Summary
Impaired insulin signaling is central to the development of the metabolic syndrome and can promote cardiovascular disease indirectly through development of abnormal glucose and lipid metabolism, hypertension and a proinflammatory state. However, insulin action directly on vascular endothelium, atherosclerotic plaque macrophages, and in the heart, kidney, and retina has now been described, and impaired insulin signaling in these locations can alter progression of cardiovascular disease in the metabolic syndrome and affect development of microvascular complications of diabetes. Recent advances in our understanding of the complex pathophysiology of insulin’s effects on vascular tissues offer new opportunities for preventing these cardiovascular disorders.
Introduction
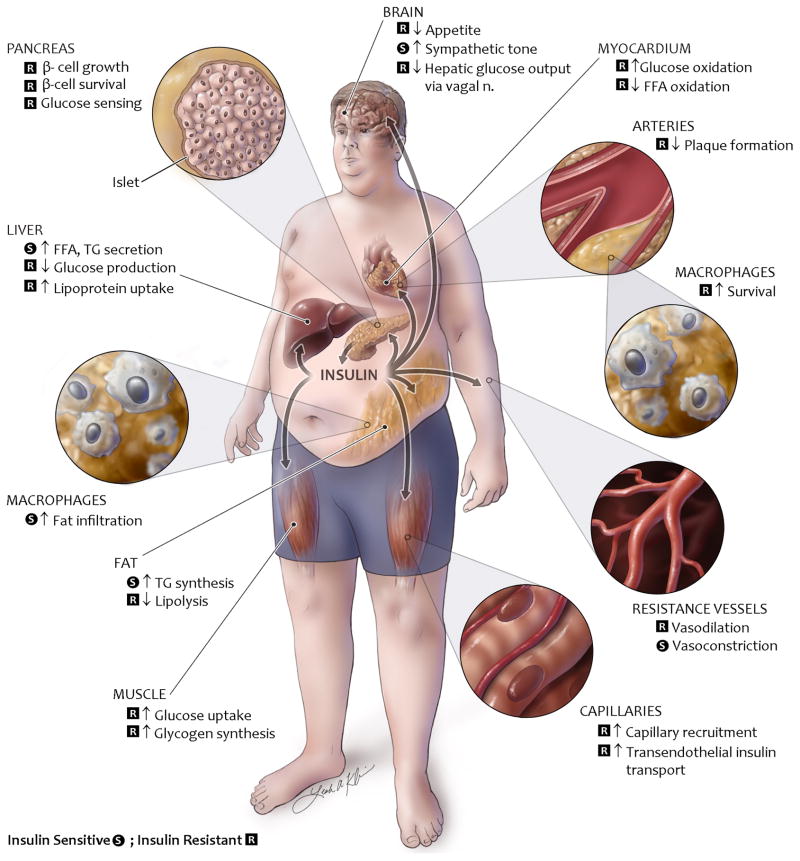
The rising prevalence of obesity worldwide is predisposing individuals to many diseases and disorders and has led to the prediction that children in America, for the first time, could have a shorter life expectancy than their parents [1]. A large part of this risk is due to the fact that obesity is a central factor in development of insulin resistance, type 2 diabetes and metabolic syndrome, all of which create an increased risk of cardiovascular disease [2]. The metabolic syndrome itself includes central obesity, impaired glucose tolerance or diabetes, hypertension, and dyslipidemia with high plasma concentrations of triglyceride and low concentrations of high density lipoprotein cholesterol, all which can contribute to cardiovascular risk [2]. Intense interest in the metabolic syndrome over the past two decades has improved awareness of the complex integrative physiology which determines the development and the consequences of this condition. The effects of insulin action at the whole body level are summarized in Figure 1. In this review, we will discuss the roles of insulin signaling and insulin resistance in a wide range of cells and tissues in the metabolic syndrome with a special focus on how they promote the associated cardiovascular complications.
Figure 1. Physiology of insulin signaling in metabolic syndrome.
Overview of the physiology of insulin signaling in the metabolic syndrome. Insulin actions which are insulin resistant in metabolic syndrome are labeled in red, whereas insulin actions which remain insulin sensitive in metabolic syndrome are labeled in green.
The pathogenesis of metabolic syndrome remains debated. However, initiation of the typical case of metabolic syndrome is due to a degree of genetic predisposition created by multiple genes coupled with a sedentary lifestyle and a diet containing excess calories. A positive energy balance leads to increased storage of fat in adipose tissue but with development of obesity, the ability of adipocytes to store triglycerides is impaired or exceeded. Consequently, fat is stored in other cell types, including in liver and skeletal muscle [3]. Ectopic lipid and their metabolites or increased concentrations of circulating free fatty acids cause insulin resistance in muscle and other tissues [3]. Concurrently, fat tissue is infiltrated with macrophages and other immune cells because of adipocyte expression of monocyte chemoattractant protein-1 and other cytokines, or in response to adipose tissue hypoxia or adipocyte death [4]. Circulating cytokines released by adipose tissue macrophages also contribute to insulin resistance in muscle, liver and other tissues. In the brain, impaired insulin signaling and compromised nutrient sensing contributes to obesity by failing to suppress appetite. Brain insulin resistance also leads to glucose intolerance by impairing the ability of insulin to suppress hepatic glucose output through innervation of the liver. Other factors almost certainly contribute, including increased insulin production and the resulting hyperinsulinemia which can itself promote insulin resistance.
At a molecular level insulin resistance can be caused by impaired insulin signaling due to increased serine phosphorylation of insulin receptor substrate-1 (IRS-1). This change causes inhibition of IRS-1 tyrosine phosphorylation, decreased binding of the downstream enzyme phosphatidylinositol 3-kinase (PI3K), and decreased phosphorylation and activation of the kinase Akt. IRS-1 can be phosphorylated on serine residues by various isoforms of protein kinase C (PKC), which are activated by the lipid intermediate diacylglycerol (DAG) [5], or by the stress kinase c-Jun N-terminal kinase when activated by proinflammatory cytokines [4] or endoplasmic reticulum (ER) stress [6]. Many other mechanisms have been proposed and their quantitative contribution to insulin resistance is still unresolved.
