Abstract
The popularity of day case surgical procedures has increased immensely over the last few years. Though various techniques are available for carrying out day-case anesthesia, preference for a technique depends upon the type of procedure, patient profile, associated co-morbidities, available infrastructure and back-up facilities, monitoring devices and comfort of the attending anesthesiologist with the technique. Day-case spinal anesthesia for ambulatory surgery has gained a wider acceptance and numerous drugs are available for use in loco-regional anesthesia. Articaine is one such amide local anesthetic drug which is increasingly being used in day care surgeries. Properties of articaine such as faster onset, shorter elimination time and rapid recovery from sensory and motor blockade make it a very useful agent in local and regional anesthesia for day care surgical procedures. This article aims to review these properties of articaine so as to evaluate how useful articaine can be for ambulatory surgical procedures.
Keywords: Articaine, Bupivacaine, Day-care surgery, Lignocaine, Neuraxial anesthesia, Prilocaine, Regional anesthesia
Introduction
The increasing popularity of day case surgical procedures has been made possible by a variety of factors such as development of preanesthetic out-patient departments (OPDs), anesthetic techniques to reduce emesis, availability of better modern monitoring devices to assess recovery and short acting anesthetic drugs. People of all age groups prefer surgery on outpatient basis and desire to return home early. Other potential benefits include minimal occupancy of hospital beds, decrease in incidence of nosocomial infections, lower cost-benefit ratio and early resumption of professional and social activities.[1]
The popularity of spinal anesthesia in day care surgeries has also seen a spurt in the recent years with availability of many short acting anesthetics and modernization of regional anesthetic techniques.[2,3] For subarachnoid block, lignocaine was widely used as a short acting local anesthetic but it fell into disrepute after reports of transitional neurological syndrome following its use. These symptoms were probably due to neurotoxicity from high concentration used for spinal anesthesia.[4,5]
Articaine, a short acting amide local anesthetic has already gained immense popularity in dental anesthesia. Numerous studies have been carried out and are underway to prove its efficacy in regional and neuraxial anesthesia for day-case surgical procedures. The aim of this article is to review the clinical pharmacology of articaine as well as assess its various potential uses in loco-regional anesthesia for ambulatory surgical procedures. Plain articaine was approved for clinical use by US Food and Drug Administration in March 2006 whereas the combination of articaine and epinephrine was approved much earlier.
Pharmacology
Articaine, a 4-methyl-3(2-[propylamino] propionamido)-2-thiophenecarboxylic acid, methyl ester hydrochloride, originally named carticaine was first prepared by Rusching et al in 1969. It entered clinical practice in Germany in 1976 under the changed name of articaine.[6] It is the only amide local anesthetic that contains a thiophene ring and an additional ester ring [Figure 1].[6,7] Its molecular weight is 320.84. The thiophene ring increases its lipid solubility.[1,2] It has a pKa of 7.8 similar to that of lignocaine while that of bupivacaine is 8.1.[1] It is highly diffusible and penetrates tissues effectively. 95% is plasma protein bound. The presence of both an amide and an ester linkage minimizes the risk of overdose leading to toxic reaction as its biotransformation occurs both in the plasma (hydrolysis by plasma esterase) and the liver (hepatic microsomal enzymes).[8] Metabolism is initiated by hydrolysis of the carboxylic acid ester groups to generate free carboxylic acid. Articainic acid is the primary metabolite, or M1.[9] Additional inactive metabolites, or M2, have been detected. Elimination is through the kidneys. 5 to 10% is excreted unchanged and 89% as metabolites (M1 87% and M2 2%).[10] The elimination half life of most amide local anesthetics is 90 minutes while that of articaine is 27 minutes.[8] It was first used clinically in dentistry and is the most common local anesthetics used in dentistry today.
Figure 1.
