Abstract
Polycystic Ovary Syndrome (PCOS) is a leading cause of infertility. We studied the rheological properties of cervical-vaginal secretions in five PCOS patients during variable treatment intervals with metformin. Five ovulatory normal women for a total of thirteen cycles served as control patients. All subjects collected daily cervical-vaginal fluid(CVF) samples with an aspirator, and CVF samples were characterized by a flow metric, die swell ratio (B), which measured CVF elasticity. Ovulatory cycles were indexed to the day of positive urine or serum LH (luteinizing hormone). CVF B levels from ovulatory normal women had a characteristic concave parabolic pattern of a minimum near the day of ovulation with higher values outside the periovulatory phase. In contrast, the five PCOS patients with or without metformin treatment had no periodicity of CVF B, and their CVF B levels were typically less compared to those in the early preovulatory and luteal phases of normal patients.
Keywords: Cervical--vaginal fluid, infertility, PCOS, rheology
INTRODUCTION
Polycystic Ovary syndrome is a common condition in women frequently leading to anovulatory cycles and reduced fertility and is associated with insulin resistance and type 2 diabetes.[1] In the treatment of anovulatory PCOS patients with or without type 2 diabetes (PCOS±DM), metformin is a safe ovulation induction agent; however, induction of ovulation does restore fertility as one might predict.[2]
One potential factor in PCOS infertility is the level of secretion and/or structure of the polymeric hydrogel, cervical mucus, which is critical for sperm transport and conception.[3,4] Cervical mucus is extruded through the cervical os and combines with vaginal transudate, cells and flora to form cervical-vaginal fluid (CVF), a derivative secretion.[5,6] CVF is viscoelastic, and the material property, elasticity, undergoes a periodic change during the normal ovulatory menstrual cycle[7] : higher elasticity in the preovulatory and luteal phases and reduced elasticity in the immediate, fertile time preceding ovulation - a concave parabolic signature. The level of elasticity of polymeric solutions can be quantitated by die swell analysis,[7] in which CVF is extruded through a die or capillary and the level of fluid expansion or swell measured as a die swell ratio, B, where B = (diameter of maximum fluid swell/inner diameter of die).
We investigated the hypothesis that the elasticity of CVF from PCOS±DM women is abnormal, and found in five PCOS±DM women, with or without metformin treatment (±M), the elasticity of their cervical vaginal secretions is reduced and lacks periodicity.
CLINICAL CASE
The normal and PCOS±DM patients (ages 19 – 41) were not using any hormonal or IUD contraceptive and had no vaginitis. Five ovulatory normal (non-diabetic, non-PCOS) women served as controls and provided a total of thirteen ovulatory cycles. The PCOS±DM patients had two essential biochemical and clinical features: Anovulation and clinical hyperandrogenism (hirsutism).[1] Two PCOS women (PT3 and PT6) and three PCOS+DM women (PT5, PT9 and PT12) were studied during anovulatory intervals; ovulation was induced with metformin(+M) in PT3 and PT6. PT6 and PT5 were studied before and after metformin treatment(±M), PT3 and PT9 were already under treatment with metformin, and PT12 received no metformin. The lengths of metformin treatment for the PCOS±DM patients at the time of the CVF collections were: PT3=12 months, PT6=4.5 months, PT5=4.5 months, PT9=12months, PT12=0 months.
A vaginal aspirator (Rovumeter™) was used by the patients to self-collect daily samples of CVF as previously published.[7,8] The five PCOS±DM patients aspirated during anovulatory intervals and collected CVF every day to every other day depending upon the level of vaginal dryness. CVF samples were collected in vials and analyzed by extrusion through a die swell device with measurement of B.[7] Urine LH and serum hormone measurements (LH, estradiol, progesterone, and total testosterone(T) were obtained throughout ovulatory cycles and anovulatory intervals, and ovulatory cycles indexed to the first day of urine LH signal and/or day of serum LH surge (‘Day 0’). Ovulatory cycles were ascertained by serum progesterone > 3 ng/ml and biphasic basal body temperature.
The five ovulatory normal patients showed the periodic signature of CVF B during the menstrual cycle that has been previously published[7] [Figure 1, bottom; Figure 2]: A cyclic concave parabolic pattern. The CVF elasticity during the ovulatory normal cycle was: Initially high B with negative slope, a minimum B one to two days before ovulation, and an increasing postovulatory B after this inflection point. There was a considerable range in the CVF B levels, ~ 0.9 – 2.4, throughout the normal menstrual cycles [Figure 1a].
Figure 1.
