Abstract
Exercise is an efficacious treatment for Major Depressive Disorder (MDD) and has independently been shown to have anti-inflammatory effects in non depressed subjects. Patients with MDD have elevated inflammatory cytokines but it is not known if exercise affects inflammation in MDD patients and whether these changes are clinically relevant. In the TReatment with Exercise Augmentation for Depression (TREAD) study, participants who were partial responders to a Selective Serotonin Reuptake Inhibitor (SSRI) were randomized to receive one of two doses of exercise: 16 kilocalories per kilogram of body weight (KKW), or 4 KKW for 12 weeks.
Blood samples were collected before initiation and again at the end of the 12-week exercise intervention. Serum was analyzed using a multiplexed ELISA for Interferon-γ (IFN-γ), Interleukin 1-β (IL-1β), Interleukin-6 (IL-6), and Tumor Necrosis Factor-α (TNF-α).
Higher baseline levels of TNF-α were associated with greater decrease in depression symptoms over the 12 week exercise period (p = 0.0023). In addition, a significant positive correlation between change in IL-1β and change in depression symptom scores was observed (p=0.0441). There were no significant changes in mean level of any cytokine following the 12-week intervention, and no significant relationship between exercise dose and change in mean cytokine level.
Results suggest that high TNF-α may differentially predict better outcomes with exercise treatment as opposed to antidepressant medications for which high TNF-α is linked to poor response. Our results also confirm findings from studies of antidepressant medications that tie decreasing IL-1β to positive depression treatment outcomes.
Keywords: exercise, physical activity, depression, inflammation, cytokines
Introduction
The prevalence of depressive disorders and their associated socioeconomic burden are of growing concern. Evidence suggests that of those receiving adequate medication trials, most will not achieve remission following initial treatment1 and nearly one-third will not achieve remission even following several treatment steps2, 3. The identification of moderators of treatment response is a critical step in the pursuit of developing methods to better match patients with treatments. These moderators could be used to develop new diagnostic methods that subtype patients into groups with differences in underlying pathophysiology as well as for personalizing treatment.
Exercise has been shown to be efficacious as a stand-alone4, 5 and as an augmentation treatment6-8 for MDD. Our recent work identified gender and family history as significant moderators of treatment response for exercise augmentation8. In addition, we examined changes in Brain-Derived Neurotrophic Factor (BDNF) associated with exercise augmentation and found higher levels of BDNF at baseline predicted a significantly greater decrease in depressive symptoms following exercise treatment9. These findings, along with previous research showing that treatment outcome may be based in part on underlying genetic variation10, suggest there may be underlying biological moderators associated with antidepressant response to exercise and support the further identification of biomarkers related to the treatment effect of exercise.
Inflammatory cytokines have potential for biomarker development in MDD. Recent studies have revealed that these markers are elevated in depressed patients when compared to healthy controls. Elevations of Interleukin-6 (IL-6) and Tumor Necrosis Factor α (TNF-α) have been confirmed in a meta-analysis11. In addition, antidepressant treatment, particularly with SSRIs, has been shown to decrease some MDD associated cytokine elevations. In a recent meta-analysis17 findings confirmed that levels of inflammatory cytokines Interleukin 1-β (IL-1β)12, 13, IL-614, 15, and TNF-α15, 16 are reduced following treatment with SSRIs. Studies have also shown that elevated baseline TNF-α and IL-6 correlate with treatment failure of SSRIs17, 18. In studies of healthy controls and subjects with medical illness, exercise interventions reduced levels of IL-6, TNF-α, and Interferon γ (IFN-γ)19-21. To our knowledge, no study has evaluated the relationship between exercise and inflammatory markers in a depressed sample.
In the TReatment with Exercise Augmentation for Depression (TREAD) study, adults with MDD who failed to remit with an adequate trial of a single SSRI were treated with an exercise augmentation regimen. Subjects provided blood samples for analysis of inflammatory markers at baseline and at the end of treatment.
This report examines the extent to which inflammatory markers (IL-1β, IL-6, TNF-α, IFN-γ) can be used to predict response to exercise treatment after an incomplete response to an SSRI. It also examines how the inflammatory markers change with exercise and if those changes are associated with dose of exercise or changes in symptom severity.
Materials and Methods
Details of the design and outcomes of the TREAD study have been published previously8, 22, 23.
Participants
TREAD recruited adults, age 18-70, with MDD, who were currently taking an adequate dose of a single SSRI but were non-responders as defined by a score of ≥ 14 on the 17- item Hamilton Rating Scale of Depression (HRSD17), following >6 weeks and <6 months of treatment. Participants were excluded for presence of psychosis or if they regularly engaged in physical activity.
Intervention
Participants were randomly assigned to one of two exercise dose groups: the low dose group had a target energy expenditure of 4 kilocalories per kilogram of body weight per week (KKW) and the high dose group 16 KKW over 12 weeks. The high dose was designed to meet or exceed current physical activity guidelines for public health from federal agencies and professional associations24, 25. Participants engaged in aerobic exercise (treadmill, cycle ergometers or a combination) at self-selected exercise intensity. The exercise dose was completed in a combination of supervised and home-based sessions, and participants logged actual activity using a web based system.
Assessments
Self-report and clinician-rated measures were collected prior to the first exercise session of each week. Trained personnel blinded to group assignment completed clinician-rated assessments. The primary outcome assessment was the 30-item clinician-rated Inventory of Depressive Symptomatology (IDS-C30)26-28; additional assessments of depressive symptoms included the 30-item self-rated Inventory of Depressive Symptomatology (IDS-SR30)26-28 and the (HRSD17)29.