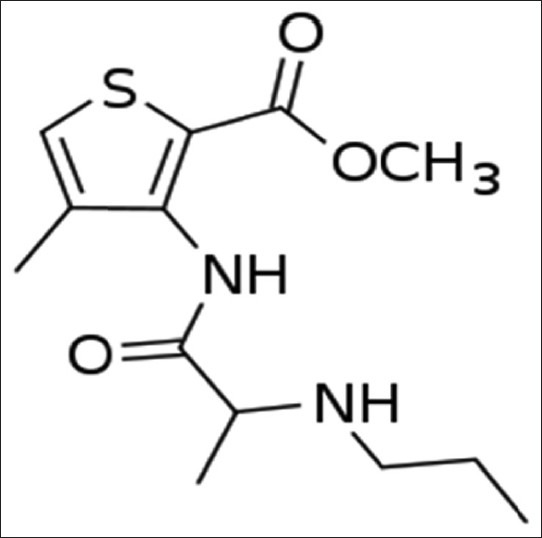
Chemical structure of articaine
Mechanism of action
Articaine acts by inhibition of nerve impulse conduction due to blockade of sodium channels.[1] Addition of epinephrine causes local vasoconstriction, slowing its absorption and increasing the duration of action. It is clinically used in 4% concentration.[1] The onset of action of 4% articaine with 1:200000 epinephrine is 1.5-1.8 minutes for maxillary infiltration and 1.4-3.6 minutes for inferior alveolar nerve block.[7,8] In a study comparing the effects of ropivacaine and articaine in infiltration anesthesia in dentistry, the duration of action and soft tissue anesthesia was observed to be 63.7 and 195.2 minutes, respectively with articaine. Complete anesthesia with articaine lasts for approximately 1 hour for infiltrations and up to approximately 2 hours for nerve block.[11,12] Surprisingly, it has been observed that patients receiving 4% articaine with 1:100,000 epinephrine, had a significantly earlier onset of anesthetic effect as compared to 4% plain articaine (7.2 minutes vs. 9.2 minutes; P =.001) Even the duration of soft tissue anesthesia has been observed to be significantly longer in patients receiving 4% articaine with epinephrine as compared to 4% plain articaine (3.8 hours vs. 2.5 hours; P <.0001).[13]
Adverse effects
There are no serious reported adverse effects. Minor adverse events include post-procedural pain, headache, facial edema; infections, gingivitis and transient paresthesia.[1] These effects are similar to those of lignocaine and occur with similar frequency in both. Articaine has a very low immunogenic potential. Allergic reactions are rare. Presence of antioxidant sodium bisulphite and antibacterial preservative methylparaben in some commercially available preparations of articaine with epinephrine can cause allergic reactions such as edema, urticaria, erythema and anaphylactic shock.[14] Some local anesthetics can cause methemoglobinemia but articaine is not associated with any increase in the levels of methemoglobin.[15] Overdose can cause unconsciousness, apnoea, hypotension, hypoxia, bradycardia and may initiate seizure activity.[16] The overall incidence of adverse effect with articaine 4% (4 % with 1:100,000 epinephrine) is 22% as compared to 20% for lignocaine (2% with 1:100,000 epinephrine).[8]
Dose
The maximum dose of articaine with epinephrine, for an adult patient, is 500 mg (6.6-7 mg/kg), which is the same as for lignocaine.[8] Articaine is available as 4% solution. In a randomized, prospective double blind study involving 40 patients with irreversible pulpitis, 4% articaine was compared with 2% lignocaine for maxillary buccal infiltration in posterior teeth. The efficacy of 4% articaine was superior to that of 2% lignocaine for buccal infiltration.[17]
In another prospective randomized double blind study, 4% articaine with adrenaline was compared with 2% lignocaine with adrenaline, in 57 patients, for assessing the degree of pulpal anesthesia in inferior alveolar nerve block. Similar pulpal anesthesia as achieved with 4% articaine as by use of 2% lignocaine.[18]
Contraindications
Although, articaine is assumed to be a safe local anesthetic, a few contraindications to its use in clinical practice are:
Patients allergic to amide-type anesthetics
Patients allergic to metabisulfites (preservative present in the formula to extend the life of the epinephrine). There is no cross-allergenicity between sulphites (preservatives), sulphur, and the “sulpha”-type antibiotics[19]
Articaine is not contraindicated in patients with sulfa allergies; there is no cross-allergenicity between articaine's sulphur-bearing thiophene ring and sulfonamides.[20]
To prevent majority of adverse effects associated with the use of Articaine, methylparaben is no longer present in any dental local anesthetic formula available in North America.[21]
Articaine for day care surgical procedures
4% articaine with 1:1,00,000 epinephrine and 2% lignocaine with 1:1,00,000 epinephrine have similar efficacy. Studies have shown that articaine is comparable to other local anesthetics in its anesthetic efficacy during dental procedures.[6] The time of onset and duration of anesthesia, using 4% articaine with 1:200000 epinephrine for maxillary nerve block, is comparable with other similar agents.[12,22]
Efficacy in dental procedures
