Abstract
Background
Multilevel orthopedic surgery is considered to be the gold standard treatment for ambulatory children with cerebral palsy (CP), classified at levels I, II, or III according to the Gross Motor Function Classification System (GMFCS). Hip enlocation and stability are the main goals of orthopedic intervention in the GMFCS level IV subgroup and are well researched; however, there is no evidence to date to support or challenge the effectiveness of orthopedic treatment to preserve functional mobility in this patient group. The aim of this study was to evaluate the results of orthopedic surgery to maintain or restore standing transfers and supported walking in children with CP at GMFCS level IV.
Methods
Twenty-two children with CP GMFCS level IV who underwent orthopedic surgery to improve mobility between the years 2004 and 2008 were included in this study. A retrospective chart review was performed and a satisfaction questionnaire sent to all patients. The primary outcome measure was the attainment and maintenance of mobility goals 2 years post-surgery. The secondary outcome measures were family/patient satisfaction, Functional Mobility Scale (FMS), and complications.
Results
The two goals identified by the patients and carers were standing transfers and supported walking. At the 2-year post-surgery assessment, 14 children (63.6 %) did not reach their pre-determined goals. In the questionnaire, 21.4 % of the families reported that surgery was not beneficial. The FMS score remained unchanged in 95.4 % of the patients. Fourteen patients (63.6 %) had at least one complication that prolonged their post-operative rehabilitation (e.g., neuropraxia).
Conclusion
This study suggests that orthopedic surgery in children with CP at GMFCS level IV is unlikely to maintain or restore mobility. Furthermore, it carries a significant risk of complications.
Level of evidence
Case series, Level IV.
Keywords: Cerebral palsy, Orthopedic surgery, Mobility
Introduction
Cerebral palsy (CP) is the most common physical disability affecting children in developed countries, with an overall incidence of 2.0–2.5 per 1,000 live births [1]. The Gross Motor Function Classification System (GMFCS) [2] is one of the most useful methods to classify children with CP, based on their functional abilities and limitations. Motor growth curves have been described in CP using the Gross Motor Function Measure (GMFM), showing a decline in mobility as children at GMFCS levels III, IV, and V enter their teenage years [3, 4]. The knowledge of the natural history of CP has allowed clinicians to better establish goals and propose treatment plans for these patients [5].
In ambulatory patients (GMFCS levels I, II, and III), single-event multilevel surgery has become widely accepted as the gold standard to improve gait [6–10]. However, the effectiveness of orthopedic surgery to improve and maintain mobility in children with lower functional levels (GMFCS level IV) has not been ascertained.
The most common aim in orthopedic surgery for children with CP GMFCS level IV is limited to the treatment and prevention of spastic hip disease and scoliosis [11, 12]. Children classified at GMFCS level IV have very limited mobility, but may be able to transfer and walk small distances with external support at a young age [2].
The ability to retain standing transfers in adolescents and young adults with CP means that they do not require lifting or hoisting by their carers. It is known that caregivers of children with CP are at a higher risk of mental and/or physical distress, which correlates with the increased caregiving demands of their children [13].
Supported walking and standing in a therapeutic setting for non-ambulatory children with CP seem to improve participation in activities of daily living and social roles, as well as pulmonary and gastrointestinal function [14]. Weight-bearing can potentially have a positive effect on bone mineral density, although its role in children with CP is still unclear [15].
Measuring functional outcomes can be challenging in patients with CP at GMFCS level IV. Functional goals can vary significantly and few valid and reliable tools are available for this specific patient group. The International Classification of Functioning, Disability and Health (ICF) [16] provides a framework for outcome assessment following clinical intervention. In this setting, satisfaction questionnaires are often employed to obtain feedback from patients and families [17].
Standardized scales to measure mobility, such as the Functional Mobility Scale (FMS) and the Gillette Functional Assessment Questionnaire, can be used to evaluate ambulatory children with CP [18, 19]. However, these instruments may lack the sensitivity to detect changes in children at GMFCS level IV.
