Abstract
Background:
The mandibular foramen (MF) is an opening on the internal surface of the ramus for divisions of the mandibular vessels and nerve to pass. The aim of this study is to determine the position of the MF from various anatomical landmarks in several dry adult mandibles.
Materials and Methods:
A total of 102 human dry mandibles were examined, of which 93 were of dentulous and 9 were of edentulous. The measurements were taken from the anterior border of the ramus (coronoid notch) to the midportion of the MF and then from the midportion of the MF to the other landmarks such as internal oblique ridge, inferior border, sigmoid notch, and condyle were measured and recorded.
Results:
The data were compared using Student's t-test. The MF is positioned at a mean distance of 19 mm (with SD 2.34) from coronoid notch of the anterior border of the ramus. Superio-inferiorly from the condyle to the inferior border MF is situated 5 mm inferior to the midpoint of condyle to the inferior border distance (ramus height).
Conclusion:
We conclude that failures in the anesthesia of the inferior alveolar nerve are due to the operator error and not due to the anatomical variation.
Keywords: Failure of anesthesia, inferior alveolar nerve, mandible foramen
INTRODUCTION
The mandibular foramen (MF) is an opening on the internal surface of the ramus for divisions of the mandibular vessels and nerve to pass. The mandibular canal starts at the MF and descends obliquely forward in the ramus, and later in the body of bone containing the inferior alveolar neurovascular bundle.[1] This study was conducted to localize the MF accurately in several dry adult mandibles and provide the data to our students and practitioners in dentistry to improve their technique on the inferior alveolar nerve anesthetic method.
The assessment of the MF is of a considerable importance for inferior alveolar nerve anesthesia, dento alveolar surgery planning, endodontic treatments, and lesions diagnosis. Incorrect estimations of its location might be the explanation to the unsuccessful anesthesia of the inferior alveolar nerve.[2]
The most frequent technique failure in anesthesia of the inferior alveolar lies in the inappropriate setting of the needle, due to the inaccurate location of anatomic structures mandible foramen[3]
Anesthesia in the mandible may be associated with some difficulty. The success of this technique depends on the proximity between the anesthetic needle and the MF.[4]
Imperfections in the attainment of the anesthesia of the lower alveolar nerve must generally due to the lack of observance of the localization of the mandible foramen, noticing them its variations.[5]
Numerous articles in the literature describe the anatomic structures relevant to successful mandibular anesthesia, but failures in this technique still persist.[6]
The absence of a specific anatomic bony landmark, along with variations in the ramus width and height and the inferior alveolar nerve foramen position, is responsible for failure to achieve profound anesthesia. Some authors have estimated the failure rate of inferior alveolar nerve blocks to be approximately 20–25%.[7]
The past studies revealed the importance of MF in the success of InferiorAlveolarNnerveBlock.(IANB) Although several reports in the literature mentioned about the MF position from various landmarks, no study was available to explain the technical aspect of the nerve block to overcome these failures. The purpose of this study is to determine the position of the MF from various anatomical landmarks in several dry adult mandibles and provide valuable information for dental students and dental practitioners.
Aims and objectives
The purpose of this study is to identify the landmarks that would provide the most reliable and predictable indicators of the exact position of the MF and to provide the clinician with a suitable modifications in the technique to accommodate these variations.
MATERIALS AND METHODS
This study was carried out in Department of Anatomy, Faculty of Medicine, University of Vinayaka, India, for a period of 6 months from Jan 2011 to July 2011. A total of 102 human dry mandibles were examined, of which 93 were of dentulous and 9 were of edentulous. The measurements were taken from the anterior border of the ramus (coronoid notch) to the midportion of the MF and then from the midportion of the MF to the posterior border of the ramus. Similarly, from the midpoint of foramen to other landmarks such as internal oblique ridge, inferior border, sigmoid notch, and condyle were measured and recorded. The distances from the MF to various landmarks were calculated as a mean of two measurements recorded independently by two people. Measurements were recorded to the nearest millimeter. All the measurements were registered in millimeters. The ramus height from the head of condyle to the inferior border of mandible was also measured. The location of the foramen in relation to the mandibular occlusal plane and the coronoid notch was determined and recorded.
