Abstract
Objective
Millions of women in the United States and across the globe abruptly discontinued postmenopausal hormone therapy (HT) after the initial Women’s Health Initiative trial publication. Few data describing the effects of HT cessation on hip fracture incidence in the general population are available. We evaluated the impact of HT cessation on hip fracture incidence in a large cohort from the Southern California Kaiser Permanente health management organization.
Methods
In this longitudinal observational study, 80,955 postmenopausal women using HT as of July 2002 were followed up through December 2008. Data on HT use after July 2002, antiosteoporotic medication use, and occurrence of hip fracture were collected from the electronic medical record system. Bone mineral density (BMD) was assessed in 54,209 women once during the study period using the dual-energy x-ray absorptiometry scan.
Results
After 6.5 years of follow-up, age- and race-adjusted Cox proportional hazard models showed that women who discontinued HT were at 55% greater risk of hip fracture compared with those who continued using HT (hazard ratio, 1.55; 95% CI, 1.36–1.77). Hip fracture risk increased as early as 2 years after cessation of HT (hazard ratio, 1.52; 95% CI, 1.26–1.84), and the risk incrementally increased with longer duration of cessation (P for trend < 0.0001). Longer duration of HT cessation was linearly correlated with lower BMD (β estimate [SE]) = −0.13 [0.003] T-score SD unit per year of HT cessation; P < 0.0001).
Conclusions
Women who discontinued postmenopausal HT had significantly increased risk of hip fracture and lower BMD compared with women who continued taking HT. The protective association of HT with hip fracture disappeared within 2 years of cessation of HT. These results have public health implications with regard to morbidity and mortality from hip fracture.
Keywords: Hormone therapy, Hip fracture, Bone mineral density, Women’s Health Initiative
Since the publication of the initial Women’s Health Initiative (WHI) trial findings in June 2002,1 millions of women have discontinued postmenopausal hormone therapy (HT),2–4 and HT prescriptions have concordantly dropped.5 In a survey of US obstetrician-gynecologists, although 53% of clinicians reported that they were unlikely to change their HT prescription pattern after WHI, 93% of their patients were willing to discontinue HT, and 92% were less likely to request HT.6 It is clearly apparent that a large number of postmenopausal women abruptly stopped HT after the initial WHI publications. However, little epidemiologic research of the clinical outcomes associated with HT cessation has been evaluated in these women.
Protection from bone loss and fracture is a conclusive HT benefit.7 It is therefore conceivable that hip fracture risk, which is associated with a 25% case-fatality rate, has increased in the post-WHI era.8,9 However, this potential public health malady has not been examined in the general population. In a large cohort of 80,955 postmenopausal women who were using HT until June 2002, we calculated the hip fracture incidence after HT cessation compared with those who continued using HT.
METHODS
Study population
Kaiser Permanente Southern California (KaiserSCAL) is a Health Maintenance Organization that includes 11 Southern California medical centers. This longitudinal study included 80,955 postmenopausal women enrolled in KaiserSCAL who were 60 years or older and had filled HT prescriptions at least once between January 2002 and June 2002. The women were followed up through December 2008.
Exposures and outcomes
KaiserSCAL uses an electronic medical record (EMR) system that records medical data in a standardized format across all 11 medical centers. EMR data are passed to and stored in a central data warehouse (“Clarity”) daily using the Health Connect software. Hip fracture outcomes, dual-energy x-ray absorptiometry (DXA) scan, and demographic data were collected from the Clarity database. All hip fractures were subsequently verified from a chart review by R.M.D., who was blinded to HT status.10 Hip fractures secondary to tumors, periprosthetic fractures, and high-energy trauma were excluded from this analysis. Incident hip fractures were identified by the diagnosis date of fracture, which usually was followed by corrective surgery. We did not have data on fracture history; therefore, the fractures identified included some unknown number of recurrent fractures. Hip fractures diagnosed in KaiserSCAL but treated outside (<2%) Kaiser-SCAL were also included in this analysis.