Articaine is widely used in Germany, Canada and many other countries.[16] It is used for maxillary and mandibular infiltrations and block anesthesia for routine dental treatments.-[8] The reasons for its popularity are fast onset, short duration of action, good periosteal penetration and low degree of toxicity.[23,24] However, pediatric patients pose a difficulty, especially those with extensive restoration needs. Articaine should not be used children < 4years as they are at high risk of overdose. In addition, the children requiring extensive treatment are frequently sedated. The addition of depressant effects of high blood levels of local anesthetic to the depressant effects of sedatives increases the incidence and severity of overdose reactions. Meticulous dose calculation is required so as not to exceed the maximum recommended dose for each patient. High blood levels can be avoided by spreading the dose injected over the entire period of single treatment rather than injecting the whole dose at the beginning. Negative aspiration should be carried out each time one injects and very extensive procedures should not be carried out in single sittings.[8]
Ropivacaine is increasingly used for regional anesthesia as it has a higher safety margin. A comparative evaluation of 0.55% ropivacaine with 4% articaine was carried out in patients administered maxillary infiltration anesthesia undergoing dental procedures with emphasis on efficacy, onset time and duration of anesthesia and a possible effect on cardiovascular parameters. The mean onset time of anesthesia was significantly shorter for ropivacaine (2.22 minutes) as compared to articaine (4.08 minutes) (P < 0.05) and duration of anesthesia was significantly longer for ropivacaine (79.2 minutes) when compared with articaine (63.7 minutes) (P < 0.05). Surprisingly, the impact on cardiovascular parameters was significant with ropivacaine as mean blood pressure and mean heart rate were significantly higher in patients who were administered ropivacaine as compared to patients who were administered articaine. (P < 0.05).[25]
Success of Articaine in regional and neuraxial anesthesia
Articaine when used for brachial plexus block and for epidural block has a faster onset of action and a slightly shorter duration of action than lignocaine.[26] Subarachnoid blocks using hyperbaric articaine have a similar short lasting action as with hyperbaric lignocaine. However, when used for spinal anesthesia, the onset of action is faster with articaine as compared to hyperbaric tetracaine and hyperbaric or hypobaric bupivacaine. The quicker onset and rapid recovery time due to faster elimination weighs in favor of the potential use of articaine in day care surgeries such as arthroscopy (shoulder, knee), hand and foot surgery. The penetration of articaine through bone and soft tissues is much better and rapid as compared to other local anesthetics. [24] The side effects of articaine are less.[26] Recovery of both motor as well as sensory block is rapid allowing early ambulation (approximately 2 hours).[26] There is a lack of any dose response relationship which may be due to rapid vascular uptake of articaine and its inactivation by ester hydrolysis.[24] When used intrathecally, the sensory and motor block develops faster with articaine compared to lignocaine while the duration of both sensory as well as motor block was similar.[27] Intrathecal articaine has a shorter duration of surgical anesthesia as compared to other local anesthetics.[28] Kozlov et al. compared hyperbaric articaine with hyperbaric bupivacaine for spinal anesthesia and found that onset of both sensory and sympathetic block was faster with articaine.[29] Hypotension occurred early and more frequently with articaine.[13] Since lignocaine has a high incidence of neurotoxicity, articaine may be an alternative for short acting (ambulatory) spinal anesthesia. However, the potential for neurotoxicity with articaine is yet not completely known. Residual paresthesia or dysesthesia after dental anesthesia has raised concerns regarding possible neurotoxicity with articaine.[14] Some research points to needle trauma as the cause of the paresthesia events.[30]
Administration of subarachnoid block with hyperbaric bupivacaine is very common but studies regarding the use of hyperbaric articaine for spinal anesthesia are very few. It is assumed that the properties of articaine such as rapid onset, faster clearance and predictable duration of action can be judiciously used for day case spinal anesthesia. In a study, intrathecal hyperbaric articaine (84 mg) was compared with intrathecal hyperbaric bupivacaine (7mg) plus 10mcg of fentanyl in patients undergoing inguinal herniorrhaphy. Sensory block up to T-4 level was achieved with articaine in all the patients whereas it could not be reached in seven out of 40 patients in bupivacaine group. Patients who were administered articaine had a significantly faster median time of onset of surgical anesthesia (median time 4 minutes (range 2-20)) as compared to patient population who were given bupivacaine and fentanyl. Similarly median recovery time from the weaning of the effect of sensory block was significantly shorter (P = 0.002) in group receiving articaine (2.5 hours) as compared to patients receiving bupivacaine and fentanyl (3 hours). Other significant observations were the minimal need for changing the position of the table to achieve the desired level of anesthesia and a need for a little higher dose of ephedrine in the articaine group to control hypotension.[31]