Sample Collection and Analysis
Of the 126 randomized TREAD participants, 108 signed additional consent for blood analysis at baseline (105 samples were available); 73 of these completed the study and provided week 12 samples. Resting blood samples were collected at baseline and following the 12-week intervention. All samples were drawn in the morning; participants fasted a minimum of 3 hours prior to blood draw, and were at least 24 hours from the last exercise session. Ten ml of peripheral venous blood was drawn and centrifuged at 900rpm for ten minutes at room temperature to separate the blood components. Serum was subsequently frozen at −80°C until the time of analysis. We analyzed samples in duplicate using a multiplexed chemo-iluminesce ELISA method (MesoScale Discovery, Gaithersburg, MD) for IFN-γ, IL-1β, IL-6, and TNF-α. The plates were read using the MSD Discovery Workbench analyzer and software package (MesoScale Discovery). All data were calibrated using standard curves generated for each cytokine.
Statistical Analysis
Demographic and clinical characteristics for the evaluable sample and for both dose groups were described using the sample mean and standard deviation for continuous variables and the frequency and percentage for categorical variables. We compared variables across dose groups using independent sample t-tests (for continuous variables) correcting for unequal variances with the Satterthwaite method as needed, or Chi-square tests (for categorical variables).
We used a linear mixed model repeated measures analysis to examine the relationship between each baseline cytokine level and treatment outcome on the IDS-C over the 12-week study period. Each model contained fixed effects terms for baseline cytokine level (pg/mL), time, and cytokine level by time interaction. The intercept was included as a random effect. Time was log transformed to provide a more linear relationship with outcome. Restricted maximum likelihood estimation and Type 3 tests of fixed effects were used, with the Kenward-Roger correction30 applied to the spatial power covariance structure. The parameter estimate was interpreted from the solution for fixed effects in the mixed model analysis. The following covariates were included in the mixed model: Baseline IDS-C, Family History of MDD, Recurrent MDD, Gender, Age, Race, BMI, SF36 Mental, and SF36 Physical. Covariates and baseline cytokine level were centered.
We conducted a non-parametric analysis to determine the relationship between change in each cytokine and change in symptom severity. Specifically, Spearman’s rank-order correlation coefficient (rs) was used to examine the relationship between change in each inflammatory cytokine and change in depression severity on the HRSD17, IDS-C30, and IDS-SR30, for all participants who completed the study (N=73) and separately within each dose group.
We computed the mean level of each cytokine at baseline and week 12, and compared the mean change using the Wilcoxon Signed-Rank test for all participants who had a week 12 sample, and separately within the 16 KKW and 4 KKW dose-exercise groups. In order to determine the effect of exercise dose on change in cytokine level over the study period, we performed an Analysis of Covariance (ANCOVA) on each cytokine level at week 12, while controlling for baseline cytokine level, BMI, and the physical subscale of the SF-36.
The current study examines four inflammatory markers as potential mediators and moderators of treatment response. Since we are examining a limited number of markers that have been potentially shown to be associated with antidepressant treatment response, all tests were conducted as two-tailed at the p < 0.05 and not corrected for multiple comparisons, as emphasized by Lazzeroni & Ray31, Bender & Lange32, and Rothman33. All analyses were carried out using SAS software, version 9.2 (SAS Institute, Inc., Cary, North Carolina, USA).
Results
Participant Characteristics
A total of 105 baseline samples were available and analysed by cytokine assay. One baseline value for TNF-α and two baseline values for IFN-γ were greater than five standard deviations above the sample mean and thus excluded from further analysis. Two participants had missing baseline values for IL-1β and were also excluded. An additional participant sample had no value for 12 week IL-1β – this participant was included in the mixed model but excluded from the correlation analysis. Tables 1 and 2 show the number of participants who were included in each analysis.
Table 1.
Baseline Demographic and Clinical Characteristics for Total Sample
| Variable | All N | M(SD) | 16 KK W n |
M(SD) | 4 KKW n |
M(SD) |
t -test or χ2 |
p-valuea |
|---|---|---|---|---|---|---|---|---|
| Age (years) | 105 | 47.51 (9.44) | 53 | 45.83 (9.54) | 52 | 49.23 (9.11) | 1.87 | 0.06 |
| Female (%) | 105 | 80 | 53 | 84.91 | 52 | 75 | 1.61 | 0.20 |
| IDS-C | 105 | 34.14 (7.25) | 53 | 33.15 (6.49) | 52 | 35.15 (7.88) | 1.42 | 0.16 |
| IDS-SR | 101 | 32.66 (9.38) | 50 | 31.68 (7.84) | 51 | 33.62 (10.67) | 1.05 | 0.30 |
| HRSD | 105 | 18.10 (3.86) | 53 | 17.79 (3.80) | 52 | 18.42 (3.94) | 0.83 | 0.41 |
| IFN-γ | 103 | 1.33 (1.11) | 52 | 1.21 (0.71) | 51 | 1.45 (1.39) | 1.09 | 0.28 |
| IL-1β | 103 | 0.10 (0.06) | 52 | 0.09 (0.07 | 51 | 0.10 (0.06) | 0.69 | 0.49 |
| IL-6 | 105 | 0.88 (0.68) | 53 | 0.89 (0.67) | 52 | 0.88 (0.69) | 0.04 | 0.97 |
| TNF-α | 104 | 5.75 (1.67) | 53 | 5.31 (1.58) | 51 | 6.20 (1.70) | 2.76 | 0.01 |
| BMI | 105 | 30.89 (6.31) | 53 | 30.36 (6.99) | 52 | 31.44 (5.55) | 0.87 | 0.39 |
| SF-36 Physical Health |
101 | 80.18 (20.79) | 50 | 80.60 (19.83) | 51 | 79.77 (21.88) | 0.2 | 0.84 |
| Recurrent MDD (%) | 105 | 67.62 | 53 | 67.92 | 52 | 71.15 | 0.13 | 0.72 |
| Family History of MDD (%) |
105 | 67.62 | 53 | 67.92 | 52 | 67.31 | 0.004 | 0.95 |
| Length of Illness (years) |
104 | 20.19 (12.12) | 52 | 18.31 (11.17) | 52 | 22.07 (12.82) | 1.6 | 0.11 |
| Length of Current MDD Episode (years) |
105 | 7.09 (8.28) | 53 | 6.21 (7.81) | 52 | 7.99 (8.73) | 1.1 | 0.28 |
Tested for differences between 16 KKW and 4 KKW exercise groups on each demographic/clinical characteristic in a separate model.
