Abstract
Purpose
Congenital vertical talus (CVT) appears as an idiopathic or non-idiopathic deformity. In this study, we analysed the talar axis–first metatarsal base angle (TAMBA) values of idiopathic and non-idiopathic CVT cases treated with the Dobbs method.
Materials and methods
Between January 2007 and July 2012, 20 cases of CVT were treated, starting with a manipulation, casting and a minimally invasive surgical approach. We analysed retrospectively the TAMBA values in idiopathic and non-idiopathic CVT. As a new indicator for the mobility in the talonavicular complex, we used the difference of the TAMBA in neutral position and the TAMBA in plantarflexion. TAMBA measurements of CVT successfully treated with the Dobbs method were compared to TAMBA values of CVT unsuccessfully treated using a minimally invasive approach.
Results
Out of 20 CVT, 14 were successfully treated with the Dobbs method. Of these 14, five feet were non-idiopathic and nine feet were idiopathic. Six feet did not have complete correction following the Dobbs protocol, and were associated with arthrogryposis or caudal regression syndrome. The initial TAMBA in idiopathic feet ranged from 70 to 110° (mean 88°). The TAMBA in non-idiopathic feet ranged from 75 to 128° (mean 105). Feet successfully treated with the Dobbs method had an initial TAMBA between 74 and 110° (mean 87°). Feet unsuccessfully treated with the Dobbs method had an initial TAMBA between 95 and 128° (mean 118°).The measurement difference between the TAMBA in neutral and plantarflexion positions in cases unsuccessfully treated with the Dobbs method were smaller compared to values of feet successfully treated with the Dobbs method. These differences were statistically significant (p < 0.0001).
Conclusion
In our series, the success of the Dobbs method in CVT treatment depended on the flexibility in the talonavicular complex. The TAMBA value and TAMBA difference (TAMBA neutral minus TAMBA plantarflexion) express the flexibility in the talonavicular joint and could be predictive for the success of a minimally invasive treatment. Only in a few cases is the success of the Dobbs method limited. These feet are associated with a TAMBA greater than 120° in neutral position and, particularly, a TAMBA difference smaller than 25°.
Keywords: Vertical talus, Minimally invasive treatment, Reversed Ponseti technique, Flatfoot, Pes calcaneovalgus
Introduction
Congenital vertical talus (CVT) is a very rare foot disorder, with clinical appearance of a rocker bottom deformity with a hindfoot equinus and a dorsiflexed forefoot (Fig. 1). The deformity is characterised by a rigid dislocation of the talonavicular joint, and the talar head is displaced medioplantar. The navicular is dislocated into the dorsolateral aspect of the talus head, or, in severe cases, onto the neck of the talus. The medial tendons, the calcaneonavicular ligament and the anterior fibres of the delta ligament are elongated. Contractures are on the dorsolateral side and include the peroneal tendons, the extensor tendons, the calcaneofibular ligament, the talonavicular ligaments and the capsule of the ankle and the subtalar joint [1].
Fig. 1.

Clinical appearance of a severe congenital vertical talus (CVT) associated with arthrogryposis
Flexible deformities, such as pes calcaneovalgus or oblique talus, should be distinguished from CVT [2]. In contrast to congenital clubfoot, there is currently no clinical classification for CVT which assesses the severity of the deformity; current classifications are more focused on associated disorders [3, 4].
The talar axis–first metatarsal base angle (TAMBA) described by Hamanishi is a radiological measurement to differentiate oblique talus and true vertical talus, and to assess the severity of the dislocation in the talonavicular complex [3].
The treatment of CVT is complex, and, in the past, extensive surgery with soft-tissue releases was the treatment of choice. The Dobbs method, published in 2006, is a new minimally invasive concept for vertical talus treatment using manipulation, casting and percutaneous tenotomy [5]. Several papers show promising short-term results for idiopathic CVT [5–7].
In this prospective series, we included idiopathic and non-idiopathic cases. The clinical results of idiopathic and non-idiopathic CVT are presented. TAMBA measurements from subjects in which the Dobbs method was successful were compared to TAMBA measurements from cases in which the Dobbs method was unsuccessful.