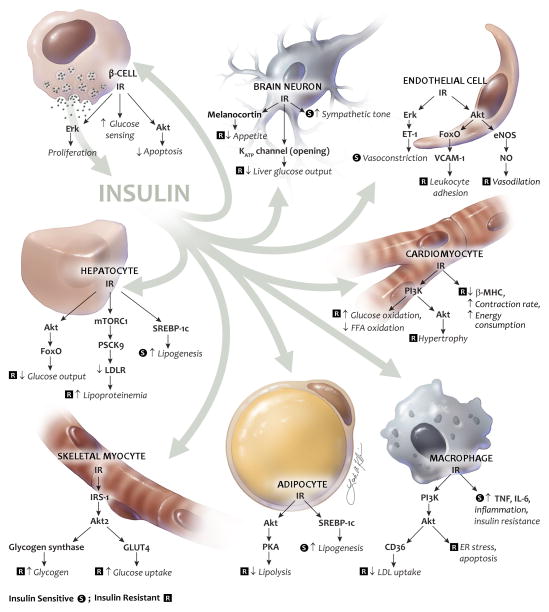
Insight into tissue-specific insulin signaling has been aided by mouse models of insulin receptor knockout restricted to certain cell types. They reveal the overall effects of insulin by loss of insulin action. However, they often do not accurately represent insulin signaling in the metabolic syndrome or other insulin resistant states where some, but not all, post-receptor insulin signaling pathways are impaired. Such selective, or mixed, insulin resistance can occur in blood vessels where insulin-stimulated activation of Erk is preserved or enhanced [7] or in the liver where insulin-stimulated activation of the transcription factor sterol regulatory element binding protein-1c (SREBP-1c) remains fully sensitive [8]. Examples of insulin action and insulin signaling which is resistant or sensitive in the metabolic syndrome are discussed further below and illustrated in Figure 1 and 2.
Figure 2. Molecular mechanisms of insulin signaling.
Important insulin signaling pathways in various cell types. Abbreviations: IR, insulin receptor; LDLR, low density lipoprotein receptor; MHC, myosin heavy chain; mTORC1, mammalian target of rapamycin complex 1; PCSK9, proprotein convertase subtilisin/kexin type 9; PKA, protein kinase A; TNF, tumor necrosis factor-α. For other abbreviations, please see text.
Insulin signaling in development of the metabolic syndrome
Altered insulin signaling pathways contribute to many aspects of the metabolic syndrome. The most important changes in insulin signaling are summarized in Figure 2 and discussed below.
Insulin signaling in adipocytes and macrophages promotes fat tissue expansion and inflammation
Adipose tissue expansion is caused by adipocyte hypertrophy rather than increased numbers of adipocytes, and large adipocytes are less sensitive to the anti-lipolytic action of insulin and express higher levels of the proinflammatory chemokine monocyte chemoattractant protein-1 [3]. Mice with adipocyte-specific knockout of the insulin receptor have a decrease in the ability of insulin to suppress lipolysis as well as impaired insulin-stimulated glucose uptake and triglyceride synthesis in adipocytes [9]. This leads to a reduction in fat mass and protection against obesity induced by a high-fat diet or hypothalamic injury [9]. However, it is possible that impaired suppression of lipolysis in combination with a preserved ability of insulin to activate fatty acid synthesis through SREBP-1c may contribute to adipose tissue expansion during development of obesity.
A major component of obesity-related insulin resistance is the establishment of a chronic inflammatory state with invasion of white adipose tissue by mononuclear cells. These cells release pro-inflammatory cytokines which promote insulin resistance in skeletal muscle, liver, and other tissues [4]. Deletion of the insulin receptor in myeloid cells (monocytes, macrophages, and neutrophils) causes reduced accumulation of macrophages in white adipose tissue during high-fat feeding due to an impairment of matrix metalloproteinase-9 expression and activity in these cells [10]. As a consequence, these animals have reduced circulating levels of tumor necrosis factor-α, reduced activation of stress kinases in muscle, and are protected from the development of insulin resistance upon high fat feeding [10]. Thus insulin action in myeloid cells plays an unexpected, but important, role in the regulation of macrophage invasion into white adipose tissue and the development of obesity-associated insulin resistance.
Impaired insulin signaling in muscle causes insulin resistance
Skeletal muscle is the main tissue accounting for insulin-stimulated glucose disposal. In healthy people subjected to a euglycemic, hyperinsulinemic clamp approximately 80% of glucose is taken up by skeletal muscle and used for glycogen synthesis and glycolysis [11]. In insulin resistance, insulin signaling through IRS-1, PI3K and Akt is decreased which ultimately results in a decrease in translocation of the glucose transporter GLUT4 to the plasma membrane and impaired insulin-stimulated glucose transport into the cell [11].
Mice with muscle-specific insulin receptor knockout have profound insulin resistance in muscle, but glucose tolerance stays normal since insulin-independent glucose uptake in muscle remains intact along with increased glucose uptake in fat tissue. As a result, fat mass is increased in these animals and insulin-stimulated glucose uptake in fat is increased by 3-fold [12].
Hepatocyte insulin resistance leads to increased glucose output and dyslipidemia
Insulin action on hepatocytes suppresses gluconeogenesis and glycogenolysis and increases glycogen synthesis, resulting in decreased glucose output from the liver. Insulin resistance in the liver is the major cause of fasting hyperglycemia in the metabolic syndrome [11]. In mice with insulin receptor deletion in hepatocytes, insulin suppression of hepatic glucose output is completely lost. At a molecular level this is represented by increased expression of the gluconeogenic enzymes phosphoenolpyruvate carboxykinase and glucose 6-phosphatase and decreased expression of enzymes which regulate glycogen synthesis and glycolysis, including glucokinase and pyruvate kinase [13].