The two-independent sample t-test (for continuous outcomes), with Satterthwaite method for unequal variances was used when appropriate.
Note. Mean=sample mean; SD=standard deviation; N=total sample size of all completers; n=sample size per group; each cytokine was measured in pg/mL; KKW=Kilocalories per Kilogram per Week; IDS-C=Inventory of Depressive Symptoms - Clinician Rated; Inventory of Depressive Symptoms - Self-Rated; HRSD=Hamilton Rating Scale for Depression; MDD=Major Depressive Disorder
Table 2.
Spearman correlation coefficients (rs) between the change in each inflammatory cytokine level and change in depression severity for all completers and within each dose-exercise group
| Change in Depression Severity |
Group | n | rs | p-value | n | rs | p-value | n | rs | p-value | n | rs | p-value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| INF-γ | IL1-β | IL-6 | TNF-α | ||||||||||
| HRSD | ALL | 71 | 0.02 | 0.89 | 69 | 0.24 | 0.05 | 72 | 0.22 | 0.07 | 71 | −0.01 | 0.95 |
|
|
|||||||||||||
| 4 KKW | 39 | −0.12 | 0.45 | 38 | 0.13 | 0.42 | 39 | 0.23 | 0.15 | 38 | −0.18 | 0.29 | |
| 16 KKW | 32 | 0.21 | 0.24 | 31 | 0.38 | 0.04 | 33 | 0.17 | 0.35 | 33 | 0.19 | 0.29 | |
|
| |||||||||||||
| IDS-C | ALL | 70 | −0.04 | 0.75 | 68 | 0.24 | 0.04 | 71 | 0.20 | 0.09 | 70 | 0.05 | 0.69 |
|
|
|||||||||||||
| 4 KKW | 39 | −0.19 | 0.25 | 38 | 0.20 | 0.23 | 39 | 0.23 | 0.16 | 38 | −0.04 | 0.83 | |
| 16 KKW | 31 | 0.12 | 0.52 | 30 | 0.29 | 0.12 | 32 | 0.15 | 0.41 | 32 | 0.09 | 0.62 | |
|
| |||||||||||||
| IDS-SR | ALL | 69 | −0.10 | 0.42 | 68 | 0.24 | 0.05 | 70 | 0.02 | 0.90 | 69 | −0.11 | 0.38 |
|
|
|||||||||||||
| 4 KKW | 38 | −0.25 | 0.13 | 37 | 0.16 | 0.35 | 38 | 0.13 | 0.44 | 37 | −0.15 | 0.37 | |
| 16 KKW | 31 | 0.07 | 0.70 | 31 | 0.36 | 0.05 | 32 | −0.03 | 0.25 | 32 | −0.10 | 0.60 | |
Note: Change was operationally defined as week 12 cytokine level minus baseline cytokine level.
Note. KKW=Kilocalories per Kilogram per Week; IDS-C=Inventory of Depressive Symptoms - Clinician Rated; Inventory of Depressive Symptoms - Self-Rated; HRSD=Hamilton Rating Scale for Depression
Participants’ baseline demographic and clinical characteristics as well as mean baseline cytokine levels for all participants and for each exercise dose group are reported in Table 1. The sub-sample of those who completed the study did not differ in any demographic or clinical variable from the entire sample.
Effect of Baseline Cytokine Level on Depression Symptom Improvement
The linear mixed model repeated measures analyses revealed a significant two-way TNF-α × time interaction (parameter estimate = −0.6155, p=0.0023) on the primary outcome of IDS-C total, indicating that higher levels of baseline TNF-α were related to a greater decrease in IDS-C total scores over the course of the 12-week study. The pattern of this relationship is graphically depicted in Figure 1, which presents adjusted Least Squares Means for IDS-C Total by Week for those above (>) and below (≤) the median baseline TNF-α value of 5.493 pg/mL. Separate linear mixed model repeated measures analyses showed no significant 3-way (cytokine × group × time) interactions, indicating dose of exercise did not affect this relationship (results not shown). No other baseline cytokine affected treatment outcome in our analysis.
Figure 1.
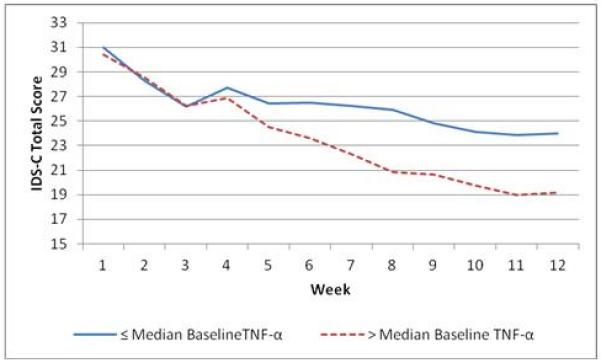
Plot of adjusted Least Squares Means* for IDS-C Total by Week for those above (>) and below (≤) the median baseline TNF-α value of 5.493 pg/mL.