RESULTS
Tables 1–4 show the results obtained in this study. The mean distance of MF from various landmarks of dentulous and edentulous mandible is shown in Figures 1–3. The MF is positioned at a mean distance of 19 mm (with SD 2.34) from the coronoid notch of the anterior border of the ramus. It was found in this study that the location of MF is not at the centre of ramus in the horizontal plane. It is situated at a distance of 2.75 mm posterior to the midpoint of anteroposterior width of ramus. Superio-inferiorly (ramus height) the MF is situated 5 mm inferior to the midpoint of the condyle-inferior border height in a vertical plane. Superio-inferiorly from the sigmoid notch to the inferior border the MF was situated 3 mm above the midpoint of the sigmoid to the inferior border height. It was found in this study that the MF was either at the level of occlusal plane of lower molars or few millimeters below the level of occlusal plane of lower molars. The location of MF was found to be around 10 mm inferior to the level of coronoid notch of the anterior border. The MF was located few millimeters above the cervical margins lower molars.
Table 1.
Anterior boarder to mandibular foramen distance in mm
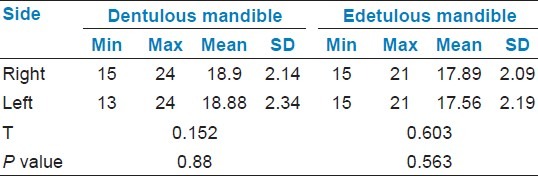
Table 4.
Inferior boarder to mandibular foramen distance in mm

Figure 1.

Localization of MF from various landmarks
Figure 3.
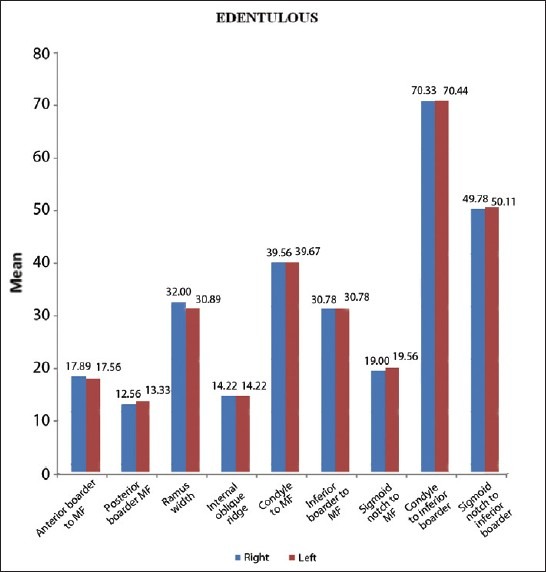
MF distance from various landmarks in edentulous mandible
Table 2.
Posterior boarder to mandibular foramen distance in mm
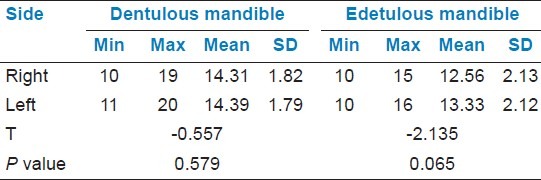
Table 3.
Condyle to mandibular foramen distance in mm
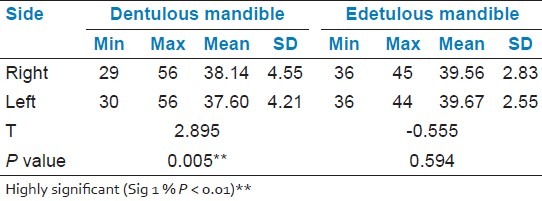
Figure 2.