Materials and methods
Between January 2007 and July 2012, 14 children with 24 severe calcaneovalgus deformities presented in our clinic. Oblique talus and vertical talus were differentiated using plantarflexion radiographs. There were four oblique talus and 20 true CVT deformities. Oblique talus deformities were excluded from the study; we included idiopathic and non-idiopathic CVT cases.
Treatment of the CVT cases followed the recommendations of Dobbs et al. from 2006 [5]. Treatment started with manipulation and casting. Manipulation included a reversed Ponseti manoeuvre, stretching the foot into plantarflexion and inversion, while counter-pressure is applied to the medially displaced talar head. In cases of complete reduction of the talonavicular joint by manipulation and casting alone, a percutaneous K-wire was introduced for temporary joint fixation for 6 weeks. In cases with incomplete reduction, we performed an open reduction of the talonavicular joint using a medial mini-incision. In cases of severe dislocation of the talonavicular complex after casting, we started with open reduction of the talonavicular joint, followed by a soft-tissue release adapted to the severity of the deformity, using a modified Cincinnati approach. Post-operative treatment differed from the Dobbs protocol; instead of a Dennis Brown bar, we used a unilateral ankle–foot orthosis with a high arch to support the correction.
The patient data were prospectively documented. Documented data include gender, age at the beginning of treatment, associated disorders, and dorsiflexion and plantarflexion at the most current follow-up.
We retrospectively analysed the radiological measurements. Radiological measurements included pre-operative TAMBA neutral position, TAMBA in plantarflexion and TAMBA at the most current follow-up. As an indicator of the mobility in the talonavicular joint, we introduced the difference between the TAMBA in neutral position and the TAMBA in plantarflexion (TAMBA dif.). TAMBA measurements of feet in which the Dobbs method was successful were compared to measurements of CVT where this approach was unsuccessful. A t-test was used for the statistical analysis.
The clinical and radiological results were evaluated using the Hamanishi score and measurements of dorsiflexion and plantarflexion.
Results
Out of 24 deformities, four feet were oblique talus deformities. According to the radiological classification of Hamanishi using the TAMBA, the TAMBA of these feet ranged from 30 to 64° (mean 44.5°) in neutral position and from 0 to 15° (mean 5.25°) in plantarflexion. These were excluded from the study.
Between January 2007 and July 2012, we treated 20 CVT deformities. There were eight boys and six girls, and their age at presentation was between 20 days and 14 months. There were 11 non-idiopathic feet and nine with idiopathic CVT. The non-idiopathic feet were associated with two children with arthrogryposis, two children with chromosomal abnormalities, one child with an unknown neuromuscular disorder and one child with caudal regression syndrome.
Fourteen feet were corrected using the minimally invasive concept from Dobbs (nine idiopathic feet, five non-idiopathic feet). Twelve feet had closed reduction of the talonavicular joint and two feet had an open reduction via a medial mini-incision. All 14 feet had percutaneous tenotomy of the Achilles tendon.
Six non-idiopathic feet were treated with more invasive approaches. They were associated with arthrogryposis and caudal regression syndrome. Two feet underwent posterior, medial and lateral releases, and two feet were planned for soft-tissue release after unsuccessful casting; in these cases, the TAMBA values were greater than 120° and TAMBA dif. was between 3° and 16°. Two feet received an unsuccessful trial with an open reduction of the talonavicular joint via a medial mini-incision with K-wire fixation, percutaneous tenotomy of the Achilles tendon and a closed reduction of the calcaneocuboid joint with K-wire fixation. In this case, the pre-operative TAMBA was 95° on the right and 110° on the left sides, and TAMBA dif. was 13° and 20°, respectively.
The TAMBA of idiopathic and non-idiopathic feet ranged from 74 to 128° (mean 93.7°) in neutral position and from 30 to 124° (mean 58.9°) in plantarflexion.
In idiopathic feet, the initial TAMBA ranged from 70 to 110° (mean 88°) in neutral position and from 32 to 60° (mean 45°) in plantarflexion. TAMBA dif. ranged from 26 to 54° (mean 41°).
In non-idiopathic feet, the initial TAMBA ranged from 75 to 128° (mean 105°) in neutral position and from 30 to 124° (mean 82°) in plantarflexion. TAMBA dif. ranged from 3 to 57° (mean 24.8°).