Dyslipidemia of the metabolic syndrome and type 2 diabetes is characterized by elevated plasma concentrations of fatty acids and triglyceride, relatively low plasma concentrations of low density lipoprotein (LDL), and small, dense LDL. Regulation of circulating lipids through insulin action on liver is affected by insulin resistance and hyperinsulinemia in several ways. First, insulin increases synthesis of fatty acids and triglyceride by activating SREBP-1c, which in turn increases transcription of lipogenic enzymes, including acetyl-coenzyme A carboxylase and fatty acid synthase. Unlike signaling through Akt and FoxO, this pathway appears to be unimpaired, or at least less impaired, in the metabolic syndrome [8]. As a result, the hyperinsulinemia associated with metabolic syndrome causes increased circulating levels of free fatty acids and triglyceride. Hepatic insulin resistance also contributes to hyperlipidemia through downregulation of the LDL receptor (LDLR) [14], at least in part through an impaired ability of insulin to decrease transcription of proprotein convertase subtilisin/kexin type 9 (PCSK9) which promotes post-translational downregulation of the LDLR [15]. Therefore, liver insulin resistance causes decreased clearance of LDL and very low density lipoprotein (VLDL) [14]. Finally, absence of insulin receptors in hepatocytes increases secretion apolipoprotein B, the main apolipoprotein in LDL and VLDL [14].
Insulin resistance in the hypothalamus contributes to fasting hyperglycemia and impaired appetite regulation
Insulin suppression of hepatic glucose output is also controlled by insulin action in the hypothalamus of the brain which leads to a suppression of hepatic glucose output mediated by the vagal nerve. This effect can be blocked by injecting a KATP channel blocker in the mediobasal hypothalamus, by gene knockout of a subunit of KATP channels, or by resection of the hepatic branch of the vagal nerve [16]. Central insulin action also promotes adipose tissue expansion through sympathetic innervation of adipose tissue [17]. In addition, insulin suppresses appetite by activating neurons in the arcuate nucleus in the hypothalamus. At least part of this anorexic effect is mediated by melanocortin [18], and it is blunted in obesity.
Insulin resistance in β-cells plays a role in progression of glucose intolerance to type 2 diabetes
Whether mild to moderate insulin resistance progresses to diabetes depends on the ability of pancreatic cells to maintain insulin levels high enough to overcome the insulin resistance and limit hyperglycemia [19]. Insulin secretion and β-cell mass is upregulated in response to periodic hyperglycemia through glucose sensing by β-cells, resulting in increased insulin secretion and increased β-cell mass [20]. Conversely, β-cells with insulin receptor knockout have decreased DNA and protein synthesis and slower growth in response to increased glucose concentrations [20]. Mice with insulin receptor knockout in β-cells also lose first-phase insulin secretion and develop glucose intolerance [21]. These mice have exacerbated glucose intolerance after developing diet-induced obesity with almost complete failure of compensatory β-cell hyperplasia [22].
Endothelial cell insulin resistance can limit insulin delivery to target tissues
Insulin action and insulin resistance in endothelial cells can play a role in glucose homeostasis through at least two potential mechanisms: effects of insulin to induce vasodilatation and the role of transendothelial transport in delivery of insulin to its target tissues. Studies in humans first demonstrated that insulin-stimulated vasodilation could be a significant contributor to insulin-stimulated glucose uptake [23] by a mechanism which could be blocked by an inhibitor of nitric oxide (NO) synthase and which was impaired in people with obesity or type 2 diabetes [24]. Subsequent studies have suggested that an effect of insulin resulting in an increased number of perfused capillaries in a given tissue, a phenomenon known as capillary recruitment, may be more important for glucose tolerance than an insulin effect on total blood flow [24]. In rats subjected to a euglycemic hyperinsulinemic clamp where plasma insulin concentrations were increased by 2-fold without changing blood glucose there was a 2-fold increase in hindlimb blood volume, indicating capillary recruitment. This change was seen as quickly as 5 minutes after start of the insulin infusion, i.e. before changes in blood flow occurred [25]. Capillary recruitment can be blocked by inhibitors of NO synthase [25] and is blunted in obese rats [24]. Insulin-stimulated capillary recruitment could affect muscle glucose uptake by redistributing muscle perfusion from a non-nutritive to a nutritive route. Capillary recruitment could also contribute to increased delivery of insulin to muscle and increase the endothelial surface available for transendothelial insulin transport.
Studies in dogs using labeled insulin and microdialysis of muscle interstitial fluid indicate that there is a significant delay of insulin delivery to the interstitium created by passage through the vascular wall [26]. While some experiments suggest that this transfer of insulin from the intravascular to extravascular space occurs by passive diffusion, several lines of evidence support the notion that transendothelial transport of insulin is dependent on insulin receptors. This concept was pioneered using tissue culture studies which showed that transport of labeled insulin across monolayers of cultured endothelial cells was saturable because it could be blocked by excess unlabeled insulin, and that the carrier could be blocked by insulin receptor antibodies [27]. Ten minutes after a bolus of labeled insulin is injected, its localization in muscle is primarily in endothelial cells [28]. Further, cell culture studies have shown that transendothelial insulin transport requires endothelial insulin signaling and may be mediated by a vesicular mechanism involving caveolin-1 [28]. In mice with knockout of IRS-2 targeted to endothelial cells, endothelial cell insulin signaling, capillary recruitment, insulin delivery to interstitium, and gluocose tolerance are impaired, and this correlates with a decreased insulin-stimulated muscle glucose uptake in vivo, but not ex vivo where muscle perfusion does not operate [29]. Given these changes it is surprising that glucose tolerance is not impaired in mice with endothelial cell insulin receptor knockout [30]. Hypothetically, this discrepancy could be explained by insulin-stimulated occlusion of non-nutritive blood flow through induction of endothelin-1 independently of signaling through IRS proteins. This would contribute to glucose disposal in endothelial cell IRS-1 knockout mice, but be absent in endothelial cell insulin receptor knockout mice.