*Least Squares Means were adjusted for Baseline IDS-C, Family History of MDD, Recurrent MDD, Gender, Race, BMI, SF36 Mental, and SF36 Physical and Age.
Correlation between Change in Cytokine Level and Depression Symptoms
Spearman correlation coefficients between the change in each inflammatory cytokine level and change in depression severity for all completers and within each dose group are shown in Table 2. The Spearman correlations for all completers revealed a significant positive relationship between change in IL-1β and change in IDS-C30 (rs = 0.24, p<0.05), change in HRSD17 (rs = 0.2415, p<0.05), and change in IDS-SR30 (rs = 0.2417, p=0.0470). Significant associations were also observed in the high dose exercise group, with significant positive relationships between change in IL-1β and change in HRSD17 (rs = 0.38, p<0.04) as well as change in IDS-SR (rs = 0.36, p<0.05), respectively. Correlations between change in depression severity and change in other cytokines were not significant (Table 2).
Change in Cytokine Level
Mean inflammatory cytokine levels at baseline and week 12, as well as change in the means for all completers and by dose group, are reported in Table 3. There was no significant change in any of the mean cytokine levels over the study period in the entire sample or within either exercise-dose group.
Table 3.
Change in mean and median inflammatory cytokine levels for all completers and within each dose-exercise group from baseline to week 12
| Baseline | Week 12 | Δ M | p-valuea | ||
|---|---|---|---|---|---|
| n | M(SD) | M(SD) | M(SD) | Signed Rank | |
|
| |||||
| Group | IFN-γ | ||||
| All Completers | 72 | 1.36(1.21) | 1.45 (1.16) | 0.09 (0.93) | 0.32 |
| 4 KKW | 40 | 1.54(1.55) | 1.60 (1.49) | 0.06 (1.15) | 0.96 |
| 16 KKW | 32 | 1.13 (0.43) | 1.25 (0.45) | 0.12 (0.56) | 0.13 |
|
| |||||
| Group | IL-1β | ||||
|
| |||||
| All Completers | 70 | 0.10 (0.07) | 0.13 (0.27) | 0.03 (0.28) | 0.38 |
| 4 KKW | 39 | 0.10 (0.06) | 0.11 (0.06) | 0.01 (0.07) | 0.77 |
| 16 KKW | 31 | 0.09 (0.08) | 0.16 (0.41) | 0.07 (0.42) | 0.2 |
|
| |||||
| Group | IL-6 | ||||
|
| |||||
| All Completers | 73 | 0.89 (0.77 ) | 0.77 (0.52) | −0.12 (0.79) | 0.57 |
| 4 KKW | 40 | 0.87 (0.75) | 0.79 (0.56) | −0.08 (0.79) | 0.88 |
| 16 KKW | 33 | 0.91 (0.79) | 0.74 (0.46) | −0.17 (0.81) | 0.52 |
|
| |||||
| Group | IL-6 | ||||
|
| |||||
| All Completers | 72 | 5.77 (1.74) | 5.60 (1.67) | −0.17 (0.97) | 0.19 |
| 4 KKW | 39 | 6.18 (1.75) | 5.86 (1.67) | −0.32 (1.06) | 0.14 |
| 16 KKW | 33 | 5.28 (1.62) | 5.29 (1.64) | 0.01 (0.83) | 0.91 |
Note. M =Sample Mean; SD =Standard Devation; ΔM = Mean change in cytokine level; KKW = Kilocalories per Kilogram per Week
Note. Each cytokine was measured in pg/mL.
Note. p value = Wilcoxon signed ranked test was used to test for differences in sample
p-value from Wilcoxon signed rank test (two-tailed) for test of Mean change.
Exercise Group Effect on Cytokine Level
The ANCOVA of each inflammatory cytokine outcome, controlling for baseline cytokine level, BMI, and SF-36 physical health, revealed no significant exercise group differences in any of the individual cytokine mean values at week 12 (p’s > 0.37) (Table 4). We carried out similar ANCOVA models with baseline IDS-C, age, gender, years of illness, and length of current MDD episode (years) included as covariates in the model, but the basic results did not differ from those mentioned above (results not reported).
Table 4.
ANCOVA results for exercise group effect on each inflammatory cytokine at week 12
| IFN-γ | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Exercise Group | n | M | SE | 95% CI for M | F | p-value |
| Week 12 | 0.39 | 0.54 | ||||
| 4 KKW | 40 | 1.51 | 0.14 | 1.24 to 1.78 | ||
| 16 KKW | 32 | 1.38 | 0.15 | 1.07 to 1.68 | ||
|
| ||||||
| IL-1β | ||||||
|
| ||||||
| Exercise Group | n | M | SE | 95% CI for M | F | p-value |
|
| ||||||
| Week 12 | 0.79 | 0.38 | ||||
| 4 KKW | 39 | 0.11 | 0.05 | 0.02 to 0.2 | ||
| 16 KKW | 31 | 0.17 | 0.05 | 0.07 to 0.27 | ||
|
| ||||||
| IL-6 | ||||||
|
| ||||||
| Exercise Group | n | M | SE | 95% CI for M | F | p-value |
|
| ||||||
| Week 12 | 0.20 | 0.66 | ||||
| 4 KKW | 40 | 0.75 | 0.07 | 0.62 to 0.88 | ||
| 16 KKW | 33 | 0.79 | 0.07 | 0.65 to 0.94 | ||
|
| ||||||
| TNF-α | ||||||
|
| ||||||
| Exercise Group | n | M | SE | 95% CI for M | F | p-value |
|
| ||||||
| Week 12 | 0.74 | 0.39 | ||||
| 4 KKW | 39 | 5.51 | 0.15 | 5.21 to 5.81 | ||
| 16 KKW | 33 | 5.71 | 0.17 | 5.38 to 6.04 | ||
Note. M = Least Squares Mean; SE = Standard Error; 95% CI = 95% Confidence Interval for the expected mean value; n = sample size per group; KKW = Kilocalories per Kilogram per Week. Each cytokine was measured in pg/mL. F statistic was used to test for mean cytokine level difference between the two Dose-Exercise Groups at week 12 while controlling for baseline cytokine level, BMI, SF-36 Physical Health. Least squares means at week 12 were adjusted for respective baseline cytokine level, BMI, and SF-36 Physical Health.
