Abstract
Pregnancy in a patient with acromegaly is a rare occurrence. Here in, we report a patient with acromegaly who presented to us in the 2nd trimester of pregnancy with visual loss in the right eye. Her vision improved after surgery. She went on to have an uneventful pregnancy and delivered a term baby, by caesarian section. One year following her delivery, she received stereotactic radiotherapy. Subsequent follow-up revealed that her tumor had regressed and her IGF-1 levels had normalized.
Keywords: Acromegaly, pregnancy, stereotactic radiotherapy, surgery, visual loss
INTRODUCTION
Pregnancy in acromegaly is quite rare. Although various series of such cases have been published over the years in foreign journals, our indigenous case is unique for the following reasons: It describes a lady who went upto late 2nd trimester before undergoing transnasal transsphenoidal resection of pituitary adenoma to restore her vision. Moreover, as she took cabergoline for the entire duration of the gestation with no untoward side effects, we believe this is the first reported case from our country.
CASE REPORT
A 30-year-old lady (Gravida 2 Parity 1 Live Birth 1) whose last child birth was 9 years ago presented to us in the 2nd trimester of pregnancy (August 2007), with progressive decrease in vision in the right eye for 6 weeks. She also complained of coarsening of facial features and enlargement of hands and feet for 3 years. She had mild intermittent headache.
Clinical examination revealed acromegalic features. Her blood pressure was normal. The fundal height corresponded with the period of gestation (18 weeks). Central nervous system examination revealed right temporal field defect with temporal pallor of the right optic disc. Examination of the left eye was normal. Rest of the systemic examination was normal.
Her blood sugars were normal. Hormonal profile revealed elevated human growth hormone (HGH) 37.9 ng/dl and insulin-like growth factor 1 (IGF-1) 424 ng/ml (normal 117-329 ng/ml), her serum prolactin was also mildly elevated, i.e. 107 ng/ml. Magnetic resonance imaging of the brain revealed a 34 × 23 × 20 mm sellar, suprasellar mass abutting the third ventricle [Figure 1]. Ultrasound of the abdomen revealed a single live fetus, corresponding to the period of gestation.
Figure 1.
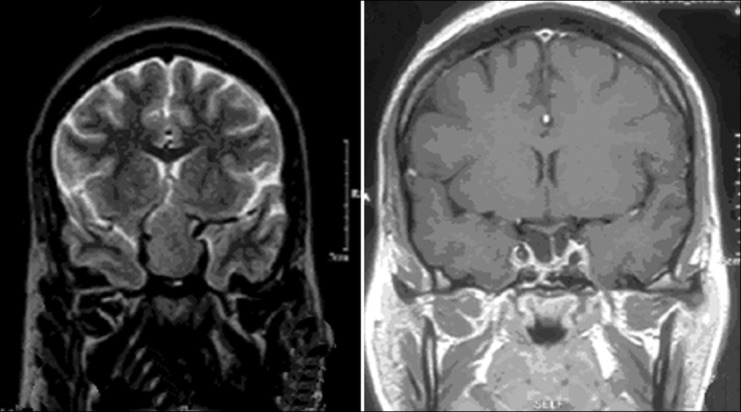
MRI pictures of pituitary tumor-sagittal view-Left-before surgery, Right-after surgery
We discussed the treatment options and the risks involved with the patient and her family. She agreed for surgery.
She underwent endoscopic transnasal transsphenoidal radical excision of the tumor in the 22nd week of pregnancy.The postoperative period was uneventful. Biopsy revealed sparsely granulated GH secreting tumor (MIB-1 index 2%). (MIB-1 stands for MIndBobmb homolog-1: A commonly used monoclonal antibody that detects the Ki-67 antigen which is a cellular marker for proliferation [name derived from city of origin-Kiel, Germany and the number of the original clone in the 96-well plate]. Ki-67 is an excellent marker to determine the growth fraction of a given cell population. The fraction of Ki-67-positive tumor cells (the Ki-67 labeling index) is often correlated with the clinical course of cancer. MIB-1 index is used in clinical applications to determine this index. One of its primary advantages over the original Ki-67 antibody (and the reason why it has essentially supplanted the original antibody for clinical use) is that it can be used on formalin-fixed paraffin-embedded sections, after heat-mediated antigen retrieval).
