Abstract
Background:
In recent years the incidence of Tinea capitis, infection of scalp by dermatophytes, has increased in United Kingdom and North America. The trend may be similar in India. The objective of this study is to find the prevalence of Tinea capitis in school going urban children in Kolkata, West Bengal state.
Materials and Methods:
The present study is a cross-sectional study conducted in a government higher primary school in Kolkata.
Results:
Totally 505 students were screened and 52 were diagnosed to have Tinea capitis by clinical examination, giving a prevalence rate of 10% among school children. Prevalence rates among the age groups of 6–8, 9–11 and 12–14 years were almost the same, ranging from 9 to 11%. The prevalence rate was significantly high among the boys (14%). There was no significant difference in prevalence of infection among coconut oil users and castor oil users. Measures of general hygiene were similar among those who were infected with Tinea capitis and those who were not. The commonest clinical type of infection found was dull grey patches. Itching with hair loss was the major symptom and most of the infected children had cervical lymphadenopathy. The potassium hydroxide studies revealed endothrix spores in majority of samples.
Conclusion:
Tinea capitis in prevalent in school going urban children in Kolkata, West Bengal state and necessary measures must be undertaken to curtail this incidence.
Keywords: Prevalence, school children, Tinea capitis
INTRODUCTION
Tinea capitis is a fungal infection of the scalp hair follicles and the surrounding skin caused by dermatophytes. Dermatophytes are a unique group of fungi that infect keratinous tissue of lower animals and humans. The genera include Trichophyton, Epidermophyton and Microspora. They are characterized by their ability to invade the superficial layers of the epidermis, particularly the stratum corneum and the high keratin-concentration containing appendages, the hair and nails of the living host. Only under exceptional circumstances do they survive or proliferate in the deeper tissues of the body. Tinea capitis is one of the most common dermatophytosis seen in school going children, with diverse clinical presentations and a worldwide prevalence. Children are particularly susceptible to dermatophytic infections because of their poor personal hygiene habits and poor environmental sanitation. The disease may present in different patterns i.e. kerion, agminate folliculitis, favus, black dot or grey patch type. Tinea capitis is mainly observed in the school going children, more frequent in boys compared with girls.[1] Transmission occurs via infected persons, shed infected hair, animal vectors and fomites. Clinically it is characterized by erythema, scaling, pruritus and alopecia. It is very rarely seen among adults. Moreover, the infection can exist as an asymptomatic carriage in children, which in turn may be a source for its anthroponotic transmission. Anthropophilic organism Trichophyton tonsurans and T. violaceum are presumed to be associated with higher rates of asymptomatic carriage. Asymptomatic carriage is considered to correlate with incidence of Tinea capitis in a community. Asymptomatic carriers are the subjects with no clinical signs and symptoms of the disease but are culture positive for the fungi responsible for Tinea capitis. In Spain and Italy, the frequency of asymptomatic carriage is reported to be 0.2% and 0.3%, respectively. A higher rate of the carriage and asymptomatic disease has been reported from South Africa. Most of the studies in our part of the world have shown T. violaceum to be the most common pathogen although other organisms are occasionally found. In recent years, the incidence of Tinea capitis has increased in United Kingdom particularly among the Afro-Caribbean children living in large cities.[2] This is one of the problems which is of increasing public health importance in North America.[3] There are only a few studies on the prevalence in India.[4–7] Tinea capitis is not a reportable disease but is a cause of concern because of its contagious nature. Children are particularly susceptible to Tinea capitis as contact among children is more frequent between the school ages of 6 and 14 years than in early childhood; this age group is at greater risk of contracting infectious diseases. For this reason school surveys are good at measuring the magnitude of the problem.
The objective of the present communication is to present the prevalence of Tinea capitis in school going urban children in Kolkata, West Bengal State and to find out if there is a similar trend of increase in the prevalence. An assessment of sex-wise distribution and the influence of measures of personal hygiene (head bath, oil and shampoos) on the prevalence of Tinea capitis has also been carried out.
MATERIALS AND METHODS
The study was planned as a cross-sectional study to assess the prevalence of Tinea capitis. The approval of the institutional ethical committee was obtained for conducting the study. Students with the consent of their parents were enrolled. The study was carried out in one Government higher primary school in Kolkata city. The school had a total strength of about 505 students in the age group of 6–14 years. All the children (classes I–VII standard) were included in the study. Students, not in the age group of 6–14 years were excluded from the study. Exclusion criteria were students receiving anti-fungal treatment, but no such history of medication was found.
The data was collected through:
Questionnaires designed and adapted for collecting demographic and socio-economic aspects of the child. The socioeconomic status of the students surveyed was categorized into high level (satisfactory) and low level (unsatisfactory). This categorization took onto account many factors that contribute to the living standards: family size, family income, parents educational level and parents employment status. The level of crowding at home was calculated as the number of persons living at home per room.
