Abstract
Diabetes has emerged as a disease of major public health importance in India affecting the rich and the poor alike. Conventionally, comprehensive diabetes management is aimed at preventing micro and macro vascular complications. However, morbidity and mortality due to infections are also significant. In developing countries like India, the concept of adult immunization is far from reality. Recently the H1N1 pandemic has triggered the necessity for considering immunization in all age groups for the prevention of vaccine-preventable fatal infectious diseases. Considering the economics of immunization in a developing country, providing free vaccines to all adults may not be a practical solution, although the free universal immunization program for children is in existence for several decades. There is no consensus on the use of vaccines in diabetes subjects in India. However, there are some clinics offering routine pneumococcal, influenza and other vaccinations. Patients with diabetes have a deranged immune system making them more prone for infections. Hospitalization and death due to pneumococcal disease and influenza are higher in diabetes patients. They, like other healthy individuals, have a normal humoral response to vaccination with clinically significant benefits. The American Diabetes Association, Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention, World Health Organization, United Kingdom Guidelines and a number of other scientific organizations have well defined guidelines for vaccination in diabetes. In this article we make some suggestions for clinicians in India, regarding use of vaccines in subjects with diabetes.
Keywords: Diabetes, vaccination, immunization
INTRODUCTION
According to the International Diabetes Federation (IDF) Diabetes Atlas, in 2011 India is already home to 61.3 million diabetes subjects and this number is predicted to reach 101.2 million by 2030.[1] Diabetes complications are looming large and 65% of the reported deaths are due to the cardiovascular complications.[2] Diabetes also confers an increased risk of developing and dying from infectious diseases and it is now considered an important complication of diabetes.[3] Indeed, the morbidity and mortality associated with infectious diseases like influenza and pneumonia, which are preventable by appropriate vaccination, are also very high. Although people of all ages are prone to infectious diseases like pneumonia and influenza, extremes of age and certain underlying medical conditions such as diabetes, asthma, and cardiovascular disease (CVD) aggravate the risk.[4]
Recommendations for vaccines assume great significance due to the increased prevalence of drug-resistant influenza and pneumococcal disease, and related complications in the elderly. The increased susceptibility of diabetes subjects to pneumonia is mainly due to hyperglycemia, poor long-term diabetes control, longer duration of diabetes, decreased immunity, impaired lung function, pulmonary micro angiopathy, increased risk of aspiration and coexisting morbidity.[5] Longer duration of diabetes and poor glycemic control causes a 25–75% increase in the relative risk of pneumonia-related hospitalizations in diabetes subjects emphasizing the increased importance of immunization in diabetes subjects.[6]
The Centers for Disease Control's (CDC′s) Advisory Committee on Immunization Practices recommends influenza and pneumococcal vaccines for all individuals with diabetes.[7] A recent publication from India addresses the specific issue of Pneumococcal vaccination.[8]
In this article we review the role of all vaccinations in relation to diabetes. A systematic literature review was done and 52 studies were identified with particular focus on pneumonia and influenza vaccinations. Thirty-two Medline indexed studies are referenced along with Immunization Schedules and Morbidity and Mortality Week Reports (MMWR) by the CDC.
PREVALENCE OF INFECTIONS IN DIABETES
Pneumococcal infections
According to the World Health Organization (WHO), the mortality rate due to pneumococcal infections averages 10–20% while it may exceed 50% in high risk groups.[9] It is estimated that people with diabetes are almost three times at higher risk of death due to pneumonia-related complications.[10] Patients with Type 1 diabetes and type 2 diabetes have a 4.4- and 1.2-fold risk of pneumonia-related hospitalizations, respectively. Diabetes subjects with a HbA1c ≥9% are at 60% increased risk of pneumonia-related hospitalization. It is of interests that even those with an A1c <7% have 22% increased risk in comparison to nondiabetic subjects.[6] There is increasing evidence which suggest that diabetes is one of the most common co-morbidities associated with pneumococcal infections.[11]
Diabetes mellitus is an independent risk factor for developing respiratory tract infections due to alterations of host defenses.[10,12] This is attributed to several factors such as
Poor antibody response
Cell mediated abnormalities
-
Decreased CD4/CD8 lymphocyte ratios
- Changes in natural killer cell function
- Reduced lymphocyte blastogenesis
- Defects in interleukin-2 function
- Reduced phagocytic function of monocytes
Impaired leukocyte function
Predisposition to colonization and pneumonia
A recent study shows that patients with preexisting diabetes are at increased risk of community-acquired pneumonia, mainly due to the worsening of existing cardiovascular and kidney disease.[13] Unfortunately there is no published data from India on the prevalence of pneumonia or influenza in diabetes patients.
Influenza Infection
Mortality due to influenza is around 10,000–30,000 annually and people with diabetes are six times more likely to be hospitalized during an influenza epidemic[5] report that people with diabetes are six times more likely to be hospitalized during an influenza epidemic than those without diabetes, with the mortality varying between 5% and 15%. Evidence that influenza can trigger coronary complications, when taken in the context of diabetic subjects, gains more significance since the risk for CVD is already 2- to 4-fold higher in this sub group.[14] Sub group analysis and subsequent studies have shown vaccination to be efficacious as well as cost-effective in reducing hospital admissions as well as its associated complications.