Hyperinsulinemia may cause sympathetic overactivity and hypertension
Obesity is associated with overactivity of the sympathetic nervous system, which may contribute to glucose intolerance by stimulating gluconeogenesis and lipolysis through sympathetic innervation of liver and fat, respectively [31]. Insulin action also has a role in control of sympathetic activity, which increases in response to raised insulin levels following a mixed meal or during a euglycemic hyperinsulinemic clamp and decreases with fasting. Insulin can activate sympathetic nerve activity by acting on neurons in the arcuate nucleus of the hypothalamus [32]. In obese individuals, sympathetic nerve activity is increased under basal conditions, but does not increase further during a euglycemic hyperinsulinemic clamp as seen in insulin sensitive control subjects [33]. Sympathetic overactivity in obesity can cause hypertension through vasoconstrictor effects mediated by sympathetic innervation of resistance vessels or the kidney. The latter can result in glomerular hyperfiltration, increased renal sodium reabsorption, and increased renin release [31]. Increased sympathetic outflow can also contribute to left ventricular diastolic dysfunction, left ventricular hypertrophy, heart failure, and cardiac arrhythmia [31].
Insulin signaling in tissues affected by cardiovascular disease and microvascular complications
Changes in insulin signaling is central to development of the metabolic syndrome as discussed above. These disturbances can play a role in promoting cardiovascular disease in the metabolic syndrome and in developing vascular complications of diabetes by creating an environment of hyperglycemia, dyslipidemia, inflammation and hypertension. However, abnormal insulin signaling in arteries and in vascular and other cells in the heart, kidney, and retina also contributes to disease in these organs.
Endothelial cell insulin resistance increases vascular wall inflammation and atherosclerosis
Insulin action directly on vascular endothelial cells affects endothelial function beyond regulating blood flow or capillary recruitment. Conditional knockout of the insulin receptor in endothelial cells causes a 2- to 3-fold increase in atherosclerotic lesion size in apolipoprotein E null mice. This large effect occurs without changes in glucose tolerance, insulin sensitivity, cholesterol levels, or blood pressure [34]. Therefore, the increased atherogenesis in this model can be attributed to insulin action directly on endothelial cells rather than effects mediated through systemic parameters. The accelerated atherosclerosis in mice with endothelial cell insulin receptor knockout is preceded by a dramatic increase in leukocyte rolling and adhesion to endothelium and an increase in expression of vascular cell adhesion molecule-1 (VCAM-1). Although NO-mediated vasorelaxation is impaired in these mice, insulin-stimulated downregulation of VCAM-1 in endothelial cells is not blocked by inhibitors of NO synthase, suggesting that insulin signaling independent of NO is responsible for this effect [34].
Similar endothelial cell abnormalities are likely present in the metabolic syndrome. Thus, impaired endothelium-dependent vasodilation is present in people with obesity [35] and type 2 diabetes [36]. Furthermore, a blunted ability of insulin to activate Akt and endothelial NO synthase (eNOS) is observed in aorta of rats with obesity-associated insulin resistance [37] and in mice with obesity induced by a high-fat diet [29, 38] or by leptin deficiency [29]. Endothelial cell insulin resistance develops through similar mechanisms as in other tissues, including activation of toll-like receptor 4 by free fatty acids [38], signaling activated by tumor necrosis factor-α or other proinflammatory cytokines [39], or downregulation of IRS proteins secondary to hyperinsulinemia [29].
Insulin regulates certain genes by activation of Akt which phosphorylates FoxO, causing this transcription factor to be excluded from the nucleus. In LDLR knockout mice with deletion of all 3 major FoxO isoforms in endothelial cells, atherosclerosis is reduced by a remarkable 77% [40]. In these animals, there is an increase in NO production and a decrease in production of reactive oxygen species, activation of nuclear factor κB, and expression of intercellular adhesion molecule-1, VCAM-1, and proinflammatory cytokines [40]. These data suggest that endothelial cell genes which are regulated by FoxO could be good potential drug targets for prevention of atherosclerosis in people with the metabolic syndrome.
Insulin resistance in macrophages promotes necrotic core formation in atherosclerosis
Loss of insulin action in macrophages may affect atherosclerosis progression by increasing the expression of CD36 or scavenger receptor A leading to increased uptake of modified lipoprotein [41] or by inhibiting proinflammatory activation [42]. However, the overall effects on atherosclerotic lesion growth appears to be modest, based on studies of mice with conditional deletion of the insulin receptor in macrophages [42] or mice with bone marrow transplantation using cells from mice with systemic defects in insulin signaling [41, 43]. Insulin resistance in macrophages, however, promotes formation of a necrotic core in atherosclerotic plaques by enhancing macrophage apoptosis [41]. This is an important event in advanced atherosclerosis because exposure of the necrotic core to circulating blood in the event of plaque rupture can precipitate thrombosis, leading to unstable angina pectoris, transitory cerebral ischemia, stroke or myocardial infarction [44]. Proapoptotic pathways can be activated in insulin resistant macrophages because they are more susceptible to ER stress and activation of the unfolded protein response [41].
Cardiac insulin resistance causes substrate inflexibility and mitochondrial uncoupling
Myocardial metabolism is changed in obesity. Isolated working hearts from ob/ob mice have higher rates of fatty acid oxidation and lower rates of glucose oxidation than hearts from normal lean mice [45]. Hearts from obese animals also express higher levels of the β isoform of myosin heavy chain, which is dominant in fetal life and upregulated during remodeling in heart failure. Furthermore, the myocardium in obesity is unable to adapt to changes in substrate availability and is metabolically inefficient. In hearts from lean wildtype mice, insulin increases glycolysis and glucose oxidation and reduces oxidation of free fatty acids, but these effects are blunted in ob/ob mice, in particular during high concentrations of fatty acids [45].