Clinical examination of all the children with/without relevant symptoms for Tinea capitis: All areas of the scalp were thoroughly examined for evidence of scaling, crusting, follicular inflammation, hair loss or erythema. Other parts of the body (nails, hands, chest and legs) were examined for any evidence of scaling or erythema.
Potassium hydroxide studies of hair samples from suspected cases of Tinea capitis as per standard procedure. Hair samples were obtained by sterile hairbrush technique. Specimens were subjected to light microscopy after treating with 25% potassium hydroxide solution.
Operational constraints
Conducting a community-based survey in a developing country is fraught with problems. The main problems we encountered and the steps we took to resolve them were:
Most people interviewed (teachers and children) were unaware of Tinea capitis; its clinical features, mode of transmission and prognosis.
Before examination and data collection we had to advise the schools on the nature of tinea captis and the objectives of our visit.
To ease the anxieties of children about the examinations and hair removal, the survey team had to spend considerable time explaining the procedure and allaying fears.
Obtaining questionnaire information from children under 9 years of age was particularly difficult. Information often had to be obtained from older siblings, teachers or from the students file.
Incorrect information was sometimes given, particularly regarding monthly income and personal hygiene (frequency of bathing). As a consequence, the monthly income was ignored during data analysis and personal hygiene was assessed by the survey team during interview.
The individuals observed to have Tinea capitis in clinical examination were taken as “cases” for the study. The data were collected using the questionnaire and entered into a computer on SPSS (Statistical Package for Social Sciences). Pearson's Chi-square test was used to test for statistical significance. A P value of <0.05 was taken as statistically significant.
RESULTS
Out of 505 students screened in the study, 52 were observed to have Tinea capitis by clinical examination, providing an overall prevalence rate of 10% among the school children.
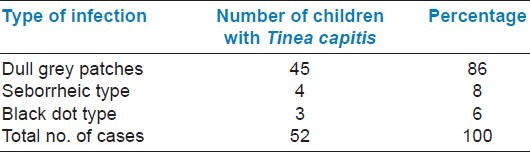
There was no significant difference in the prevalence rates between the age groups indicating an almost similar prevalence rate ranging from 9 to 11% in the age groups 6–8, 9–11 and 12–14 years [Table 1]. The prevalence rate among boys was 14% compared to the 5% in girls and the difference in the prevalence rate was significant [Table 2]. The most common clinical type of Tinea capitis among the school children was dull grey patches [Table 3].
Table 1.
Prevalence of Tinea capitis according to age
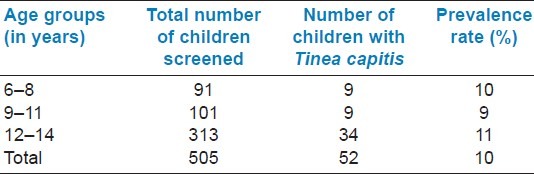
Table 2.
Sex-wise prevalence of Tinea capitis
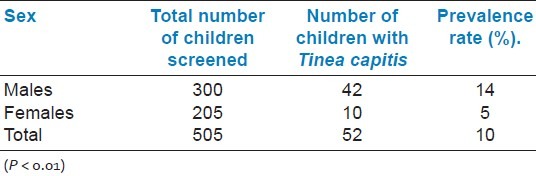
Table 3.
Distribution of clinical types of Tinea capitis
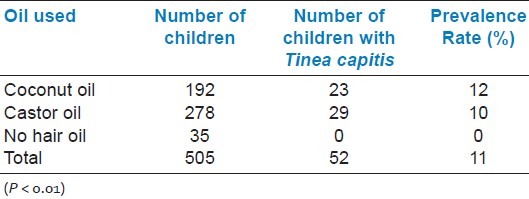
Bathing habits among children such as frequency of head bath, use of shampoos and use of hair oils was obtained from all the children. It was observed that in the children with Tinea capitis and in the children without Tinea capitis, the measures of personal hygiene (bathing habits) were similar. Among the 505 students, 38 students did not use hair oil at all. But they had no symptoms of Tinea capitis. No significant difference was observed between children using coconut oil or castor oil [Table 4].
Table 4.
Prevalence of Tinea capitis according to the hair oil used
Potassium hydroxide studies were carried out on hair samples from 52 clinically identified cases of Tinea capitis. Spores were found in 48 cases; endothrix spores were observed in 39 cases and ectothrix spores were seen in 9 cases. Out of the 52 children who had Tinea capitis, 48 children had cervical lymphadenopathy.
