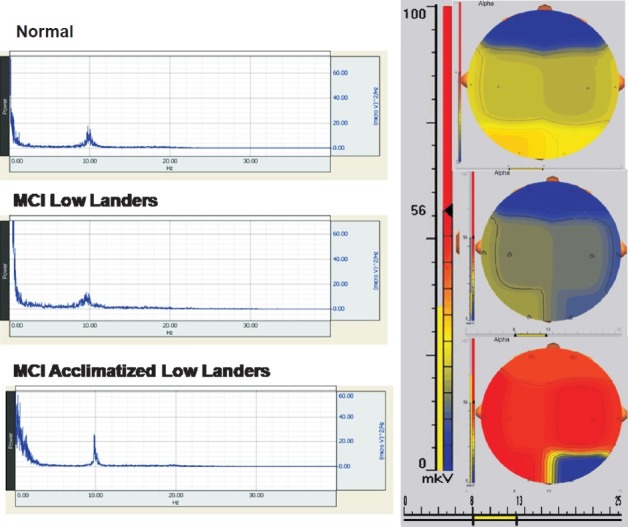
Power spectrum analysis of alpha waves. Comparison of spectral brain maps for regional activity of Normal, MCI individuals.
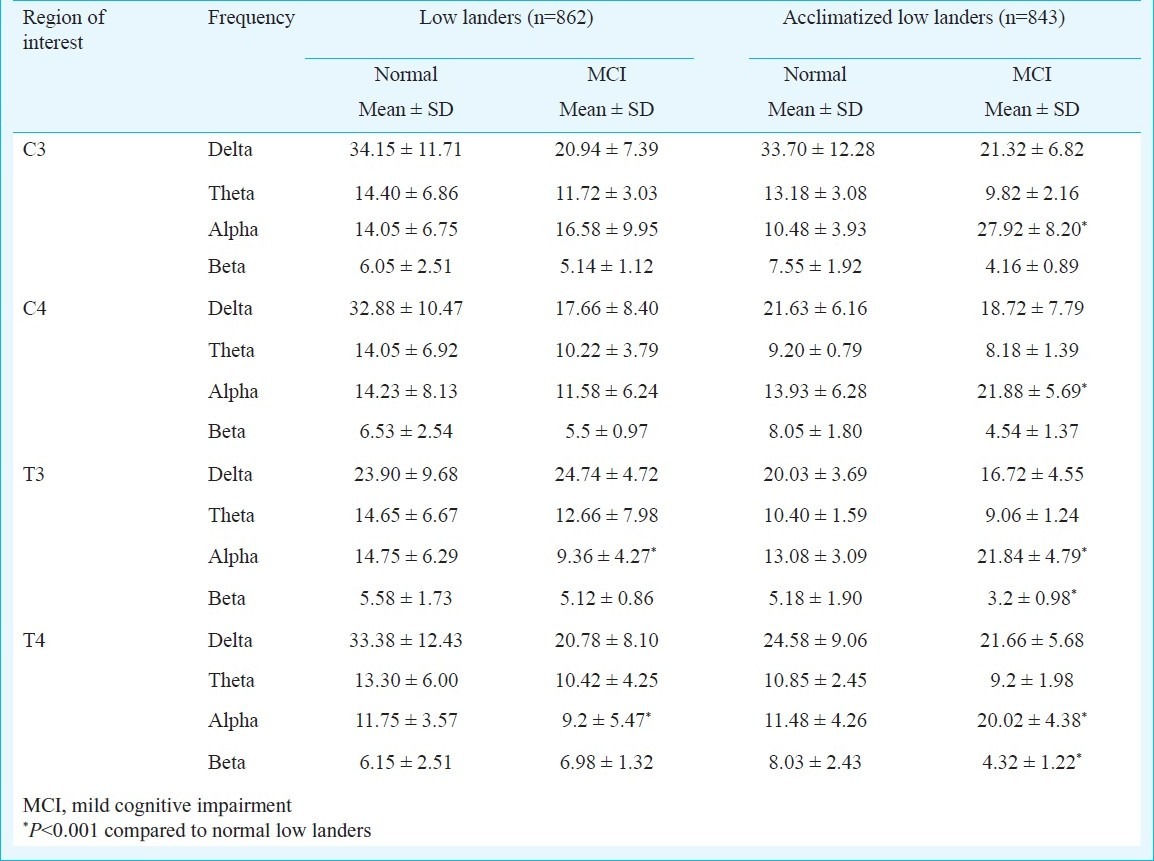
Power spectrum analysis of the EEG data (Fig. 2) acquired from resting subjects in eyes closed position showed decrease in alpha wave amplitude at the T3 and T4 sources in MCI subjects belonging to the LL group while there was increase in amplitude values for alpha wave in these regions in the ALL groups (Table V). Interestingly, the subjects diagnosed with MCI in the ALL group also showed decreased amplitude values in the beta range in the T3 (3.2 ± 0.98, P<0.001) and the T4 (4.32 ± 1.22, P<0.001) sources when compared to the normal LL subjects as well as LL diagnosed with MCI. In contrast to the LL population, the MCI subjects in the ALL population also had increased alpha amplitudes in the C3 (27.92 ± 8.20, P<0.001) and C4 (21.88 ± 5.69, P<0.001) regions.