Discussion
Our analysis provides evidence that inflammatory cytokines may be useful biomarkers of the antidepressant action of exercise. We found that TNF-α level at baseline functioned as a predictor of treatment outcome, with higher TNF-α associated with more rapid improvement on the IDS-C. Additionally, we found a significant positive correlation between changes in IL-1β and depressive symptoms on all three symptom measures used in TREAD, such that participants who experienced larger drops in IL-1β level also had larger decreases in symptom scores. This relationship maintained significance in the higher dose 16 KKW subgroup, but not in the lower dose 4 KKW subgroup, indicating a dose response relationship. Contrary to our initial assumption, we did not find that exercise augmentation treatment lowered mean cytokine levels or that a higher dose of exercise had a stronger effect on mean cytokine levels.
Interestingly, our finding associating higher baseline TNF-α with a more rapid drop in depressive symptom severity over the course of the 12-week study is in contrast to several studies examining medication treatment. Eller et al.17 found higher baseline levels of TNF-α were associated with non-response to an SSRI, while Lanquillon et al.18 found no moderating effect of baseline levels of TNF-α on antidepressant response. The Hannestad et al. meta-analysis34 also supports the association between higher baseline TNF-α and treatment resistance with medication. These findings suggest that TNF-α may be a differential moderator between SSRI and exercise treatment. Although further work clarifying this effect is needed, we hypothesize that since the TREAD sample was comprised of MDD patients who had an inadequate response to an SSRI, it likely contained a subset of patients with high TNF-α who presumably failed SSRIs directly or indirectly because of this elevation. We can postulate that exercise successfully treated this subset, whereas the rest of our sample may have failed initial SSRI treatment due to other, unknown, reasons, which may or may not have responded to exercise. Taken together with our previous findings of a moderating effect of BDNF on treatment outcome with exercise, these results provide an attractive model to test in future prospective randomized comparisons of exercise and SSRI in order to develop a personalized treatment approach. If the finding that exercise treatment is superior to antidepressant medication for those with high TNF-α is confirmed, it would be significant since TNF-α level could be used to recommend exercise rather than medication as part of a personalized treatment algorithm.
Our finding that a change in IL-1β correlates with change in symptom severity, on the other hand, is consistent with a growing body of research on cytokines and SSRI treatment. For example, Song et al.35 found that responders to SSRI treatment had lower end treatment IL-1β than non-responders. The recent meta-analysis by Hannestad et al.34 also found reductions in IL-1β correlate with better outcome with SSRIs. Our finding is significant, however, in that it is the first replication of this relationship in a sample treated with exercise. We also found significant correlations between change in IL-1β and change in depressive symptom severity in the 16 KKW group but not in the 4 KKW group. This suggests a dose-response effect on IL-1β might have been found in a larger or better characterized (i.e. for inflammatory abnormalities) sample. Since animal studies have shown that IL-1β down regulates hippocampal neurogenesis36 there is theory to support the importance of IL-1β in the pathophysiology of at least some cases of depression. All of these results suggest that IL-1β should be a focus of future clinical trials aimed at identifying and treating depression associated with inflammation.
We did not find that exercise augmentation treatment lowered mean cytokine levels or that a higher dose of exercise had a stronger effect on mean cytokine levels. This finding is in disagreement with both studies of exercise in healthy and medically ill samples, and with studies of SSRI treatment in depressed samples. Similarly, we failed to find a dose effect on cytokine change. It is probable that pretreatment with SSRIs in this sample obscured our ability to detect change in cytokine levels, since SSRIs are known to lower cytokines. Similarly, SSRI pretreatment likely reduced baseline depressive symptoms in our sample. Future research examining the effect of exercise on inflammatory cytokines in treatment-naïve patients would provide the information necessary for comparison to previous SSRI trials. The severity of depression at baseline in this study’s population appears to be intermediate between that of effectiveness augmentation trials such as STAR*D37 and that of efficacy augmentation trials such as ADAPT-A38 and this may have had an impact on the levels of cytokines reported. In addition, there are other factors that may have confounded our results, including the age distribution of participants – although we attempted to address these by adjusting our model, future studies prospectively accounting for sample characteristics are desirable.
While it is clear that there is a substantial relationship between inflammation and depression, several mechanisms appear to be involved and may play different roles across patients39. These include inflammatory disruption of synthesis, reuptake and metabolism of neurotransmitters40, alteration of hypothalamic-pituitary-adrenal (HPA) axis function41, and decrease in hippocampal neurogenesis36. Not only has exercise been shown to be broadly anti-inflammatory, but it has been specifically demonstrated to act on each of these pathways to reverse the effects of inflammation42. Any or all of these mechanisms could be involved in the efficacy of exercise as a treatment of MDD, and future studies better characterizing baseline inflammation and its change over the course of exercise treatment may elucidate which mechanisms are most important in clinical recovery.