A prospective study on the effects of a large-scale intervention with influenza and 23 valent pneumococcal vaccines in adults aged 65 years or older revealed that in general, vaccination leads to substantial health benefits and to a reduction of mortality from all causes in this age group.[15]
Hepatitis B infection
Hepatitis B virus (HBV) causes a life-threatening liver infection that often leads to chronic liver disease and puts people at high risk of death from cirrhosis of the liver and hepato-cellular carcinoma.
Patients with diabetes are at a 2.1 times increased risk of infection by the HBV than nondiabetics.[16] HBV can be transmitted by medical equipment that is contaminated with blood that is not visible to the unaided eye.[17] Exposures to HBV may occur as a result of assisted monitoring of blood glucose and other procedures involving multi-patient use of finger stick devices designed for single-patient use and inadequate disinfection and cleaning of blood glucose monitors between patients.[18]
RECOMMENDATIONS FOR VARIOUS VACCINATIONS
Pneumococcal vaccination
There are currently two types of pneumococcal vaccines: Pneumococcal conjugate vaccine (PCV7 and PCV13) and pneumococcal polysaccharide vaccine (PPV). PCV13 is slowly replacing PCV7.[7] The minimum age for administration of PCV and PPV are 6 weeks and 2 years, respectively.
Pneumococcal polysaccharide vaccine
Pneumococcal vaccine is a polyvalent, sterile, liquid vaccine for intramuscular or subcutaneous injection consisting of a mixture of highly purified capsular polysaccharides from the 23 most prevalent or invasive pneumococcal types of Streptococcus pneumoniae. The polyvalent polysaccharide vaccine contains 25 micrograms of purified capsular polysaccharide (0.5 ml per dose) from each of the 23 capsular types of Streptococcus pneumoniae, which is responsible for 90% of serious pneumococcal disease. The serotypes included in the vaccine are 1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V 10A, 11A, 12F, 14, 15B, 17F, 18C, 19A, 19F, 20, 22F, 23F, and 33F. The six serotypes that cause invasive drug resistant pneumococcal infections (6B, 9V, 14, 19A, 19F, and 23F) are represented in the 23 valent vaccine.
Pneumococcal conjugate vaccine
These are pneumococcal vaccines based on the conjugation of selected capsular polysaccharides to a protein carrier. The conjugate vaccine is supposed to be more efficient than the polysaccharide vaccine for the prevention of pneumococcal disease in children on account of immunological considerations and based on safety, immunogenicity, and efficacy trials.
Recommendations for vaccinations are based on the main risk factors for infectious diseases such as age, presence of chronic diseases, immuno-suppression, smoking status, alcohol use, and ethnic group. The organizations that have issued guidelines for pneumococcal vaccination include:
American Diabetes Association (ADA)
Advisory Committee on Immunization Practices (ACIP), USA.
The Australian Technical Advisory Group on Immunization(ATAGI)
The Canadian National Advisory Committee on Immunization
The United Kingdom Department of Health, and
The Geriatric Society of India
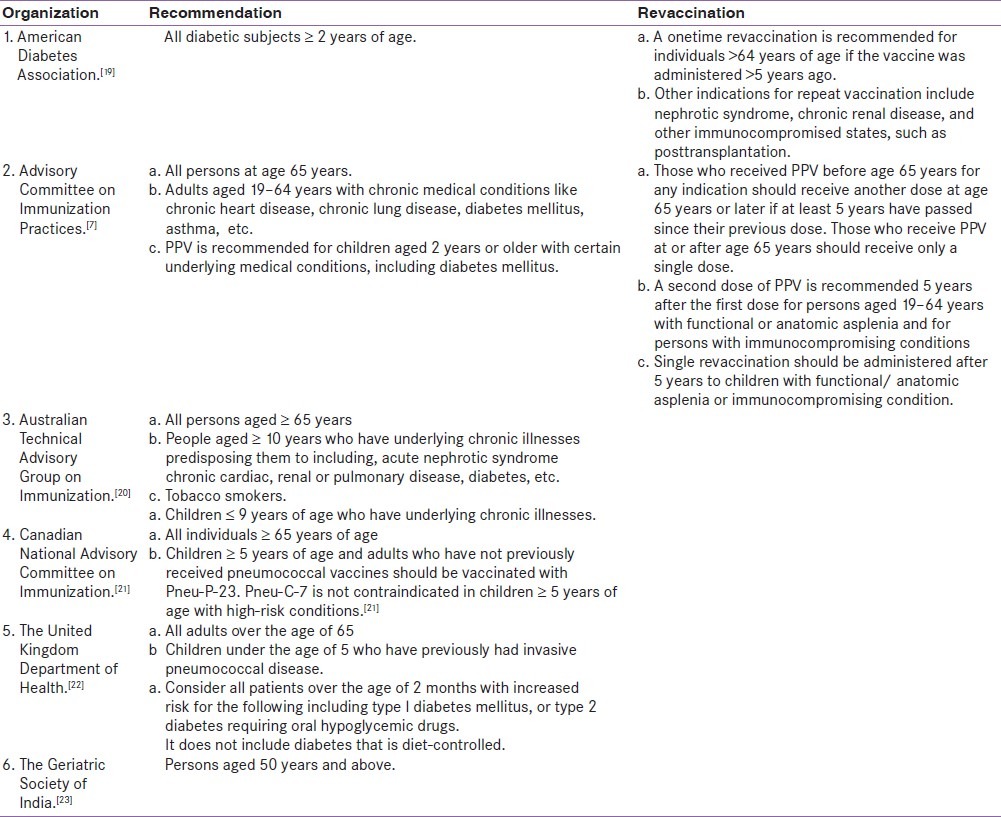
Recommendations by different organizations on Pneumococcal Vaccination are listed in Table 1.
