Sir,
Polycystic pancreas is a rare condition usually found incidentally at surgery orautopsy. It is often asymptomatic, or presents with vague abdominal pain. Polycystic disease is usually associated with renal, hepatic, cerebellar, and retinal anomalies. Here we present the case of a 24-yr-old man who was found incidentally to have an isolated polycystic pancreas during evaluation of patient. The evaluation comprise of ultrasonography and color flow imaging followed by MR evaluation. This obviated use of computed tomography in the work up of this patient.
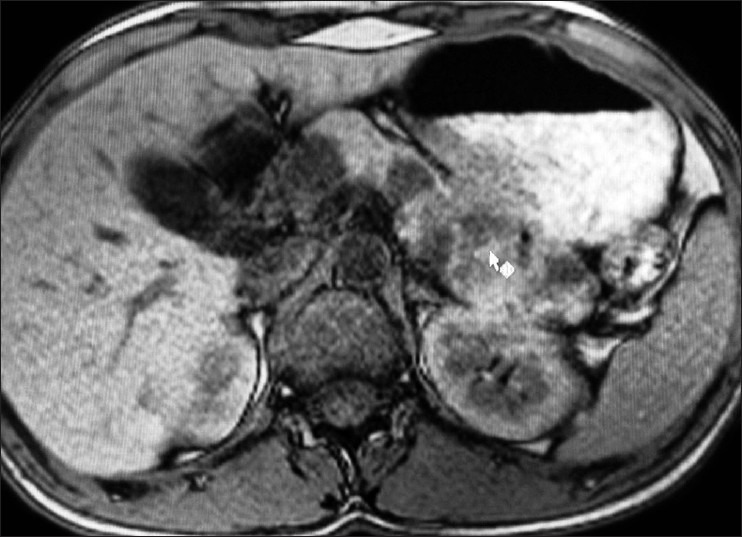
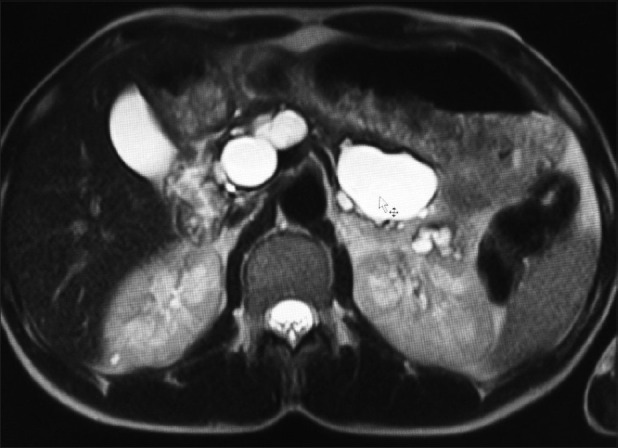
A 24 year old male patient presented with history of vague recurrent abdominal pain since four months. Physical and systemic examination was unremarkable. Bowel sounds were normal, and no tenderness, guarding, ascites, hepatosplenomegaly or lump was appreciated. Rectal examination was normal. Bio chemical examination was normal. Ultrasonography revealed multiple hypo echoic cysts diffusely involving the pancreas [Figure 1]. No evidence of calcific foci was noted. Color flow and pulse Doppler confirmed the non vascular nature of the lesion. There was no involvement of liver spleen or kidneys. Rest of the abdomen was unremarkable. The cysts were not very large hence, MR imaging was done to define the anatomical details. MR evaluation [Figures 2–6] showed diffuse involvement of pancreas with multiple cyst of variable size. The cyst was largely uncomplicated with no evidence of hemorrhage or inflammation. No other evidence of involvement of other organ system was noted. Histology revealed cysts lined by cuboidal-to-flat epithelium and contain fluid with both amylase and proteolytic enzyme activity, suggestive of true cysts.
Figure 1.
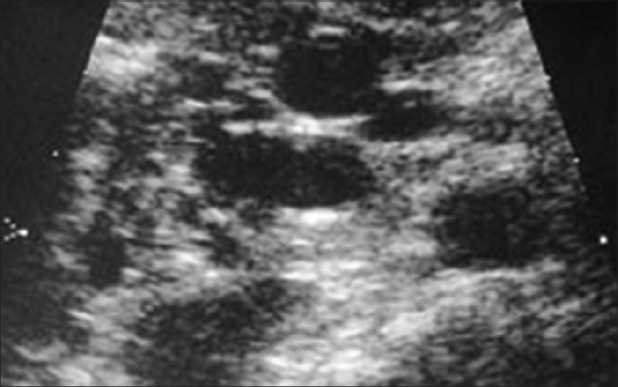
Focused ultrasound of pancreas showing multiple cysts of variable sizes
Figure 2.
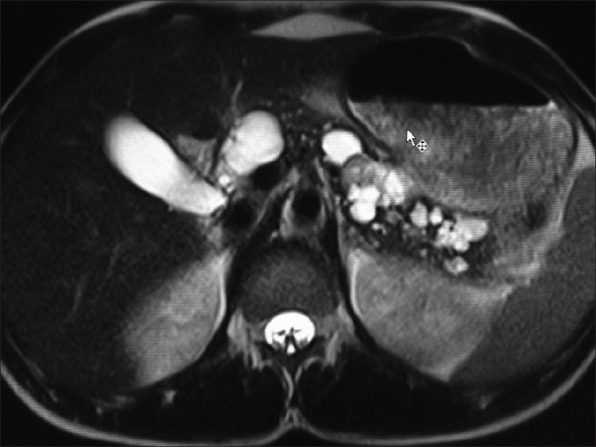
Axial heavily T2 weighted MR imaging of abdomen showing multiple simple cysts of variable sizes diffusely involving pancreas
Figure 6.