The faster onset and shorter duration of action of articaine was the basis for its comparison with bupivacaine when administered intrathecally in patients undergoing day case lower limb surgery. Intrathecal hyperbaric articaine (80mg) was compared with plain bupivacaine (15mg) with emphasis on recovery from motor block as the primary outcome measure while secondary outcome included: onset of sensory and motor block, maximum spread of sensory block, time to micturition, discharge from the hospital and any associated complications. Median time to complete regression of motor blockade in articaine group was 101 minutes as compared to 307 minutes in the bupivacaine group (P < 0.0005). Among the secondary outcome measures, spontaneous micturition occurred after 257 minutes in articaine group as compared to 350 minutes in bupivacaine group (P < 0.0005) while to time to discharge was significantly earlier (P < 0.0005) in the articaine group (300 minutes) as compared to bupivacaine group (380 minutes). Articaine possesses a good potential to be used as day care regional anesthetic.[32]
In a double blind randomized trial among patients undergoing day-care knee arthroscopy, plain articaine (50mg) was compared with plain prilocaine (50 mg) for spinal anesthesia as both these agents are short acting anesthetics with faster onset of action and rapid cessation of anesthetic effect as well. Mean time to full motor function was significantly (P < 0.001) earlier with articaine (140 minutes) as compared to prilocaine (184 minutes). Among the secondary outcome mean time to spontaneous voiding was significantly shorter with articaine (184 minutes) when compared to prilocaine (227 minutes). The study established that surgical anesthesia was comparable with both articaine and prilocaine but faster recovery of motor function and early spontaneous voiding with articaine makes it a better choice for day-case regional anesthetic.[33]
A double blind randomized study was performed to compare three different doses of hyperbaric articaine (60 mg, 84 mg and 108 mg) in patients undergoing spinal ambulatory anesthesia for lower extremity surgery. Patients receiving 108 mg of articaine had a significantly higher incidence of hypotension (P = 0.018), nausea and vomiting (P = 0.027), delayed intake of oral fluids (P = 0.031), delayed sensory block (P = 0.017) and motor block recovery (P = 0.009). Peri-operative analgesia was needed in 5 patients receiving 60 mg articaine as compared to 2 and none in patients receiving 84 and 108 mg of articaine respectively. Based on this study, it can be recommended that 84 mg of articaine is a suitable dose to be used in day-case spinal anesthesia.[26]
A similar double-blind, randomized, controlled trial was carried out among 78 adult patients below the age of 65 years who underwent day-case knee arthroscopy under spinal anesthesia. The study aimed at comparing plain chloroprocaine 40 mg with plain articaine 60 mg as both these drugs have recently gained interest as short acting spinal anesthetics. It was observed that duration of sensory block was significantly shorter and complete recovery was significantly faster (P < 0.0001) with chloroprocaine as compared to articaine. The observations from the study helped in reinforcing the fact that incidence of transient neurologic symptoms are uncommon after spinal chloroprocaine and articaine. However, more studies are needed to establish the safety profile of chloroprocaine in spinal anesthesia.[34]
Role in brachial plexus blockade
Comparative studies have been carried out to observe the clinical and pharmacokinetic effects of articaine with lignocaine in patients undergoing auxiliary brachial plexus block anesthesia. The onset of sensory block was approximately 10 minutes in the median nerve distribution and was comparable with both the drugs. However, the significant observation was the rapid clearance and elimination of articaine as compared to lignocaine as was evident from the biexponential elimination pattern of lignocaine (t1/2α of 9.95±14.3 minutes and t1/2 β of 2.86 ± 1.55 hours) and monoexponential elimination pattern of articaine (t1/2 β of 0.95 ± 0.39 hour).The volume of distribution [V(d)] and clearance of articaine is significantly higher than lignocaine (P < 0.0001). The observations of these studies shows that articaine can be preferably used for achieving brachial plexus block as compared to lignocaine and the preference is based on pharmacokinetic and pharmacodynamic properties.[35]