Table 1.
Recommendations by different organizations on pneumococcal vaccination
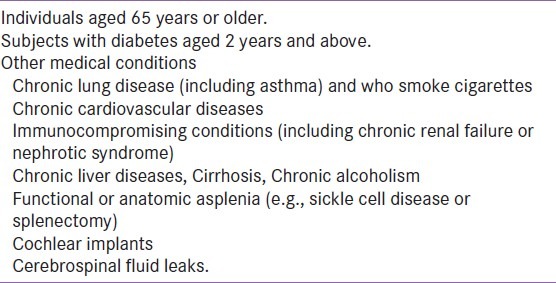
General indications for administration of Pneumococcal Polysaccharide Vaccination (PPV)[23] are enumerated in Table 2.
Table 2.
General indications for administration of pneumococcal polysaccharide vaccination[7]
Influenza vaccination
Influenza vaccine is recommended for all persons aged ≥6 months who do not have any contraindications to vaccination. Trivalent inactivated influenza vaccine (TIV) can be used for any person aged ≥6 months, including those with high-risk conditions. Live, attenuated influenza vaccine (LAIV) may be used for healthy nonpregnant persons aged 2–49 years. Since the safety or effectiveness of LAIV has not been established in persons with underlying medical conditions like chronic pulmonary (including asthma), cardiovascular (except hypertension) or metabolic (including diabetes mellitus) disorders that confer a higher risk for influenza complications, these persons should be vaccinated only with TIV. TIV contains inactivated viruses and thus cannot cause influenza. Only subvirion and purified surface antigen preparations of TIV (often referred to as “split” and subunit vaccines, respectively) are available. LAIV is administered intranasally, whereas TIV is administered intramuscularly.[24]
ACIP provides yearly guidelines on the prevention and treatment of influenza.[24] Pediatric guidelines from the American Academy of Pediatrics (AAP) are consistent with the ACIP recommendations for the 2011–2012 flu season.[25] According to the ACIP recommendations, vaccinating individuals at high risk before the influenza season each year is the most effective measure for reducing the impact of influenza. Annual influenza vaccination is recommended for all diabetes patients, both type 1 and type 2. On account of the change in circulating strains (antigenic drift) and waning immunity, yearly revaccination is required.
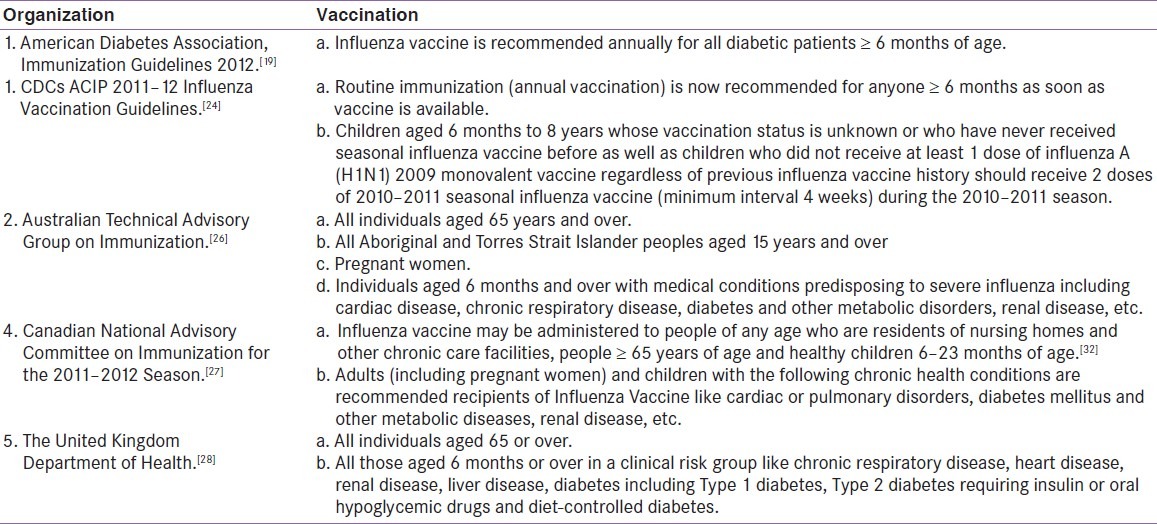
Recommendations by different organizations for Influenza vaccination is listed in Table 3.