KaiserSCAL uses an electronic Pharmacy Information Management System, which was used to collect HT and other antiosteoporotic medication (bisphosphonates) prescriptions from all 11 KaiserSCAL medical centers. Clarity and Pharmacy Information Management System databases were linked by a medical record number unique to each member. In each calendar year, a woman was considered to be an HT user if at least two HT prescriptions were filled in that year; if one or no HT prescriptions were filled, the woman was considered to be an HT nonuser for that calendar year. Each HT prescription provides 3 months of medication supply. Bisphosphonate use in each calendar year was identified using a similar definition.
Bone mineral density (BMD) of the hip and lumbar regions was measured as T scores in 54,209 women by DXA scans performed between 2002 and 2008; body mass index (BMI) was available for 43,024 of these women. According to the guidelines of the National Osteoporosis Foundation, the lower BMD of the two regions (hip and lumbar) was recorded. Baseline age was categorized into 5-year increments (<65, 65–69, 70–74, 75–79, ≥80 y). Self-reported race was defined as non-Hispanic white, black, Hispanic, Asian, others, and unknown. BMI was categorized according to Centers for Disease Control and Prevention cut points (<18, 18–24, 25–29, ≥30 kg/m2).
The study was approved by the institutional review board of KaiserSCAL.
Statistical analysis
Hip fracture outcome
Directly age-standardized hip fracture rates for each calendar year (2002–2008) were calculated with age-specific hip fracture rates standardized to the age distribution of the 2000 California female population (US Census 2000). The trend in the hip fracture rates over calendar years was assessed using the Poisson regression in a generalized linear model with a log-link function (SAS GENMOD procedure). The rates of HT use for each calendar year were calculated as the number of women using HT divided by the total number of women in that year.
Cox proportional hazards regression was used to evaluate the impact of not using HT in a given year (time-dependent variable) on the risk of having a hip fracture in the subsequent year. Person-years of follow-up were accrued from July 2002 to date of hip fracture. For women who did not have a hip fracture, follow-up was censored at the earliest of death, date of termination of KaiserSCAL membership, or June 30, 2008. A total of 6,928 (9%) women died, and 12,486 (15%) women terminated their KaiserSCAL membership during the follow-up period. The cumulative duration of HT nonuse (in years; modeled as a time-dependent variable) from 2002 was also tested for an association with hip fracture in a separate Cox regression model. Baseline age, race, and BMI were fixed in univariate and multivariate Cox regression models. The proportional hazards assumption for the association of HT nonuse with hip fracture risk was evaluated and met (P > 0.90 for the proportional hazard assumption test). Estimates of association were expressed as hazard rate ratios (HRs) with 95% CIs. Because BMI data were available in a subset (n = 43,024) of women, multivariate models with and without BMI were compared to examine the confounding effect of BMI in this subset. The HRs for HT nonuse did not substantially differ in the two models; hence, the final model was not adjusted for BMI and included all women. Adjustment for bisphosphonate use did not alter the association between HT nonuse and hip fracture and was, therefore, not included in the final model. To evaluate any modifying effect of age on the risk of hip fracture associated with not using HT, stratified modeling was performed by the 5-year incremental age group; a formal test of interaction was also evaluated by introducing a product term of age group and HT nonuse in the Cox proportional hazard model.
Bone density outcome
BMD was correlated with HT nonuse using a linear regression model. For this analysis, a cumulative variable was created for each woman counting the number of years not using HT from baseline (2002) to the year of DXA scan. Continuous HT users were assigned a value of zero. In the linear regression model, the T score from each participant’s DXA scan was the dependent variable, and the cumulative years of HT nonuse was the independent variable. The model was adjusted for race, age, BMI, bisphosphonate use at the time of DXA scan, and year of DXA scan.
All statistical analyses were performed using SAS, version 9.1 (SAS Institute, Cary, NC).
RESULTS
A total of 80,955 women contributed 532,686 person-years of observation between July 2002 and December 2008. The mean (SD) follow-up was 5.6 (1.1) years. The mean (SD) age of the women at baseline was 68.8 (6.8) years; 80% of the women were between 60 and 74 years old. Most of the women were white (54%), with a mean (SD) BMI of 26.9 (5.3) kg/m2. Compared with the women taking HT, those who discontinued at baseline were more likely to take bisphosphonates (8% vs 11%, P < 0.0001; Table 1). Fewer white and more nonwhite women discontinued HT at baseline (P < 0.0001). Bisphosphonate drug use increased from 8% to 23% during the study period.