Following surgery, her right-eye vision improved. Her HGH however, continued to be elevated, 4.37 ng/dl on the 1st post-op day and 5.58 ng/dl on the 7th post-day. As she could not afford Inj. Octreotide, she was started on tab. cabergoline 0.5 mg twice-a-week. She continued this drug throughout the pregnancy without any untoward side effects.
She then went on to deliver a full-term baby boy by caesarian section in January 2008 (birth weight- 3.14 kg).Following delivery, she was unable to breast feed the child, however, she resumed having her normal periods.
She came for her 1st follow-up visit in February 2009. At this stage, she was found to have elevated HGH levels [Table 1]. The MRI scan also showed residual tumor. She received stereotactic radiotherapy one year after the delivery.
Table 1.
Serial investigations of patient
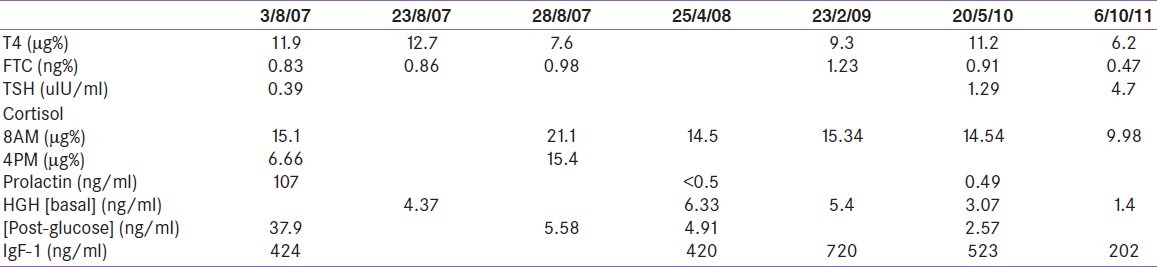
She was last seen in October 2011. Her acromegalic features had regressed, IGF-1 levels had normalized [Table 1] and there was no tumor detected in the MRI scan [Figure 1].
DISCUSSION
Pregnancy in a patient with acromegaly is very unusual, as the enlarging pituitary adenoma suppresses gonadotropin secretion rendering the patient amenorrheic and infertile. Up to 30% of HGH-secreting pituitary adenomas also secrete prolactin and this adds to the problem. Pituitary stalk compression by the adenoma will also elevate prolactin levels.[1] Our patient is unusual, in that she conceived spontaneously while having active disease.
Although pregnancy is unusual in acromegaly, it is by no means rare. Twenty-four patients with acromegaly and pregnancy were reported by Cozzi, et al.,[2] in the same year, Caron, et al.[3] also reported 59 pregnancies in 43 women with acromegaly. More recently, Cheng, et al.[4] have reported a much larger series of patients.
Pregnancy by itself causes physiological enlargement of the normal pituitary gland. This effect is more marked in a patient with a pituitary macro adenoma and this leads to headache, visual symptoms, and field defects.[5]
Normal pregnancy and pregnancy in a patient with acromegaly have markedly different effects on growth hormone (GH) physiology. In normal women, during the 1st trimester, pituitary growth hormone (HGH) is the only measurable GH in maternal serum. After the 1st trimester, placental growth hormone (GH-V) contributes the major portion of circulating GH. GH-V in turn stimulates 1GF-1 production, and this will inhibit maternal HGH production. HGH secretion is pulsatile vs. GH-V secretion which is non-pulsatile.[6] In contrast, patients with acromegaly have persistent unregulated secretion of HGH throughout pregnancy. Beckers, et al.[6] showed that patients with acromegaly demonstrate a paradoxical rise of HGH with thyrotropin releasing hormone. GH-V is resistant to stimulation by GH secretagogues.