Table 3.
Recommendations by different organizations for infl uenza vaccination
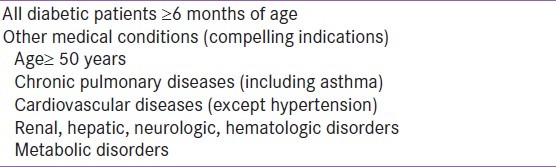
General indications for Influenza vaccination.[24] is enumerated in Table 4.
Table 4.
General indications for infl uenza vaccination
Fluzone high dose is an approved inactivated vaccine for subjects ≥65 years. People in this age group are at highest risk for seasonal influenza complications, which may result in hospitalization and death.[24] In clinical studies, Fluzone High-Dose demonstrated an enhanced immune response compared with Fluzone in individuals aged 65 years and older.[29]
Hepatitis B vaccination
On the basis of available information about HBV risk, morbidity and mortality, available vaccines, age at diagnosis of diabetes, and cost-effectiveness, ACIP 2012 recommends Hepatitis B vaccination for all unvaccinated adults with diabetes younger than 60 years as soon as feasible after diagnosis. Hepatitis B vaccination may be administered at the discretion of the treating clinician to unvaccinated adults with diabetes who are aged ≥60 years.[30] This may be based on likelihood of acquiring the infection at chronic care facilities (assisted blood glucose monitoring, insulin injections). Patients with Chronic Kidney Disease including those on hemodialysis should also be vaccinated.[31]
The vaccine is made from the inactivated (dead) hepatitis B virus. Two single-antigen recombinant hepatitis B vaccines are available. Hepatitis B vaccination usually consists of three doses of vaccine administered intramuscularly at 0, 1, and 6 months.[32]
EFFICACY AND SAFETY OF PNEUMOCOCCAL AND INFLUENZA VACCINATIONS
The efficacy and safety of pneumococcal vaccine have been shown in multiple case control studies as ranging from 56% to 81%.[33] In an indirect cohort analysis,[34] the efficacy of PPV23 was found to be 84% in diabetic patients and the efficacy of the vaccine did not decline with increasing interval after vaccination. In a retrospective study of a large cohort of 47,365 subjects aged 65 years or older, evidences suggest a vaccine effectiveness of 44% against pneumococcal bacteremia and hence its cost effectiveness for this indication.[35] There are a few studies claiming cost-effectiveness of pneumococcal vaccine and the most notable is a study from the US showing the vaccine to be highly cost effective in preventing pneumococcal bacteremia in people aged >65 years.[36] Pneumococcal vaccine is considered a safe and time-tested vaccine where moderately severe systemic reactions like fever and myalgia are uncommon while severe anaphylactic reactions are extremely rare.[37]
The newly licensed conjugate vaccine holds promise as a novel way of improving the immunogenicity of pure polysaccharide antigens and also of polysaccharides converted to T-cell dependent forms by protein conjugation.[38]
Literature search reveals statistically significant increase of antibody titer and an increased percentage of B-lymphocytes 1 week after influenza vaccination in diabetic subjects marking valid protection against the influenza virus. In a nested case-control study conducted during the 1999–2000 influenza A epidemic which was part of the Prevention of Influenza, Surveillance and Management (PRISMA) study, it was observed that adults with type 2 diabetes benefited considerably from influenza vaccination. Vaccination was associated with a 56% reduction in any complication (95% CI 36–70%), a 54% reduction in hospitalizations (26–71%), and 58% reduction in deaths (13–80%).[39]
Other vaccinations
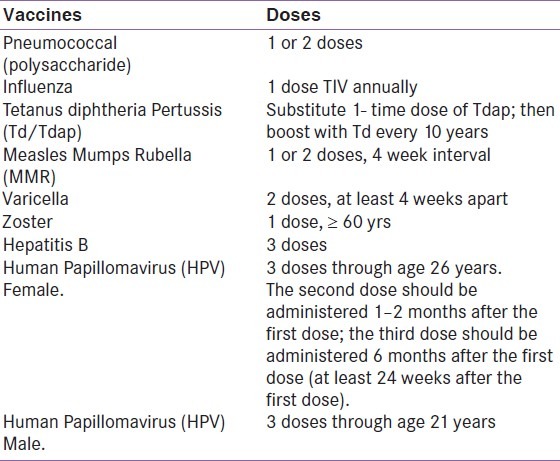
According to the Diabetes Public Health Resource of the Centers for Disease Control and Prevention, the following vaccinations are recommended for diabetes patients[40] In the Indian scenario there is a lack of evidence supporting the routine use of all the vaccines listed by CDC. Patients can be counseled on the necessity for Pneumococcal and Influenza vaccines, but other vaccines may be considered optional. It is quite obvious that immunization against vaccine preventable infections will be of considerable benefit in diabetes but their long-term cost effectiveness needs to be evaluated.
Recommended vaccines for diabetes patients[41] are given in Table 5.
Table 5.