Fig. 2.
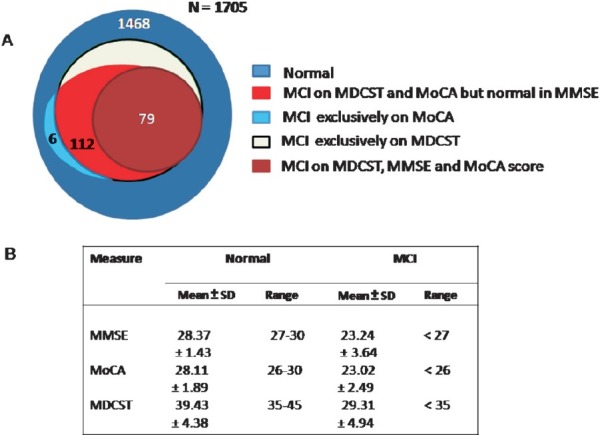
Comparison of MDCST, MoCA and MMSE Scores. (A) Graph showing percentage prevalence of MCI in the volunteers when assessed independently by MDCST, MoCA and MMSE. (B) Scores gained Normal and MCI individuals when assessed independently by Multi domain cognitive screening test (MDCST), Montreal cognitive assessment (MoCA) and Mini mental state examination (MMSE).
Table V.
Amplitudes of EEG waves
Discussion
The present study was an attempt to investigate the effect of prolonged stay at high altitude on the cognitive performance of ALL. The study also differs from previous investigations in terms of domain specific evaluation of cognitive performance at high altitude in a considerably large population. Besides that, the psychological assessment was coupled with electrophysiological recordings to obtain quantitative measures for high altitude induced cognitive impairment. Only healthy subjects with no clinical antecedents of depression, alcoholism or drug abuse were recruited to negate the influence of these factors on the cognitive performance. The subjects were recruited randomly in both the high altitude and low altitude locations according to their qualification in the inclusion criterion.
Keeping in mind the limitations of MMSE and MoCA, MDCST was designed to establish an easy to administer and more sensitive test for detection of early stages of MCI. The test was validated in a small group by adhering to standard procedures as mentioned in previous literatures. The key requirements of psychological tests including good test retest reliability16, validity, practice effects and equivalent forms were evaluated prior to being implemented during this demographic study. MDCST exhibited a correlation coefficient of 0.96 at 3 months and 0.93 at 6 months indicating high test retest reliability. The test also had a Cronbach's alpha of 0.87 indicating excellent internal consistency17.
Psychological assessment of the ALL and LL populations with MMSE, MoCA and MDCST showed increased percentage prevalence of MCI in the ALL population when compared to the LL population. Domain specific assessment by MDCST showed decline in visuo-spatial executive, attention and delayed recall in the subjects showing MCI in both the LL and ALL populations. The MCI subjects in the ALL population also showed decline in immediate recall, procedural memory and mind body co-ordination which was negligible in the LL population. This is perhaps the first study on high altitude related cognitive impairment that reports the specific domains affected due to global hypobaric hypoxia. Though our previous studies1,18 have shown a decrease in vigilance and an increase in reaction time after stay at high altitude for a short duration of 3 months, the other cognitive domains remained to be studied.
Diagnosis of MCI was also established by analysis of EEG data acquired from resting subjects in eyes closed position. Consistent to the findings of Babiloni et al19 for progressive MCI, we observed a decrease in alpha wave amplitude in the T3 and T4 regions of subjects showing MCI in the LL group. MCI subjects on the other hand showed increased alpha wave amplitude at the T3, T4, C3 and C4 sources along with decrease in beta wave amplitude in the T3 and T4 regions.
The study however, had a few limitations. Longitudinal study on the progression of mild MCI to moderate MCI and cognitive impairment needs to be performed in a clinical set up to extend the utility of the test for clinical practice in detection of Alzheimer's disease and vascular dementia. Since all the subjects in the present study had education of 10-12 years, the efficacy of the test in illiterate population also needs to be validated. Another limitation in the study was that the EEG recordings were performed with 8 channels which was due to logistic problems in the remote locations in the high altitude regions. Also, since a major part of the study was conducted in actual field conditions greater than 4300 m, visual and auditory evoked potential could not be studied due to the logistic problems like availability of adequate power source, portable equipment, etc.
In summary, MDCST exhibited excellent psychometric properties in terms of sensitivity, and test-retest reliability qualifying it to be used as a more effective cognitive measure for assessment of MCI in demographic studies in comparison to traditional measures. The domain specific evaluation of cognitive performance using MDCST could also assist in detection of early stages of MCI and in clinical assessment of its progression as well as the effectiveness of the therapy being implemented to reverse or decrease its progression. The study also showed the increased prevalence of MCI in ALL staying for longer durations at high altitude which is neurophysiologically distinct from MCI leading to Alzheimer's disease. We hypothesize that the effect of global hypoxia at high altitude could be different from vascular dementia and more adversely affect the cognitive performance due to its manifestation on all the brain regions. Further investigations on the brain function and electrophysiology in both these conditions could provide information that would be helpful in devising clinical management strategies for hypobaric hypoxia induced cognitive impairment.