TABLE 1.
Baseline characteristics of participants (n = 80,955)
| Characteristics | HT continuers | HT discontinuers | P |
|---|---|---|---|
| Age, y | |||
| <65 | 23,007 (34%) | 4,152 (33%) | |
| 65–69 | 18,896 (28%) | 3,483 (28%) | |
| 70–74 | 12,603 (18%) | 2,306 (19%) | 0.9 |
| 75–80 | 7,857 (11%) | 1,421 (11%) | |
| >80 | 6,124 (9%) | 1,106 (9%) | |
| Mean (SD) | 68.8 (6.8) y | 68.8 (6.8) y | 0.9 |
| BMI, kg/m2 | |||
| <18 | 449 (1%) | 75 (1%) | |
| 18–24 | 12,735 (35%) | 2,267 (35%) | 0.9 |
| 25–29 | 13,679 (37%) | 2,459 (38%) | |
| ≥30 | 9,691 (27%) | 1,712 (26%) | |
| Mean (SD) | 26.8 (5.3) kg/m 2 | 26.9 (5.3) kg/m 2 | 0.7 |
| Race | |||
| White | 37,739 (55%) | 6,213 (50%) | |
| Black | 4,104 (6%) | 827 (7%) | |
| Hispanic | 5,309 (8%) | 1,126 (9%) | <0.0001 |
| Asian | 2,489 (4%) | 712 (6%) | |
| Unknown | 17,796 (26%) | 3,423 (28%) | |
| Other | 352 (1%) | 58 (1%) | |
| Use of bisphosphonate | |||
| No | 63,069 (92%) | 11,118 (89%) | <0.0001 |
| Yes | 5,418 (8%) | 1,350 (11%) | |
BMI was available in 43,024 women.
HT, hormone therapy; BMI, body mass index.
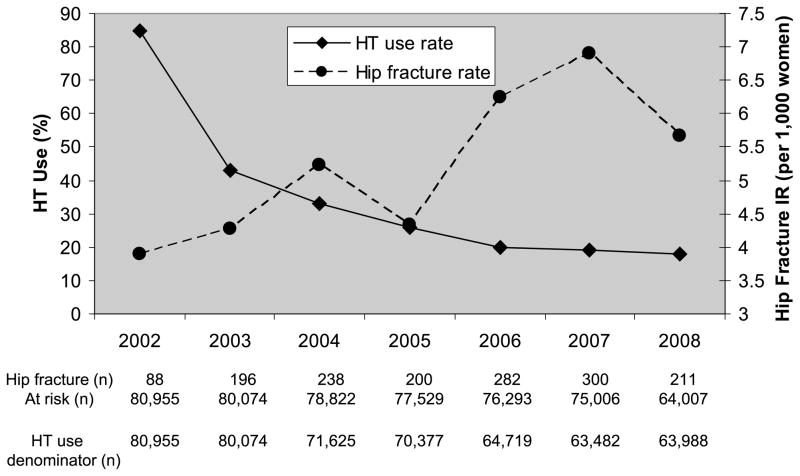
HT use substantially decreased between July 2002 and December 2008 from 85% to 18%. The age-standardized annual hip fracture rate increased from 3.9 to 5.67 per 1,000 women during this same period (Fig. 1; P for trend < 0.0001). In unadjusted Cox regression models, hip fracture risk was positively associated with age and inversely associated with BMI (both P values for trend < 0.0001; Table 2). Compared with non-Hispanic white women, black, Hispanic, and Asian women had significantly lower hip fracture risk. Compared with HT users, the women who did not use HT in the previous year were 58% more likely to have a hip fracture in the following year (HR, 1.58; 95% CI, 1.38–1.80).
FIG. 1.
Trend in annual HT use (percent) and age-standardized hip fracture IRs between 2002 and 2008. Note that the female population in California from Census 2000 was used as the standard population to calculate the age-standardized rates. The rate for 2002 was divided by 0.50 because the data during the 6-month period (July-December) were used. The difference in the number of women available for hip fracture rate and HT use prevalence rate is due to missing HT use data in years 2004, 2005, 2006, 2007, and 2008. HT, hormone therapy; IR, incidence rate.
TABLE 2.
