Abstract
Vascular anomalies constitute some of the most difficult diagnostic and therapeutic enigmas in the head and neck region. It is of paramount importance that a modern classification system is established to differentiate vascular lesions from vascular malformations. Vascular malformations are usually congenital and venous anomalies usually expand because of hormonal changes such as puberty, pregnancy, or secondary to trauma. Here, we report a case which was diagnosed as low flow vascular malformation of buccal mucosa involving the lower lip and subsequently treated with 3% sodium tetra decyl sulfate. This paper provides overall understanding regarding the presentation and management of small vascular lesions in the orofacial region. Percutaneous sodium tetradecyl sulfate when used either alone or as adjunct to surgery is a safe, effective, and inexpensive agent in the treatment of venous malformations. However, proper case selection, evaluation, and careful planning are necessary to reduce the unwarranted risks and complications.
Keywords: Intralesional sclerotherapy, low-flow vascular malformation, vascular lesions, 3% sodium tetradecyl
INTRODUCTION
The vascular lesions of the skin are divided into congenital and acquired lesions. Acquired and congenital vascular lesions are described as follows:
Acquired vascular lesions
The most significant acquired vascular lesions of infancy are hemangiomas.[1] The lesions are composed of proliferating blood vessels and, although benign, have a potentially destructive character. Hemangiomas undergo a proliferative and an involution stage. Pyogenic granuloma is another acquired vascular lesion that is frequently observed during childhood. It is of minor esthetic significance compared to hemangiomas.[2] After infancy, acquired vascular lesions are associated with aging (senile angiomas), trauma (arteriovenous fistulas), systemic conditions (spider angioma), and malignancy (Kaposi's sarcoma).
Congenital vascular lesions
The most common congenital vascular lesions are vascular malformations. Vascular malformations are the outcome of errors in vascular formation during embryonic life. They do not proliferate. The dilated blood vessels that build up these lesions gradually enlarge. Vascular malformations can be classified based on their type of blood flow into slow-flow lesions (capillary, venous, and lymphatic), high-flow lesions (arterial), and lesions with a combined slow and fast blood flow.
CASE REPORT
A 42-year-old female patient came to the Department of Oral and Maxillofacial Surgery as an outpatient with a chief complaint of swelling in the left side of the lower lip. The patient gives a history of small negligible swelling present since 5 years and gradually increased in size due to repeated trauma during mastication with a short span of bleeding when exposed to trauma and subsequent arrest of bleeding by itself. Her blood report was within normal limits. Local examination revealed a single, oval, well-defined, nonpulsating, soft and compressible swelling roughly measuring 1.6 × 1.5 × 0.8 cm3 [Figure 1] involving buccal mucosa in the left side of the lower lip. Color of the lesion was bluish red with erythematous areas on the surface. On careful inspection, a fine capillary network of blood vessels seen in the mucosa mimicking a vascular lesion. The diascopy test was positive with escape of coloration upon compressibility resulting in blanching of the lesion when placing a microscope glass slide under pressure which gave us the impression of vascular lesion.
Figure 1.

Preoperative appearance of the lesion
For confirmatory diagnosis, the lesion was subjected to a Duplex Ultrasound Color Doppler study followed by magnetic resonance imaging (MRI) and magnetic resonance venography (MRV) scans. An ultrasound color Doppler scan reported with heterogeneously hypo echoic with multiple tiny cystic areas and mild internal vascularity within the lesion [Figure 2], while the MRI scan reported a homogenously hyperintense in T2W and STIR sequences and hypointense in T1W sequences [Figure 3]. On a postcontrast study, MRV, homogenous enhancement of the lesion was seen with no evidence of prominent vessel around the lesion and was diagnosed as slow-flow vascular malformation of the buccal mucosa involving the lower lip [Figure 4].
Figure 2.