Benefits in eyelid surgery
A wide number of minor oculoplastic surgical procedures are carried out under office anesthesia to avoid time and money expended in intravenous sedation. However, the main disadvantage is pain experienced during infiltration of local anesthetic agent. This is probably due to acidic pH of the local anesthetic solution. The pain decreases with addition of sodium bicarbonate due to decreased tissue irritation by a more physiologic pH. The disadvantage of adding sodium bicarbonate is decreased shelf life and a possibility of precipitate formation leading to central retinal artery embolization. Pain on injection may be less with articaine possibly due to less acidic pH and due to the presence of thiophene ring leading to faster transport across the nerve cell membrane.[36]
Application in procedures for tumescent local anesthesia:
Tumescent local anesthesia is used for surgery on skin and fatty tissue, such as liposuction and vein surgery. As large doses of local anesthetic are used in this, the chances of systemic toxicity are higher. Articaine has a similar analgesic efficacy as compared to lignocaine. Further it has a lower central nervous system toxicity and rapid hydrolysis of ester group in tissues with a low allergic potential. Met hemoglobin formation is also not a problem compared with prilocaine. Articaine is safe for tumescent local anesthesia.[37]
Use in intravenous regional anesthesia
The effectiveness of articaine has been tested in IVRA by comparing it with lignocaine and prilocaine during upper limb surgery.[38] The onset of sensory anesthesia was significantly (P < 0.05) shorter with articaine (2.5 minutes) as compared to lignocaine (11.1minutes) and prilocaine (10.9 minutes) but there was not any significant difference in the establishment of motor block. These effects correlated with the plasma levels of the local anesthetics measured with high performance liquid chromatography.[38] The comparative evaluation between articaine and prilocaine had been reported differently by earlier studies despite similar physiochemical properties of the two local anesthetic agents. It is assumed that articaine possess a low degree of toxicity as it is rapidly metabolized by the esterase's which can also make it an extremely useful agent for day care surgery. Pitkanen et al. studied the comparative effect of 0.5% articaine and 0.5% prilocaine in healthy volunteer subjects who were administered IVRA with these two agents at least a week apart from the last administration. The observation made by them revealed that these two anesthetics are quite similar in achieving onset of analgesia, establishment of motor blockade and recovery from the effect of these agents.[38] One remarkable finding associated with articaine usage included appearance of erythematous non-itching skin rash in 8 of 10 volunteers, which disappeared within 1 hour spontaneously, as compared to just 2 in prilocaine group.[39]
Role in bone marrow biopsy
Bone marrow biopsy is a day care procedure which is associated with excruciating pain and discomfort.[40,41] This is a routine procedure in the diagnosis and management of hematological malignancies and as such this subset of patients are exposed to multiple bone marrow biopsy procedures. The primary aim of the attending anesthesiologists is to provide pain relief on a day care basis.[42] Traditionally lignocaine infiltration has been used for years to provide required analgesia but recently articaine has become popular because of its better bone penetrating and nerve block properties.[24,41,43] Articaine when used in concentration of 40mg/ml provide slightly better analgesia than 20mg/ml of articaine solution.[43] However, infiltration anesthesia seems to be inadequate in biopsy procedures, as the pain occurs during stretching and disruption of bone marrow and it requires a larger volume of local anesthetic solution.[42] These limitations can be overcome by addition of supplementary analgesia in the form of oral analgesics such as tramadol.[43] An important factor in performance of such procedures is also the skill level of the operator.[40,43]
Impact of old age on metabolism of articaine