Risk factors associated with hip fracture in women older than 60 years
| Risk factors (univariate analysis) | Hazard ratio (95% CI) | P |
|---|---|---|
| Age, y | <0.0001a | |
| <65 | 1.0 | |
| 65–69 | 1.90 (1.48–2.43) | |
| 70–74 | 4.34 (3.45–5.47) | |
| 75–80 | 9.52 (7.63–11.9) | |
| >80 | 19.4 (15.7–24.1) | |
| Race | ||
| White | 1.0 | <0.0001 |
| Black | 0.34 (0.25–0.46) | |
| Hispanic | 0.57 (0.46–0.71) | |
| Asian | 0.39 (0.22–0.43) | |
| Unknown | 0.16 (0.13–0.20) | |
| Others | 0.30 (0.10–0.93) | |
| BMI, kg/m 2 | <0.0001a | |
| <18 | 4.05 (3.00–5.54) | |
| 18–24 | 1.0 | |
| 25–29 | 0.50 (0.41–0.59) | |
| ≥30 | 0.28 (0.21–0.35) | |
| HT use in the current year | ||
| Yes | 1.0 | |
| No | 1.51 (1.32–1.72) | <0.0001 |
| HT use in the previous year | ||
| Yes | 1.0 | |
| No | 1.58 (1.38–1.80) | <0.0001 |
BMI, body mass index; HT, hormone therapy.
P value for trend.
After adjustment for age and race, the women not using HT in the previous year had a 55% increased risk of hip fracture (HR, 1.55; 95% CI, 1.36–1.77; Table 3). Adjustment for bisphosphonate use did not attenuate the hip fracture risk associated with not using HT in the prior year (adjusted HR, 1.66; 95% CI, 1.46–1.90). The impact of BMI on this association of HT cessation was tested in the subset of 43,024 women with BMI data. The HR (95% CI) associated with HT nonusers was 1.81 (1.49–2.20) in the model that included age, race, and BMI and 1.77 (1.45–2.14) in the model that did not include BMI.
TABLE 3.
Multivariate analysis for risk of hip fracture and HT use
| Risk factors | Hazard ratio (95% CI) | P |
|---|---|---|
| Model 1 | ||
| No HT use in the previous yeara | 1.55 (1.36–1.77) | <0.0001 |
| Race | ||
| White | 1.0 | |
| Black | 0.51 (0.38–0.69) | <0.0001 |
| Hispanic | 0.74 (0.60–0.91) | |
| Asian | 0.44 (0.31–0.63) | |
| Unknown | 0.30 (0.24–0.37) | |
| Other | 0.51 (0.19–1.37) | |
| Age (5-y increment) | 1.97 (1.89–2.05) | <0.0001 |
| Model 2 (adjusted for age and race) | ||
| Total no. of years not on HT after 2002a | <0.0001 | |
| 0 | 1.0 | |
| 1 | 1.16 (0.96–1.40) | |
| 2 | 1.52 (1.26–1.84) | |
| 3 | 1.64 (1.34–2.00) | |
| 4 | 1.68 (1.36–2.08) | |
| ≥5 | 1.77 (1.44–2.18) | |
HT, hormone therapy.
Variables considered time-dependent in Cox regression model.
The multivariate model used to test the cumulative years of not using HT during the 6.5-year follow-up showed that hip fracture risk significantly increased with longer duration of HT cessation (P < 0.0001). Compared with the women who continued HT from 2002 through 2008, the women who discontinued HT showed increasing hip fracture risk over time: 52% after 2 years, 64% after 3 years, 68% after 4 years, and 77% after 5 years of cessation (Table 3).
Stratified analysis by the 5-year incremental age group showed no modifying effect of age on hip fracture risk associated with not using HT (P value for interaction = 0.10).