DISCUSSION
The prevalence rate of Tinea capitis in school going children in Kolkata city was observed to be 10%. Ghannoum et al.[3] in Cleveland estimated a prevalence of 13%, and found that all the affected were African American children. In another study in London, Hay et al. observed that the prevalence ranged between 0 and 12% with a mean of 2.5%.[8] Two studies carried out in Africa reported a prevalence rate of 33.3%.[9] and 11.3%.[1] A study in Rajasthan carried out among persons with superficial mycosis estimated the incidence of Tinea capitis to be 4.43%.[4]
The prevalence among the boys is about 14% and among the girls is about 5%, giving a male to female ratio of 2.8:1. The male preponderance in the present study is observed to be higher than studies carried out at Kenya and Rajasthan; 2:1[9] and 1.8:1,[4] respectively.
There was no significant difference in the prevalence rate of Tinea capitis between different age groups in school children of Kolkata city. Menan et al.[1] observed a higher incidence among the children in the age group of 8–11 years, and Ayaya et al.[9] have reported a significantly higher number of affected children of around the age of 10 years. Singhal et al.[6] in a study carried out in Delhi have found that 90% of the children with Tinea capitis were below the age of 15 years.
The present study has observed that the prevalence of Tinea capitis among the children who used coconut oil was 12% and among those who used castor oil was 10% and the difference was not significant. Kalla et al.[4] showed a decrease in severity of the lesion among those who used hair oil regularly.
Potassium hydroxide test was positive in 92% of case with Tinea capitis, and 81% of these samples showed endothrix spores. The study of Kumar et al.[6] in Delhi has identified endothrix spores in 88% of the samples studied and Reddy et al.[7] in Pondicherry had endothrix spores in 58.8% of the samples evaluated.
CONCLUSION
The present study reveals a prevalence of 10% of Tinea capitis among the school going urban children aged 6–14yrs in Kolkata, West Bengal. The prevalence was similar in different age groups. The prevalence rate in boys was higher than that in girls. The influence of traditional practices of personal hygiene on the prevalence of Tinea capitis was observed to be not significant. Lymphadenopathy was present in majority of the cases. Itching with hair loss was the major symptom and dull grey patches were the commonest clinical type of Tinea capitis. Endothrix spores were predominantly found in samples subjected to potassium hydroxide studies.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Menan El, Zongo Bonou O, Rouet F, Kiki-barro PC. Tinea capitis in school children from Ivory coast (western Africa) A 1998-1999 cross sectional study. Int J Dermatol. 2002;41:204–7. doi: 10.1046/j.1365-4362.2002.01456.x. [DOI] [PubMed] [Google Scholar]
- 2.Buckley DA, Fuller LC, Higgins EM, du Vivier AW. Tinea capitis in adults. BMJ. 2000;320:1389. doi: 10.1136/bmj.320.7246.1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghannoum M, Isham N, Hajjeh R, Cano M, Al-Hasawi F, Yearick D, et al. Tinea capitis in Cleveland: Survey of elementary school students. J Am Acad Dermatol. 2003;48:189–93. doi: 10.1067/mjd.2003.109. [DOI] [PubMed] [Google Scholar]
- 4.Kalla G, Begra B, Solanki A, Goyal A, Batra A. Clinico-Mycological study of Tinea capitis in Desert district of Rajasthan. Indian J Dermatol Venereol Leprol. 1995;61:342–5. [PubMed] [Google Scholar]
- 5.Singhal A, Rawat S, Bhattacharya SN, Mohanty S, Baruah MC. Clinico mycological profile of Tinea capitis in North India and response to griseofulvin. J Dermatol. 2001;28:22–6. doi: 10.1111/j.1346-8138.2001.tb00081.x. [DOI] [PubMed] [Google Scholar]
- 6.Vijay K, Sharma RC, Ram C. Clinico mycological study of Tinea capitis. Indian J Dermatol Venereol Leprol. 1996;62:207–9. [PubMed] [Google Scholar]
- 7.Reddy BS, Swaminathan G, Reba K, D’Souza M. Clinico mycological study of Tinea capitis in Pondicherry. Indian J Dermatol Venereol Leprol. 1991;57:180–2. [Google Scholar]
- 8.Hay RJ, Clayton YM, De Silva N, Midgley G, Rossor E. Tinea capitis in South-east London a new pattern of infection with public health implications. Br J Dermatol. 1996;135:955–8. doi: 10.1046/j.1365-2133.1996.d01-1101.x. [DOI] [PubMed] [Google Scholar]
- 9.Ayaya SO, Kamar KK, Kakai R. Aetiology of Tinea capitis in school children. East Afr Med J. 2001;78:531–5. doi: 10.4314/eamj.v78i10.8963. [DOI] [PubMed] [Google Scholar]