Recommended vaccines for diabetes patients
STRATEGIES TO IMPROVE THE RATE OF VACCINATION
Maintaining a diabetes registry, systemic tracking system, and reminder system serve as tools for improvising the acceptance to vaccination.[42] Standing Orders Programs (SOPs) that allow nonphysician medical staff to assess eligibility and administer vaccines without an individualized physician's order are a proven method to increase vaccination rates.[43] However, recent data on their use are not available.[44] Close follow-up by the diabetes treatment team of the subjects especially with those aged ≥65 years would help achieve the vaccination goals in the most vulnerable groups. Communication with the subjects about the need for vaccination and initiatives like educational packages on immunization, etc., will help generate awareness on the importance of immunization. Setting up a vaccine-only clinic as adjunct or making provision for vaccination during routine visits to the clinic and strictly following the ADA and ACIP recommendations, are some of the strategies for effective immunization. According to the ADA position statement, benchmarking organizations and national policy should emphasize guideline implementation strategies for improving the rate of immunization.[45] Successful implementation of standing orders for vaccination and immunization are essential for increasing vaccination rates. Periodic training of the staff accompanied by ongoing assessment of immunization rates, work flow, and missed opportunities to immunize patients are critical to sustain and enhance improvements.[46] There should be a detailed plan for the program's infrastructure, key service delivery components and quality assurance.[47]
In the Indian clinic set up, the diabetologist, dietitian, diabetes educator, pharmacist, psychologist, and other members of the diabetes care team may take over the responsibility of counseling the patients on the availability and requirement of routine vaccinations. Use of educational material in local language, discussion on vaccination during diabetes education and the use of vaccination cards will boost confidence among the patients. Some of the strategies that may improve the rate and outcomes of vaccination include:
Identification of eligible candidates for vaccination.
Informing the patients and caregivers regarding the benefits and risks of the vaccination and documenting the delivery of that information.
Documenting refusal to take vaccination or presence of a contraindication like allergy to egg, a recent episode of Guillain–Barre syndrome, etc.
Recording the administration of a vaccine and records of revaccination or postvaccination adverse events.
Providing a documentation of vaccine administration to subjects like vaccination card with full information regarding the vaccines.
The standing order protocols should be implemented such that the health care professionals should be trained to:
screen patients who are most likely to benefit from and identifying those with contraindications to vaccinations
administer vaccines
monitor patients for adverse events.
The standards for adult immunization practice established by the National Coalition for Adult Immunization recommend a standard personal and institutional immunization record to verify the immunization status of patients and thus avoid the risk of inappropriate revaccination. Also a close follow-up with the vaccinee or his care giver by the treatment team or health care professional is highly beneficial in minimizing the risk of inappropriate re-vaccinations. The protocols should also aim at implementing a quality assurance process so that the standards of care are maintained.
EXPERIENCE WITH VACCINATION IN INDIA
In India, till date there is lack of consensus or published guidelines on vaccination in diabetes. There are some clinics offering routine pneumococcal and influenza vaccinations while other clinics do not recommend any vaccinations. From the available evidence, the two vaccinations which will be of profound clinical benefit and cost effective in diabetes subjects would be influenza and pneumococcal vaccines.
We present experiences with vaccination at two diabetes centers in India–one from south and one from north India.
In a Diabetes Research Center located in Trivandrum, south India, pneumococcal vaccine has been routinely administered to all consenting subjects with diabetes since 2005. Influenza vaccination has also been similarly practiced since 2009. During clinic visits, patients and their caregivers, are briefed on the availability of pneumococcal and influenza vaccines, its advantages in diabetes and long-term safety and efficacy. They are also provided with vaccination cards.
Affordability, willingness, and attitude toward the procedure are taken into consideration before vaccinating each subject. On analysis of the electronic data of subjects on regular follow up with the Diabetes Tele Management System (DTMS®) at Jothydev's Diabetes and Research Centre JDC,[48] of the 2057 subjects who underwent pneumococcal vaccinations, only 17 reported mild pain and redness at the site of injection which subsided in a day or two with oral paracetamol tablet. A total of 908 patients underwent flu shots since 2009 and none of them reported any injection side reactions or allergic responses. We found that 73% of the subjects aged >65 years had been administered the vaccine during one of their routine consultation visits. Of the subjects who received the pneumococcal vaccine 23% of the subjects were suffering from various diabetes-related complications like CVD, renal disease, retinopathy, etc. Age, gender, marital status, geographic area, educational level, occupation, type, duration and therapy of diabetes, and co-morbidities did not have a statistically significant effect on vaccination acceptance.
In a diabetes clinic at Kolkata, 1568 patients (duration >5.3 years) with diabetes were vaccinated against pneumonia and flu till December 15, 2010. The only side effects observed were aches or pain in joints or muscles, fever, local rash, or swollen glands. No severe allergic reactions were reported. Incidence of flu was drastically less with reduction of symptoms and absenteeism from flu when compared with the mean event rate as observed in the past 6 years.