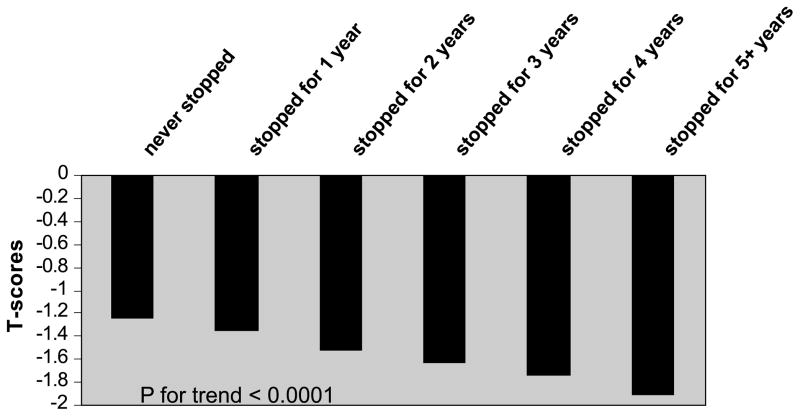
The mean BMD T-scores in linear regression models were significantly inversely associated with cumulative years of HT nonuse. Adjusted for age, race, BMI, and bisphosphonate use, the mean (SEM) T scores for the women who continued HT from 2002 was −1.24 (0.01) compared with −1.88 (0.01) in those who did not use HT from 2002 to 2008; Adjusted for age, race, BMI and bisphosphonate use, mean (SEM) T-scores for women who continued HT from 2002 was −1.24 (0.01) compared to −1.88 (0.01) in those who did not use HT from 2002 to 2008; longer duration of HT cessation was linearly correlated with lower BMD (β-estimate [SE]) = −0.13 (0.003) T-score SD unit per year of HT cessation (P for trend < 0.0001; Fig. 2). In this subgroup of women with BMD data, we tested the association of BMD with fracture risk subsequent to BMD measurement (data not shown). Lower BMD was also significantly associated with a risk of hip fracture; compared with the women with a T score greater than −1, the women with T scores between −1 and −2.5 were 2.5 times more likely (HR, 2.54; 95% confidence limit, 1.51–4.27) and the women with T scores less than −2.5 were 7.6 times more likely to have a hip fracture (HR, 7.59; 95% confidence limit, 4.53–12.7).
FIG. 2.
T scores in relation to years of not using HT since 2002. Note the mean BMD T-scores by cumulative years of HT nonuse before the year of DXA scan in 54,209 women. The linear regression model was adjusted for age, race, BMI, bisphosphonate use at the time of DXA scan, and year of DXA scan. HT, hormone therapy; BMD, bone mineral density; DXA, dual-energy x-ray absorptiometry; BMI, body mass index.
DISCUSSION
In this large cohort of postmenopausal women followed for 6.5 years, HT discontinuation was associated with an overall 55% increased hip fracture risk (P < 0.0001). More importantly, this risk increased in as little as 2 years of HT discontinuation. The lower BMD in women who discontinued HT (P for trend < 0.0001), as previously noted,11,12 is likely to be associated with the increased fracture risk. The public health message for women and physicians is that discontinuation of HT is associated with an increased hip fracture risk and lower BMD compared with women who continue to take HT.
Observational studies have consistently reported a significant 38% to 60% reduction in the risk of fractures including hip, wrist, and vertebral fractures among current or ever users of HT compared with never users.13–16 A meta-analysis of 22 clinical trials reported an overall 27% reduction in nonvertebral fractures among current estrogen users.17 WHI is the first large-scale, randomized, controlled trial to demonstrate that HT reduces incident bone fractures including hip fractures. The WHI estrogen-progestin trial documented significant reductions in hip, lower arm/wrist, vertebral, and total fracture incidence by 33%, 29%, 35%, and 24%, respectively, among women assigned to estrogen plus progestin compared with placebo during a 5.6-year trial period.1,18 Reports from the WHI estrogen trial documented similar protection (35%–39% reduction) for hip fracture and improvement in BMD among estrogen-treated compared with placebo-treated women during a 7-year trial period.19,20 Importantly, the WHI trials convincingly demonstrated that HT is beneficial in reducing bone fracture, because unlike all previous bone fracture trials, the WHI cohort was not selected for low BMD or previous fractures. Therefore, the WHI trial results have general application to all postmenopausal women seeking HT for the primary prevention of bone fracture.