In the group of feet successfully treated with the Dobbs method, the initial TAMBA in neutral position ranged from 74 to 110° (mean 87°) and from 30 to 60° (mean 45°) in plantarflexion. TAMBA dif. ranged from 26 to 57° (mean 41°) (Fig. 2a–c).
Fig. 2.
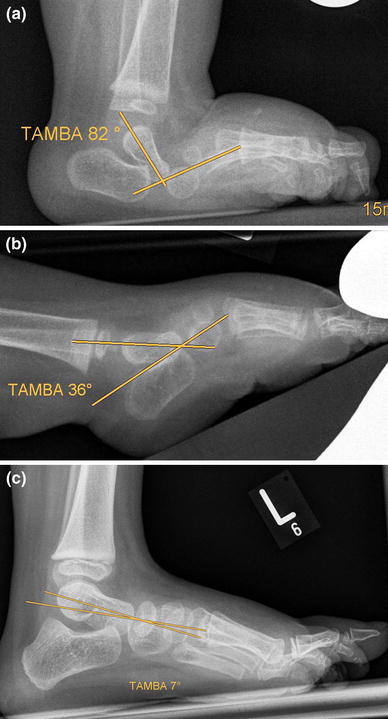
CVT associated with chromosomal abnormality in chromosome 8. a Initial talar axis–first metatarsal base angle (TAMBA) was 82° at first presentation, age 9 months. b Plantarflexion radiograph at first presentation with TAMBA of 36°. The TAMBA difference between neutral position and in plantarflexion as a sign for the mobility in the talonavicular complex was 46°. c At the age of 3.5 years, complete correction with TAMBA 7°, following minimally invasive treatment, casting, closed reduction of the talonavicular joint with temporary percutaneous K-wire fixation and percutaneous tenotomy of the Achilles tendon
In the group of feet unsuccessfully treated with the Dobbs method, the initial TAMBA in neutral position ranged from 95 to 128° (mean 118°) and from 82 to 124° (mean 106°) in plantarflexion. TAMBA dif. ranged from 3 to 20° (mean 11°) (Fig. 3a–c).
Fig. 3.
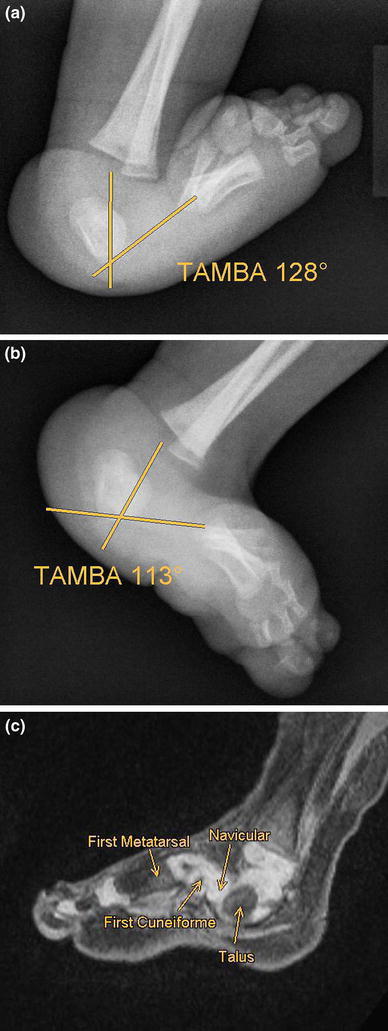
CVT associated with arthrogryposis. a, b There is minimal difference between the TAMBA values in neutral position and in plantarflexion, showing a severe rigidity in the talonavicular complex, c Magnetic resonance imaging (MRI) scan after casting with persistent severe deformity. The navicular is impacted in the space between the first cuneiforme and the talus
Maximal TAMBA values of feet successfully treated using the Dobbs method were lower, but not statistically significantly lower compared with the maximal values of feet in which the minimally invasive approach was unsuccessful. The measurements of TAMBA dif. were smaller in cases unsuccessfully treated with the Dobbs method compared to values of feet with successful treatment.
These differences were statistically significant (p < 0.0001) and are summarised in Table 1 and Fig. 4.
Table 1.