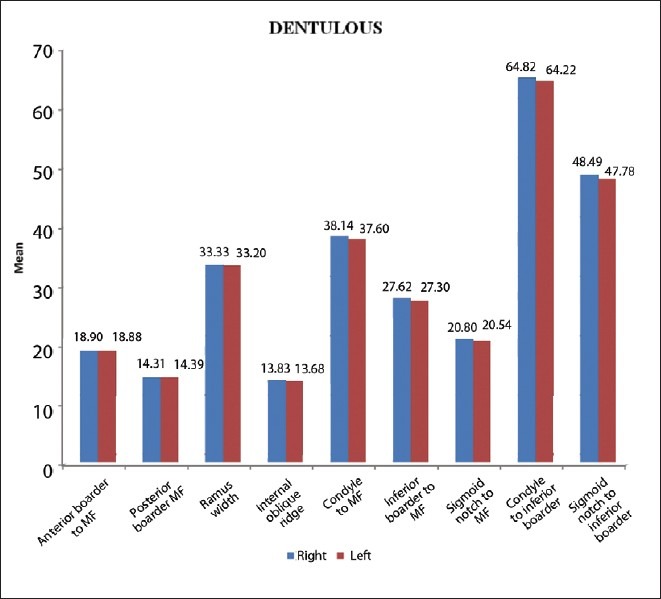
MF distance from various landmarks in dentulous mandible
DISCUSSION
The knowledge of the position of the MF is of a great importance for many procedures in dentistry. Its precise location enables a more effective anesthesia, which in turn leads to an easier patient conditioning.[8–10] The importance of knowledge of the position of MF in the inferior alveolar nerve block was mentioned in several studies which were mentioned in the introduction part of this text.
This study clearly shows that the MF is situated at or below the occlusal surface of lower teeth and at a mean distance of 19 mm (SD 2.34 mm) from AB; and without significant difference between the right and the left side (bilateral symmetry) [Table 1]; the MF was situated at a distance of 2.75 mm posteriorly from the midpoint of anteroposterior width of ramus and 3 mm superiorly from the midpoint of vertical height (between sigmoid notch to inferior border). The above findings are more or less similar to the studies carried out by Heston et al., Williams et al., Hayward et al., and Mbajiorgu, but differed from Nicholson's study. Heston et al. stated that the MF was located immediately posterior to the center of the ramus.[11] According to Williams et al.'s study, the MF was located above the center of the ramus on the medial surface.[12]
Hayward in their study stated that the mean size of the anterior dimension was greater than the mean size of the posterior dimension of the ramus in all instances; the MF was found to be located in the third quadrant anteroposteriorly; there was no right- or left-side dominance in the ramus size and position of the MF.[13]
A study by Mbajiorgu showed that the position of the MF was highly individualistic but on average lies at about 2.56 mm (right) and 2.0 (left) behind the midpoint of ramus width.[14]
According to Nicholson's study, the MF was predominantly located at the center of the mandibular ramus,[4] which differed from our study.
Therefore, in the IANB technique, insertion of a needle 10 mm above the occlusal plane (posterior to anterior border in the medial side of ramus) and deposition of anesthetic solution at a distance of 19 mm from the anterior border should anesthetize the inferior alveolar nerve. When a patient opens the mouth, the IAN may move few mms posteriorly. Therefore, 19 plus 4 mm (23 mm) distance of needle insertion inside the tissues from the anterior border of ramus would take the needle tip nearer to the inferior alveolar nerve.
The above findings help in the success of anesthesia of the IAN block. When a dentist is aware of the location of MF from the anterior border of ramus, he/she could be sure of his/her depth of insertion to reach the nerve. The knowledge of the position of MF in relation to the occlusal plane of mandibular teeth helps the dentist to select the site of needle insertion in the vertical plane.
Nicholson's study stated that the positions of the foramen were found to be variable; and concluded that the marked variability in the position of the MF may be responsible for an occasional failure to block the inferior alveolar nerve.[4] This study found that the variability was not significant enough to produce anesthesia failure.