Presentation of WHI trial results in June 2002 had an immediate impact on HT prescription patterns. In the United States, HT prescription rates declined by 46% between July 2002 and December 2002,2 whereas another report showed a 44% decline between 2001 and 2003.5 A similar magnitude of decline in HT prescriptions was also observed around the world after the diffusion of WHI trial results.4,21,22 Guidelines for HT were subsequently modified with recommendations against HT for chronic disease prevention including osteoporosis in postmenopausal women.23 A recent study using a claims database for multiple healthcare plans documented significantly higher age-adjusted incidence rate of osteoporosis-related fractures among 40- to 69-year-old women between 2004 and 2005 compared with rates between 2000 and 2001.24 Our results confirm and extend this observation showing an increase in hip fracture incidence between 2002 and 2008 in women who discontinued HT.
Our findings that link HT cessation with fracture risk are supported by a 2.4-year follow-up of WHI estrogen-progestin participants after termination of the trial whereby all fractures were analyzed according to randomized status during the trial.25 Although the HR did not statistically differ between the randomized trial and posttrial follow-up, the HT protective effect on fractures documented during the trial (HR, 0.76 relative to placebo; 95% CI, 0.69–0.83) was not evident in the posttrial follow-up (HR, 0.91; 95% CI, 0.78–1.06). These data support the idea that the protective effect of HT on bone fracture does not continue upon HT cessation. However, the analytic approach used in this WHI report may have underestimated the bone fracture burden as a consequence of HT discontinuance because HT use after trial cessation was not modeled. In the current study, only women using HT until June 2002 and then who discontinued HT were compared with those who continued HT.
In this report, we showed that in the past users of HT, hip fracture risk increased with longer duration of HT nonuse compared with women who continued. Hip fracture risk was significantly elevated relative to current users within 2 years of HT cessation and remained elevated thereafter (Table 3). This is consistent with a report from the Million Women Study, where bone protection from HT disappeared rapidly and an increased risk of fracture incidence was observed 3 years after HT cessation among past HT users.13
Our data showed no alteration in hip fracture risk associated with HT discontinuation after controlling for bisphosphonate use. This means that the increased risk of hip fracture in women who stopped taking HT was not confounded by the effect of bisphosphonates on hip fracture.
Consistent with our fracture results, we also found a significant correlation of longer duration of HT nonuse with lower BMD and longer duration of HT nonuse (P for trend < 0.0001; Fig. 2). These results are consistent with clinical trials evaluating the effect of HT discontinuation on BMD and bone marker changes in younger12 and older postmenopausal women.11 However, because BMD was assessed one time only in this study, we were not able to examine the longitudinal changes in BMD by the presence and duration of HT cessation. Our findings confirm these data in a much larger group of women with a longer follow-up.
The major strength of our study is the large group of women (n = 80,955) well representative of the general population. In addition, linking electronic pharmacy records with EMR provides a powerful tool for concomitantly tracking medication prescriptions and clinical outcomes. Of note, each hip fracture diagnosis was verified by a single orthopedic surgeon who was blinded to HT exposure status (R.M.D.).
The major limitation of this study is lack of data before 2002 concerning HT use for bone fracture. It is possible that fracture risk after HT cessation was higher among women with previous fractures; however, it is not known whether previous fracture history influenced the continuation of HT use. If anything, women with prior fracture are less likely to stop HT. In this case, results of our study would be biased toward the null, and thus, the increased risk of hip fracture observed in our study with HT cessation is probably conservative. However, other studies including the relevant data are required to substantiate our conjectures regarding the pattern of HT use among women with prior fractures. Another limitation of our study is incomplete BMI information, which might have confounded the association between HT use and fracture risk. However, in the Cox regression models among the subset of 43,024 women with measured BMI, the HRs for HT nonuse did not differ in models with and without adjustment for BMI (HR, 1.81 vs 1.77). Hence, BMI was not a likely confounder in this analysis. We were unable to control for key factors known to be associated with bone fracture risk including smoking, low physical activity, and diet. Therefore, these results should be interpreted with caution.