SUGGESTED RECOMMENDATIONS FOR VACCINATION IN INDIA
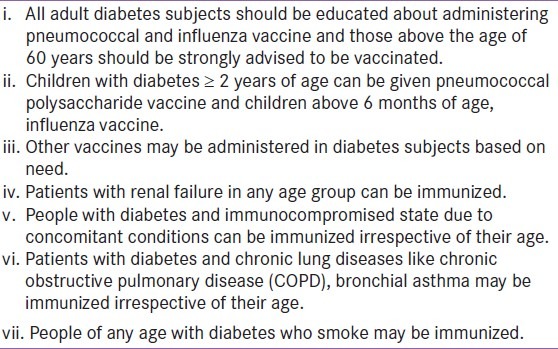
Based on our experience we make some recommendations for the use of pneumococcal and influenza vaccinations in patients with diabetes in India.
The suggested criteria for vaccination are listed in Table 6.
Table 6.
The suggested criteria for vaccination
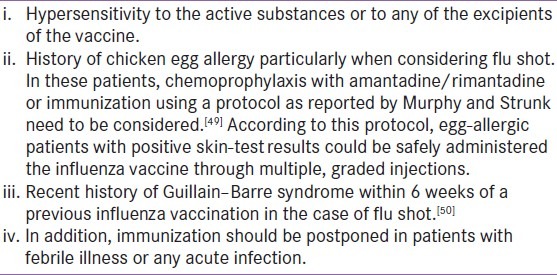
Contraindications to vaccination are listed in Table 7.
Table 7.
Contraindications to vaccination
CONCLUSION
Apart from considering conventional micro and macro vascular events as diabetes complications, infections due to influenza and pneumococci should also be regarded as having significant public health importance. All clinics where vaccinations are being advocated for diabetes should keep records of it so that efficacy of the vaccination may be assessed in relation to occurrence of fever, pneumonia, or hospitalization in vaccinated individuals compared with nonvaccinated subjects. Vaccination strategies in diabetes should evolve as part of routine care and a central registry need to be maintained. Long-term studies and research aimed at evaluating the cost-effectiveness of vaccination among diabetes patients in India would provide more evidence and support for the suggested vaccination guidelines.[50]
Footnotes
Source of Support: Nil
Conflict of Interest: No
REFERENCES
- 1.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 2.Fradkin J, Rodgers GP. The economic imperative to conquer diabetes. Diabetes Care. 2008;31:624–5. doi: 10.2337/dc08-0088. [DOI] [PubMed] [Google Scholar]
- 3.Shah BR, Hux JE. Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care. 2003;26:510–3. doi: 10.2337/diacare.26.2.510. [DOI] [PubMed] [Google Scholar]
- 4.Mohan V, Shanthirani CS, Deepa M, Deepa R, Unnikrishnan RI, Datta M. Mortality rates due to diabetes in a selected urban south Indian population–the Chennai Urban Population Study [CUPS-16] J Assoc Physicians India. 2006;54:113–7. [PubMed] [Google Scholar]
- 5.Smith SA, Poland GA. Use of influenza and pneumococcal vaccines in people with diabetes. Diabetes Care. 2000;23:95–108. doi: 10.2337/diacare.23.1.95. [DOI] [PubMed] [Google Scholar]
- 6.Kornum JB, Thomsen RW, Riis A, Lervang HH, Schønheyder HC, Sørensen HT. Diabetes, glycemic control, and risk of hospitalization with pneumonia: A population-based case-control study. Diabetes Care. 2008;31:1541–5. doi: 10.2337/dc08-0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Recommended adult immunization schedule–United States, 2012. J Midwifery Womens Health. 2012;57:188–95. doi: 10.1111/j.1542-2011.2011.00157.x. [DOI] [PubMed] [Google Scholar]
- 8.Mohan V, Unnikrishnan R, Thomas N, Bhansali A, Wangnoo SK, Thomas K. Pneumococcal infections and immunization in diabetic patients. J Postgrad Med. 2011;57:78–81. doi: 10.4103/0022-3859.74299. [DOI] [PubMed] [Google Scholar]
- 9.Pneumococcal vaccines [Internet] [Cited 2012 Apr 4]. Available from: http://www.who.int/vaccines/en/pneumococcus.shtml .