Mice with knockout of the insulin receptor have confirmed this role of insulin in cardiomyocyte function. Mice with conditional knockout of the insulin receptor driven by the muscle creatine kinase promoter were found to have up to a 28% reduction in heart size [46]. This can be explained by a similar reduction in cardiomyocyte volume. Adult cardiomyocytes from the knockout mice express higher levels of GLUT4 and of the fetal isoform of myosin heavy chain and they have lower expression of GLUT1 and genes encoding for enzymes that catalyze mitochondrial β-oxidation. These mice have mitochondrial uncoupling and oxidative stress related to reduced oxidative phosphorylation of fatty acid oxidation and reduced flux through the citric acid cycle [47]. Surprisingly, insulin increased glucose oxidation and glycogenolysis in mice with cardiomyocyte insulin receptor knockout, indicating that insulin signaling in non-cardiomyocytes can regulate cardiomyocyte metabolism by paracrine signaling [46]. Mice with cardiomyocyte insulin receptor knockout under control of the α-myosin heavy chain promoter had similar findings although downregulation of genes in the electron transport chain was more predominant than genes involved in mitochondrial β-oxidation [48]. Cardiac systolic function in mice with cardiomyocyte knockout of the insulin receptor is only mildly impaired with reductions in ejection fraction of 12% or less [46, 48]. However, it is likely that the changes in metabolic substrate inflexibility and increased mitochondrial production of oxidants caused by cardiomyocyte insulin resistance can contribute to development of heart failure in the metabolic syndrome.
Insulin receptor signaling in cardiac muscle in insulin resistant states is partially compensated for by insulin-like growth factor-1 (IGF-1) receptor signaling. Mice with conditional knockout of both the insulin and IGF-1 receptor controlled by the muscle creatine kinase promoter die within the first 3 weeks of life due to cardiomyopathy and heart failure [48]. These mice also exhibit a coordinated down-regulation of genes encoding components of the electron transport chain and mitochondrial fatty acid β-oxidation pathways and altered expression of contractile proteins. Thus, some combination of insulin and IGF-1 receptor signaling is required for normal cardiac metabolism and function.
Retinal and glomerular insulin action may influence microvascular complications of diabetes
The course of microvascular complications of diabetes, particularly retinopathy and nephropathy, may be affected by changes in insulin action directly on the affected tissue. In the retina, insulin receptors are expressed primarily in photoreceptor cells and blood vessels [49]. Insulin can act as a survival factor for retinal neurons and knockout of the insulin receptor in rod photoreceptors decreases survival of these cells [50]. Insulin may also promote proliferative retinopathy, either by upregulating vascular endothelial growth factor (VEGF) [51] or through direct effects on endothelial cells. Thus, knockout of the insulin receptor in endothelial cells reduced angiogenesis during retinal ischemia in mice by almost 60%, and a similar, but lesser, effect was observed after knockout of the IGF-1 receptor in endothelial cells [30]. This potentially important protective effect of endothelial insulin resistance in retinopathy needs further study.
In the kidney, podocytes are an important component in the renal glomerular filtration barrier, and recent data have shown that insulin action on podocytes can be an important survival signal for this cell type. Mice with podocyte-specific knockout of the insulin receptor have normal kidneys during the first few weeks of life [52]. However, in young adulthood they develop regression of the podocyte foot processes which are important in plasma filtration. They also exhibit increased production of basal membrane proteins, podocyte apoptosis, and albuminuria, all changes which can be seen in diabetic nephropathy. Some mice even develop scarred kidneys and mild deterioration of kidney function despite maintaining normoglycemia [52]. Renal glomeruli have impaired insulin signaling in rat models of both type 1 and 2 diabetes [53], but whether insulin resistance in glomerular cells contributes to diabetic nephropathy remains to be determined.
Conclusion
Research on insulin receptor signaling using tissue-specific gene manipulation in mice and other methods has provided important insights into insulin action and revealed insulin effects in tissues that a decade or two ago were considered non-responsive to insulin. New knowledge about tissue-specific insulin signaling and selective insulin resistance has helped us appreciate the complexity of insulin resistance in the metabolic syndrome and related disorders. These insights have practical consequences. First, insulin sensitizers would theoretically have better profiles of action if they improved insulin resistance in tissues regulating glucose and lipid metabolism as well as in endothelium and other vascular tissue where impaired insulin signaling is proatherosclerotic independent of metabolic effects [34]. Second, insulin analogues should be carefully evaluated for deleterious effects on insulin signaling pathways which are not affected by insulin resistance such as those pathways which promote dyslipidemia [8] or increase vascular expression of endothelin-1 [54]. Third, genes regulated by insulin signaling in vascular tissue may be candidates for drug development. For example, one study identified 21 genes in endothelial cells which were directly regulated by FoxO, many without known function in this cell type [55]. Some of these genes could be important determinants of proatherosclerotic effects of endothelial cell FoxO [40]. These concepts provide exciting new possibilities for treating the metabolic syndrome and preventing cardiovascular disease.