During the evaluation of the clinical profile of articaine, the impact of age on the pharmacokinetic and pharmacodynamic properties of articaine was studied in elderly and young volunteers undergoing routine dental procedures requiring administration of local anesthetics. High performance liquid chromatography was used to determine concentrations of articaine in serum and basic pharmacokinetic parameters were calculated according to standard procedures using a two-exponent equation. The clearance and volume of distribution were lower in the elderly as compared to young healthy volunteers. However, other parameters like area under the serum concentration-time curve, maximum drug concentration, terminal half life of the drug and time to reach maximum serum concentration did not show any significant statistical difference in young and elderly volunteers. The study showed that metabolism of articaine is age independent and no change in the dosage is required in the elderly population.[44]
Antibacterial effects of articaine
Quite a few drugs used in anesthesiology exhibit unusual clinical properties besides their known anesthetic effects and side effects. Drugs like ketamine, bupivacaine, lignocaine, articaine and ropivacaine have shown antibacterial effects when used in clinical practice. It has been observed that articaine can inhibit growth of various bacteria such as Pseudomonas aeruginosa, Proteus mirabilis, Staphylococcus aureus, Escherichia coli and many others.[45] These properties can be extremely useful for certain situations such as: tracheal suctioning and broncho-alveolar lavage, infiltration during local anesthesia, in nerve blocks and in tumescent anesthesia for liposuction.[45–47] The antibacterial properties can be of significantly useful in ophthalmology as has been successfully demonstrated in earlier studies.[45,48] There is evidence of potential antibacterial role of lignocaine and articaine during treatment of open wounds colonized or infected with antibiotic-resistant bacteria.[45,49] The mechanism of antibacterial action is possibly mediated via inhibition of cell wall synthesis or distortion of cytoplasmic membrane by the local anesthetics. This is supported by the evidence of membrane stabilizing properties of lignocaine when used in cardiac arrhythmias.[45]
Conclusion
No serious adverse events with the use of articaine have been reported so far. A faster onset of action, lowest peak plasma concentration, shorter elimination time, rapid recovery from the sensory and motor effects of the drugs and minimal effect on cardiovascular parameters makes articaine a better choice, over lignocaine, prilocaine and mepivacaine, for loco-regional anesthesia in day-care surgical procedures. However, large randomized studies are required to establish it as a first choice agent in various regional anesthetic techniques employed during day-care procedures.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Verma R, Alladi R, Jackson I. Day case and short stay surgery: 2. Anesthesia. 2011;66:417–34. doi: 10.1111/j.1365-2044.2011.06651.x. [DOI] [PubMed] [Google Scholar]
- 2.Gupta A, Kaur S, Khetarpal R, Kaur H. Evaluation of spinal and epidural anesthesia for day care surgery in lower limb and inguinoscrotal region. J Anesthesiol Clin Pharmacol. 2011;27:62–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Harsoor SS. Changing concepts in anesthesia for day care surgery. Indian J Anesth. 2010;54:485–8. doi: 10.4103/0019-5049.72635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salazar F, Bogdanovich A, Adalia R. Transient neurologic symptoms after spinal anesthesia using isobaric 2% mepivacaine and isobaric 2% lidocaine. Acta Anesthesiol Scand. 2001;45:240–5. doi: 10.1034/j.1399-6576.2001.450216.x. [DOI] [PubMed] [Google Scholar]
- 5.deWeert K, Traksel M, Gielen M. The incidence of transient neurological symptoms after spinal anesthesia with lidocaine compared to prilocaine. Anesthesia. 2000;55:1020–4. doi: 10.1046/j.1365-2044.2000.01618-4.x. [DOI] [PubMed] [Google Scholar]
- 6.Malamed SF, Gagnon S, Leblanc D. Efficacy of Artcaine: A new amide local anesthetic. J Am Dent Assoc. 2000;131:635–42. doi: 10.14219/jada.archive.2000.0237. [DOI] [PubMed] [Google Scholar]
- 7.Malamed SF, Gagnon S, Leblanc D. Articaine hydrochloride: A study of the safety of a new amide local anesthetic. J Am Dent Assoc. 2001;132:177–85. doi: 10.14219/jada.archive.2001.0152. [DOI] [PubMed] [Google Scholar]
- 8.Katyal V. The efficacy and safety of articaine versus lignocaine in dental treatments: A meta-analysis. J Dent. 2010;38:307–17. doi: 10.1016/j.jdent.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Vree TB, Van Oss GE, Gielen MJ, Booij LH. Epidural metabolism of articaine to its metabolite articainic acid in five patients after epidural administration of 600 mg articaine. J Pharm Pharmacol. 1997;49:158–63. doi: 10.1111/j.2042-7158.1997.tb06772.x. [DOI] [PubMed] [Google Scholar]