- 10.Akbar DH. Bacterial pneumonia: Comparison between diabetics and non-diabetics. Acta Diabetol. 2001;38:77–82. doi: 10.1007/s005920170017. [DOI] [PubMed] [Google Scholar]
- 11.Kyaw MH, Rose CE, Jr, Fry AM, Singleton JA, Moore Z, Zell ER, et al. The influence of chronic illnesses on the incidence of invasive pneumococcal disease in adults. J Infect Dis. 2005;192:377–86. doi: 10.1086/431521. [DOI] [PubMed] [Google Scholar]
- 12.Kornum JB, Thomsen RW, Riis A, Lervang HH, Schønheyder HC, Sørensen HT. Type 2 diabetes and pneumonia outcomes: A population-based cohort study. Diabetes Care. 2007;30:2251–7. doi: 10.2337/dc06-2417. [DOI] [PubMed] [Google Scholar]
- 13.Yende S, van der Poll T, Lee M, Huang DT, Newman AB, Kong L, et al. The influence of pre-existing diabetes mellitus on the host immune response and outcome of pneumonia: Analysis of two multicentre cohort studies. Thorax. 2010;65:870–7. doi: 10.1136/thx.2010.136317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warren-Gash C, Smeeth L, Hayward AC. Influenza as a trigger for acute myocardial infarction or death from cardiovascular disease: A systematic review. Lancet Infect Dis. 2009;9:601–10. doi: 10.1016/S1473-3099(09)70233-6. [DOI] [PubMed] [Google Scholar]
- 15.Christenson B, Lundbergh P, Hedlund J, Ortqvist A. Effects of a large-scale intervention with influenza and 23-valent pneumococcal vaccines in adults aged 65 years or older: A prospective study. Lancet. 2001;357:1008–11. doi: 10.1016/S0140-6736(00)04237-9. [DOI] [PubMed] [Google Scholar]
- 16.Reilly ML, Poissant T, Vonderwahl CW, Gerard K, Murphy TV. Presented at the 49th Annual Meeting of the Infectious Disease Society of America and the HIV Medicine Association. Boston, MA: 2011. Oct 20–23, Incidence of acute hepatitis B among adults with and without diabetes, 2009–2010. [Google Scholar]
- 17.Thompson ND, Perz JF. Eliminating the blood: ongoing outbreaks of hepatitis B virus infection and the need for innovative glucose monitoring technologies. J Diabetes Sci Technol. 2009;3:283–8. doi: 10.1177/193229680900300208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klonoff DC, Perz JF. Assisted monitoring of blood glucose: Special safety needs for a new paradigm in testing glucose. J Diabetes Sci Technol. 2010;4:1027–31. doi: 10.1177/193229681000400501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Diabetes Association. Standards of medical care in diabetes–2012. Diabetes Care. 2012;35(Suppl 1):S11–63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Australian Immunization Handbook.[Internet] 9th ed. 2008. [Cited 2012 Apr 4]. Available from: http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook-pneumococcal .
- 21.Government of Canada PHA of C. Part 3 - Recommended Immunization - Canadian Immunization Guide. Public Health Agency of Canada. 7th ed. 2006. [cited 2012 Apr 4]. Available from: http://www.phac-aspc.gc.ca/publicat/cig-gci/p03-07-eng.php .
- 22.Immunisation Schedule (UK) | Health | Patient.co.uk [Internet]. Patient.co.uk. [cited 2012 Apr 4]. Available from: http://www.patient.co.uk/doctor/Immunisation-Schedule-(UK).htm .
- 23.Guidelines for the use of Pneumococcal Polysaccharide Vaccine in India. A guide for geriatricians, chest physicians, internists, family physicians 2008. Developed by Geriatric Society of India [Google Scholar]
- 24.Centers for Disease Control and Prevention. Prevention and control of influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2011. Am J Transplant. 2011;11:2250–5. doi: 10.1111/j.1600-6143.2011.03793.x. [DOI] [PubMed] [Google Scholar]
- 25.American Academy of Pediatrics Committee on Infectious Diseases. Recommendations for prevention and control of influenza in children, 2011-2012. Pediatrics. 2011;128:813–25. doi: 10.1542/peds.2011-2295. [DOI] [PubMed] [Google Scholar]
- 26.The Australian Immunization Handbook. [Internet] Published by Australian Government, Department of Health and Ageing, National Health and Medical Research Council. 9th ed. 2008. [Cited 2012 Apr 4]. pp. 184–94. Available from: http://www.immunise.health.gov.au/internet/immunise/Publishing.nsf/content/40E9F669E3096146CA2579BA00097533/$File/ATAGI-advice-TIV-march2012-V2.pdf .
- 27.Government of Canada PHAOC. Statement on Seasonal Influenza Vaccine for 2011-2012 - Public Health Agency of Canada [Internet] [Cited 2012 Apr 4]. Available from: http://www.phac-aspc.gc.ca/publicat/ccdr-rmtc/11vol37/acs-dcc-5/index-eng.php .
- 28.Influenza Vaccination | Health | Patient.co.uk [Internet]. Patient. co.uk. [Cited 2012 Apr 5]. Available from: http://www.patient.co.uk/showdoc/40024883/
- 29.Falsey AR, Treanor JJ, Tornieporth N, Capellan J, Gorse GJ. Randomized, double-blind controlled phase 3 trial comparing the immunogenicity of high-dose and standard-dose influenza vaccine in adults 65 years of age and older. J Infect Dis. 2009;200:172–80. doi: 10.1086/599790. [DOI] [PubMed] [Google Scholar]
- 30.Kuehn BM. Immunization recommendations expanded for hepatitis B, HPV, pertussis vaccines. JAMA. 2012;307:1353–4. doi: 10.1001/jama.2012.367. [DOI] [PubMed] [Google Scholar]
- 31.Recommended Adult Immunization Schedule - United States [Internet] [Cited 2012 Apr 4]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6104a9.htm .