Our data confirm the rapidity of bone loss and increased hip fracture incidence with HT cessation. Bone fracture is a large public health issue with major medical and economic consequences. The cost of medical care associated with osteoporotic fractures is estimated to be more than $18 billion annually in the United States alone. Hip fractures result in a greater cost, disability, and mortality than all other osteoporotic fractures combined. Within the first year of a hip fracture, there is an approximate 25% increase in mortality.9,26 According to a recent meta-analysis, the excess annual mortality among white women having hip fracture was 8%, 11%, 18%, and 22% at 1, 2, 5, and 10 years after injury.27 In addition, 25% of women require long-term care after a hip fracture, and 50% will have long-term loss of mobility. A 50% increased risk of bone fracture associated with a 50% decreased use of HT in the United States has been estimated to result in 43,000 extra bone fractures per year.8 A recent cost-effectiveness analysis suggested a considerable gain in quality-adjusted life-years among HT user and cost-effectiveness of HT use.28
CONCLUSIONS
Our results indicate that the protective association of HT on hip fracture does not extend after cessation. Cessation of HT among postmenopausal women is associated with a significant greater risk of hip fracture within 2 years of cessation. The associations of HT cessation on mortality and other health outcomes in this cohort will be presented in future publications. Consistent with hip fracture risk, longer duration of cessation of HT was also associated with low BMD. As with all medications, women should discuss the risks and benefits as well as alternative therapies for the prevention of bone loss and bone fracture, especially hip fracture before terminating HT. With approximately 1 million women entering menopause each year in the United States alone, the health consequences of bone fracture may have potentially enormous survival and economic consequences if an effective prevention strategy is not in place.
Acknowledgments
Funding/support: This study was not funded by any source.
Footnotes
Financial disclosure/conflicts of interest: None reported.
References
- 1.Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 2.Buist DS, Newton KM, Miglioretti DL, et al. Hormone therapy prescribing patterns in the United States. Obstet Gynecol. 2004;104:1042–1050. doi: 10.1097/01.AOG.0000143826.38439.af. [DOI] [PubMed] [Google Scholar]
- 3.Parente L, Uyehara C, Larsen W, Whitcomb B, Farley J. Long-term impact of the Women’s Health Initiative on HRT. Arch Gynecol Obstet. 2008;277:219–224. doi: 10.1007/s00404-007-0442-1. [DOI] [PubMed] [Google Scholar]
- 4.Barbaglia G, Macia F, Comas M, et al. Trends in hormone therapy use before and after publication of the Women’s Health Initiative trial: 10 years of follow-up. Menopause. 2009;16:1061–1064. doi: 10.1097/gme.0b013e3181a02b44. [DOI] [PubMed] [Google Scholar]
- 5.Hing E, Brett KM. Changes in U.S. prescribing patterns of menopausal hormone therapy, 2001–2003. Obstet Gynecol. 2006;108:33–40. doi: 10.1097/01.AOG.0000220502.77153.5a. [DOI] [PubMed] [Google Scholar]
- 6.Power ML, Zinberg S, Schulkin J. A survey of obstetrician-gynecologists concerning practice patterns and attitudes toward hormone therapy. Menopause. 2006;13:434–441. doi: 10.1097/01.gme.0000185753.77704.65. [DOI] [PubMed] [Google Scholar]
- 7.Wells G, Little WC. Current treatment and future directions in heart failure. Curr Opin Pharmacol. 2002;2:148–153. doi: 10.1016/s1471-4892(02)00135-2. [DOI] [PubMed] [Google Scholar]
- 8.Gambacciani M, Ciaponi M, Genazzani AR. The HRT misuse and osteoporosis epidemic: a possible future scenario. Climacteric. 2007;10:273–275. doi: 10.1080/13697130701511277. [DOI] [PubMed] [Google Scholar]
- 9.Owen RA, Melton LJ, 3rd, Gallagher JC, Riggs BL. The national cost of acute care of hip fractures associated with osteoporosis. Clin Orthop Relat Res. 1980:172–176. [PubMed] [Google Scholar]
- 10.Dell R, Greene D, Schelkun SR, Williams K. Osteoporosis disease management: the role of the orthopaedic surgeon. J Bone Joint Surg Am. 2008;90:188–194. doi: 10.2106/JBJS.H.00628. [DOI] [PubMed] [Google Scholar]