- 10.Hoizey G, Lamiable D, Gozalo C, Miric T, Thomas A, Binet L, et al. Determination of articaine in human plasma by liquid chromatography-mass spectrometry and its application in a preliminary pharmacokinetic study. J Pharm Biomed Anal. 2009;49:1082–7. doi: 10.1016/j.jpba.2009.01.028. [DOI] [PubMed] [Google Scholar]
- 11.Krzemińnski TF, Gilowski L, Wiench R, Płocica I, Kondzielnik P, Sielańnczyk A. Comparison of ropivacaine and articaine with epinephrine for infiltration anaesthesia in dentistry - a randomized study. Int Endod J. 2011;44:746–51. doi: 10.1111/j.1365-2591.2011.01881.x. [DOI] [PubMed] [Google Scholar]
- 12.Malamed SF. Local anesthetics: Dentistry's most important drugs, clinical update 2006. J Calif Dent Assoc. 2006;34:971–6. [PubMed] [Google Scholar]
- 13.Kämmerer PW, Palarie V, Daubländer M, Bicer C, Shabazfar N, Brüllmann D, et al. Comparison of 4% articaine with epinephrine (1:100,000) and without epinephrine in inferior alveolar block for tooth extraction: Double-blind randomized clinical trial of anesthetic efficacy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2012;113:495–9. doi: 10.1016/j.tripleo.2011.04.037. [DOI] [PubMed] [Google Scholar]
- 14.El-Qutob D, Morales C, Peláez A. Allergic reaction caused by articaine. Allergol Immunopathol. 2005;33:115–6. doi: 10.1157/13072924. [DOI] [PubMed] [Google Scholar]
- 15.Malamed SF, Gagnon S, Leblanc D. Articaine hydrochloride: A study of the safety of a new amide local anesthetic. J Am Dent Assoc. 2001;132:177–85. doi: 10.14219/jada.archive.2001.0152. [DOI] [PubMed] [Google Scholar]
- 16.Malamed SF, Gagnon S, Leblanc D. Efficacy of articaine: A new amide local anesthetic. J Am Dent Assoc. 2000;131:635–42. doi: 10.14219/jada.archive.2000.0237. [DOI] [PubMed] [Google Scholar]
- 17.Srinivasan N, Kavitha M, Loganathan CS, Padmini G. Comparison of anesthetic efficacy of 4% articaine and 2% lidocaine for maxillary buccal infiltration in patients with irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:133–6. doi: 10.1016/j.tripleo.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Mikesell P, Nusstein J, Reader A, Beck M, Weaver J. A comparison of articaine and lidocaine for inferior alveolar nerve blocks. J Endod. 2005;31:265–70. doi: 10.1097/01.don.0000140576.36513.cb. [DOI] [PubMed] [Google Scholar]
- 19.Malamed SF. 5th ed. St. Louis: Mosby; 2004. Handbook of local anesthesia; p. 320. [Google Scholar]
- 20.Becker DE, Reed KL. Essentials of Local Anesthetic Pharmacology. Anesth Prog. 2006;53:98–109. doi: 10.2344/0003-3006(2006)53[98:EOLAP]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malamed SF. 5th ed. St. Louis: Mosby; 2004. Handbook of local anesthesia; p. 73. [Google Scholar]
- 22.Pabst L, Nusstein J, Drum M, Reader A, Beck M. The Efficacy of a Repeated Buccal Infiltration of Articaine in Prolonging Duration of Pulpal Anesthesia in the Mandibular First Molar. Anesth Prog. 2009;56:128–34. doi: 10.2344/0003-3006-56.4.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oertel R, Rahn R, Kirch W. Clinical pharmacokinetics of articaine. Clin Pharmacokinet. 1997;33:417–25. doi: 10.2165/00003088-199733060-00002. [DOI] [PubMed] [Google Scholar]
- 24.Vree TB, Gielen MJ. Clinical pharmacology and the use of articaine for local and regional anesthesia. Best Pract Res Clin Anesthesiol. 2005;19:293–308. doi: 10.1016/j.bpa.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 25.Krzemińnski TF, Gilowski Ł, Wiench R, Płocica I, Kondzielnik P, Sielańnczyk A. Comparison of ropivacaine and articaine with epinephrine for infiltration anesthesia in dentistry - A randomized study. Int Endod J. 2011;44:746–51. doi: 10.1111/j.1365-2591.2011.01881.x. [DOI] [PubMed] [Google Scholar]
- 26.Kallio H, Snall EVT, Rosenberg PH. Hyperbaric articaine for day-case spinal anesthesia. Br J Anesth. 2006;97:704–9. doi: 10.1093/bja/ael222. [DOI] [PubMed] [Google Scholar]
- 27.Chelly JE, Gebhard R, Greger J, Al Samsam T. Regional anesthesia for outpatient orthopedic surgery. Minerva Anestesiol. 2001;67(9 Suppl 1):227–32. [PubMed] [Google Scholar]
- 28.Dijkstra T, Reesink JA, Verdouw BC, Van der Pol WS, Feberwee T, Vulto AG. Spinal anesthesia with articaine 5% vs. bupivacaine 0.5% for day-case lower limb surgery: A double-blind randomized clinical trial. Br J Anaesth. 2008;100:104–8. doi: 10.1093/bja/aem332. [DOI] [PubMed] [Google Scholar]
- 29.Kozlov SP, Svetlov VA, Luk’ianov MV. Pharmacology of local anesthetics and clinical aspects of segmental blocking. II. Spinal anesthesia. Anesteziol Reanimatol. 1998;5:37–42. [PubMed] [Google Scholar]