- 32.Use of Hepatitis B Vaccination for Adults with Diabetes Mellitus: Recommendations of the Advisory Committee on Immunization Practices (ACIP) [Internet] [Cited 2012 May 14]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6050a4.htm . [PubMed]
- 33.Shapiro ED. Prevention of pneumococcal infection with vaccines: An evolving story. JAMA. 2012;307:847–9. doi: 10.1001/jama.2012.194. [DOI] [PubMed] [Google Scholar]
- 34.Butler JC, Breiman RF, Campbell JF, Lipman HB, Broome CV, Facklam RR. Pneumococcal polysaccharide vaccine efficacy.An evaluation of current recommendations. JAMA. 1993;270:1826–31. [PubMed] [Google Scholar]
- 35.Jackson LA, Neuzil KM, Yu O, Benson P, Barlow WE, Adams AL, et al. Effectiveness of pneumococcal polysaccharide vaccine in older adults. N Engl J Med. 2003;348:1747–55. doi: 10.1056/NEJMoa022678. [DOI] [PubMed] [Google Scholar]
- 36.Sisk JE, Moskowitz AJ, Whang W, Lin JD, Fedson DS, McBean AM, et al. Cost-effectiveness of vaccination against pneumococcal bacteremia among elderly people. JAMA. 1997;278:1333–9. [PubMed] [Google Scholar]
- 37.Honkanen PO, Keistinen T, Kivelä SL. Reactions following administration of influenza vaccine alone or with pneumococcal vaccine to the elderly. Arch Intern Med. 1996;56:205–8. [PubMed] [Google Scholar]
- 38.Ortqvist A. Pneumococcal vaccination: Current and future issues. Eur Respir J. 2001;18:184–95. doi: 10.1183/09031936.01.00084401. [DOI] [PubMed] [Google Scholar]
- 39.Looijmans-Van den Akker I, Verheij TJ, Buskens E, Nichol KL, Rutten GE, Hak E. Clinical effectiveness of first and repeat influenza vaccination in adult and elderly diabetic patients. Diabetes Care. 2006;29:1771–6. doi: 10.2337/dc05-2517. [DOI] [PubMed] [Google Scholar]
- 40.CDC – Vaccinations - Take Charge of Your Diabetes – Publications - Diabetes DDT [Internet] [Cited 2012 Apr 4]. Available from: http://www.cdc.gov/diabetes/pubs/tcyd/vaccin.htm .
- 41.Recommended Adult Immunization Schedule - United States, 2012 [Internet] [Cited 2012 May 14]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6104a9.htm .
- 42.Smith SA, Poland GA. Influenza and pneumococcal immunization in diabetes. Diabetes Care. 2004;27(Suppl 1):S111–3. doi: 10.2337/diacare.27.2007.s111. [DOI] [PubMed] [Google Scholar]
- 43.Zimmerman RK, Albert SM, Nowalk MP, Yonas MA, Ahmed F. Use of standing orders for adult influenza vaccination a national survey of primary care physicians. Am J Prev Med. 2011;40:144–8. doi: 10.1016/j.amepre.2010.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yonas MA, Nowalk MP, Zimmerman RK, Ahmed F, Albert SM. Examining structural and clinical factors associated with implementation of standing orders for adult immunization [Internet] J Healthc Qual. 2011 doi: 10.1111/j.1945-1474.2011.00144.x. [In press] [DOI] [PubMed] [Google Scholar]
- 45.Smith SA, Poland GA American Diabetes Association. Influenza and pneumococcal immunization in diabetes. Diabetes Care. 2004;27(Suppl 1):S111–3. doi: 10.2337/diacare.27.2007.s111. [DOI] [PubMed] [Google Scholar]
- 46.Swenson CJ, Appel A, Sheehan M, Hammer A, Fenner Z, Phibbs S, et al. Using information technology to improve adult immunization delivery in an integrated urban health system. Jt Comm J Qual Patient Saf. 2012;38:15–23. doi: 10.1016/s1553-7250(12)38003-3. [DOI] [PubMed] [Google Scholar]
- 47.McKibben LJ, Stange PV, Sneller VP, Strikas RA, Rodewald LE. Use of standing orders programs to increase adult vaccination rates. MMWR Recomm Rep. 2000;49:15–16. [PubMed] [Google Scholar]
- 48.Kesavadev J, Shankar A, Shamsudeen J, Dinkar G, Pillai PB, Gopalakrishnan Telefollow up and SMBG via “DTMS” - A cost effective tool for A1c lowering. Diabetes. 2010;59(Suppl 1):A546. [Google Scholar]
- 49.Murphy KR, Strunk RC. Safe administration of influenza vaccine in asthmatic children hypersensitive to egg proteins. J Pediatr. 1985;106:931–3. doi: 10.1016/s0022-3476(85)80241-9. [DOI] [PubMed] [Google Scholar]
- 50.Lasky T, Terracciano GJ, Magder L, Koski CL, Ballesteros M, Nash D, et al. The Guillain-Barré syndrome and the 1992-1993 and 1993-1994 influenza vaccines. N Engl J Med. 1998;339:1797–802. doi: 10.1056/NEJM199812173392501. [DOI] [PubMed] [Google Scholar]