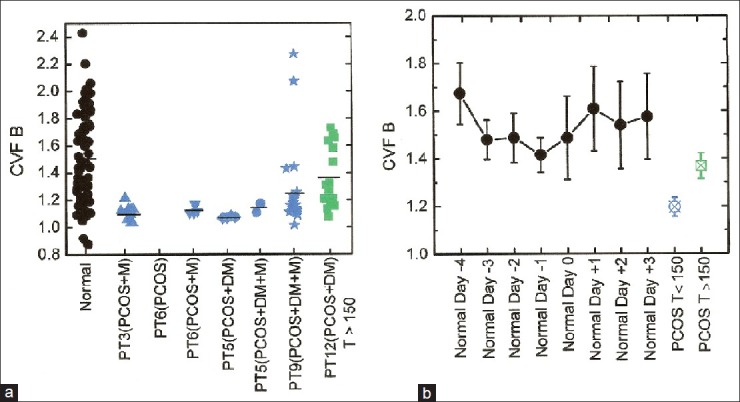
Cervical-vaginal fluid (CVF) elasticity comparison for five ovulatory normal versus five PCOS±DM women: absence of CVF B periodicity and reduced CVF B levels in PCOS. Top: Scatter plot of total CVF die swell ratio (CVF B) values for normal and PCOS±DM women. All normal CVF B values are from ovulatory cycles and include pre-ovulatory, ovulatory, and luteal phase results (thirteen total cycles). PCOS CVF B values are from PCOS patients: PT3, PT6, PT5, PT9, PT12. Patients who underwent treatment with metformin (+M) are indicated. Anovulatory interval PT6(PCOS) did not produce enough CVF for B measurements. Only Cycle PT3(PCOS+M) and Cycle PT6(PCOS+M) were ovulatory after metformin treatment. Bottom: Mean day-specific CVF B values for ovulatory normal women and mean CVF B values for combined intervals/cycles from PCOS±DM women. The PCOS±DM patients are here segregated into two groups, PCOS±DM women PT3, PT5, PT6, PT9 with Testosterone (T) levels < 150 ng/dl (blue) and PCOS+DM woman PT12 with T levels > 150 ng/dl. Mean CVF B values are from 5 normal ovulatory patients, 13 total cycles, 52 total values. PCOS (T<150) mean CVF B is from 53 total values (four total patients), and PCOS (T>150) mean CVF B is from 16 total values (one patient).
Figure 2.
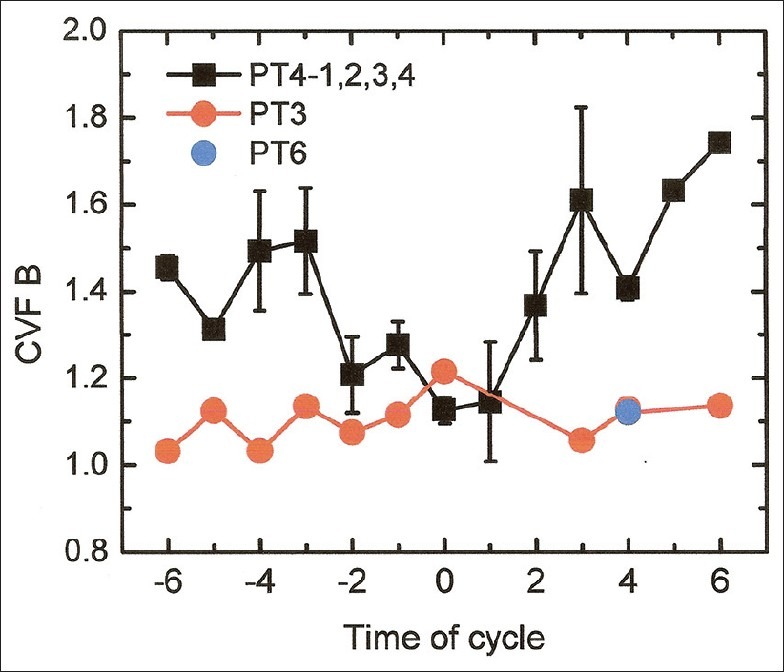
Day-specific cervical-vaginal fluid die swell ratio (CVF B) for two PCOS cycles, in which ovulation was induced with metformin treatment, compared with the mean day-specific CVF B for four ovulatory normal cycles: metformin-induced ovulation did not restore a normal CVF B signature. Results for PCOS patients, PT3 and PT6, and normal patient, PT4 (cycles PT4-1,2,3,4), are shown. Metformin treatment in patients PT3 and PT6 was for 12 months and 4.5 months, respectively. Even with metformin treatment, cycle PT6(PCOS+M) generated scant daily CVF volume (<0.2ml) and consequently die swell ratio measurements were limited (Day +4).
No periodic changes were observed in CVF elasticity in any of the intervals or cycles from the PCOS±DM patients [Figures 1 and 2]. The mean CVF B for patient PT12 with high T levels (>150 ng/dl) was significantly higher than the mean CVF B for the other PCOS patients, PT3, PT5, PT6, and PT9 (Student's t-test, P value <0.05).