Acknowledgments
Dr. Rask-Madsen is supported by NIH grant EY018677 and Dr. Kahn by NIH grants DK31036, DK33201, DK55545, DK82659 and R24DK085610, as well as the Mary K. Iacocca Professorship. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
References
- 1.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, Hayflick L, Butler RN, Allison DB, Ludwig DS. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 2.Reaven GM. The metabolic syndrome: time to get off the merry-go-round? J Intern Med. 2011;269:127–136. doi: 10.1111/j.1365-2796.2010.02325.x. [DOI] [PubMed] [Google Scholar]
- 3.Guilherme A, Virbasius JV, Puri V, Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9:367–377. doi: 10.1038/nrm2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol. 2011;11:98–107. doi: 10.1038/nri2925. [DOI] [PubMed] [Google Scholar]
- 5.Samuel VT, Petersen KF, Shulman GI. Lipid-induced insulin resistance: unravelling the mechanism. Lancet. 2010;375:2267–2277. doi: 10.1016/S0140-6736(10)60408-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hotamisligil GS. Endoplasmic reticulum stress and the inflammatory basis of metabolic disease. Cell. 2010;140:900–917. doi: 10.1016/j.cell.2010.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jiang ZY, Lin YW, Clemont A, Feener EP, Hein KD, Igarashi M, Yamauchi T, White MF, King GL. Characterization of selective resistance to insulin signaling in the vasculature of obese Zucker (fa/fa) rats. J Clin Invest. 1999;104:447–457. doi: 10.1172/JCI5971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shimomura I, Matsuda M, Hammer RE, Bashmakov Y, Brown MS, Goldstein JL. Decreased IRS-2 and increased SREBP-1c lead to mixed insulin resistance and sensitivity in livers of lipodystrophic and ob/ob mice. Mol Cell. 2000;6:77–86. [PubMed] [Google Scholar]
- 9.Bluher M, Michael MD, Peroni OD, Ueki K, Carter N, Kahn BB, Kahn CR. Adipose tissue selective insulin receptor knockout protects against obesity and obesity-related glucose intolerance. Dev Cell. 2002;3:25–38. doi: 10.1016/s1534-5807(02)00199-5. [DOI] [PubMed] [Google Scholar]
- 10.Mauer J, Chaurasia B, Plum L, Quast T, Hampel B, Bluher M, Kolanus W, Kahn CR, Bruning JC. Myeloid cell-restricted insulin receptor deficiency protects against obesity-induced inflammation and systemic insulin resistance. PLoS Genet. 2010;6:e1000938. doi: 10.1371/journal.pgen.1000938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009;32 (Suppl 2):S157–163. doi: 10.2337/dc09-S302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bruning JC, Michael MD, Winnay JN, Hayashi T, Horsch D, Accili D, Goodyear LJ, Kahn CR. A muscle-specific insulin receptor knockout exhibits features of the metabolic syndrome of NIDDM without altering glucose tolerance. Mol Cell. 1998;2:559–569. doi: 10.1016/s1097-2765(00)80155-0. [DOI] [PubMed] [Google Scholar]
- 13.Michael MD, Kulkarni RN, Postic C, Previs SF, Shulman GI, Magnuson MA, Kahn CR. Loss of insulin signaling in hepatocytes leads to severe insulin resistance and progressive hepatic dysfunction. Mol Cell. 2000;6:87–97. [PubMed] [Google Scholar]
- 14.Biddinger SB, Hernandez-Ono A, Rask-Madsen C, Haas JT, Aleman JO, Suzuki R, Scapa EF, Agarwal C, Carey MC, Stephanopoulos G, Cohen DE, King GL, Ginsberg HN, Kahn CR. Hepatic insulin resistance is sufficient to produce dyslipidemia and susceptibility to atherosclerosis. Cell Metab. 2008;7:125–134. doi: 10.1016/j.cmet.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ai D, Chen C, Han S, Ganda A, Murphy AJ, Haeusler R, Thorp E, Accili D, Horton JD, Tall AR. Regulation of hepatic LDL receptors by mTORC1 and PCSK9 in mice. J Clin Invest. 2012;122:1262–1270. doi: 10.1172/JCI61919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pocai A, Lam TK, Gutierrez-Juarez R, Obici S, Schwartz GJ, Bryan J, Aguilar-Bryan L, Rossetti L. Hypothalamic K(ATP) channels control hepatic glucose production. Nature. 2005;434:1026–1031. doi: 10.1038/nature03439. [DOI] [PubMed] [Google Scholar]
- 17.Scherer T, O’Hare J, Diggs-Andrews K, Schweiger M, Cheng B, Lindtner C, Zielinski E, Vempati P, Su K, Dighe S, Milsom T, Puchowicz M, Scheja L, Zechner R, Fisher SJ, Previs SF, Buettner C. Brain insulin controls adipose tissue lipolysis and lipogenesis. Cell Metab. 2011;13:183–194. doi: 10.1016/j.cmet.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benoit SC, Air EL, Coolen LM, Strauss R, Jackman A, Clegg DJ, Seeley RJ, Woods SC. The catabolic action of insulin in the brain is mediated by melanocortins. J Neurosci. 2002;22:9048–9052. doi: 10.1523/JNEUROSCI.22-20-09048.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashcroft FM, Rorsman P. Diabetes Mellitus and the beta Cell: The Last Ten Years. Cell. 2012;148:1160–1171. doi: 10.1016/j.cell.2012.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Assmann A, Ueki K, Winnay JN, Kadowaki T, Kulkarni RN. Glucose effects on beta-cell growth and survival require activation of insulin receptors and insulin receptor substrate 2. Mol Cell Biol. 2009;29:3219–3228. doi: 10.1128/MCB.01489-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kulkarni RN, Bruning JC, Winnay JN, Postic C, Magnuson MA, Kahn CR. Tissue-specific knockout of the insulin receptor in pancreatic beta cells creates an insulin secretory defect similar to that in type 2 diabetes. Cell. 1999;96:329–339. doi: 10.1016/s0092-8674(00)80546-2. [DOI] [PubMed] [Google Scholar]