Talar axis–first metatarsal base angle (TAMBA) measurements of the different groups evaluated in the presented study
| TAMBA neutral | TAMBA plantarflexion | TAMBA difference (neutral − plantar) | |
|---|---|---|---|
| Idiopathic CVT | 70–110° (Ø 88°) | 32–60° (Ø 45°) | 26–54° (Ø 24,8°) |
| Non-idiopathic CVT | 75–128° (Ø 105°) | 30–124° (Ø 82°) | 3–57° (Ø 41°) |
| CVT successfully treated with Dobbs method | 74–110° (Ø 87°) | 30–60° (Ø 45°) | 26–57° (Ø 41°) |
| CVT unsuccessfully treated with Dobbs method | 95–128° (Ø 118°) | 82–124° (Ø 106°) | 3–20° (Ø 11°) |
Range and mean values in parentheses are shown
Fig. 4.
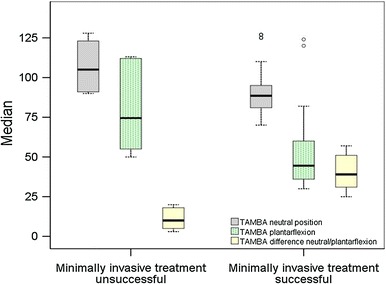
Box plot showing the range and the mean values of TAMBA in neutral position, TAMBA in plantarflexion and TAMBA difference (TAMBA neutral position − TAMBA plantarflexion) in CVT cases following successful and unsuccessful treatment with the Dobbs method (minimally invasive approach)
There was no correlation between the age and the success of the minimally invasive approach. Although we started with casting in the cases associated with arthrogryposis earlier than in the other CVT cases, we were not successful with manipulation, casting and percutaneous tenotomy in these cases.
At the most current follow-up (3–60 months, mean 24 months), feet with a successful treatment using the Dobbs method had a mean dorsiflexion of 23.3° (20–30°) and a mean plantarflexion of 35.5° (20–40°). One child with closed reduction and percutaneous tenotomy of the Achilles tendon (initial post-operative TAMBA 20°) developed a relapse, with a TAMBA of 79°. In this group, the TAMBA at the most current follow-up was 2–25° (mean 9.1°). According to the Hamanishi radiological score, we had nine excellent and two good results. The relapse must be regarded as a complete luxation of the talonavicular joint.
Discussion
With an incidence of 1 in 10,000 newborns, CVT is less frequent than congenital clubfoot. In about 50 % of the cases, this deformity is associated with neuromuscular or genetic disorders. Typical disorders associated with CVT are arthrogryposis, caudal regression syndrome, myelodysplasia or genetic abnormalities like trisomy 13, 15 and 18 [1, 4, 8]. In our series, 54 % were associated with neurological or genetic disorders, including arthrogryposis, caudal regression syndrome, unknown neuromuscular disorders or chromosomal abnormalities in chromosomes 1 and 8.
In the past, many approaches for treating CVT have been described [1, 9–15]. Giannestras published a manipulation technique for CVT in 1970, with successful treatment in mild cases [9]. Silk and Wainwright reduced the talonavicular joint with manipulation and casting, the posterior contractures being corrected by Achilles lengthening and capsulotomy [10]. In the 1990s, soft-tissue releases in one-stage procedures became the preferred treatment. Influenced by the Ponseti treatment for congenital clubfoot, Dobbs introduced a new approach for treating CVT in 2006. The concept includes manipulation and casting with a so-called reversed Ponseti technique, a closed reduction of the talonavicular joint with a temporary percutaneous K-wire fixation and a percutaneous tenotomy of the Achilles tendon for the posterior contracture. For cases with incomplete reduction of the talonavicular joint after casting, he recommended an open reduction via a mini-incision [5].
In this series, we followed the protocol from Dobbs et al. in 2006 [5]. We were able to correct idiopathic CVT (n = 9 feet), CVT associated with chromosomal abnormalities (n = 4 feet) and CVT with unknown neurological disorder (n = 1 foot). In severe cases associated with arthrogryposis and caudal regression syndrome (n = 6 feet), we were not able to achieve full correction using the above-mentioned Dobbs protocol.