Lavanya et al. found that the average distance of MF from the mandibular notch was found to be around 20–25 mm in both dentulous and edentulous mandibles. The same was found to be around 16 mm from the anterior border of ramus and around 13 mm from the posterior border of ramus in both groups of mandibles. In dentulous mandibles, the average distance from the third molar tooth was found to be around 15–17 mm.[15] The author would have taken the measurement from the anterior border of MF where as our study had taken the midpoint of MF for measurement and record.
Dr. K. Narayana et al's study confirmed the bilateral symmetry of the MF by assessing human dry mandibles; in our study also, there was no significant difference between the right and left side. He further stated the MF was located above the center of the ramus on the medial surface. He further stated, “In children aged 3 years, the MF has been located 4.12 mm below the occlusal plane; in 9-year-old children it has reached the occlusal plane; in adults it is 4.16 mm above the occlusal plane”.[1] We did not study the mandibles age wise, but generally, the MF was below or at the level of occlusal plane of mandible teeth, not at above the occlusal plane as author quoted.
In 2011 Ashkenazi et al. studied the effect of age on the anteroposterior (A–P) position of the MF and on the size of the gonial angle (GA). According to their study, the anterior movement of the MF and the decreased size of the GA that occurred with changing age and dentition were related to growth process. The MF moves anteriorly, and the GA decreases with age.[16] Our study data could not identify this finding.
The knowledge of location of MF from the anterior border and the occlusal plane helps the dental surgeons to locate the inferior alveolar nerve entry into its foramen correctly in neurectomy surgeries and nerve block techniques. Damage to the inferior alveolar nerve can be avoided in horizontal, vertical, and oblique osteotomies in the ramus. The knowledge of distance of MF to the internal oblique ridge would be helpful in innovation of a new inferior alveolar nerve block technique using the internal oblique ridge as the main landmark.
The knowledge of distance of MF from the posterior border of ramus and the inferior border of mandible and condyle would be helpful in the innovation of new extra oral inferior alveolar nerve block techniques. It is also helpful to study of dental X-rays.
From our study, the position of foramen seems to be determined by size, width, and height of mandible. However, this did not change the position MF to occlusal plane of mandible teeth relation. Most of the studies had taken sigmoid notch as one of the main reference points to quote MF at the centre of ramus. To make a success of IANB it is essential to find the distance of MF from the anterior border and posterior border of ramus. It is also essential to find the MF position in vertical plane superior-inferiorly from the condyle to inferior border to make extra oral blocks effective. Since the sigmoid notch is difficult to feel externally, this study did not include the sigmoid notch as one of the main landmarks.
CONCLUSION
Although it is being mentioned in the literature, the anatomical variation is the cause for failure of anesthesia but this study found the foramen was always at the level of the occlusal plane or below the occlusal plane. Therefore, deposition of anesthetic solution above the foramen level should anesthetize the nerve. It was found in this study that the MF was positioned at a mean distance of 19 mm (with SD 2.34 mm) from the coronoid notch of anterior border of ramus. The variability of distance from AB to MF was also not significant enough to produce failure of anesthesia. Deposition of solution around 23 mm (mean 19 + 4 mm for posterior movement of nerve on the open