The aims of this study are: (1) to evaluate the results of orthopedic surgery to maintain or restore standing transfers and supported walking in children with CP at GMFCS Level IV, (2) to analyze the rate of complications, and (3) to assess family/patient satisfaction with the medium-term outcomes.
Methods
A retrospective chart review of children with CP treated at a tertiary hospital was conducted. Baseline and post-operative data were collected from the medical records and clinical notes. Additional post-operative data were collected prospectively via a self-reported questionnaire. Written consent was obtained from each child’s parent or legal guardian. The study was approved by the institution’s ethics committee.
The cohort was represented by a consecutive sample of children who underwent orthopedic surgery between the years 2004 and 2008. All children were treated by two senior pediatric orthopedic surgeons (M.W.A., P.S.) specialized in the treatment of CP and neuromuscular disorders. Two authors conducted the chart review independently (F.C.B., J.C.N.W.). Any discrepancies in data were resolved through consultation with a third author (M.W.A.), serving as arbitrator when necessary.
The inclusion criteria were: (1) children with a diagnosis of CP, (2) GMFCS level IV, classified at the peak mobility level, (3) surgical goal of maintaining or restoring functional mobility, and (4) minimum follow-up of 2 years. Patients who underwent orthopedic surgery exclusively for hip stability and enlocation were not included. Patients who had undergone previous orthopedic interventions in the lower limbs were also excluded.
Family-reported decline in function with concomitant increase in dependency was a fundamental indication for surgery. The procedures performed aimed to address deformities contributing to the loss of function. In particular, to achieve hip enlocation, full knee extension, and plantigrade braceable feet. Post-operative rehabilitation consisted of 1–2 physiotherapy sessions per week, with an additional weekly session of hydrotherapy for the first 3 months. Patients continued regular physiotherapy for 18–24 months after surgery.
The primary outcome measure was the attainment and maintenance of mobility goals 2 years post-surgery. The secondary outcomes were: (1) rate of surgical complications, (2) FMS score, and (3) satisfaction, determined by a self-reported questionnaire.
For children classified at GMFCS level IV, the two main mobility goals identified in this study were standing transfers and supported walking. For the purposes of this study, standing transfer was defined as the ability to transfer (e.g., from the wheelchair to the bed) with partial or full weight-bearing through the lower limbs, with or without assistance from another person. Supported walking was defined as the ability to walk short distances (5 m) with a supportive walker and assistance from a caregiver (FMS score 1,1,1).
A self-reported satisfaction questionnaire was mailed to all families to assess parents’ perceptions of treatment benefits and acceptance of further similar treatment in the event of a relapse. The parents were asked to rate outcome satisfaction using a 10-point scale, where 1 represents “not worthwhile” and 10 represents “extremely worthwhile”. The researcher responsible for the questionnaire analysis (K.V.B.) was blinded to the information collected in the chart review and had no previous relationship with the families.
Statistical analysis
Descriptive data were expressed as means and standard deviations (SDs) for normally distributed continuous data and as medians for ordinal or skewed data. Prevalence estimates were presented as percentages. The association between categorical variables was verified by the Chi-square and McNemar tests. Mean differences of continuous data were compared between groups using the t-test for independent samples. For all statistical tests, a 95 % confidence interval was used and p < 0.05 was deemed statistically significant.
Results
Twenty-two patients were included in this study, with a mean age of 12 years at the time of surgery (range 7–16 years) (Table 1). There were 15 males (68 %) and 7 females (32 %). All patients had spastic quadriplegia and were classified as GMFCS level IV. The median number of surgical procedures performed was 8 (range 2–14) (Table 1).
Table 1.