Acknowledgment
The study was supported by Defence Research and Development Organization (DRDO), Ministry of Defence, Government of India. The authors acknowledge the contribution of Ladakh Institute of Prevention, Leh, India.
References
- 1.Singh SB, Thakur L, Anand JP, Panjwani U, Yadav D, Selvamurthy W. Effect of high altitude (HA) on event related brain potentials. Indian J Physiol Pharmacol. 2003;47:52–8. [PubMed] [Google Scholar]
- 2.Yan X, Zhang J, Gong Q, Weng X. Prolonged high-altitude residence impacts verbal working memory: an fMRI study. Exp Brain Res. 2011;208:437–45. doi: 10.1007/s00221-010-2494-x. [DOI] [PubMed] [Google Scholar]
- 3.Petersen RC, Stevens JC, Ganguli M, Tangalos EG, Cummings JL, DeKosky ST. Practice parameter: early detection of dementia: MCI (an evidence-based review).Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1133–42. doi: 10.1212/wnl.56.9.1133. [DOI] [PubMed] [Google Scholar]
- 4.Morris JC, Storandt M, Miller JP, McKeel DW, Price JL, Rubin EH, Berg L. Mild cognitive impairment represents early-stage Alzheimer disease. Arch Neurol. 2001;58:397–405. doi: 10.1001/archneur.58.3.397. [DOI] [PubMed] [Google Scholar]
- 5.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State” A practical method for grading cognitive state of patients for the clinicians. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 6.Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 7.Borson S. The mini-cog: a cognitive “vitals signs” measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15:1021–7. doi: 10.1002/1099-1166(200011)15:11<1021::aid-gps234>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 8.Jane BT, Emory H, Laboff JA. Self-Administered Screening for Mild Cognitive Impairment: Initial validation of a computerized test battery. J Neuropsych Clin Neurosc. 2005;17:98–105. doi: 10.1176/appi.neuropsych.17.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lori F, Jennifer AF, Leah K, Mary KM, Louis SM, Cornelia B, et al. Validation of a new symptom impact questionnaire for mild to moderate cognitive impairment. Int Psychogeriatr. 2006;18:135–56. doi: 10.1017/S1041610205002887. [DOI] [PubMed] [Google Scholar]
- 10.Saxton J, Morrow L, Eschman A, Archer G, Luther J, Zuccolotto A. Computer assessment of mild cognitive impairment. Postgrad Med. 2009;121:177–85. doi: 10.3810/pgm.2009.03.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Visser PJ, Kester A, Jolles J, Verhey F. Ten-year risk of dementia in subjects with mild cognitive impairment. Neurology. 2006;67:1201–7. doi: 10.1212/01.wnl.0000238517.59286.c5. [DOI] [PubMed] [Google Scholar]
- 12.Switzerland: WHO STEPS Surveillance; [accessed on August 12, 2008]. World Health Organization. Available from: www.who.int/chp/steps . [Google Scholar]
- 13.Fillenbaum G, Chandra V, Ganguli M, Pandav R, Gilby J, Seaberg E, et al. Development of an activities of daily living scale to screen for dementia in an illiterate rural older population in India. Age and Ageing. 1999;28:161–8. doi: 10.1093/ageing/28.2.161. [DOI] [PubMed] [Google Scholar]
- 14.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 15.Leidy N K, Revicki DA, Geneste B. Recommendations for evaluating the validity of quality of life claims for labeling and promotion. Value Health. 1999;2:113–27. doi: 10.1046/j.1524-4733.1999.02210.x. [DOI] [PubMed] [Google Scholar]
- 16.Ferris SH, Kluger A. Assessing cognition in Alzheimer disease research. Alzheimer Dis Assoc Disord. 1997;11:45–9. [PubMed] [Google Scholar]
- 17.Kline JP, Schwartz GE, Dikman ZV, Bell IR. Electroencephalographic registration of low concentrations of isoamyl acetate. Conscious Cogn. 2000;9:50–65. doi: 10.1006/ccog.1999.0422. [DOI] [PubMed] [Google Scholar]
- 18.Singh SB, Thakur L, Anand JP, Yadav D, Amitab, Banejee PK. Effect of chronic hypobaric hypoxia on components of the human even related potential. Indian J Med Res. 2004;120:94–9. [PubMed] [Google Scholar]
- 19.Babiloni C, Frisoni GB, Vecchio F, Lizio R, Pievani M, Cristina G, et al. Stability of clinical condition in mild cognitive impairment is related to cortical sources of alpha rhythms: An electroencephalographic study. Hum Brain Mapp. 2011;32:1916–31. doi: 10.1002/hbm.21157. [DOI] [PMC free article] [PubMed] [Google Scholar]