A superior section acquired with Axial T1 weighted MR imaging of abdomen showing multiple simple cysts diffusely involving pancreas without similar cysts in liver and kidneys
Figure 3.
Axial heavily T2 weighted MR imaging of abdomen showing multiple simple cysts diffusely involving pancreas without similar cysts in liver and kidneys
Figure 4.
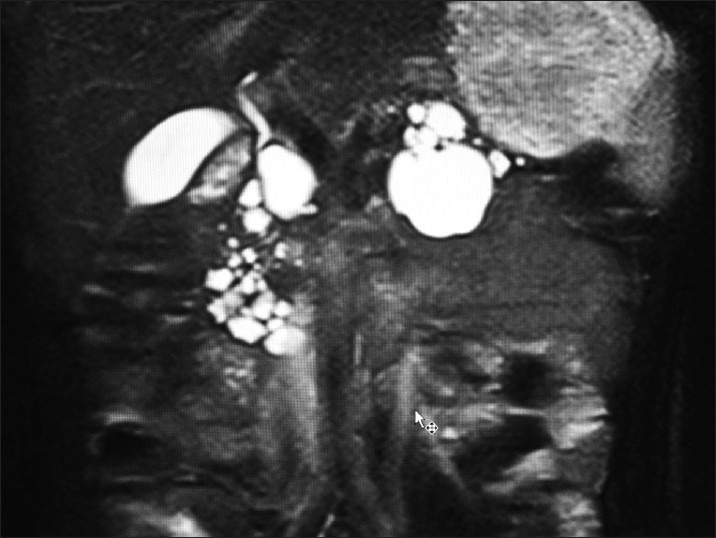
Coronal heavily T2 weighted MR imaging of abdomen showing multiple simple cysts diffusely involving pancreas without similar cysts in liver and kidneys
Figure 5.

Axial T1 weighted MR imaging of abdomen showing multiple simple cysts diffusely involving pancreas without similar cysts in liver and kidneys
Pancreatic cysts are broadly classified as congenital-developmental cysts, retention cysts, duplication cysts, pseudo cysts, neoplastic cysts, and parasitic cysts.[1] It is accepted that true cysts occur as a result of developmental anomalies related to the sequestration of primitive pancreatic ducts. In our case, the presence of multiple cysts diffusely involving pancreas were evaluated as indicators of ductal developmental anomaly. Histology in our case confirmed the same. Congenital pancreatic cysts are generally asymptomatic, although abdominal distention, vomiting, jaundice, or pancreatitis can be observed.[1,2] Localization in the head of the pancreas was reported in 32% of cases.[1] In our case, it was noted that the cysts diffusely involved the entire pancreas. For evaluation of the abdominal masses, ultrasonography is a rapid and reliable technique used for cystic-solid differentiation. Use of color flow can help in distinguishing the vascular nature of lesions.[3] However, for an accurate localization there is a frequent necessity of cross sectional imaging. MR imaging may be insufficient for evaluating the origin of huge cysts. However, the relationship between a cyst and surrounding tissues, and extensions of a cyst can be demonstrated better with MR imaging due to its multiplanar capacity than with CT. In the present case, MR imaging provided excellent tissue characterization and soft tissue contrast. Polycystic disease of the pancreas, also known as dysontogenetic cysts, frequently occurs with other cysts. This suggests an etiologic relationship.[4] Most cases of congenital pancreatic cysts were associated with inherited polycystic disease of the kidney, liver, and spleen. Multiple pancreatic cysts have been described in patients with cystic fibrosis.[2] In our patient, evident symptoms related to the cystic mass had not been observed. True cysts are frequently localized in the tail or neck of the pancreas, 62%.[5,6] Our patient had no specific complaints related to his incidental underlying condition. USG and MR evaluation is a comprehensive work up for such patients supplanting CT scan and radiation exposure. In our case the cysts were not very large and MR imaging was sufficient to define the anatomical details of the pathology. The findings need to be confirmed histopathologically.
REFERENCES
- 1.Rowe MI, O’Neill JA Jr, Grosfeld JL, Fonkalsrud EW, Coran AG, editors. Essentials of pediatric surgery. Louis MO: MosbyYear Book; 1995. Disorders of the pancreas; pp. 663–74. [Google Scholar]
- 2.Daher P, Diab N, Melki I, Abi-Aad G, Korkmaz G. Congenital cyst of the pancreas.Antenatal diagnosis. Eur J Pediatr Surg. 1996;6:180–2. doi: 10.1055/s-2008-1066503. [DOI] [PubMed] [Google Scholar]
- 3.Casadei R, Campione O, Greco VM, Marrano D. Congenital true pancreatic cysts in young adults: Case report and literature review. Pancreas. 1996;12:419–21. doi: 10.1097/00006676-199605000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Nygaard KK, Walters W. Polycysticdiseaseof thepancreas(dysontogeneticcysts): Report of a case with partial pancreatectomy. Ann Surg. 1937;106:49–53. doi: 10.1097/00000658-193707000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cotran RS, Kumar V, Robbins SL. Robbins pathologic basis of disease. 5th ed. Philadelphia: WB Saunders; 1994. pp. 981–1010. [Google Scholar]
- 6.Kazez A, Akpolat N, Kocakoç E, Parmaksiz ME, Köseoğullari AA. Congenital true pancreatic cyst: A rare case. Diagn Interv Radiol. 2006;12:31–3. [PubMed] [Google Scholar]