Details of the patients, gender, age at surgery, baseline Functional Mobility Scale (FMS) score, surgery goals, achievement of goals, surgery performed, and number of procedures in the 22 included children with cerebral palsy (CP) Gross Motor Function Classification System (GMFCS) level IV
| Case | Gender | Age at surgery (years) | Baseline FMS score | Surgery goals | All goals achieved? | Surgery performed | Number of procedures | ||
|---|---|---|---|---|---|---|---|---|---|
| Hip | Knee | Foot | |||||||
| 1 | M | 14.4 | 1,1,1 | ST | No | PR, AR | DFEO, STT, MHL | – | 10 |
| 2 | M | 8.4 | 2,1,1 | ST, W | Yes | VDRO, AR | STT, MHL | – | 8 |
| 3 | F | 11.4 | 1,1,1 | ST | Yes | – | DFEO, STT, MHL, LHL | CL, TPL | 10 |
| 4 | M | 13.7 | 1,1,1 | ST | No | VDRO, PO, PR, AR | PC, STT, MHL, LHL | – | 14 |
| 5 | F | 12.4 | 1,1,1 | ST | No | PR, AR | DFEO, STT, MHL | SF | 8 |
| 6 | M | 7.0 | 1,1,1 | ST | Yes | AR | STT, MHL | – | 6 |
| 7 | F | 12.5 | 1,1,1 | ST, W | No | PR, AR | MHL | TPL | 6 |
| 8 | M | 10.7 | 1,1,1 | ST, W | Yes | PR, AR | PC, STT, MHL, LHL | – | 12 |
| 9 | M | 12.3 | 1,1,1 | ST, W | Yes | PR, AR | STT, MHL | SF, LCL, CL | 11 |
| 10 | M | 11.8 | 1,1,1 | ST, W | No | PR, AR | STT, MHL | SF, CL | 12 |
| 11 | M | 14.8 | 1,1,1 | ST, W | Yes | AR | STT, MHL | SF, CL | 10 |
| 12 | F | 8.6 | 1,1,1 | ST, W | No | VDRO, PO, PR, AR | DFAH, STT, MHL, RFT | CL | 14* |
| 13 | M | 15.6 | 1,1,1 | ST, W | No | AR | MHL | – | 4 |
| 14 | M | 11.8 | 1,1,1 | ST | No | AR | STT, MHL | – | 6 |
| 15 | M | 14.4 | 1,1,1 | ST, W | Yes | – | DFEO | – | 2 |
| 16 | F | 9.7 | 2,1,1 | ST, W | No | PR, AR | DFEO, STT, MHL | CL | 12 |
| 17 | F | 13.2 | 1,1,1 | ST | No | PR, AR | RFT | – | 6 |
| 18 | F | 16.6 | 1,1,1 | ST | No | PR, AR | DFEO, PTS, MHL | – | 7 |
| 19 | M | 12.3 | 1,1,1 | ST | No | – | DFEO, MHL, LHL | – | 6 |
| 20 | M | 12.5 | 1,1,1 | ST, W | Yes | VDRO, PO | MHL, LHL, RFT | – | 8* |
| 21 | M | 12.0 | 1,1,1 | ST | No | PR | DFEO | – | 4 |
| 22 | M | 7.4 | 1,1,1 | ST | No | VDRO, AR | DFEO, STT, MHL | – | 10* |
FMS Functional Mobility Scale. Surgery goals: ST standing transfers, W supported walking. Surgery performed: hip: AR adductors release, PO pelvic osteotomy, PR psoas release, VDRO varus derotation osteotomy; knee: DFEO distal femoral extension osteotomy, DFAH distal femur anterior hemiepiphysiodesis, PC posterior capsulotomy, PTS patellar tendon shortening, STT semitendinosus transfer to adductor magnus, RTF rectus femoris transfer, MHL medial hamstrings lengthening, LHL lateral hamstrings lengthening; foot: CL calf muscles lengthening, LCL lateral column lengthening, SF subtalar fusion, TPL tibialis posterior lengthening. Number of procedures: asterisk surgery performed in two stages. Note that, in some patients, one or more procedures were unilateral
The ability to do standing transfers was identified as a goal for surgery in all the patients, whereas supported walking was a goal for 11 children (50 %). At the 2-year post-surgery assessment, 14 children (63.6 %) did not reach their pre-determined goals. No statistically significant difference was found in goal achievement considering age (p = 0.47) and gender (p = 0.14).