- 30.Malinovsky JM. Is 4% articaine suitable for spinal anesthesia. Eur J Anesthesiol. 2012;29:5–6. doi: 10.1097/EJA.0b013e32834de295. [DOI] [PubMed] [Google Scholar]
- 31.Bachmann M, Pere P, Kairaluoma P, Rosenberg PH, Kallio H. Randomized comparison of hyperbaric articaine and hyperbaric low-dose bupivacaine along with fentanyl in spinal anesthesia for day-case inguinal herniorrhaphy. Eur J Anesthesiol. 2012;29:22–7. doi: 10.1097/EJA.0b013e32834a11be. [DOI] [PubMed] [Google Scholar]
- 32.Dijkstra T, Reesink JA, Verdouw BC, Van der Pol WS, Feberwee T, Vulto AG. Spinal anesthesia with articaine 5% vs. bupivacaine 0.5% for day-case lower limb surgery: A double-blind randomized clinical trial. Br J Anesth. 2008;100:104–8. doi: 10.1093/bja/aem332. [DOI] [PubMed] [Google Scholar]
- 33.Hendriks MP, de Weert CJ, Snoeck MM, Hu HP, Pluim MA, Gielen MJ. Plain articaine or prilocaine for spinal anesthesia in day-case knee arthroscopy: A double-blind randomized trial. Br J Anesth. 2009;102:259–63. doi: 10.1093/bja/aen357. [DOI] [PubMed] [Google Scholar]
- 34.Förster JG, Kallio H, Rosenberg PH, Harilainen A, Sandelin J, Pitkänen MT. Chloroprocaine vs. articaine as spinal anesthetics for day-case knee arthroscopy. Acta Anesthesiol Scand. 2011;55:273–81. doi: 10.1111/j.1399-6576.2010.02325.x. [DOI] [PubMed] [Google Scholar]
- 35.Simon MA, Vree TB, Gielen MJ. Similar motor block effects with different disposition kinetics between lidocaine and (+ or -) Articaine in patients undergoing auxiliary brachial plexus block during day case surgery. Int J Clin Pharmacol Ther. 1999;37:598–607. [PubMed] [Google Scholar]
- 36.Steele EA, Ng JD, Poissant TM, Campbell NM. Comparison of injection pain of articaine and lidocaine in eyelid surgery. Ophthal Plast Reconstr Surg. 2009;25:13–5. doi: 10.1097/IOP.0b013e3181912016. [DOI] [PubMed] [Google Scholar]
- 37.Grossmann M, Sattler G, Pistner H, Oertel R, Richter K, Schinzel S, et al. Pharmacokinetics of articaine hydrochloride in tumescent local anesthesia for liposuction. J Clin Pharmacol. 2004;44:1282–9. doi: 10.1177/0091270004269014. [DOI] [PubMed] [Google Scholar]
- 38.Simon MA, Gielen MJ, Alberink N, Vree TB, van Egmond J. Intravenous regional anesthesia with 0.5% articaine, 0.5% lidocaine, or 0.5% prilocaine. A double-blind randomized clinical study. Reg Anesth. 1997;22:29–34. doi: 10.1016/s1098-7339(06)80053-2. [DOI] [PubMed] [Google Scholar]
- 39.Pitkanen MT, Xu M, Haasio J. Comparison of 0.5% Articaine and 0.5% Prilocaine in Intravenous Regional Anesthesia of the Arm: A Cross-Over Study in Volunteers. Reg Anesth Pain Med. 1999;24:131–5. [PubMed] [Google Scholar]
- 40.Vanhelleputte P, Nijs K, Delforge M, Evers G, Vanderschueren S. Pain during bone marrow aspiration: Prevalence and prevention. J Pain Symptom Manage. 2003;26:860–6. doi: 10.1016/s0885-3924(03)00312-9. [DOI] [PubMed] [Google Scholar]
- 41.Giannoutsos I, Grech H, Maboreke T, Morgenstern G. Performing bone marrow biopsies with or without sedation: A comparison. Clin Lab Haematol. 2004;26:201–4. doi: 10.1111/j.1365-2257.2004.00608.x. [DOI] [PubMed] [Google Scholar]
- 42.Bain BJ. Bone marrow biopsy morbidity: Review of 2003. J Clin Pathol. 2005;58:406–8. doi: 10.1136/jcp.2004.022178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuivalainen AM, Niemi-Murola L, Widenius T, Elonen E, Rosenberg PH. Comparison of articaine and lidocaine for infiltration anesthesia in patients undergoing bone marrow aspiration and biopsy. Eur J Pain. 2010;14:160–3. doi: 10.1016/j.ejpain.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 44.Oertel R, Ebert U, Rahn R, Kirch W. The Effect of Age on Pharmacokinetics of the Local Anesthetic Drug Articaine. Reg Anesth Pain Med. 1999;24:524–8. doi: 10.1016/s1098-7339(99)90043-3. [DOI] [PubMed] [Google Scholar]
- 45.Kaya K, Rota S, Dogan B, Kokten G, Gunaydin B, Bozdayi G. Comparison of the Antibacterial Effects of Two Local Anesthetics: Lidocaine and Articaine. Turk J Med Sci. 2007;37:7–10. [Google Scholar]
- 46.Olsen KM, Peddicord TE, Campbell GD, Rupp ME. Antimicrobial effects of lidocaine in bronchoalveolar lavage fluid. J Antimicrobiol Chem. 2000;45:217–9. doi: 10.1093/jac/45.2.217. [DOI] [PubMed] [Google Scholar]
- 47.Klein JA. Antibacterial effect of tumescent lidocaine. Plast Reconst Surg. 1999;104:1934–5. [PubMed] [Google Scholar]
- 48.Mullin GS, Rubinfeld RS. The antibacterial activity of topical anesthetics. Cornea. 1997;16:662–5. [PubMed] [Google Scholar]
- 49.Parr AM, Zoutman DE, Davidson JSD. Antimicrobial activity of lidocaine against bacteria associated with nosocomial infection. Ann Plast Surg. 1999;43:239–45. doi: 10.1097/00000637-199909000-00003. [DOI] [PubMed] [Google Scholar]