Broadly, our results suggest that exercise may be an effective treatment strategy within specific subpopulations of those with MDD. For example, chronic elevation of inflammatory markers is associated with metabolic syndrome and insulin resistance43, syndromes which, in turn, may be associated with treatment-resistant depression44. Given that exercise typically reduces inflammation45, normalizes insulin resistance46, 47, and improves several characteristics of metabolic syndrome48-50, it is plausible that exercise may be especially effective as a stand alone or augmentative treatment for MDD in patients with comorbid metabolic syndrome, diabetes, and other inflammatory conditions.
Acknowledgements
The authors thank the following individuals for their contributions to this project: Several persons assisted with trial implementation, including Tyson M. Bain, MS; Heather O. Chambliss, PhD, FACSM; Alexander N. Jordan, MS; Heather Kitzman-Ulrich, PhD; Jennifer Kupper, MS; Lucille Marcoux, ANP, MSN, RN; Erin L. Sinclair, MA, LPC (all affiliated with The Cooper Institute, Dallas, Texas, at the time of their participation); Ella Daly, MB, MRCPsych (Dr. Daly is currently a full-time employee of Johnson & Johnson Pharmaceutical Research & Development and completed work on this study while she was on the faculty at The University of Texas Southwestern Medical Center at Dallas); Mariam Andersen, MA; Shailesh Jain, MD, MPH; Beverly Kleiber, PhD; David W. Morris, PhD; Anne Marie Jones, MS; and Michelle Rivas, MS, CCRC (all affiliated with The University of Texas Southwestern Medical Center at Dallas at the time of their participation). For assistance with database management, we thank Bradley Witte, BS (The University of Texas Southwestern Medical Center at Dallas), and Beth Wright, MS; Carrie E. Finley, MS; Mei Sui, MD, MPH; and Carolyn E. Barlow, MS (all affiliated with The Cooper Institute, Dallas, Texas). For assistance with statistical analyses (development of moderator selection methodology), we thank Richard M. Golden, PhD, MSEE, BSEE (University of Texas at Dallas) and T. Michael Kashner, PhD, JD, MPH (The University of Texas Southwestern Medical Center at Dallas). We thank A. John Rush, MD, for providing comments on the study design (Dr. Rush was affiliated with The University of Texas Southwestern Medical Center at Dallas at the time of his contribution to the study; he has received consulting fees from the University of Michigan and Brain Resource; has received speaker fees from Otsuka Pharmaceuticals; has received author royalties from Guilford Publications and The University of Texas Southwestern Medical Center at Dallas; and has received research support from the National Institute of Mental Health). We are very grateful to all of the study participants who contributed to this project. We also thank Eric Nestler, MD, PhD, and Carol A. Tamminga, MD, both of the Department of Psychiatry, The University of Texas Southwestern Medical Center, Dallas, for administrative support. None of the acknowledged individuals have potential conflicts of interests or disclosures to report except as noted above.
TREAD support: TREAD was supported by NIMH grant #5-R01-MH067692 (PI: Dr. Trivedi) and by a NARSAD Independent Investigator Award (PI: Dr. Trivedi). Funding for the BDNF ELISAs was provided by the Sara M and Charles E Seay Center for Basic and Applied Research. Neither NIMH, NARSAD, nor the Seay Center had further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Conflict of Interest Chad D. Rethorst does not have any disclosures to report.
Marisa S. Toups does not have any disclosures to report.
Tracy L. Greer has received research funding from NARSAD.
Thomas J. Carmody has received a consulting fee from Cyberonics, Inc.
Bruce D. Grannemann does not have any disclosures to report.
Paul A. Nakonezny does not have any disclosures to report.
Ryan M. Huebinger does not have any disclosures to report.
Robert C. Barber does not have any disclosures to report.
Madhukar H. Trivedi has received research support from the Agency for Healthcare Research and Quality (AHRQ), Corcept Therapeutics, Inc., Cyberonics, Inc., Merck, National Alliance for Research in Schizophrenia and Depression, National Institute of Mental Health, National Institute on Drug Abuse, Naurex, Novartis, Pharmacia & Upjohn, Predix Pharmaceuticals (Epix), Solvay Pharmaceuticals, Inc., Targacept, and Valient. He has received consulting and speaker fees from Abbott Laboratories, Inc., Abdi Ibrahim, Akzo (Organon Pharmaceuticals Inc.), Alkermes, AstraZeneca, Axon Advisors, Bristol-Myers Squibb Company, Cephalon, Inc., Evotec, Fabre Kramer Pharmaceuticals, Inc., Forest Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica Products, Johnson & Johnson PRD, Libby, LP, Eli Lilly & Company, Lundbeck, Meade Johnson, MedAvante, Medtronic, Neuronetics, Otsuka Pharmaceuticals, Pamlab, Parke-Davis Pharmaceuticals, Inc., Pfizer Inc., PgxHealth, Rexahn Pharmaceuticals, Sepracor, SHIRE Development, Sierra, Takeda,Tal Medical/Puretech, Transcept, VantagePoint, and Wyeth-Ayerst Laboratories.