The distribution of patients with the ability to do standing transfers and supported walking at baseline and 2 years post-surgery is illustrated in Figs. 1 and 2. There was a decrease in the number of patients able to perform standing transfers 2 years after surgery, and this was borderline statistically significant (p = 0.07). The same decrease was observed for the ability to do supported walking, which was not statistically significant (p = 0.69).
Fig. 1.
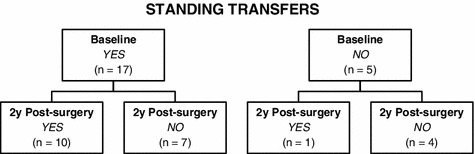
Comparison between baseline and 2 years post-surgery assessment for the outcome ‘ability to do standing transfers’ (McNemar Chi-square: p = 0.07)
Fig. 2.
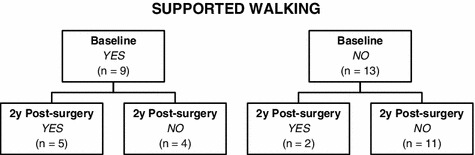
Comparison between baseline and 2 years post-surgery assessment for the outcome ‘ability to do supported walking’ (McNemar Chi-square: p = 0.69)
Fourteen patients (63.6 %) had at least one complication that prolonged their post-operative rehabilitation (e.g., neuropraxia) (Table 2). Complications occurred in 42 % of patients who had soft-tissue procedures and in 73 % of those who had bony and soft-tissue procedures. This difference was not statistically significant (p = 0.16).
Table 2.
Complications prevalence
| Complicationsa | Number of patients | Percent |
|---|---|---|
| Neuropraxia | 8 | 36.4 |
| Neuropathic pain | 6 | 27.3 |
| Knee hyperextension | 4 | 18.2 |
| Pressure sores | 3 | 13.6 |
aComplications interfering with the post-operative rehabilitation. Note that some patients developed more than one type of complication
The FMS score at 2 years post-surgery remained unchanged for almost all patients, except for one (case 16), who regressed from 2,1,1 to 1,1,1. One child managed to maintain an FMS score of 2,1,1 after 2 years post-surgery (case 2).
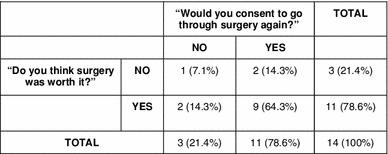
Prospective questionnaire data were obtained for 14 patients (63.6 %). Two patients refused to participate (9.1 %), five were lost to follow-up (22.7 %), and one patient did not reply due to language restrictions (4.6 %). Only three families (21.3 %) reported that surgery was not worth it. Eleven families (78.6 %) reported that they would agree to similar surgery should a relapse occur (Table 3). The median of the outcome score rated by the families was 7.5 (interquartile range = 6–9).
Table 3.
Summary of the answers to the self-reported questionnaire
Discussion
To our knowledge, this study is the first to evaluate the effectiveness of orthopedic surgery in improving mobility in children with CP, specifically, GMFCS level IV. The patients included in this review were part of a multidisciplinary service and received comprehensive care. The GMFCS levels were classified at the peak of their motor curve development [3, 4].
Several authors have reported favorable results of multilevel orthopedic surgery in the management of ambulatory patients with CP [5–9]. Benefits include improvements in gait, relief of joint contractures, reduction of energy expenditure, and increase in functional parameters [20].
Khan [21] reported a series of previously untreated 85 non-walker children with diplegic CP who underwent multilevel surgery. All patients improved and became walkers. However, since the GMFCS was not used, their cohort cannot be compared to this study [22].
We found a low rate of success after surgery in our series, with only 36.4 % of the patients achieving their goals. The FMS scores remained the same in 95.4 % of the patients. Only one patient maintained an FMS score of 2,1,1 at 2 years follow-up, which may be related to the fact that this patient was 8 years old at the time of surgery. Some children lost their ability to do supported walking and standing transfers at 2 years post-surgery (Figs. 1 and 2). These data emphasize the inherent functional limitation of these patients and the inability of complex orthopedic surgery and intensive rehabilitation to overcome such limitations.