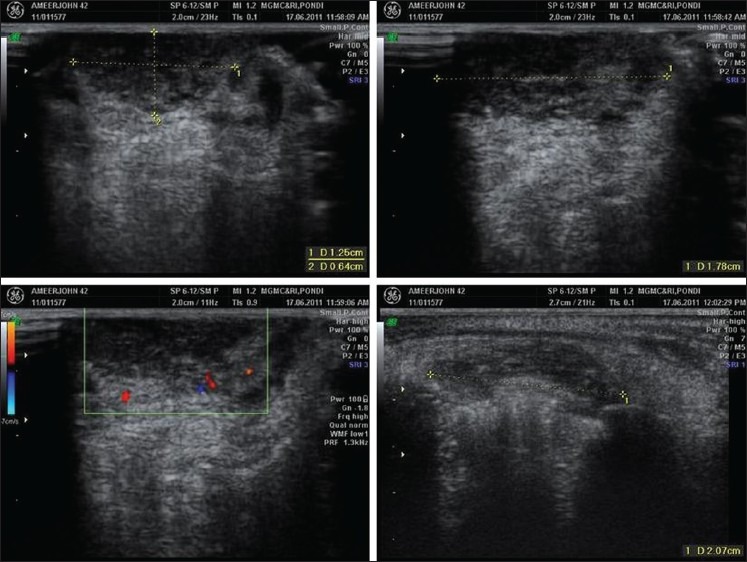
Ultrasound color Doppler study showing hypo echoic with multiple tiny cystic areas and mild internal vascularity within the lesion
Figure 3.
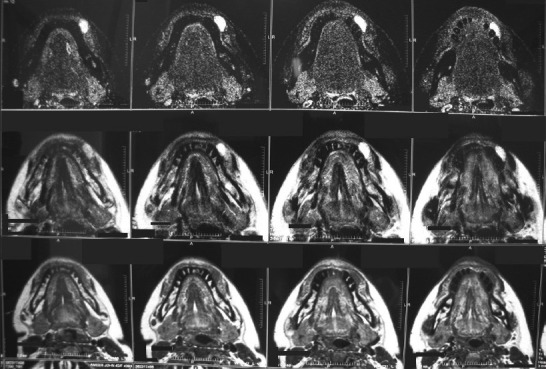
MRI scan showing a homogenously hyperintense in T2W and STIR sequences and hypointense in T1W sequences
Figure 4.
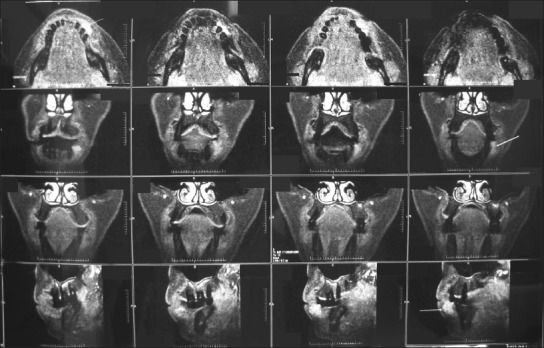
MRV demonstrating a homogenous enhancement of the lesion with no evidence of prominent vessels around the lesion
The patient was planned for conservative treatment by sclerotherapy with 3% sodium tetra decyl sulfate (STS). A test dose was given and found no signs of hypersensitivity. The area to be injected was cleansed and local infiltration (2% lignocaine with 1:2,00,000 adrenaline) was administered at the base and periphery of the lesion. STS was injected directly into the lesion through the mucosa at multiple sites without any radiological guidelines. In total, 1.5 ml of STS was injected. After withdrawal of the needle, manual compression for 10–15 min was done over the lesion with a sterile gauze. The patient was advised to take anti-inflammatory and analgesics and recalled after 15 days. In the second visit, the patient was reviewed with complete resolution of the lesion [Figure 5]. In our case, the patient experienced transient severe pain postoperatively with minor complications such as local inflammatory response including cutaneous blistering which gradually reduced. The patient was reviewed after 15 days and bimonthly interval, found the complete absence of the lesion and no evidence of recurrence.
Figure 5.

Postoperative appearance after 15 days showing complete resolution of the lesion
DISCUSSION
The diagnosis of vascular malformations is based on the patient's medical history and a physical examination.[1] Vascular low flow lesions may present a progressive increase with age, trauma, and after partial resection. Ectatic blood vessels and the reddish-blue surface are characteristically found in this lesion. Change on pressure is a common finding with return to original color on withdrawal of pressure. We believe that our case corresponds to vascular low flow malformation due to their reddish-purple aspect, consistence, response to diascopy, and the absence of vascular pulsation.[3]
The appropriate combination of noninvasive to minimally invasive tests should follow in order to confirm or exclude the clinical impression.[4] Duplex ultrasound scanning is the first choice for noninvasive evaluation of patients with vascular malformations, doppler mode to assess flow characteristics.[5] Minimally invasive tests such as MRI[6] and MRV[7] are useful to confirm the extent and type of venous malformations, delineates feeding and draining vessels, distinguishes between different soft tissues (muscle, fat) and the vascular structures.