- 22.Okada T, Liew CW, Hu J, Hinault C, Michael MD, Krtzfeldt J, Yin C, Holzenberger M, Stoffel M, Kulkarni RN. Insulin receptors in beta-cells are critical for islet compensatory growth response to insulin resistance. Proc Natl Acad Sci U S A. 2007;104:8977–8982. doi: 10.1073/pnas.0608703104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Laakso M, Edelman SV, Brechtel G, Baron AD. Decreased effect of insulin to stimulate skeletal muscle blood flow in obese man. A novel mechanism for insulin resistance. J Clin Invest. 1990;85:1844–1852. doi: 10.1172/JCI114644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clark MG, Wallis MG, Barrett EJ, Vincent MA, Richards SM, Clerk LH, Rattigan S. Blood flow and muscle metabolism: a focus on insulin action. Am J Physiol Endocrinol Metab. 2003;284:E241–258. doi: 10.1152/ajpendo.00408.2002. [DOI] [PubMed] [Google Scholar]
- 25.Vincent MA, Clerk LH, Lindner JR, Klibanov AL, Clark MG, Rattigan S, Barrett EJ. Microvascular recruitment is an early insulin effect that regulates skeletal muscle glucose uptake in vivo. Diabetes. 2004;53:1418–1423. doi: 10.2337/diabetes.53.6.1418. [DOI] [PubMed] [Google Scholar]
- 26.Chiu JD, Richey JM, Harrison LN, Zuniga E, Kolka CM, Kirkman E, Ellmerer M, Bergman RN. Direct administration of insulin into skeletal muscle reveals that the transport of insulin across the capillary endothelium limits the time course of insulin to activate glucose disposal. Diabetes. 2008;57:828–835. doi: 10.2337/db07-1444. [DOI] [PubMed] [Google Scholar]
- 27.King GL, Johnson SM. Receptor-mediated transport of insulin across endothelial cells. Science. 1985;227:1583–1586. doi: 10.1126/science.3883490. [DOI] [PubMed] [Google Scholar]
- 28.Barrett EJ, Wang H, Upchurch CT, Liu Z. Insulin regulates its own delivery to skeletal muscle by feed-forward actions on the vasculature. Am J Physiol Endocrinol Metab. 2011;301:E252–263. doi: 10.1152/ajpendo.00186.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kubota T, Kubota N, Kumagai H, Yamaguchi S, Kozono H, Takahashi T, Inoue M, Itoh S, Takamoto I, Sasako T, Kumagai K, Kawai T, Hashimoto S, Kobayashi T, Sato M, Tokuyama K, Nishimura S, Tsunoda M, Ide T, Murakami K, Yamazaki T, Ezaki O, Kawamura K, Masuda H, Moroi M, Sugi K, Oike Y, Shimokawa H, Yanagihara N, Tsutsui M, Terauchi Y, Tobe K, Nagai R, Kamata K, Inoue K, Kodama T, Ueki K, Kadowaki T. Impaired insulin signaling in endothelial cells reduces insulin-induced glucose uptake by skeletal muscle. Cell Metab. 2011;13:294–307. doi: 10.1016/j.cmet.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 30.Vicent D, Ilany J, Kondo T, Naruse K, Fisher SJ, Kisanuki YY, Bursell S, Yanagisawa M, King GL, Kahn CR. The role of endothelial insulin signaling in the regulation of vascular tone and insulin resistance. J Clin Invest. 2003;111:1373–1380. doi: 10.1172/JCI15211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lambert GW, Straznicky NE, Lambert EA, Dixon JB, Schlaich MP. Sympathetic nervous activation in obesity and the metabolic syndrome--causes, consequences and therapeutic implications. Pharmacol Ther. 2010;126:159–172. doi: 10.1016/j.pharmthera.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 32.Cassaglia PA, Hermes SM, Aicher SA, Brooks VL. Insulin acts in the arcuate nucleus to increase lumbar sympathetic nerve activity and baroreflex function in rats. J Physiol. 2011;589:1643–1662. doi: 10.1113/jphysiol.2011.205575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vollenweider P, Randin D, Tappy L, Jequier E, Nicod P, Scherrer U. Impaired insulin-induced sympathetic neural activation and vasodilation in skeletal muscle in obese humans. J Clin Invest. 1994;93:2365–2371. doi: 10.1172/JCI117242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rask-Madsen C, Li Q, Freund B, Feather D, Abramov R, Wu IH, Chen K, Yamamoto-Hiraoka J, Goldenbogen J, Sotiropoulos KB, Clermont A, Geraldes P, Dall’Osso C, Wagers AJ, Huang PL, Rekhter M, Scalia R, Kahn CR, King GL. Loss of insulin signaling in vascular endothelial cells accelerates atherosclerosis in apolipoprotein E null mice. Cell Metab. 2010;11:379–389. doi: 10.1016/j.cmet.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steinberg HO, Chaker H, Leaming R, Johnson A, Brechtel G, Baron AD. Obesity/insulin resistance is associated with endothelial dysfunction. Implications for the syndrome of insulin resistance. J Clin Invest. 1996;97:2601–2610. doi: 10.1172/JCI118709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rask-Madsen C, Ihlemann N, Krarup T, Christiansen E, Kober L, Nervil Kistorp C, Torp-Pedersen C. Insulin therapy improves insulin-stimulated endothelial function in patients with type 2 diabetes and ischemic heart disease. Diabetes. 2001;50:2611–2618. doi: 10.2337/diabetes.50.11.2611. [DOI] [PubMed] [Google Scholar]
- 37.Naruse K, Rask-Madsen C, Takahara N, Ha SW, Suzuma K, Way KJ, Jacobs JR, Clermont AC, Ueki K, Ohshiro Y, Zhang J, Goldfine AB, King GL. Activation of vascular protein kinase C-beta inhibits Akt-dependent endothelial nitric oxide synthase function in obesity-associated insulin resistance. Diabetes. 2006;55:691–698. doi: 10.2337/diabetes.55.03.06.db05-0771. [DOI] [PubMed] [Google Scholar]
- 38.Kim F, Pham M, Luttrell I, Bannerman DD, Tupper J, Thaler J, Hawn TR, Raines EW, Schwartz MW. Toll-like receptor-4 mediates vascular inflammation and insulin resistance in diet-induced obesity. Circ Res. 2007;100:1589–1596. doi: 10.1161/CIRCRESAHA.106.142851. [DOI] [PubMed] [Google Scholar]
- 39.Rask-Madsen C, Dominguez H, Ihlemann N, Hermann T, Kober L, Torp-Pedersen C. Tumor necrosis factor-alpha inhibits insulin’s stimulating effect on glucose uptake and endothelium-dependent vasodilation in humans. Circulation. 2003;108:1815–1821. doi: 10.1161/01.CIR.0000091406.72832.11. [DOI] [PubMed] [Google Scholar]