- 11.Gallagher JC, Rapuri PB, Haynatzki G, Detter JR. Effect of discontinuation of estrogen, calcitriol, and the combination of both on bone density and bone markers. J Clin Endocrinol Metab. 2002;87:4914–4923. doi: 10.1210/jc.2002-020727. [DOI] [PubMed] [Google Scholar]
- 12.Wasnich RD, Bagger YZ, Hosking DJ, et al. Changes in bone density and turnover after alendronate or estrogen withdrawal. Menopause. 2004;11:622–630. doi: 10.1097/01.gme.0000123641.76105.b5. [DOI] [PubMed] [Google Scholar]
- 13.Banks E, Beral V, Reeves G, Balkwill A, Barnes I. Fracture incidence in relation to the pattern of use of hormone therapy in postmenopausal women. JAMA. 2004;291:2212–2220. doi: 10.1001/jama.291.18.2212. [DOI] [PubMed] [Google Scholar]
- 14.Grodstein F, Stampfer MJ, Falkeborn M, Naessen T, Persson I. Post-menopausal hormone therapy and risk of cardiovascular disease and hip fracture in a cohort of Swedish women. Epidemiology. 1999;10:476–480. [PubMed] [Google Scholar]
- 15.Kiel DP, Felson DT, Anderson JJ, Wilson PW, Moskowitz MA. Hip fracture and the use of estrogens in postmenopausal women. The Framingham Study. N Engl J Med. 1987;317:1169–1174. doi: 10.1056/NEJM198711053171901. [DOI] [PubMed] [Google Scholar]
- 16.Cauley JA, Seeley DG, Ensrud K, Ettinger B, Black D, Cummings SR. Estrogen replacement therapy and fractures in older women. Study of Osteoporotic Fractures Research Group. Ann Intern Med. 1995;122:9–16. doi: 10.7326/0003-4819-122-1-199501010-00002. [DOI] [PubMed] [Google Scholar]
- 17.Torgerson DJ, Bell-Syer SE. Hormone replacement therapy and prevention of vertebral fractures: a meta-analysis of randomised trials. BMC Musculoskelet Disord. 2001;2:7. doi: 10.1186/1471-2474-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cauley JA, Robbins J, Chen Z, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA. 2003;290:1729–1738. doi: 10.1001/jama.290.13.1729. [DOI] [PubMed] [Google Scholar]
- 19.Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291:1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 20.Jackson RD, Wactawski-Wende J, LaCroix AZ, et al. Effects of conjugated equine estrogen on risk of fractures and BMD in postmenopausal women with hysterectomy: results from the Women’s Health Initiative randomized trial. J Bone Miner Res. 2006;21:817–828. doi: 10.1359/jbmr.060312. [DOI] [PubMed] [Google Scholar]
- 21.de Jong-van den Berg LT, Faber A, van den Berg PB. HRT use in 2001 and 2004 in the Netherlands—a world of difference. Maturitas. 2006;54:193–197. doi: 10.1016/j.maturitas.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 22.Usher C, Teeling M, Bennett K, Feely J. Effect of clinical trial publicity on HRT prescribing in Ireland. Eur J Clin Pharmacol. 2006;62:307–310. doi: 10.1007/s00228-005-0083-x. [DOI] [PubMed] [Google Scholar]
- 23.Force UPST. Hormone therapy for the prevention of chronic conditions in postmenopausal women: recommendations from the U.S. Preventive Services Task Force. Ann Intern Med. 2005;142:855–860. [PubMed] [Google Scholar]
- 24.Islam S, Liu Q, Chines A, Helzner E. Trend in incidence of osteoporosis-related fractures among 40- to 69-year-old women: analysis of a large insurance claims database, 2000–2005. Menopause. 2009;16:77–83. doi: 10.1097/gme.0b013e31817b816e. [DOI] [PubMed] [Google Scholar]
- 25.Heiss G, Wallace R, Anderson GL, et al. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA. 2008;299:1036–1045. doi: 10.1001/jama.299.9.1036. [DOI] [PubMed] [Google Scholar]
- 26.Gallagher JC, Melton LJ, Riggs BL, Bergstrath E. Epidemiology of fractures of the proximal femur in Rochester, Minnesota. Clin Orthop Relat Res. 1980:163–171. [PubMed] [Google Scholar]
- 27.Haentjens P, Magaziner J, Colon-Emeric CS, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152:380–390. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salpeter SR, Buckley NS, Liu H, Salpeter EE. The cost-effectiveness of hormone therapy in younger and older postmenopausal women. Am J Med. 2009;122:42–52. e42. doi: 10.1016/j.amjmed.2008.07.026. [DOI] [PubMed] [Google Scholar]