Sclerotherapy, the mainstay of treatment is the injection of an agent to induce inflammation and obliteration of affected veins. For small cutaneous or mucosal lesions, local injection may be effective. Intralesional sclerotherapy using liquid sclerosing agents, which is a palliative treatment in most types of vascular anomalies, produces good outcomes in smaller lesions.[8] Sclerosants can also be classified as[9]
Detergents—Disrupt vein cellular membrane (protein theft denaturation)
Sodium tetradecyl sulfate
Polidocanol
Sodium morrhuate
Ethanolamine oleate
Osmotic agents—Damage the cell by shifting the water balance through cellular gradient (osmotic) dehydration and cell membrane denaturation
Hypertonic sodium chloride solution
Sodium chloride solution with dextrose
Chemical irritants—Damage the cell wall by direct caustic destruction of endothelium
Chromated glycerin
Polyiodinated iodine
STS at low concentrations are effective in stripping endothelium over a considerable distance, and is also able to induce a hypercoagulable state, possibly by selective inhibition of protein C, and can also promote platelet aggregation. We selected 3% STS as a sclerosing agent because of its high effectiveness and minor complications like the presence of small skin ulcers and superficial skin breakdown which responded well to the application of silver sulfadiazine.[10] Intralesional sclerotherapy can be performed without serious complications if the sclerosing agent is selected and injected cautiously.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412–22. doi: 10.1097/00006534-198203000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): A clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267–76. doi: 10.1111/j.1525-1470.1991.tb00931.x. [DOI] [PubMed] [Google Scholar]
- 3.Redondo P. Classification of vascular anomalies (tumours and malformations). Clinical characteristics and natural history. An Sist Sanit Navar. 2004;27(Suppl 1):9–25. [PubMed] [Google Scholar]
- 4.Lee BB, Mattassi R, Choe YH, Vaghi M, Ahn JM, Kim Di, et al. Critical role of Duplex ultrasonography for the advanced management of a venous malformation. Phlebology. 2005;20:28–37. [Google Scholar]
- 5.Timmerman D, Wauters J, Van Calenbergh S, Van Schoubroeck, Maleux G, Van Den Bosch T, et al. Color doppler imaging is a valuable tool for the diagnosis and management of uterine vascular malformations. Ultrasound Obstet Gynecol. 2003;21:570–7. doi: 10.1002/uog.159. [DOI] [PubMed] [Google Scholar]
- 6.Smith JK, Castillo M, Wilson JD. MR characteristics of low flow facial vascular malformations in children and young adults. Clin Imaging. 1995;19:109–17. doi: 10.1016/0899-7071(94)00031-7. [DOI] [PubMed] [Google Scholar]
- 7.Yonetsu K, Nakayama E, Miwa K, Tanaka T, Araki K, Kanda S, et al. Magnetic resonance imaging of oral and maxillofacial angiomas. Oral Surg Oral Med Oral Pathol. 1993;76:783–9. doi: 10.1016/0030-4220(93)90052-6. [DOI] [PubMed] [Google Scholar]
- 8.Goldman MP, Bennet RG. Treatment of telangiectasia: A review. J Am Acad Dermatol. 1987;17(2 Pt 1):167–82. doi: 10.1016/s0190-9622(87)70187-x. [DOI] [PubMed] [Google Scholar]
- 9.Parsons ME. Sclerotherapy basics. Dermatol Clin. 2004;22:501–8. doi: 10.1016/j.det.2004.03.017. xi. [DOI] [PubMed] [Google Scholar]
- 10.Gomes AS. Embolization therapy of congenital arteriovenous malformations: Use of alternate approaches. Radiology. 1994;190:191–8. doi: 10.1148/radiology.190.1.8259403. [DOI] [PubMed] [Google Scholar]