To evaluate our results of true vertical talus, we used different TAMBA values. We distinguished oblique talus from true vertical talus. The mean TAMBA in neutral position of the oblique talus cases was 44.5°. The TAMBA in neutral position was more than 70° in all true CVT cases, with a mean of 93.7°. We measured the maximal values of the TAMBA in neutral position and in plantarflexion. As a gauge of the mobility in the talonavicular complex, we used the difference of the TAMBA in neutral position and the TAMBA in plantarflexion (TAMBA dif.). The goal was to determine whether TAMBA values before treatment are predictive for the success of the method described by Dobbs.
There is a wide spectrum of CVT deformities with different TAMBA values. In the study by Hamanishi, most CVT had TAMBA values between 60 and 100°. Six out of 69 feet had TAMBA values greater than 110° [3]. This is comparable to our series, in which most cases had TAMBA measurements between 74 and 110°. Only four feet had TAMBA values greater than 110°.
We compared the TAMBA values of patients treated successfully and unsuccessfully using the Dobbs method. In our series, there was no correlation between the success of a minimally invasive approach and whether idiopathic or non-idiopathic CVT was present. The success correlated with the primary stiffness in the talonavicular complex as measured by the TAMBA dif. value. We were able to correct five feet associated with chromosomal abnormalities and unknown neurological disorders with manipulation, casting and a percutaneous tenotomy. All five feet had a TAMBA less than 95° in neutral position and mobility in the talonavicular joint complex of more than 25° (TAMBA dif.). In contrast, six feet unsuccessfully treated using a minimally invasive approach had maximal values in neutral position of 95° or greater than 95° and a mobility less than 25° (TAMBA dif.). Four out of six feet had TAMBA values greater than 120°.
Similar to our findings, Silk and Wainwright were able to reduce the talonavicular joint with manipulation and casting in cases where the TAMBA was between 78° and 95° (data from the paper by Hamanishi) [3, 10]. Bhaskar [7] corrected idiopathic CVT with the reversed Ponseti technique in cases with TAMBA values between 40 and 70° (mean 60°).
It seems that there are a small number of CVT cases which need more than manipulation and casting, i.e. open reduction of the talonavicular joint via a mini-open incision and percutaneous tenotomy of the Achilles tendon. These feet have initial TAMBA dif. values smaller than 25°, a sign of severe rigidity in the talonavicular complex. In contrast, feet with a good chance for successful treatment with a minimally invasive approach have TAMBA dif. values of more than 25°, indicating better flexibility in the talonavicular complex. In our series, the values of TAMBA dif. were statistically smaller (p < 0.0001) in the group of CVT cases treated successfully with the Dobbs method than in the group of CVT cases where treatment was unsuccessful. CVT cases with such small initial TAMBA dif. values require more complex procedures for successful treatment. In these cases, the success of the Dobbs method from 2006 is limited.
One reason for unsuccessful casting in severe CVT cases could be the position of the navicular. In two feet, we were able to evaluate the position of the navicular in arthrogrypotic CVT by magnetic resonance imaging (MRI). The navicular was located at the neck of the talus, and after six casts, the navicular had not moved into the right position at the head of the talus. The navicular was impacted in the space between the first cuneiforme and the neck of the talus. In these cases, we achieved no essential improvement with casting (Fig. 3c).
Perhaps with modifications to the Dobbs method from 2012 it will be possible to achieve better results in this group of severe CVT [16]. A primary capsulotomy of the talonavicular joint and the calcaneocuboid joint as performed on relapses by the St. Louis group may be the best approach to achieve primary correction. This has to be proven in further studies.
A limitation of our study was the small number of cases, especially in the group of feet where the Dobbs method was unsuccessful.
Nevertheless, regarding our experience with the minimally invasive technique, the method published by Dobbs et al. in 2006 [5] is the first option when treating CVT. Manipulation by stretching the foot in plantarflexion and inversion with counter-force to the talar head is successful in reducing the talonavicular joint in most CVT cases. For the posterior contracture, in most cases, a percutaneous tenotomy of the Achilles tendon is enough for correction. Such a minimally invasive approach leads to good results in many idiopathic and non-idiopathic CVT cases. TAMBA values were achieved which were near normal. The TAMBA measurements at the most current follow-up was 8 + 1.8° for non-idiopathic feet in the St. Louis group, 6–15° (mean 10.5°) for idiopathic feet in the series by Bhaskar et al. and 2–25° (mean 9.1°) in our series of idiopathic and non-idiopathic feet [5–7].