The mean day-specific CVF B levels for the ovulatory normal cycles, which ranged from a minimum value of 1.41±0.06(SE) on Day -1 to a maximum value of 1.68±0.13(SE) on Day -4, were compared to the mean CVF B level for PCOS patients PT3, PT5, PT6 and PT9, 1.17±0.02(SE), and to the mean CVF B level for PCOS patient PT12, 1.36±0.05 [Figure 1b]. The mean day-specific CVF B levels were significantly higher than the mean CVF B levels for patients PT3, PT5, PT6, and PT9 (Student's t-test, P value<0.05); this difference did not reach statistical significance for the mean CVF B for PT12 with high T. Although metformin induced ovulation in the PCOS women, PT3 and PT6, the CVF B signature was not restored and the CVF B levels were < 1.22 [Figure 2].
DISCUSSION
For the five PCOS±DM patients, the PCOS condition was not only associated with reduced elasticity of CVF as characterized by the die swell ratio metric, but also metformin treatment of PCOS was unable to restore normal CVF elasticity and periodicity, even in the two PCOS patients when ovulation was induced.
Abnormal cervical mucus/CVF may be a factor in the infertility of women with PCOS, but there are scant published data. Vigil et al.[9] found the average pore size of cervical mucus fibers to be reduced in PCOS. The case study presented here also suggests abnormalities in structure of cervical-vaginal secretions in PCOS.
The biophysical properties of cervical mucus/cervical-vaginal secretions are critically dependent upon the hydrogel formed with the large glycoprotein MUC5B and its polymeric chains.[4,10] This polymeric structure gives cervical mucus and CVF its rheological properties. The cause of the reduced elasticity of CVF in PCOS, which appeared to exist even with metformin treatment and restoration of ovulation, is unknown. CVF B in PCOS, which was generally ≤ 1.2, probably does not indicate fertile-type cervical mucus/CVF, but rather lack of elastic hydrogel. A Newtonian fluid such as water also has low die swell ratio.[7] In fact, the fertile normal CVF with low B demonstrated spinnbarkeit and a rheological property called delayed die swell[7] that was not observed with PCOS CVF. It can be hypothesized that the low CVF B observed in the PCOS condition is due to reduced MUC5B secretion.
The present investigation of PCOS was limited to five women; larger studies are needed before rheological analysis of cervical-vaginal fluid can be recommended in routine clinical practice.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, et al. Position statement: Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: An androgen excess society guideline. J ClinEndocrinolMetab. 2006;91:4237–45. doi: 10.1210/jc.2006-0178. [DOI] [PubMed] [Google Scholar]
- 2.Legro RS, Barnhart HX, Schlaff WD, Carr BR, Diamond MP, Carson SA, et al. Clomiphene, metformin, or both for infertility in the polycystic ovary syndrome. N Engl J Med. 2007;356:551–66. doi: 10.1056/NEJMoa063971. [DOI] [PubMed] [Google Scholar]
- 3.Saurez SS, Pacey AA. Sperm transport in the female reproductive tract. Hum Reprod Update. 2006;12:23–37. doi: 10.1093/humupd/dmi047. [DOI] [PubMed] [Google Scholar]
- 4.Gipson IK, Moccia R, Spurr-Michaud S, Argueso P, Gargiulo AR, Hill JA, III, et al. The amount of MUC5B mucin in cervical mucus peaks at midcycle. J ClinEndocrinolMetab. 2001;86:594–600. doi: 10.1210/jcem.86.2.7174. [DOI] [PubMed] [Google Scholar]
- 5.Usala SJ, O’Brien-Usala F, Haciski R, Holt JA, Schumacher GF. IgG and IgA content of vaginal fluid during the menstrual cycle. J Reprod Med. 1989;34:292–94. [PubMed] [Google Scholar]
- 6.Lai SK, Wang YY, Hida K, Cone R, Hanes J. Nanoparticles reveal that human cervicovaginal mucus is riddled with pores larger than viruses. PNAS. 2010;107:598–603. doi: 10.1073/pnas.0911748107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang J, Usala SJ, O’Brien-Usala F, Biggs WC, Vaughn MW, McKenna GB. The fertile and infertile phases of the menstrual cycle are signaled by cervical-vaginal fluid die swell functions. The Endocrinologist. 2009;19:291–97. [Google Scholar]
- 8.Flynn AM, Collins WP, Royston P, Barbato M, Mena-Gonzalez P, Alliende ME. Volumetric self-sampling of cervicovaginal fluid to determine potential fertility: A multicenter pre-effectiveness study of the Rovumeter. Hum Reprod. 1997;12:1826–31. doi: 10.1093/humrep/12.8.1826. [DOI] [PubMed] [Google Scholar]
- 9.Vigil P, Cortes ME, Zuniga A, Riquelme J, Ceric F. Scanning electron and light microscopy study of the cervical mucus in women with polycystic ovary syndrome. J Electron Microscopy. 2009;1:21–27. doi: 10.1093/jmicro/dfn032. [DOI] [PubMed] [Google Scholar]
- 10.Keismer M, Makhov AM, Griffith JD, Verdugo P, Sheehan JK. Unpacking a gel-forming mucin: A view of MUC5B organization after granular release. Am J Physiol Lung Cell MolPhysiol. 2010;298:L15–L22. doi: 10.1152/ajplung.00194.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]