References
- 1.Trivedi M, Rush A, Wisniewski S, Nierenberg A, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR* D: implications for clinical practice. American Journal of Psychiatry. 2006;163(1):28. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 2.Rush A, Trivedi M, Wisniewski S, Nierenberg A, Stewart J, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR* D report. American Journal of Psychiatry. 2006;163(11):1905. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- 3.Rush A, Trivedi M, Wisniewski S, Stewart J, Nierenberg A, Thase M, et al. Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. New England Journal of Medicine. 2006;354(12):1231. doi: 10.1056/NEJMoa052963. [DOI] [PubMed] [Google Scholar]
- 4.Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression. Am J Prev Med. 2005;28(1):1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Rethorst CD, Wipfli BM, Landers DM. The antidepressive effects of exercise: A meta-analysis of randomized trials. Sports Medicine. 2009;39:21. doi: 10.2165/00007256-200939060-00004. [DOI] [PubMed] [Google Scholar]
- 6.Blumenthal JA, Babyak MA, Doraiswamy PM, Watkins L, Hoffman BM, Barbour KA, et al. Exercise and pharmacotherapy in the treatment of Major Depressive Disorder. Psychosomatic Medicine. 2007;69(7):587–596. doi: 10.1097/PSY.0b013e318148c19a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mather AS, Rodriguez C, Guthrie MF, McHarg AM, Reid IC, McMurdo ME. Effects of exercise on depressive symptoms in older adults with poorly responsive depressive disorder: randomised controlled trial. British Journal of Psychiatry. 2002;180:411. doi: 10.1192/bjp.180.5.411. [DOI] [PubMed] [Google Scholar]
- 8.Trivedi MH, Greer TL, Church TS, Carmody TJ, Grannemann BD, Galper DI, et al. Exercise as an augmentation treatment for nonremitted major depressive disorder: a randomized, parallel dose comparison. Journal of Clinical Psychiatry. 2011;72(5):677. doi: 10.4088/JCP.10m06743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toups MS, Greer TL, Kurian BT, Grannemann BD, Carmody TJ, Huebinger R, et al. Effects of serum Brain Derived Neurotrophic Factor on exercise augmentation treatment of depression. J Psychiatr Res. 2011 doi: 10.1016/j.jpsychires.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rethorst CD, Landers DM, Nagoshi CT, Ross JT. Efficacy of exercise in reducing depressive symptoms across 5-HTTLPR genotypes. Med Sci Sports Exerc. 2010;42(11):2141–2147. doi: 10.1249/MSS.0b013e3181de7d51. [DOI] [PubMed] [Google Scholar]
- 11.Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67(5):446–457. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 12.Leo R, Di Lorenzo G, Tesauro M, Razzini C, Forleo GB, Chiricolo G, et al. Association between enhanced soluble CD40 ligand and proinflammatory and prothrombotic states in major depressive disorder: pilot observations on the effects of selective serotonin reuptake inhibitor therapy. Journal of Clinical Psychiatry. 2006;67(11):1760–1766. doi: 10.4088/jcp.v67n1114. [DOI] [PubMed] [Google Scholar]
- 13.Kagaya A, Kugaya A, Takebayashi M, Fukue-Saeki M, Saeki T, Yamawaki S, et al. Plasma concentrations of interleukin-1beta, interleukin-6, soluble interleukin-2 receptor and tumor necrosis factor alpha of depressed patients in Japan. Neuropsychobiology. 2001;43(2):59. doi: 10.1159/000054867. [DOI] [PubMed] [Google Scholar]
- 14.Basterzi AD, Aydemir C, Kisa C, Aksaray S, Tuzer V, Yazici K, et al. IL-6 levels decrease with SSRI treatment in patients with major depression. Hum Psychopharmacol. 2005;20(7):473–476. doi: 10.1002/hup.717. [DOI] [PubMed] [Google Scholar]
- 15.Yoshimura R, Hori H, Ikenouchi-Sugita A, Umene-Nakano W, Ueda N, Nakamura J. Higher plasma interleukin-6 (IL-6) level is associated with SSRI- or SNRI-refractory depression. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(4):722–726. doi: 10.1016/j.pnpbp.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 16.Tuglu C, Kara SH, Caliyurt O, Vardar E, Abay E. Increased serum tumor necrosis factor-alpha levels and treatment response in major depressive disorder. Psychopharmacology. 2003;170(4):429–433. doi: 10.1007/s00213-003-1566-z. [DOI] [PubMed] [Google Scholar]
- 17.Eller T, Vasar V, Shlik J, Maron E. Pro-inflammatory cytokines and treatment response to escitalopram in major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(2):445–450. doi: 10.1016/j.pnpbp.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 18.Lanquillon S, Krieg JC, Bening-Abu-Shach U, Vedder H. Cytokine production and treatment response in major depressive disorder. Neuropsychopharmacology. 2000;22(4):370–379. doi: 10.1016/S0893-133X(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 19.Kohut M, McCann D, Russell D, Konopka D, Cunnick J, Franke W, et al. Aerobic exercise, but not flexibility/resistance exercise, reduces serum IL-18, CRP, and IL-6 independent of beta-blockers, BMI, and psychosocial factors in older adults. Brain, Behavior, and Immunity. 2006;20(3):201. doi: 10.1016/j.bbi.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Goldhammer E, Tanchilevitch A, Maor I, Beniamini Y, Rosenschein U, Sagiv M. Exercise training modulates cytokines activity in coronary heart disease patients. International Journal of Cardiology. 2005;100(1):93. doi: 10.1016/j.ijcard.2004.08.073. [DOI] [PubMed] [Google Scholar]
- 21.Smith J, Dykes R, Douglas J, Krishnaswamy G, Berk S. Long-term exercise and atherogenic activity of blood mononuclear cells in persons at risk of developing ischemic heart disease. JAMA. 1999;281(18):1722. doi: 10.1001/jama.281.18.1722. [DOI] [PubMed] [Google Scholar]
- 22.Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28(1):1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 23.Trivedi MH, Greer TL, Grannemann BD, Church TS, Galper DI, Sunderajan P, et al. TREAD: TReatment with Exercise Augmentation for Depression: study rationale and design. Clinical Trials. 2006;3(3):291. doi: 10.1191/1740774506cn151oa. [DOI] [PubMed] [Google Scholar]