Some external factors are known to influence the outcomes after orthopedic surgery, including post-operative rehabilitation, use of orthotic devices, pain-controlling strategies, adequate tone control, and presence of comorbidities [23, 24]. However, all patients in this series received a standardized physiotherapy program as described previously, and were closely monitored by the team of specialists involved in their care to ensure adequate medical management suited to their individual needs.
A significant rate of surgical complications (63.6 %) was found in this study. Nerve palsies and persistent neuropathic pain in the lower extremities were the most common and have been previously reported by other authors. We believe that most of the complications in this cohort were a result of knee extension procedures. In our opinion, full knee extension is crucial to promote stability of the lower limbs during standing and transfers. Hamstrings lengthenings/transfers and distal femoral extension osteotomies (DFEO) are the most common procedures to correct knee flexion contractures in cerebral palsy.
Lauder and White [25] reported six patients with neuropathic pain, five of whom had procedures including hamstrings releases and/or posterior capsulotomies to treat knee flexion, with no mention of ambulatory status in their cohort. Karol et al. [26] found an incidence of 9.6 % of nerve palsies following 329 hamstrings lengthening procedures, and identified the following as potential risk factors: older age, non-communicative patients, non-walkers, and epidural pain management. Their data is in accordance with our findings.
Stout et al. reported complications of up to 19 % after DFEO, including nerve palsies and neuropathies as the most common [27]. To our knowledge, the outcomes of DFEO in GMFCS level IV patients have not been previously reported. In this cohort, nine patients underwent DFEO, seven of whom presented with complications such as knee hyperextension and neuropraxia.
The questionnaire revealed a high rate of parental satisfaction. However, these results must be interpreted with caution. We were unable to collect questionnaire data from eight patients, two of whom refused to answer the questionnaire and verbally reported that they were traumatized by the orthopedic and rehabilitation interventions. Four families provided conflicting responses, which may either indicate misunderstanding of the questionnaire or its subjectivity.
Informal feedback received during post-operative clinic visits may explain the combination of poor outcomes and high satisfaction rates. One common statement was that the surgical and rehabilitation process and the respective outcomes helped the parents to better understand and accept their child’s functional limitations.
Satisfaction can be considered as a subjective outcome, defined as the state of having one’s expectations, desires, needs, or demands fulfilled. We believe that satisfaction may reflect the effectiveness of an intervention as it evaluates families’ perception of the results. Lee et al. [28] suggested that small changes in performance after multilevel surgery in CP patients are associated with a significant increase in parental satisfaction.
The retrospective nature of our study is an important limitation. The small sample size limited statistical analysis, making it difficult to identify possible predictors of poor outcomes. Furthermore, the questionnaire utilized has not been validated.
Despite the limitations of this study, the negative outcomes and significant complication rate observed in this cohort suggests that orthopedic surgery is unlikely to maintain or restore mobility in children with CP GMFCS level IV. This may represent the inevitable progression of natural history in this group of patients, as described by Palisano et al. [5]. We believe that orthopedic treatment for this patient population should focus on goals such as: adequate tone control, comfortable sitting and positioning, stable enlocated hips, and the correction of severe foot deformities and scoliosis.
Larger prospective studies could provide better evidence on this subject, but the ethical issues involved in light of our results could limit their feasibility.
Acknowledgments
We would like to acknowledge Joan Tornquist for her help in reviewing and editing the final manuscript, as well as Liz Barnes and Federica Barzi for their assistance with the statistical analysis.
Conflict of interest
None.