The presented value of TAMBA dif. is helpful in evaluating the severity of CVT. This value gives information about the flexibility in the talonavicular complex and can detect cases which require more extensive surgery. TAMBA dif. smaller than 25° represents a severe rigidity in the talonavicular joint. Maximum TAMBA measurements in neutral position of more than 95° can be regarded as a severe deformity. TAMBA measurements greater than 120° represent a very severe deformity. For these cases with unsuccessful minimally invasive treatment, the surgical treatment should be adapted to the severity of the deformity using capsulotomies of the talonavicular joint, the calcaneocuboid joint and the posterior joints. A proper casting technique can diminish the deformity and allow for easier surgical correction.
Conflict of interest
None.
References
- 1.Drennan JC. Congenital vertical talus. J Bone Joint Surg Am. 1995;77:1916–1923. [Google Scholar]
- 2.Greenberg AJ. Congenital vertical talus and congenital calcaneovalgus deformity: a comparison. J Foot Surg. 1981;20:189–193. [PubMed] [Google Scholar]
- 3.Hamanishi C. Congenital vertical talus: classification with 69 cases and new measurement system. J Pediatr Orthop. 1984;4:318–326. doi: 10.1097/01241398-198405000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Ogata K, Schoenecker PL, Sheridan J. Congenital vertical talus and its familial occurrence: an analysis of 36 patients. Clin Orthop Relat Res. 1979;139:128–132. [PubMed] [Google Scholar]
- 5.Dobbs MB, Purcell DB, Nunley R, Morcuende JA. Early results of a new method of treatment for idiopathic congenital vertical talus. J Bone Joint Surg Am. 2006;88:1192–1200. doi: 10.2106/JBJS.E.00402. [DOI] [PubMed] [Google Scholar]
- 6.Eberhardt O, Fernandez FF, Wirth T. Die Behandlung des Talus verticalis mit der Methode nach Dobbs. Z Orthop Unfall. 2011;149:219–224. doi: 10.1055/s-0030-1270822. [DOI] [PubMed] [Google Scholar]
- 7.Bhaskar A. Congenital vertical talus: treatment by reverse ponseti technique. Indian J Orthop. 2008;42:347–350. doi: 10.4103/0019-5413.41860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alaee F, Boehm S, Dobbs MB. A new approach to the treatment of congenital vertical talus. J Child Orthop. 2007;1:165–174. doi: 10.1007/s11832-007-0037-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giannestras NJ. Recognition and treatment of flatfeet in infancy. Clin Orthop Relat Res. 1970;70:10–29. [PubMed] [Google Scholar]
- 10.Silk FF, Wainwright D. The recognition and treatment of congenital flat foot in infancy. J Bone Joint Surg Br. 1967;49:628–633. [PubMed] [Google Scholar]
- 11.Seimon LP. Surgical correction of congenital vertical talus under the age of 2 years. J Pediatr Orthop. 1987;7:405–411. doi: 10.1097/01241398-198707000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Clark MW, D’Ambrosia RD, Ferguson AB. Congenital vertical talus: treatment by open reduction and navicular excision. J Bone Joint Surg Am. 1977;59:816–824. [PubMed] [Google Scholar]
- 13.Zorer G, Bagatur AE, Dogan A. Single stage surgical correction of congenital vertical talus by complete subtalar release and peritalar reduction by using the Cincinnati incision. J Pediatr Orthop B. 2002;11:60–67. doi: 10.1097/00009957-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Wirth T, Schuler P, Griss P. Early surgical treatment for congenital vertical talus. Arch Orthop Trauma Surg. 1994;113:248–253. doi: 10.1007/BF00443812. [DOI] [PubMed] [Google Scholar]
- 15.Napiontek M. Congenital vertical talus: a retrospective and critical review of 32 feet operated on by peritalar reduction. J Pediatr Orthop B. 1995;4:179–187. doi: 10.1097/01202412-199504020-00010. [DOI] [PubMed] [Google Scholar]
- 16.Chalayon O, Adams A, Dobbs MB. Minimally invasive approach for the treatment of non-isolated congenital vertical talus. J Bone Joint Surg Am. 2012;94:e73. doi: 10.2106/JBJS.K.00164. [DOI] [PubMed] [Google Scholar]