The Immulite 2000 assay (manufactured by the Siemens Health Care Diagnostics based at Tanyton, New York State, USA used with International Standard IS 98/574) used in our laboratory was unable to distinguish between HGH and GH-V in our patient.
HGH does not cross the placenta, and acromegaly in the mother has no direct bearing on the fetus and its development.
Since pregnancy itself is an insulin resistant state, elevated GH can cause impaired glucose tolerance and frank diabetes. There is also an increased incidence of hypertension and coronary artery disease in patients with acromegaly. Our patient's glycemic control and blood pressure recordings were normal and she did not require any additional treatment.
In earlier studies, the median time for surgery was in the 19th week of pregnancy,[5] our patient underwent surgery in 22nd week of pregnancy.
Earlier series used bromocriptine during pregnancy,[7] our patient received cabergoline without any untoward side effects during pregnancy.
More recently there are reports of pegvisomant being used in pregnancy.[8,9]
We report this case because of:
The rarity of spontaneous conception in a patient with untreated active acromegaly.
Successful transnasal transsphenoidal surgery during the 2nd trimester of pregnancy with no danger to the fetus or the mother.
The use of cabergoline in the treatment of acromegaly during pregnancy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Melmed S, Klienberg D. Williams Textbook of Endocrinology. 11th ed. Maryland Heights Missouri USA: W.B. Saunders AnImprint of Elsevier; 2008. Anterior pituitary. [Google Scholar]
- 2.Cozzi R, Attanasio R, Barausse M. Pregnancy in acromegaly: A one-center experience. Eur J Endocrinol. 2006;155:279–84. doi: 10.1530/eje.1.02215. [DOI] [PubMed] [Google Scholar]
- 3.Caron P, Bertherat J, Périère B, Brue T, Cortet RC, Schillo F, et al. Outcome of 59 pregnancies in 43 acromegalic women. Endocrine Abstr. 2006;11:649. [Google Scholar]
- 4.Cheng S, Grasso L, Martinez-Orozco JA, Al-Agha R, Pivonello R, Colao A, et al. Pregnancy in acromegaly: Experience from two referral centers and systematic review of the literature. Clin Endocrinol (Oxf) 2012;76:264–71. doi: 10.1111/j.1365-2265.2011.04180.x. [DOI] [PubMed] [Google Scholar]
- 5.Magyar DM, Marshall JR. Pituitary tumors and pregnancy. Am J Obstet Gynecol. 1978;132:739–51. doi: 10.1016/s0002-9378(78)80008-8. [DOI] [PubMed] [Google Scholar]
- 6.Beckers A, Stevenaert A, Foidart JM, Hennen G, Frankenne F. Placental and pituitary growth hormone secretion during pregnancy in acromegalic women. J Clin Endocrinol Metab. 1990;71:725–31. doi: 10.1210/jcem-71-3-725. [DOI] [PubMed] [Google Scholar]
- 7.Yap AS, Clouston WM, Mortimer RH, Drake RF. Acromegaly first diagnosed in pregnancy: The role of bromocriptine therapy. Am J Obstet Gynecol. 1990;163:477–8. doi: 10.1016/0002-9378(90)91178-f. [DOI] [PubMed] [Google Scholar]
- 8.Brian SR, Bidlingmaier M, Wajnrajch MP, Weinzimer SA, Inzucchi SE. Treatment of acromegaly with pegvisomant during pregnancy: Maternal and fetal effects. J Clin Endocrinol Metab. 2007;92:3374–7. doi: 10.1210/jc.2007-0997. [DOI] [PubMed] [Google Scholar]
- 9.Qureshi A, Kalu E, Ramanathan G, Bano G, Croucher C, Panahloo A. IVF/ICSI in a woman with active acromegaly: Successful outcome following treatment with pegvisomant. J Assist Reprod Genet. 2006;23:439–42. doi: 10.1007/s10815-006-9077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