- 40.Tsuchiya K, Tanaka J, Shuiqing Y, Welch CL, Depinho RA, Tabas I, Tall AR, Goldberg IJ, Accili D. FoxOs Integrate Pleiotropic Actions of Insulin in Vascular Endothelium to Protect Mice from Atherosclerosis. Cell Metab. 2012;15:372–381. doi: 10.1016/j.cmet.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Han S, Liang CP, DeVries-Seimon T, Ranalletta M, Welch CL, Collins-Fletcher K, Accili D, Tabas I, Tall AR. Macrophage insulin receptor deficiency increases ER stress-induced apoptosis and necrotic core formation in advanced atherosclerotic lesions. Cell Metab. 2006;3:257–266. doi: 10.1016/j.cmet.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 42.Baumgartl J, Baudler S, Scherner M, Babaev V, Makowski L, Suttles J, McDuffie M, Tobe K, Kadowaki T, Fazio S, Kahn CR, Hotamisligil GS, Krone W, Linton M, Bruning JC. Myeloid lineage cell-restricted insulin resistance protects apolipoproteinE-deficient mice against atherosclerosis. Cell Metab. 2006;3:247–256. doi: 10.1016/j.cmet.2006.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Galkina EV, Butcher M, Keller SR, Goff M, Bruce A, Pei H, Sarembock IJ, Sanders JM, Nagelin MH, Srinivasan S, Kulkarni RN, Hedrick CC, Lattanzio FA, Dobrian AD, Nadler JL, Ley K. Accelerated atherosclerosis in Apoe−/− mice heterozygous for the insulin receptor and the insulin receptor substrate-1. Arterioscler Thromb Vasc Biol. 2012;32:247–256. doi: 10.1161/ATVBAHA.111.240358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moore KJ, Tabas I. Macrophages in the pathogenesis of atherosclerosis. Cell. 2011;145:341–355. doi: 10.1016/j.cell.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mazumder PK, O’Neill BT, Roberts MW, Buchanan J, Yun UJ, Cooksey RC, Boudina S, Abel ED. Impaired cardiac efficiency and increased fatty acid oxidation in insulin-resistant ob/ob mouse hearts. Diabetes. 2004;53:2366–2374. doi: 10.2337/diabetes.53.9.2366. [DOI] [PubMed] [Google Scholar]
- 46.Belke DD, Betuing S, Tuttle MJ, Graveleau C, Young ME, Pham M, Zhang D, Cooksey RC, McClain DA, Litwin SE, Taegtmeyer H, Severson D, Kahn CR, Abel ED. Insulin signaling coordinately regulates cardiac size, metabolism, and contractile protein isoform expression. J Clin Invest. 2002;109:629–639. doi: 10.1172/JCI13946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boudina S, Bugger H, Sena S, O’Neill BT, Zaha VG, Ilkun O, Wright JJ, Mazumder PK, Palfreyman E, Tidwell TJ, Theobald H, Khalimonchuk O, Wayment B, Sheng X, Rodnick KJ, Centini R, Chen D, Litwin SE, Weimer BE, Abel ED. Contribution of impaired myocardial insulin signaling to mitochondrial dysfunction and oxidative stress in the heart. Circulation. 2009;119:1272–1283. doi: 10.1161/CIRCULATIONAHA.108.792101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Laustsen PG, Russell SJ, Cui L, Entingh-Pearsall A, Holzenberger M, Liao R, Kahn CR. Essential role of insulin and insulin-like growth factor 1 receptor signaling in cardiac development and function. Mol Cell Biol. 2007;27:1649–1664. doi: 10.1128/MCB.01110-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lofqvist C, Willett KL, Aspegren O, Smith AC, Aderman CM, Connor KM, Chen J, Hellstrom A, Smith LE. Quantification and localization of the IGF/insulin system expression in retinal blood vessels and neurons during oxygen-induced retinopathy in mice. Invest Ophthalmol Vis Sci. 2009;50:1831–1837. doi: 10.1167/iovs.08-2903. [DOI] [PubMed] [Google Scholar]
- 50.Rajala A, Tanito M, Le YZ, Kahn CR, Rajala RV. Loss of neuroprotective survival signal in mice lacking insulin receptor gene in rod photoreceptor cells. J Biol Chem. 2008;283:19781–19792. doi: 10.1074/jbc.M802374200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jiang ZY, He Z, King BL, Kuroki T, Opland DM, Suzuma K, Suzuma I, Ueki K, Kulkarni RN, Kahn CR, King GL. Characterization of multiple signaling pathways of insulin in the regulation of vascular endothelial growth factor expression in vascular cells and angiogenesis. J Biol Chem. 2003;278:31964–31971. doi: 10.1074/jbc.M303314200. [DOI] [PubMed] [Google Scholar]
- 52.Welsh GI, Hale LJ, Eremina V, Jeansson M, Maezawa Y, Lennon R, Pons DA, Owen RJ, Satchell SC, Miles MJ, Caunt CJ, McArdle CA, Pavenstadt H, Tavare JM, Herzenberg AM, Kahn CR, Mathieson PW, Quaggin SE, Saleem MA, Coward RJ. Insulin signaling to the glomerular podocyte is critical for normal kidney function. Cell Metab. 2010;12:329–340. doi: 10.1016/j.cmet.2010.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mima A, Ohshiro Y, Kitada M, Matsumoto M, Geraldes P, Li C, Li Q, White GS, Cahill C, Rask-Madsen C, King GL. Glomerular-specific protein kinase C-beta-induced insulin receptor substrate-1 dysfunction and insulin resistance in rat models of diabetes and obesity. Kidney Int. 2011;79:883–896. doi: 10.1038/ki.2010.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rask-Madsen C, King GL. Mechanisms of Disease: endothelial dysfunction in insulin resistance and diabetes. Nat Clin Pract Endocrinol Metab. 2007;3:46–56. doi: 10.1038/ncpendmet0366. [DOI] [PubMed] [Google Scholar]
- 55.Paik JH, Kollipara R, Chu G, Ji H, Xiao Y, Ding Z, Miao L, Tothova Z, Horner JW, Carrasco DR, Jiang S, Gilliland DG, Chin L, Wong WH, Castrillon DH, DePinho RA. FoxOs are lineage-restricted redundant tumor suppressors and regulate endothelial cell homeostasis. Cell. 2007;128:309–323. doi: 10.1016/j.cell.2006.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]