References
- 1.Stanley F, Blair E, Alberman E. Cerebral palsies: epidemiology and causal pathways. London: Mac Keith Press; 2000. [Google Scholar]
- 2.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- 3.Hanna SE, Rosenbaum PL, Bartlett DJ, Palisano RJ, Walter SD, Avery L, et al. Stability and decline in gross motor function among children and youth with cerebral palsy aged 2 to 21 years. Dev Med Child Neurol. 2009;51(4):295–302. doi: 10.1111/j.1469-8749.2008.03196.x. [DOI] [PubMed] [Google Scholar]
- 4.Beckung E, Carlsson G, Carlsdotter S, Uvebrant P. The natural history of gross motor development in children with cerebral palsy aged 1 to 15 years. Dev Med Child Neurol. 2007;49(10):751–756. doi: 10.1111/j.1469-8749.2007.00751.x. [DOI] [PubMed] [Google Scholar]
- 5.Palisano RJ, Rosenbaum P, Bartlett D, Livingston MH. Content validity of the expanded and revised Gross Motor Function Classification System. Dev Med Child Neurol. 2008;50(10):744–750. doi: 10.1111/j.1469-8749.2008.03089.x. [DOI] [PubMed] [Google Scholar]
- 6.Adolfsen SE, Ounpuu S, Bell KJ, DeLuca PA. Kinematic and kinetic outcomes after identical multilevel soft tissue surgery in children with cerebral palsy. J Pediatr Orthop. 2007;27(6):658–667. doi: 10.1097/BPO.0b013e3180dca114. [DOI] [PubMed] [Google Scholar]
- 7.Browne AO, McManus F. One-session surgery for bilateral correction of lower limb deformities in spastic diplegia. J Pediatr Orthop. 1987;7(3):259–261. doi: 10.1097/01241398-198705000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Karol LA. Surgical management of the lower extremity in ambulatory children with cerebral palsy. J Am Acad Orthop Surg. 2004;12(3):196–203. doi: 10.5435/00124635-200405000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Gough M, Eve LC, Robinson RO, Shortland AP. Short-term outcome of multilevel surgical intervention in spastic diplegic cerebral palsy compared with the natural history. Dev Med Child Neurol. 2004;46(2):91–97. doi: 10.1111/j.1469-8749.2004.tb00457.x. [DOI] [PubMed] [Google Scholar]
- 10.Rodda JM, Graham HK, Nattrass GR, Galea MP, Baker R, Wolfe R. Correction of severe crouch gait in patients with spastic diplegia with use of multilevel orthopaedic surgery. J Bone Joint Surg Am. 2006;88(12):2653–2664. doi: 10.2106/JBJS.E.00993. [DOI] [PubMed] [Google Scholar]
- 11.Soo B, Howard JJ, Boyd RN, Reid SM, Lanigan A, Wolfe R, et al. Hip displacement in cerebral palsy. J Bone Joint Surg Am. 2006;88(1):121–129. doi: 10.2106/JBJS.E.00071. [DOI] [PubMed] [Google Scholar]
- 12.Canavese F, Emara K, Sembrano JN, Bialik V, Aiona MD, Sussman MD. Varus derotation osteotomy for the treatment of hip subluxation and dislocation in GMFCS level III to V patients with unilateral hip involvement. Follow-up at skeletal maturity. J Pediatr Orthop. 2010;30(4):357–364. doi: 10.1097/BPO.0b013e3181d8fbc1. [DOI] [PubMed] [Google Scholar]
- 13.Raina P, O’Donnell M, Rosenbaum P, Brehaut J, Walter SD, Russell D, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115(6):e626–e636. doi: 10.1542/peds.2004-1689. [DOI] [PubMed] [Google Scholar]
- 14.Eisenberg S, Zuk L, Carmeli E, Katz-Leurer M. Contribution of stepping while standing to function and secondary conditions among children with cerebral palsy. Pediatr Phys Ther. 2009;21(1):79–85. doi: 10.1097/PEP.0b013e31818f57f2. [DOI] [PubMed] [Google Scholar]