position of mandible) distance from the anterior border of ramus should anesthetize the inferior alveolar nerve in larger mandibles. Deposition of solution around 20.5 mm (mean 16.5 +4 mm for posterior movement of nerve on the open position of mandible) distance from the anterior border of ramus should anesthetize the inferior alveolar nerve in smaller mandible. Therefore, we conclude the inferior alveolar nerve anesthesia failures are due to the operator error and not due to the anatomical variation. Therefore, the above said knowledge would be helpful for a dentist to introduce new technical modification to create more successful anesthesia and to perform good surgeries in the ramus of mandible.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Narayana K, Soubhagya RN, Prashanthi N, Latha VP. The location of the mandibular foramen maintains absolute bilateral symmetry in mandibles of different age groups. Hong Kong Dent J. 2005;2:35–7. [Google Scholar]
- 2.Ono E, Medici FE, Moraes LC, Castilho JC, Moraes ME. Anteroposterior location of the mandibular foramen of 7 to 12 yearold children in panoramic radiographs. Braz Dent J. 2005;8:6–12. [Google Scholar]
- 3.Ennes JP, Medeiros RM, Grant JC. Localization of Mandibular Foramen and Clinical Implications. Int J Morphol. 2009;27:1305–11. [Google Scholar]
- 4.Nicholson ML. A study of the position of the mandibular foramen in adult human mandible. Anat Rec. 1985;212:110–2. doi: 10.1002/ar.1092120116. [DOI] [PubMed] [Google Scholar]
- 5.Simon B, Komives O. Dimensional and positional variations of the ramus of the mandible. J Dent Res. 1938;17:125–49. [Google Scholar]
- 6.Barker BC, Davies PL. The applied anatomy of the pterygomandibular space. Br J Oral Surg. 1972;10:43–55. doi: 10.1016/s0007-117x(72)80008-8. [DOI] [PubMed] [Google Scholar]
- 7.Quinn JH. Inferior alveolar nerve block using the internal oblique ridge. J Am Dent Assoc. 1998;129:1147–8. doi: 10.14219/jada.archive.1998.0392. [DOI] [PubMed] [Google Scholar]
- 8.Bremer G. Measurements of special significance in connection with anesthesia of the inferior alveolar nerve. Oral Surg Oral Med Oral Pathol. 1952;5:966–88. doi: 10.1016/0030-4220(52)90050-9. [DOI] [PubMed] [Google Scholar]
- 9.Groover OS, Lorton L. Bifid mandibular nerve as a possible cause of inadequate anesthesia in the mandible. J Oral Maxillofac Surg. 1983;41:177–9. doi: 10.1016/0278-2391(83)90076-9. [DOI] [PubMed] [Google Scholar]
- 10.Heasman PA. Variation in the position of the inferior dental canal and its significance to restorative dentistry. J Dent. 1987;16:36–9. doi: 10.1016/0300-5712(88)90102-9. [DOI] [PubMed] [Google Scholar]
- 11.Hetson G, Share J, Frommer J, Kronman JH. Statistical evaluation of the position of the mandibular foramen. Oral Surg Oral Med Oral Pathol. 1988;65:32–4. doi: 10.1016/0030-4220(88)90187-9. [DOI] [PubMed] [Google Scholar]
- 12.Soames RW. Skeletal system. In: Williams PL, Bannister LH, Berry MM, editors. Gray's anatomy. New York: Churchill Livingstone; 1995. pp. 576–9. [Google Scholar]
- 13.Hayward J, Richardson ER, Malhotra SK. The mandibular foramen: Its anteroposterior position. Oral Surg Oral Med Oral Pathol. 1977;44:837–43. doi: 10.1016/0030-4220(77)90027-5. [DOI] [PubMed] [Google Scholar]
- 14.Mbajiorgu EF. A study of the position of the mandibular foramen in adult black Zimbabwean mandibles. Centr Afr J Med. 2000;46:184–90. doi: 10.4314/cajm.v46i7.8554. [DOI] [PubMed] [Google Scholar]
- 15.Lavanya CV, Imtiazul H, Rajeshwari T. Position of Mandibular Foramen in South Indian Mandibles. Anatomica Karnataka. 2011;5:53–6. [Google Scholar]
- 16.Ashkenazi M, Taubman L, Gavish A. Age-associated changes of the mandibular foramen position in anteroposterior dimension and of the mandibular angle in dry human mandibles. Anat Rec. 2011;294:1319–25. doi: 10.1002/ar.21429. [DOI] [PubMed] [Google Scholar]