- 24.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 25.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 26.Rush AJ, Carmody TJ, Reimitz PE. The Inventory of Depressive Symptomatology (IDS): Clinician (IDS C) and Self Report (IDS SR) ratings of depressive symptoms. International Journal of Methods in Psychiatric Research. 2000;9(2):45–59. [Google Scholar]
- 27.Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 28.Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, et al. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychological Medicine. 2004;34(01):73–82. doi: 10.1017/s0033291703001107. [DOI] [PubMed] [Google Scholar]
- 29.Hamilton M. A rating scale for depression. Journal of neurology, neurosurgery, and psychiatry. 1960;23(1):56. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kenward MGRJ. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53(3):983–997. [PubMed] [Google Scholar]
- 31.Lazzeroni LC, Ray A. The cost of large numbers of hypothesis tests on power, effect size and sample size. Mol Psychiatry. 2012;17(1):108–114. doi: 10.1038/mp.2010.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bender R, Lange S. Adjusting for multiple testing--when and how? J Clin Epidemiol. 2001;54(4):343–349. doi: 10.1016/s0895-4356(00)00314-0. [DOI] [PubMed] [Google Scholar]
- 33.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46. [PubMed] [Google Scholar]
- 34.Hannestad J, DellaGioia N, Bloch M. The effect of antidepressant medication treatment on serum levels of inflammatory cytokines: A meta-analysis. Neuropsychopharmacology. 2011 doi: 10.1038/npp.2011.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Song C, Halbreich U, Han C, Leonard B, Luo H. Imbalance between pro-and anti-inflammatory cytokines, and between Th1 and Th2 cytokines in depressed patients: the effect of electroacupuncture or fluoxetine treatment. Pharmacopsychiatry. 2009;42(5):182. doi: 10.1055/s-0029-1202263. [DOI] [PubMed] [Google Scholar]
- 36.Zunszain PA, Anacker C, Cattaneo A, Choudhury S, Musaelyan K, Myint AM, et al. Interleukin-1beta: A New Regulator of the Kynurenine Pathway Affecting Human Hippocampal Neurogenesis. Neuropsychopharmacology. 2011 doi: 10.1038/npp.2011.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trivedi MH, Fava M, Wisniewski SR, Thase ME, Quitkin F, Warden D, Ritz L, Nierenberg AA, Lebowitz BD, Biggs MM, Luther JF, Shores-Wilson K, Rush AJ, STAR*D Study Team Medication augmentation after the failure of SSRIs for depression. N Engl J Med. 2006;354(12):1243–52. doi: 10.1056/NEJMoa052964. [DOI] [PubMed] [Google Scholar]
- 38.Fava M, Mischoulon D, Iosifescu D, Witte J, Pencina M, Flynn M, Harper L, Levy M, Rickels K, Pollack M. A double-blind, placebo-controlled study of aripiprazole adjunctive to antidepressant therapy among depressed outpatients with inadequate response to prior antidepressant therapy (ADAPT-A Study) Psychother Psychosom. 2012;81(2):87–97. doi: 10.1159/000332050. [DOI] [PubMed] [Google Scholar]
- 39.Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65(9):732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Raison CL, Dantzer R, Kelley KW, Lawson MA, Woolwine BJ, Vogt G, et al. CSF concentrations of brain tryptophan and kynurenines during immune stimulation with IFN-alpha: relationship to CNS immune responses and depression. Mol Psychiatry. 2010;15(4):393–403. doi: 10.1038/mp.2009.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zunszain PA, Anacker C, Cattaneo A, Carvalho LA, Pariante CM. Glucocorticoids, cytokines and brain abnormalities in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(3):722–729. doi: 10.1016/j.pnpbp.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Helmich I, Latini A, Sigwalt A, Carta MG, Machado S, Velasques B, et al. Neurobiological alterations induced by exercise and their impact on depressive disorders [corrected] Clin Pract Epidemiol Ment Health. 2010;6:115–125. doi: 10.2174/1745017901006010115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ridker P, Wilson P, Grundy S. Should C-reactive protein be added to metabolic syndrome and to assessment of global cardiovascular risk? Circulation. 2004;109(23):2818. doi: 10.1161/01.CIR.0000132467.45278.59. [DOI] [PubMed] [Google Scholar]
- 44.Toups MS, Trivedi MH. The role of metabolic dysfunction in treatment resistance of major depressive disorder. Neuropsychiatry. 2011;1(5):441–455. [Google Scholar]
- 45.Nicklas BJ, Beavers KM. Exercise, Weight Loss, and Effects on Inflammation. Current Cardiovascular Risk Reports. 2010;4(4):284–292. [Google Scholar]
- 46.Ivy JL. Role of exercise training in the prevention and treatment of insulin resistance and non-insulin-dependent diabetes mellitus. Sports Medicine. 1997;24(5):321–336. doi: 10.2165/00007256-199724050-00004. [DOI] [PubMed] [Google Scholar]
- 47.Ross R, Janssen I, Dawson J, Kungl AM, Kuk JL, Wong SL, et al. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obesity Research. 2004;12(5):789–798. doi: 10.1038/oby.2004.95. [DOI] [PubMed] [Google Scholar]
- 48.Arsenault BJ, CÙtÈ M, Cartier A, Lemieux I, DesprÈs JP, Ross R, et al. Effect of exercise training on cardiometabolic risk markers among sedentary, but metabolically healthy overweight or obese postmenopausal women with elevated blood pressure. Atherosclerosis. 2009;207(2):530. doi: 10.1016/j.atherosclerosis.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure. JAMA. 2007;297(19):2081. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- 50.Church TS, Martin CK, Thompson AM, Earnest CP, Mikus CR, Blair SN. Changes in weight, waist circumference and compensatory responses with different doses of exercise among sedentary, overweight postmenopausal women. PLoS One. 2009;4(2):e4515. doi: 10.1371/journal.pone.0004515. [DOI] [PMC free article] [PubMed] [Google Scholar]