- 15.Hough JP, Boyd RN, Keating JL. Systematic review of interventions for low bone mineral density in children with cerebral palsy. Pediatrics. 2010;125(3):e670–e678. doi: 10.1542/peds.2009-0292. [DOI] [PubMed] [Google Scholar]
- 16.Cusick A, McIntyre S, Novak I, Lannin N, Lowe K. A comparison of goal attainment scaling and the Canadian Occupational Performance Measure for paediatric rehabilitation research. Pediatr Rehabil. 2006;9(2):149–157. doi: 10.1080/13638490500235581. [DOI] [PubMed] [Google Scholar]
- 17.Dickinson HO, Parkinson KN, Ravens-Sieberer U, Schirripa G, Thyen U, Arnaud C, et al. Self-reported quality of life of 8–12-year-old children with cerebral palsy: a cross-sectional European study. Lancet. 2007;369(9580):2171–2178. doi: 10.1016/S0140-6736(07)61013-7. [DOI] [PubMed] [Google Scholar]
- 18.Harvey A, Graham HK, Morris ME, Baker R, Wolfe R. The Functional Mobility Scale: ability to detect change following single event multilevel surgery. Dev Med Child Neurol. 2007;49(8):603–607. doi: 10.1111/j.1469-8749.2007.00603.x. [DOI] [PubMed] [Google Scholar]
- 19.Novacheck TF, Stout JL, Tervo R. Reliability and validity of the Gillette Functional Assessment Questionnaire as an outcome measure in children with walking disabilities. J Pediatr Orthop. 2000;20(1):75–81. [PubMed] [Google Scholar]
- 20.Godwin EM, Spero CR, Nof L, Rosenthal RR, Echternach JL. The gross motor function classification system for cerebral palsy and single-event multilevel surgery: is there a relationship between level of function and intervention over time? J Pediatr Orthop. 2009;29(8):910–915. doi: 10.1097/BPO.0b013e3181c0494f. [DOI] [PubMed] [Google Scholar]
- 21.Khan MA. Outcome of single-event multilevel surgery in untreated cerebral palsy in a developing country. J Bone Joint Surg Br. 2007;89(8):1088–1091. doi: 10.1302/0301-620X.89B8.18475. [DOI] [PubMed] [Google Scholar]
- 22.Graham HK, Harvey A. Assessment of mobility after multi-level surgery for cerebral palsy. J Bone Joint Surg Br. 2007;89(8):993–994. doi: 10.1302/0301-620X.89B8.19446. [DOI] [PubMed] [Google Scholar]
- 23.Pruitt DW, Tsai T. Common medical comorbidities associated with cerebral palsy. Phys Med Rehabil Clin N Am. 2009;20(3):453–467. doi: 10.1016/j.pmr.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Damiano DL, Alter KE, Chambers H. New clinical and research trends in lower extremity management for ambulatory children with cerebral palsy. Phys Med Rehabil Clin N Am. 2009;20(3):469–491. doi: 10.1016/j.pmr.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lauder GR, White MC. Neuropathic pain following multilevel surgery in children with cerebral palsy: a case series and review. Paediatr Anaesth. 2005;15(5):412–420. doi: 10.1111/j.1460-9592.2005.01431.x. [DOI] [PubMed] [Google Scholar]
- 26.Karol LA, Chambers C, Popejoy D, Birch JG. Nerve palsy after hamstring lengthening in patients with cerebral palsy. J Pediatr Orthop. 2008;28(7):773–776. doi: 10.1097/BPO.0b013e318186bdbb. [DOI] [PubMed] [Google Scholar]
- 27.Stout JL, Gage JR, Schwartz MH, Novacheck TF. Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. J Bone Joint Surg Am. 2008;90(11):2470–2484. doi: 10.2106/JBJS.G.00327. [DOI] [PubMed] [Google Scholar]
- 28.Lee KM, Chung CY, Park MS, Lee SH, Choi IH, Cho T-J, et al. Level of improvement determined by PODCI is related to parental satisfaction after single-event multilevel surgery in children with cerebral palsy. J Pediatr Orthop. 2010;30(4):396–402. doi: 10.1097/BPO.0b013e3181da855f. [DOI] [PubMed] [Google Scholar]


